Quality by Design of Pranoprofen Loaded Nanostructured Lipid Carriers and Their Ex Vivo Evaluation in Different Mucosae and Ocular Tissues
Abstract
:1. Introduction
2. Results
2.1. Lipid Screening
2.2. Design of Experiments
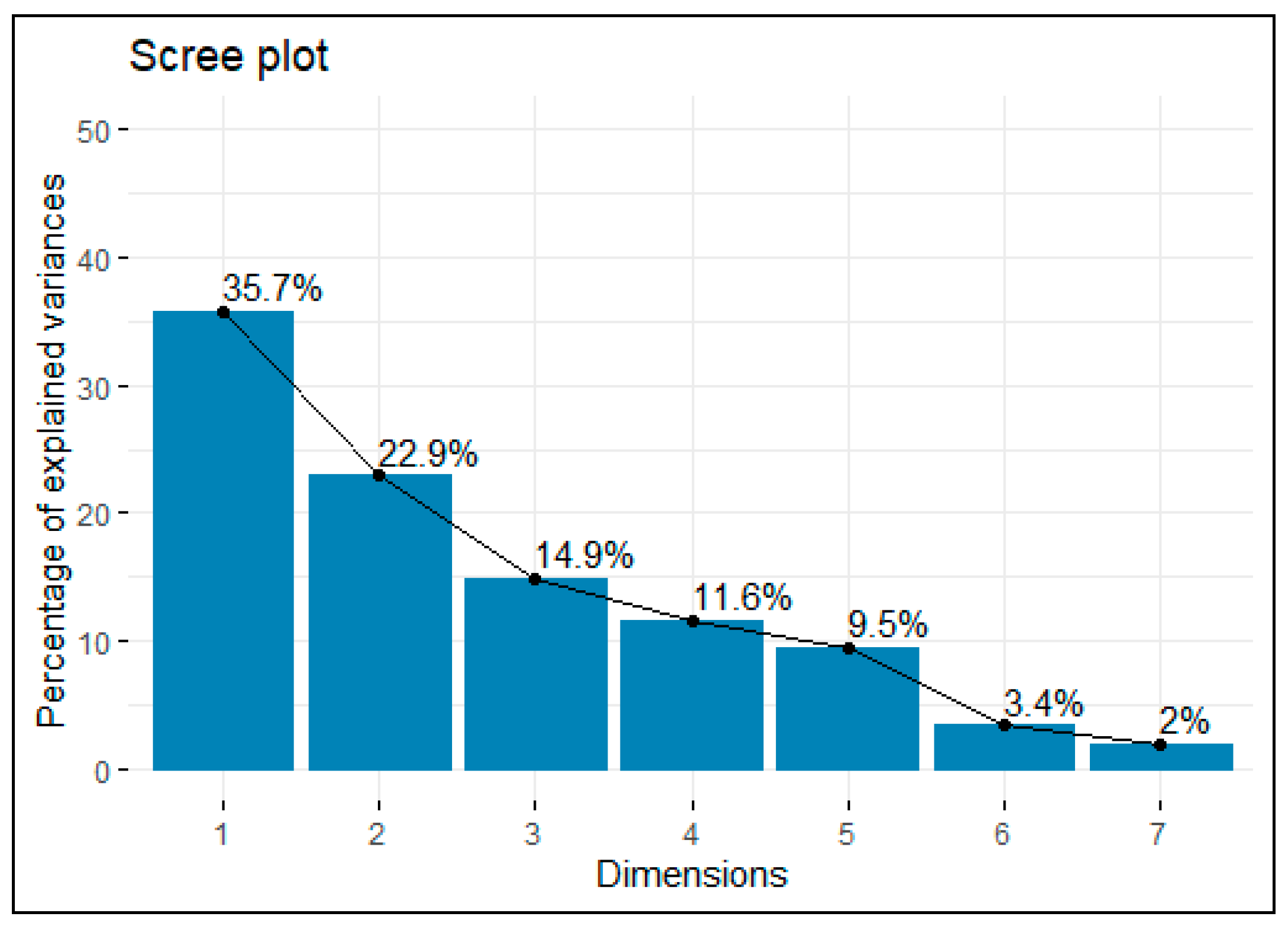
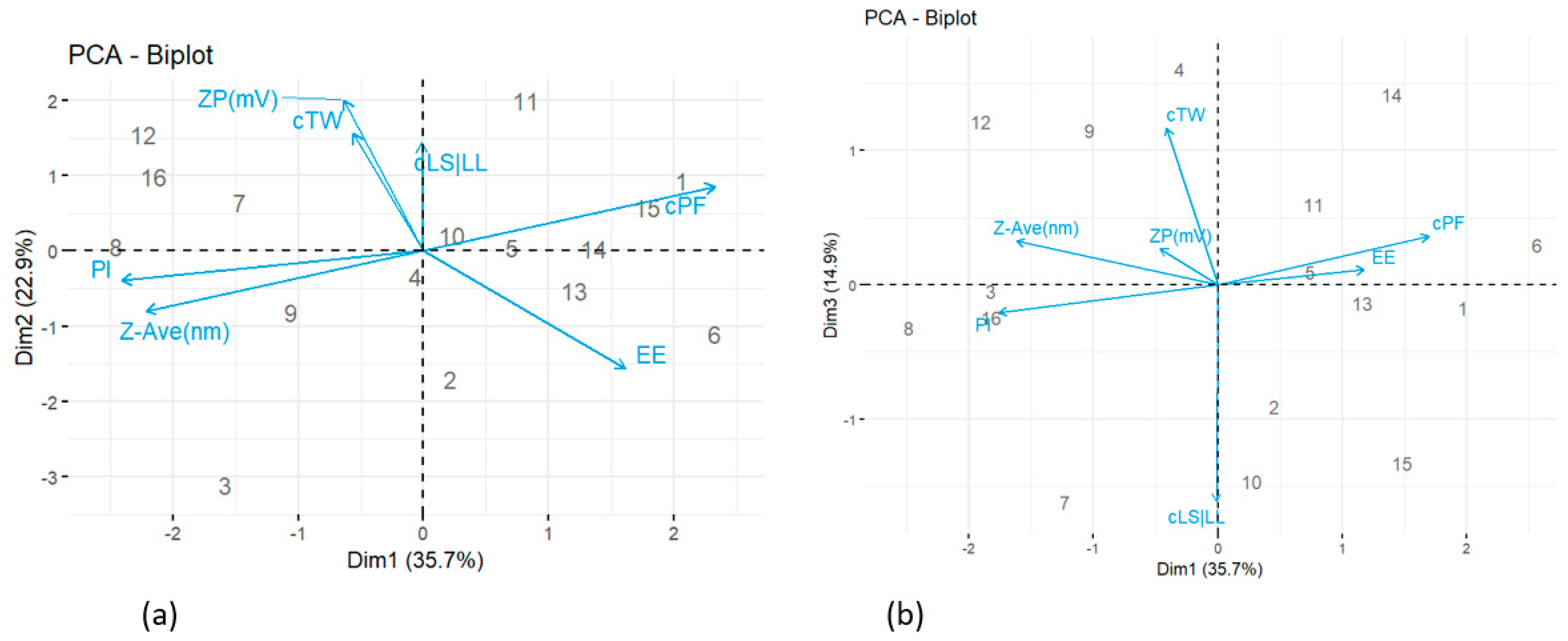
2.2.1. Principal Component Analysis (PCA)
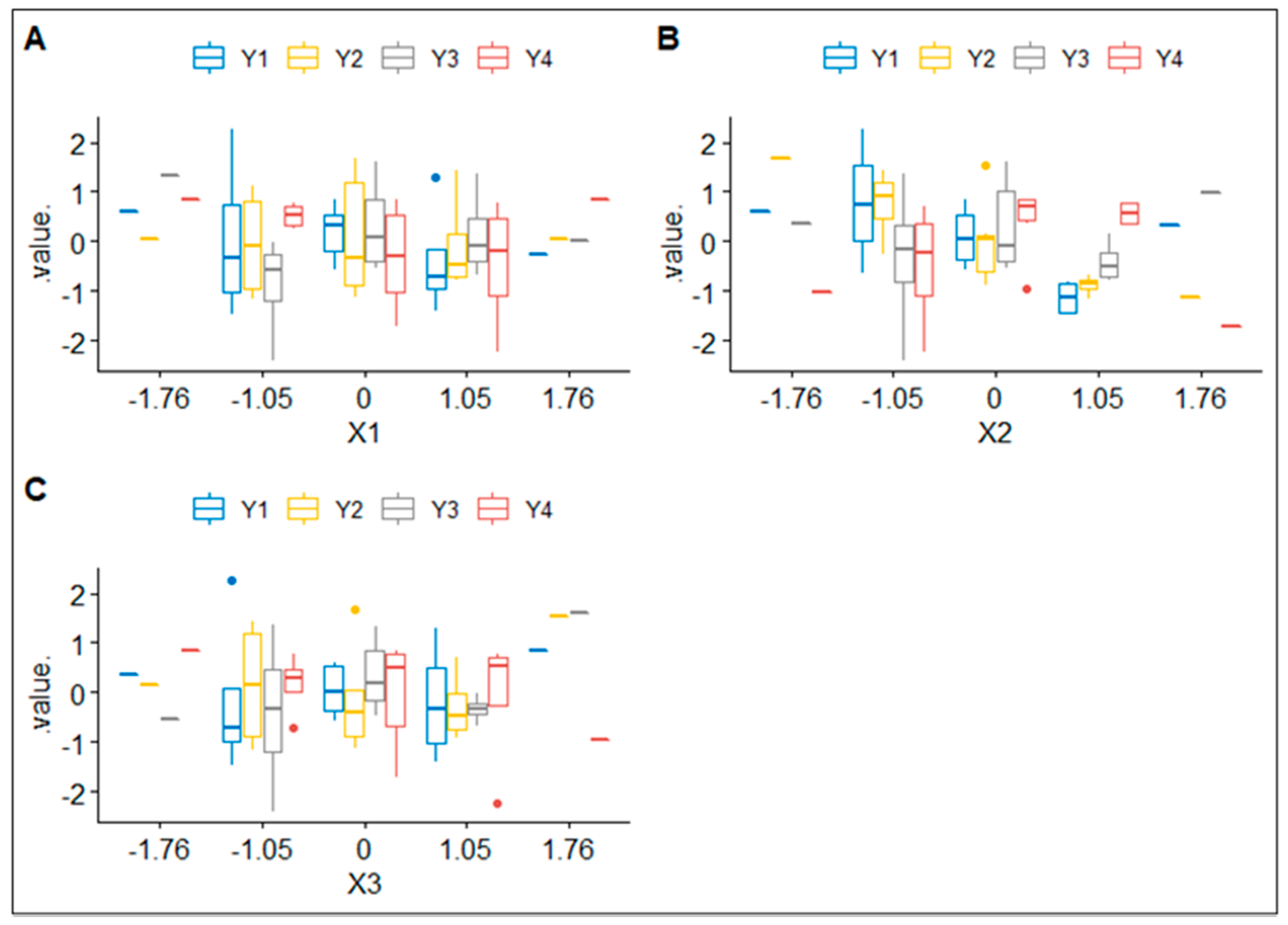
2.2.2. Boxplots
2.2.3. Multivariate Analysis of Variance
2.2.4. Four-Dimensional Graphics
2.3. Physicochemical Characterization
2.3.1. Particle Size, Zeta Potential and Encapsulation Efficiency
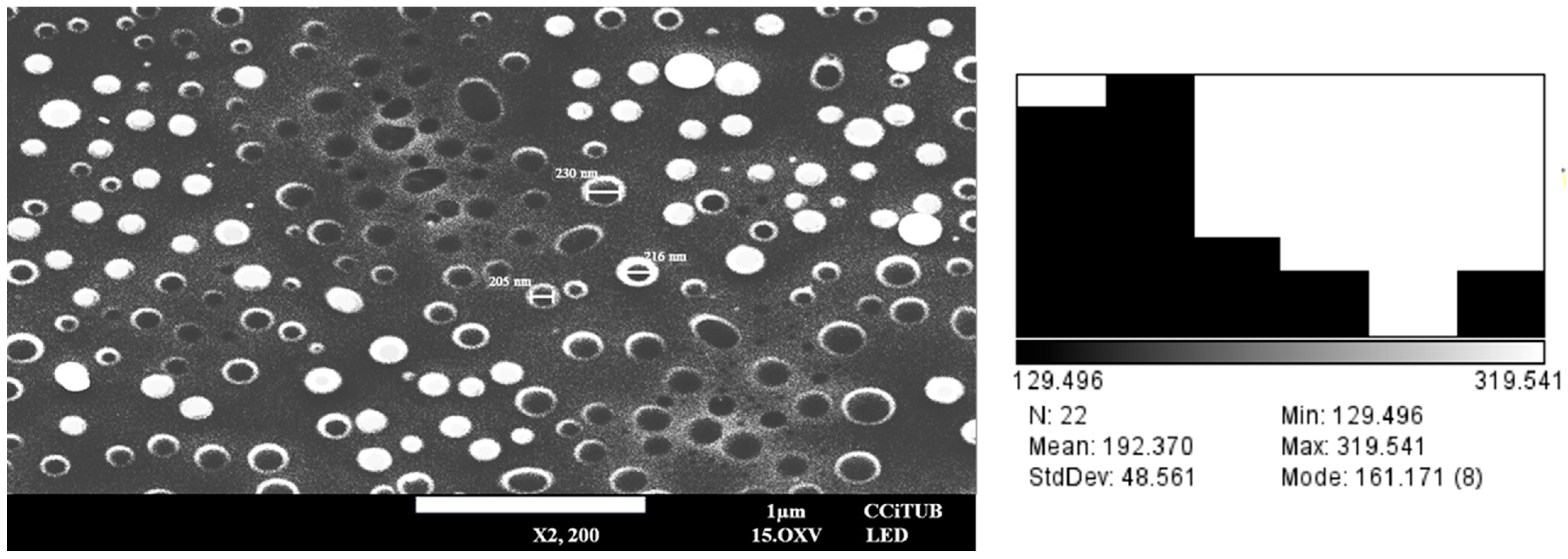
2.3.2. Morphological Characterization
2.4. Rheological Studies
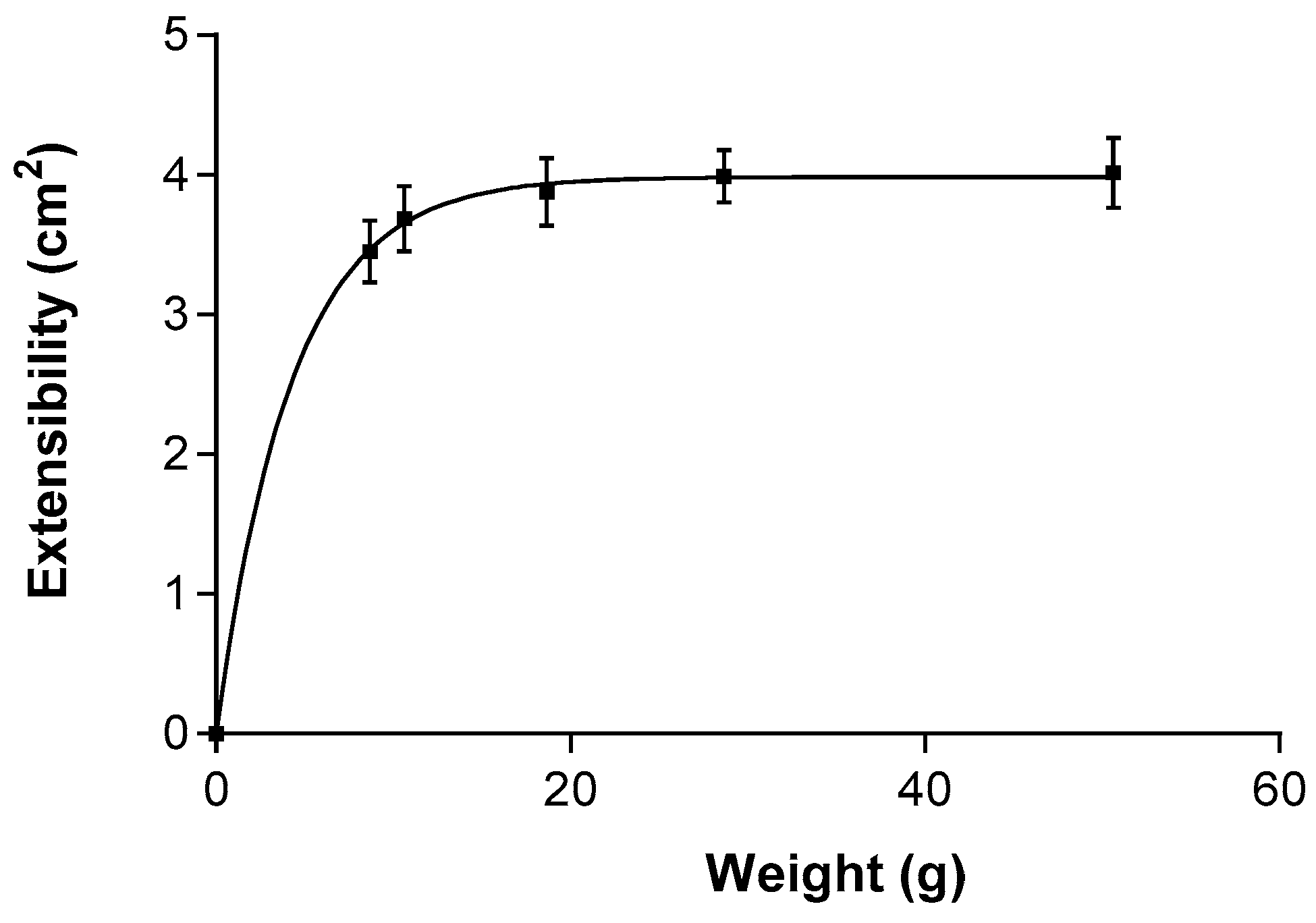
2.5. Extensibility (Spreadability)
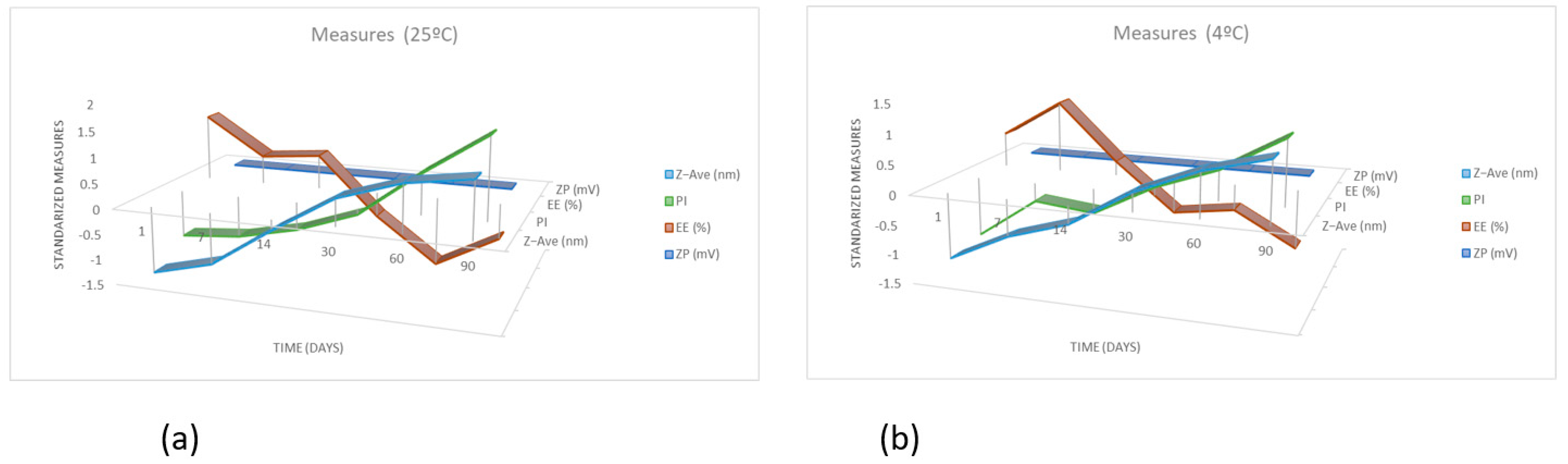
2.6. Stability Studies
2.7. Ex Vivo Permeation Studies in Porcine Mucosal Tissues
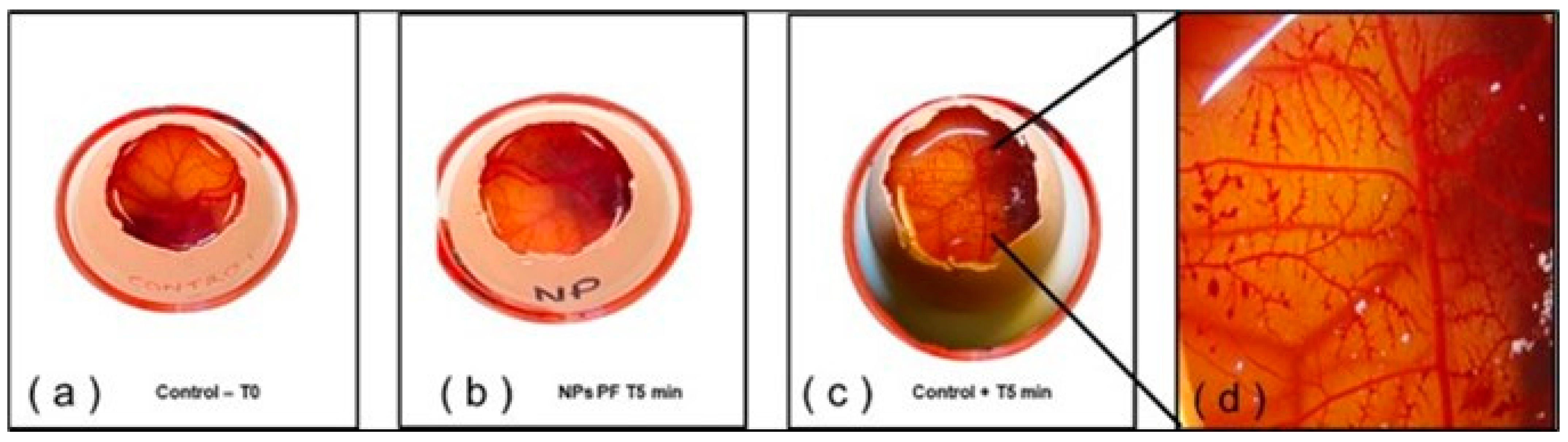
2.8. Hen’s Egg Test on the Chorioallantoic Membrane (HET-CAM)
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Lipid Screening
4.3. Development of NLCs
4.4. Design of Experiments
4.5. Physicochemical Characterization
4.5.1. Particle Size and Zeta Potential
4.5.2. Entrapment Efficiency
4.5.3. Morphological Characterization
4.6. Rheological Behavior
4.7. Extensibility (Spreadability)
4.8. Ex Vivo Permeation Study in Porcine Mucosal Tissues
4.9. Stability Studies
4.10. In Vitro Ocular Tolerance Study: Hen’s Egg Test on the Chorioallantoic Membrane (HET-CAM)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abrego, G.; Alvarado, H.; Souto, E.B.; Guevara, B.; Bellowa, L.H.; Garduño, M.L.; Garcia, M.L.; Calpena, A.C. Biopharmaceutical profile of hydrogels containing pranoprofen-loaded PLGA nanoparticles for skin administration: In vitro, ex vivo and in vivo characterization. Int. J. Pharm. 2016, 501, 350–361. [Google Scholar] [CrossRef]
- Cañadas-Enrich, C.; Abrego, G.; Alvarado, H.L.; Calpena-Campmany, A.C.; Boix-Montañes, A. Pranoprofen quantification in ex vivo corneal and scleral permeation samples: Analytical validation. J. Pharm. Biomed. Anal. 2018, 160, 109–118. [Google Scholar] [CrossRef]
- Aronson, J.K. Pranoprofen. In Meyler’s Side Effects of Drugs. The International Encyclopedia of Adverse Drug Reactions and Interactions, 16th ed.; Elsevier: Amsterdam, The Netherlands, 2016; Volume 7, p. 893. [Google Scholar]
- Akyol-Salman, I.; Leçe-Sertöz, D.; Baykal, O. Topical Pranoprofen 0.1% Is As Effective Anti-Inflammatory and Analgesic Agent as Diclofenac Sodium 0.1% After Strabismus Surgery. J. Ocul. Pharmacol. Ther. 2007, 23, 280–283. [Google Scholar] [CrossRef]
- Yao, B.; Wang, F.; Zhao, X.; Wang, B.; Yue, X.; Ding, Y.; Liu, G. Effect of a Topical Nonsteroidal Anti-Inflammatory Drug (0.1% Pranoprofen) on VEGF and COX-2 Expression in Primary Pterygium. Front. Pharmacol. 2021, 12, 709251. [Google Scholar] [CrossRef] [PubMed]
