Comparison of the 1-Year Visual and Anatomical Outcomes between Subthreshold Red (670 nm) and Yellow (577 nm) Micro-Pulse Laser Treatment for Diabetic Macular Edema
Abstract
:1. Introduction
2. Results