- Abrego, G.; Alvarado, H.; Souto, E.B.; Guevara, B.; Bellowa, L.H.; Parra, A.; Calpena, A.; Garcia, M.L. Biopharmaceutical profile of pranoprofen-loaded PLGA nanoparticles containing hydrogels for ocular administration. Eur. J. Pharm. Biopharm. 2015, 95, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Zhang, W.; Yan, P.; Mu, Y. Pranoprofen inhibits endoplasmic reticulum stress-mediated apoptosis of chondrocytes. Panminerva Med. 2020. ahead of print. [Google Scholar] [CrossRef]
- Rincón, M.; Calpena, A.C.; Clares, B.; Espina, M.; Garduño-Ramírez, M.L.; Rodríguez-Lagunas, M.J.; García, M.L.; Abrego, G. Skin-controlled release lipid nanosystems of pranoprofen for the treatment of local inflammation and pain. Nanomedicine 2018, 13, 2397–2413. [Google Scholar] [CrossRef] [PubMed]
- Mallandrich, M.; Calpena, A.C.; Clares, B.; Parra, A.; García, M.L.; Soriano, J.L.; Fernández-Campos, F. Nano-engineering of ketorolac tromethamine platforms for ocular treatment of inflammatory disorders. Nanomedicine 2021, 16, 401–414. [Google Scholar] [CrossRef]
- Battaglia, L.; Serpe, L.; Foglietta, F.; Muntoni, E.; Gallarate, M.; del Pozo-Rodriguez, A.; Solinis, M.A. Application of lipid nanoparticles to ocular drug delivery. Expert Opin. Drug Deliv. 2016, 13, 1743–1757. [Google Scholar] [CrossRef] [PubMed]
- Laffleur, F.; Bauer, B. Progress in nasal drug delivery systems. Int. J. Pharm. 2021, 607, 20994. [Google Scholar] [CrossRef]
- Akel, H.; Ismail, R.; Csóka, I. Progress and perspectives of brain-targeting lipid-based nanosystems via the nasal route in Alzheimer’s disease. Eur. J. Pharm. Biopharm. 2020, 148, 38–53. [Google Scholar] [CrossRef]
- Hua, S. Advances in Nanoparticulate Drug Delivery Approaches for Sublingual and Buccal Administration. Front. Pharmacol. 2019, 10, 1328. [Google Scholar] [CrossRef] [PubMed]
- Shirvan, A.R.; Hemmatinejad, N.; Bahrami, S.H.; Bashari, A. Fabrication of multifunctional mucoadhesive buccal patch for drug delivery applications. J. Biomed. Mater. Res. A 2021, 109, 2640–2656. [Google Scholar] [CrossRef]
- Macedo, A.S.; Castro, P.M.; Roque, L.; Thomé, N.G.; Reis, C.P.; Pintado, M.E.; Fonte, P. Novel and revisited approaches in nanoparticle systems for buccal drug delivery. J. Control. Release 2020, 320, 125–141. [Google Scholar] [CrossRef] [PubMed]
- Langoth, N.; Kalbe, J.; Bernkop-Schnürch, A. Development of buccal drug delivery systems based on a thiolated polymer. Int. J. Pharm. 2003, 252, 141–148. [Google Scholar] [CrossRef]
- de Oliveira, R.P.; de Oliveira, J.M.; Caramella, C. Special issue on vaginal drug delivery. Adv. Drug Deliv. Rev. 2015, 92, 1. [Google Scholar] [CrossRef]
- Rincón, M.; Calpena, A.C.; Fabrega, M.-J.; Garduño-Ramírez, M.L.; Espina, M.; Rodríguez-Lagunas, M.J.; García, M.L.; Abrego, G. Development of Pranoprofen Loaded Nanostructured Lipid Carriers to Improve Its Release and Therapeutic Efficacy in Skin Inflammatory Disorders. Nanomaterials 2018, 8, 1022. [Google Scholar] [CrossRef]
- Fangueiro, J.; Andreani, T.; Egea, M.A.; Garcia, M.L.; Souto, S.B.; Souto, E.B. Experimental factorial design applied to mucoadhesive lipid nanoparticles via multiple emulsion process. Colloids Surf. B Biointerfaces 2012, 100, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Politis, S.N.; Colombo, P.; Colombo, G.; Rekkas, D.M. Design of experiments (DoE) in pharmaceutical development. Drug Dev. Ind. Pharm. 2017, 43, 889–901. [Google Scholar] [CrossRef]
- Buttini, F.; Rozou, S.; Rossi, A.; Zoumpliou, V.; Rekkas, D.M. The application of Quality by Design framework in the pharmaceutical development of dry powder inhalers. Eur. J. Pharm. Sci. 2018, 113, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Peña, D. Análisis de Datos Multivariantes; McGraw-Hill/Interamericana: Madrid, Spain, 2002; pp. 137–171. [Google Scholar]
- Gómez-Segura, L.; Parra, A.; Calpena, A.C.; Gimeno, Á.; Boix-Montañes, A. Carprofen Permeation Test through Porcine Ex Vivo Mucous Membranes and Ophthalmic Tissues for Tolerability Assessments: Validation and Histological Study. Vet. Sci. 2020, 7, 152. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Villegas, V.; Clares-Naveros, B.; García-López, M.L.; Calpena-Campmany, A.C.; Bustos-Zagal, P.; Garduño-Ramírez, M.L. Development and characterization of two nano-structured systems for topical application of flavanones isolated from Eysenhardtia platycarpa. Colloids Surf. B Biointerfaces 2014, 116, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Rincón, M.; Silva-Abreu, M.; Espinoza, L.C.; Sosa, L.; Calpena, A.C.; Rodríguez-Lagunas, M.J.; Colom, H. Enhanced Transdermal Delivery of Pranoprofen Using a Thermo-Reversible Hydrogel Loaded with Lipid Nanocarriers for the Treatment of Local Inflammation. Pharmaceuticals 2021, 15, 22. [Google Scholar] [CrossRef] [PubMed]
- Middleton, S. Porcine ophthalmology. Vet. Clin. N. Am. Food Anim. Pract. 2010, 26, 557–572. [Google Scholar] [CrossRef]
- Van Eyk, A.D.; van der Bijl, P. Comparative permeability of various chemical markers through human vaginal and buccal mucosa as well as porcine buccal and mouth floor mucosa. Arch. Oral Biol. 2004, 49, 387–392. [Google Scholar] [CrossRef]
- Liu, C.; Xu, H.N.; Li, X.L. In vitro permeation of tetramethylpyr-azine across porcine buccal mucosa. Acta Pharmacol. Sin. 2002, 23, 792–796. [Google Scholar]
- Valls, M.M.; Labrador, A.M.; Bellowa, L.H.; Torres, D.B.; Granda, P.; Carmona, M.M.; Limón, D.; Campmany, A.C. Biopharmaceutical Study of Triamcinolone Acetonide Semisolid Formulations for Sublingual and Buccal Administration. Pharmaceutics 2021, 13, 1080. [Google Scholar] [CrossRef]
- Squier, C.A.; Mantz, M.J.; Schlievert, P.M.; Davis, C.C. Porcine Vagina Ex Vivo as a Model for Studying Permeability and Pathogenesis in Mucosa. J. Pharm. Sci. 2008, 97, 9–21. [Google Scholar] [CrossRef]
- Wadell, C.; Björk, E.; Camber, O. Permeability of porcine nasal mucosa correlated with human nasal absorption. Eur. J. Pharm. Sci. 2002, 18, 47–53. [Google Scholar] [CrossRef]
- Gómez-Segura, L.; Parra, A.; Calpena-Campmany, A.C.; Gimeno, Á.; de Aranda, I.G.; Boix-Montañes, A. Ex Vivo Permeation of Carprofen Vehiculated by PLGA Nanoparticles through Porcine Mucous Membranes and Ophthalmic Tissues. Nanomaterials 2020, 10, 355. [Google Scholar] [CrossRef]
- Patel, A.; Bell, M.; O’Connor, C.; Inchley, A.; Wibawa, J.; Lane, M.E. Delivery of ibuprofen to the skin. Int. J. Pharm. 2013, 457, 9–13. [Google Scholar] [CrossRef] [PubMed]
- González-Mira, E.; Egea, M.A.; García, M.L.; Souto, E.B. Design and ocular tolerance of flurbiprofen loaded ultrasound-engineered NLC. Colloids Surf. B Biointerfaces 2010, 81, 412–421. [Google Scholar] [CrossRef] [PubMed]
- López-Machado, A.; Díaz-Garrido, N.; Cano, A.; Espina, M.; Badia, J.; Baldomà, L.; Calpena, A.C.; Souto, E.B.; García, M.L.; Sánchez-López, E. Development of Lactoferrin-Loaded Liposomes for the Management of Dry Eye Disease and Ocular Inflammation. Pharmaceutics 2021, 13, 1698. [Google Scholar] [CrossRef] [PubMed]
- González-Fernández, F.; Bianchera, A.; Gasco, P.; Nicoli, S.; Pescina, S. Lipid-Based Nanocarriers for Ophthalmic Administration: Towards Experimental Design Implementation. Pharmaceutics 2021, 13, 447. [Google Scholar] [CrossRef] [PubMed]
- Celia, C.; Trapasso, E.; Cosco, D.; Paolino, D.; Fresta, M. Turbiscan Lab® Expert analysis of the stability of ethosomes® and ultradeformable liposomes containing a bilayer fluidizing agent. Colloids Surf. B Biointerfaces 2009, 72, 155–160. [Google Scholar] [CrossRef]
- Espinoza, L.C.; Silva-Abreu, M.; Clares, B.; Rodríguez-Lagunas, M.J.; Halbaut, L.; Cañas, M.-A.; Calpena, A.C. Formulation Strategies to Improve Nose-to-Brain Delivery of Donepezil. Pharmaceutics 2019, 11, 64. [Google Scholar] [CrossRef]
- Sánchez-López, E.; Esteruelas, G.; Ortiz, A.; Espina, M.; Prat, J.; Muñoz, M.; Cano, A.; Calpena, A.C.; Ettcheto, M.; Camins, A.; et al. Dexibuprofen Biodegradable Nanoparticles: One Step Closer towards a Better Ocular Interaction Study. Nanomaterials 2020, 10, 720. [Google Scholar] [CrossRef]
- Lindstrom, R.; Kim, T. Ocular permeation and inhibition of retinal inflammation: An examination of data and expert opinion on the clinical utility of nepafenac. Curr. Med. Res. Opin. 2006, 22, 397–404. [Google Scholar] [CrossRef]
- Menduni, F.; Davies, L.N.; Madrid-Costa, D.; Fratini, A.; Wolffsohn, J. Characterisation of the porcine eyeball as an in-vitro model for dry eye. Contact Lens Anterior Eye 2018, 41, 13–17. [Google Scholar] [CrossRef]
- Varela-Fernández, R.; García-Otero, X.; Díaz-Tomé, V.; Regueiro, U.; López-López, M.; González-Barcia, M.; Lema, M.I.; Otero-Espinar, F.J. Design, Optimization, and Characterization of Lactoferrin-Loaded Chitosan/TPP and Chitosan/Sulfobutylether-β-cyclodextrin Nanoparticles as a Pharmacological Alternative for Keratoconus Treatment. ACS Appl. Mater. Interfaces 2021, 13, 3559–3575. [Google Scholar] [CrossRef]
- Folle, C.; Marqués, A.M.; Díaz-Garrido, N.; Espina, M.; Sánchez-López, E.; Badia, J.; Baldoma, L.; Calpena, A.C.; García, M.L. Thymol-loaded PLGA nanoparticles: An efficient approach for acne treatment. J. Nanobiotechnol. 2021, 19, 359. [Google Scholar] [CrossRef] [PubMed]
- International Conference on Harmonization (ICH). Validation of Analytical Procedures: Text and Methodology, Q2(R1); ICH: Geneva, Switzerland, 2005. [Google Scholar]
- Prasertpol, T.; Tiyaboonchai, W. Nanostructured lipid carriers: A novel hair protective product preventing hair damage and discoloration from UV radiation and thermal treatment. J. Photochem. Photobiol. B Biol. 2020, 204, 111769. [Google Scholar] [CrossRef]
- Riangjanapatee, P.; Khongkow, M.; Treetong, A.; Unger, O.; Phungbun, C.; Jaemsai, S.; Bootsiri, C.; Okonogi, S. Development of Tea Seed Oil Nanostructured Lipid Carriers and In Vitro Studies on Their Applications in Inducing Human Hair Growth. Pharmaceutics 2022, 14, 984. [Google Scholar] [CrossRef] [PubMed]
- Velmurugan, R.; Selvamuthukumar, S. Development and optimization of ifosfamide nanostructured lipid carriers for oral delivery using response surface methodology. Appl. Nanosci. 2016, 6, 159–173. [Google Scholar] [CrossRef]
- Angelo, T.; El-Sayed, N.; Jurisic, M.; Koenneke, A.; Gelfuso, G.M.; Filho, M.C.; Taveira, S.F.; Lemor, R.; Schneider, M.; Gratieri, T. Effect of physical stimuli on hair follicle deposition of clobetasol-loaded Lipid Nanocarriers. Sci. Rep. 2020, 10, 176. [Google Scholar] [CrossRef]
- Sosa, L.; Calpena, A.C.; Silva-Abreu, M.; Espinoza, L.C.; Rincón, M.; Bozal, N.; Domenech, O.; Rodríguez-Lagunas, M.J.; Clares, B. Thermoreversible Gel-Loaded Amphotericin B for the Treatment of Dermal and Vaginal Candidiasis. Pharmaceutics 2019, 11, 312. [Google Scholar] [CrossRef] [PubMed]
- El Moussaoui, S.; Abo-Horan, I.; Halbaut, L.; Alonso, C.; Coderch, L.; Garduño-Ramírez, M.L.; Clares, B.; Soriano, J.L.; Calpena, A.C.; Fernández-Campos, F.; et al. Polymeric Nanoparticles and Chitosan Gel Loading Ketorolac Tromethamine to Alleviate Pain Associated with Condyloma Acuminata during the Pre- and Post-Ablation. Pharmaceutics 2021, 13, 1784. [Google Scholar] [CrossRef] [PubMed]
- Yoshio, I.; Iwata, A.; Isobe, M.; Takamatsu, R.; Higashi, M. The pharmacokinetics of pranoprofen in humans. Yakugaku Zasshi. 1990, 110, 509–515. [Google Scholar] [CrossRef]
- López-Machado, A.; Díaz, N.; Cano, A.; Espina, M.; Badía, J.; Baldomà, L.; Calpena, A.C.; Biancardi, M.; Souto, E.B.; García, M.L.; et al. Development of topical eye-drops of lactoferrin-loaded biodegradable nanoparticles for the treatment of anterior segment inflammatory processes. Int. J. Pharm. 2021, 609, 121188. [Google Scholar] [CrossRef] [PubMed]
- Derouiche, M.T.T.; Abdennour, S. HET-CAM test. Application to shampoos in developing countries. Toxicol. Vitr. 2017, 45, 393–396. [Google Scholar] [CrossRef] [PubMed]



| 0.1% PF | 0.5% PF | 1.0% PF | ||||
|---|---|---|---|---|---|---|
| Lipid Raw Materials | Solubility | Appearance | Solubility | Appearance | Solubility | Appearance |
| SOLID LIPIDS | ||||||
| Stearic acid | − | Semi-solid | − | Semi-solid | − | Semi-solid |
| Precifac® ATO | − | Hard | − | Hard | − | Hard |
| Compritol® 888 ATO | − | Soft | − | Soft | − | Soft |
| Lanette®18 | + | Hard | + | Hard | − | Hard |
| Precirol®ATO 5 | + | Hard | + | Hard | − | Hard |
| Gelucire® 44 | + | Semi-solid | − | Semi-solid | − | Semi-solid |
| Geleol® | − | Soft | − | Soft | − | Soft |
| LIQUID LIPIDS | ||||||
| Isopropyl myristate | + | Clear solution | − | Precipitation | − | Precipitation |
| Plantacare oil | + | Clear solution | + | Clear solution | − | Precipitation |
| Miglyol® 812 | + | Clear solution | − | Precipitation | − | Precipitation |
| Rose mosqueta oil | + | Clear solution | − | Precipitation | − | Precipitation |
| Jojoba oil | + | Clear solution | − | Precipitation | − | Precipitation |
| Castor oil | + | Clear solution | + | Clear solution | − | Precipitation |
| LAS (PEG-8 Caprylic/Capric Glycerides) | + | Clear solution | + | Clear solution | + | Clear solution |
| 1.5% PF | 2.0% PF | 3.0% PF | ||||
|---|---|---|---|---|---|---|
| Physical Mixtures of Lipids | Solubility | Appearance | Solubility | Appearance | Solubility | Appearance |
| LAS:Castor oil (50:50) | + | Clear solution | − | Precipitation | − | Precipitation |
| LAS:Castor oil (60:40) | + | Clear solution | − | Precipitation | − | Precipitation |
| LAS:Castor oil (75:25) | + | Clear solution | + | Clear solution | − | Precipitation |
| Precirol®ATO 5:(LAS-Castor oil (75:25)) 40:60 | + | Semi-solid | + | Semi-solid | − | Semi-solid |
| Precirol®ATO 5:(LAS-Castor oil (75:25)) 50:50 | + | Hard | + | Hard | − | Hard |
| Precirol®ATO 5:(LAS-Castor oil (75:25)) 60:40 | + | Hard | − | Hard | − | Hard |
| Factors | −1.68 | −1 | 0 | 1 | 1.68 |
|---|---|---|---|---|---|
| cSL/LL (%) | 43.2 | 50 | 60 | 70 | 76.8 |
| cPF (%) | 0.16 | 0.5 | 1 | 1.5 | 1.84 |
| cTW (%) | 2.16 | 2.5 | 3 | 3.5 | 3.84 |
| Formulations | Independent Variables | Dependent Variables | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| cSL/LL | cPF | cTW | Z-Ave (nm) | Pl | ZP (mV) | EE (%) | ||||
| PF-NLCs-N1 | 1 | 70 | 1 | 1.5 | 1 | 3.5 | 219.3 | 0.305 | −10.70 | 98.30 |
| PF-NLCs-N2 | 0 | 60 | 0 | 1 | −1.68 | 2.16 | 329.5 | 0.373 | −10.56 | 98.50 |
| PF-NLCs-N3 | −1 | 50 | −1 | 0.5 | −1 | 2.5 | 449.1 | 0.452 | −12.48 | 96.90 |
| PF-NLCs-N4 | −1.68 | 43.2 | 0 | 1 | 0 | 3 | 345.1 | 0.365 | −8.60 | 98.54 |
| PF-NLCs-N5 | 0 | 60 | 0 | 1 | 0 | 3 | 283.5 | 0.287 | −10.20 | 97.21 |
| PF-NLCs-N6 | −1 | 50 | 1 | 1.5 | −1 | 2.5 | 214.2 | 0.266 | −10.81 | 98.33 |
| PF-NLCs-N7 | 1 | 70 | −1 | 0.5 | −1 | 2.5 | 267.4 | 0.478 | −8.56 | 94.30 |
| PF-NLCs-N8 | 0 | 60 | −1.68 | 0.16 | 0 | 3 | 345.8 | 0.499 | −9.60 | 93.36 |
| PF-NLCs-N9 | −1 | 50 | −1 | 0.5 | 1 | 3.5 | 321.5 | 0.419 | −10.00 | 98.15 |
| PF-NLCs-N10 | 1.68 | 76.8 | 0 | 1 | 0 | 3 | 290.9 | 0.363 | −9.99 | 98.49 |
| PF-NLCs-N11 | 0 | 60 | 1.68 | 1.84 | 0 | 3 | 327.9 | 0.267 | −8.96 | 91.54 |
| PF-NLCs-N12 | 0 | 60 | 0 | 1 | 1.68 | 3.84 | 359.7 | 0.486 | −8.34 | 93.58 |
| PF-NLCs-N13 | 0 | 60 | 0 | 1 | 0 | 3 | 272.8 | 0.294 | −10.50 | 97.86 |
| PF-NLCs-N14 | −1 | 50 | 1 | 1.5 | 1 | 3.5 | 252.4 | 0.286 | −10.34 | 97.22 |
| PF-NLCs-N15 | 1 | 70 | 1 | 1.5 | −1 | 2.5 | 257.1 | 0.295 | −9.84 | 97.15 |
| PF-NLCs-N16 | 1 | 70 | −1 | 0.5 | 1 | 3.5 | 387.8 | 0.34 | −10.3 | 90.1 |
| Importance of Components | |||||||
|---|---|---|---|---|---|---|---|
| PC1 | PC2 | PC3 | PC4 | PC5 | PC6 | PC7 | |
| SD | 1.5804 | 1.2667 | 1.0206 | 0.9006 | 0.8158 | 0.4872 | 0.3770 |
| Prop V | 0.3568 | 0.2292 | 0.1488 | 0.1159 | 0.0951 | 0.0339 | 0.0203 |
| Cum P | 0.3568 | 0.5860 | 0.7348 | 0.8507 | 0.9458 | 0.9797 | 1.0000 |
| Importance of Components | |||||||
|---|---|---|---|---|---|---|---|
| PC1 | PC2 | PC3 | PC4 | PC5 | PC6 | PC7 | |
| cLS/LL | −0.01 | 0.51 | −0.79 | 0.15 | −0.25 | 0.16 | 0.04 |
| cPF | 0.83 | 0.31 | 0.18 | 0.12 | 0.26 | 0.25 | −0.19 |
| cTW | −0.20 | 0.56 | 0.57 | 0.18 | −0.53 | 0.04 | 0.00 |
| Z-Ave (nm) | −0.79 | −0.29 | 0.16 | 0.34 | 0.21 | 0.30 | 0.11 |
| Pl | −0.86 | −0.14 | −0.10 | −0.37 | −0.12 | 0.09 | −0.25 |
| ZP (mV) | −0.23 | 0.72 | 0.13 | −0.56 | 0.28 | 0.06 | 0.13 |
| EE(%) | 0.58 | −0.56 | 0.06 | −0.42 | −0.34 | 0.22 | 0.10 |
| Degrees of Freedom | Pillai | Approx F Statistic | Degrees of Freedom (Numerator) | Degrees of Freedom (Denominator) | Pr (>F) | |
|---|---|---|---|---|---|---|
| cLS/LL | 1 | 0.26843 | 0.8256 | 4 | 9 | 0.54092 |
| cPF | 1 | 0.69140 | 5.0409 | 4 | 9 | 0.02071 * |
| cTW | 1 | 0.12866 | 0.3322 | 4 | 9 | 0.84961 |
| Residuals | 12 | - | - | - | - | 0.54092 |
| Time (days) | Z-Ave (nm) ± SD | PI ± SD | ZP (mV) ± SD | EE (%) |
|---|---|---|---|---|
| 1 | 218.09 ± 3.97 | 0.297 ± 0.03 | −10.13 ± 0.11 | 98.02 |
| 7 | 232.07 ± 5.43 | 0.299 ± 0.06 | −10.01 ± 0.09 | 97.46 |
| 14 | 267.97 ± 3.93 | 0.304 ± 0.03 | −10.00 ± 0.07 | 97.54 |
| 30 | 300.72 ± 8.76 | 0.312 ± 0.05 | −9.89 ± 0.16 | 96.68 |
| 60 | 318.21 ± 5.12 | 0.329 ± 0.06 | −9.53 ± 0.20 | 96.03 |
| 90 | 326.07 ± 4.88 | 0.344 ± 0.05 | −9.48 ± 0.09 | 96.52 |
| Time (days) | Z-Ave (nm) ± SD | PI ± SD | ZP (mV) ± SD | EE (%) |
|---|---|---|---|---|
| 1 | 220.14 ± 4.92 | 0.288 ± 0.04 | −10.25± 0.10 | 97.99 |
| 7 | 242.10 ± 3.63 | 0.301 ± 0.04 | −10.16± 0.07 | 98.45 |
| 14 | 256.24 ± 4.09 | 0.299 ± 0.05 | −9.90 ± 0.09 | 97.73 |
| 30 | 284.15 ± 5.09 | 0.309 ± 0.04 | −9.76 ± 0.12 | 97.12 |
| 60 | 303.16 ± 5.94 | 0.316 ± 0.04 | −9.66 ± 0.15 | 97.23 |
| 90 | 315.02 ± 4.83 | 0.327 ± 0.06 | −9.52 ± 0.08 | 96.81 |
| Buccal | Sublingual | Nasal | Vaginal | Sclera | Cornea | |
|---|---|---|---|---|---|---|
| Jss (µg/h) | 2.46 | 2.34 | 3.26 | 2.59 | 2.57 | 5.02 |
| (2.14–2.96) | (2.14–2.63) | (2.45–5.11) | (1.96–2.84) | (2.15–2.83) | (4.15–6.32) | |
| Tl (h) | 4.10 | 3.67 | 1.18 | 0.94 | 3.66 | 0.09 |
| (3.92–4.37) | (3.14–4.99) | (0.83–1.94) | (0.51–1.31) | (2.41–4.93) | (0.04–0.11) | |
| P2 (10−1 h–1) | 0.41 | 0.45 | 1.41 | 3.26 | 0.45 | 18.52 |
| (0.38–0.42) | (0.33–0.53) | (0.86–2.01) | (1.27–1.77) | (0.33–0.69) | (15.15–41.67) | |
| P1 (10−3 cm) | 0.16 | 0.13 | 0.06 | 0.03 | 0.15 | 0.007 |
| (1.30–2.00) | (1.00–2.10) | (0.30–1.60) | (0.10–0.60) | (0.80–2.20) | (0.03–0.11) | |
| Kp (10−4 cm/h) | 0.65 (0.56–0.78) | 0.61 (0.56–0.69) | 0.85 (0.64–1.34) | 0.68 (0.51–0.74) | 0.67 (0.56–0.74) | 1.32 (1.09–1.66) |
| Membrane | Recovery (%) | RSD (%) |
|---|---|---|
| Buccal | 17.03 | 1.60 |
| Sublingual | 8.72 | 0.70 |
| Nasal | 16.03 | 1.36 |
| Vaginal | 12.65 | 0.71 |
| Sclera | 12.97 | 1.15 |
| Cornea | 15.01 | 1.34 |
| Membrane | Qr (µg/cm2/g) |
|---|---|
| Buccal | 1488.52 |
| (1227.62–1563.24) | |
| Sublingual | 3198.92 |
| (3005.43–3321.72) | |
| Nasal | 1879.92 |
| (1765.70–1990.44) | |
| Vaginal | 591.01 |
| (437.20–625.30) | |
| Sclera | 1842.73 |
| (1711.32–1897.90) | |
| Cornea | 745.09 |
| (623.72–804.57) |
| Membrane | Young Subject Css (ng/mL) | Elderly Subject Css (ng/mL) |
|---|---|---|
| Buccal | 2.14 | 4.04 |
| (1.87–2.58) | (3.51–4.87) | |
| Sublingual | 2.04 | 3.84 |
| (1.87–2.29) | (3.51–4.32) | |
| Nasal | 2.84 | 5.35 |
| (2.14–4.46) | (4.02–8.39) | |
| Vaginal | 2.26 | 4.25 |
| (1.71–2.48) | (3.22–4.67) | |
| Sclera | 2.24 | 4.22 |
| (1.87–2.47) | (3.53–4.65) | |
| Cornea | 4.38 | 8.24 |
| (3.62–5.51) | (6.81–10.38) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rincón, M.; Espinoza, L.C.; Silva-Abreu, M.; Sosa, L.; Pesantez-Narvaez, J.; Abrego, G.; Calpena, A.C.; Mallandrich, M. Quality by Design of Pranoprofen Loaded Nanostructured Lipid Carriers and Their Ex Vivo Evaluation in Different Mucosae and Ocular Tissues. Pharmaceuticals 2022, 15, 1185. https://doi.org/10.3390/ph15101185
Rincón M, Espinoza LC, Silva-Abreu M, Sosa L, Pesantez-Narvaez J, Abrego G, Calpena AC, Mallandrich M. Quality by Design of Pranoprofen Loaded Nanostructured Lipid Carriers and Their Ex Vivo Evaluation in Different Mucosae and Ocular Tissues. Pharmaceuticals. 2022; 15(10):1185. https://doi.org/10.3390/ph15101185
Chicago/Turabian StyleRincón, María, Lupe Carolina Espinoza, Marcelle Silva-Abreu, Lilian Sosa, Jessica Pesantez-Narvaez, Guadalupe Abrego, Ana Cristina Calpena, and Mireia Mallandrich. 2022. "Quality by Design of Pranoprofen Loaded Nanostructured Lipid Carriers and Their Ex Vivo Evaluation in Different Mucosae and Ocular Tissues" Pharmaceuticals 15, no. 10: 1185. https://doi.org/10.3390/ph15101185
APA StyleRincón, M., Espinoza, L. C., Silva-Abreu, M., Sosa, L., Pesantez-Narvaez, J., Abrego, G., Calpena, A. C., & Mallandrich, M. (2022). Quality by Design of Pranoprofen Loaded Nanostructured Lipid Carriers and Their Ex Vivo Evaluation in Different Mucosae and Ocular Tissues. Pharmaceuticals, 15(10), 1185. https://doi.org/10.3390/ph15101185











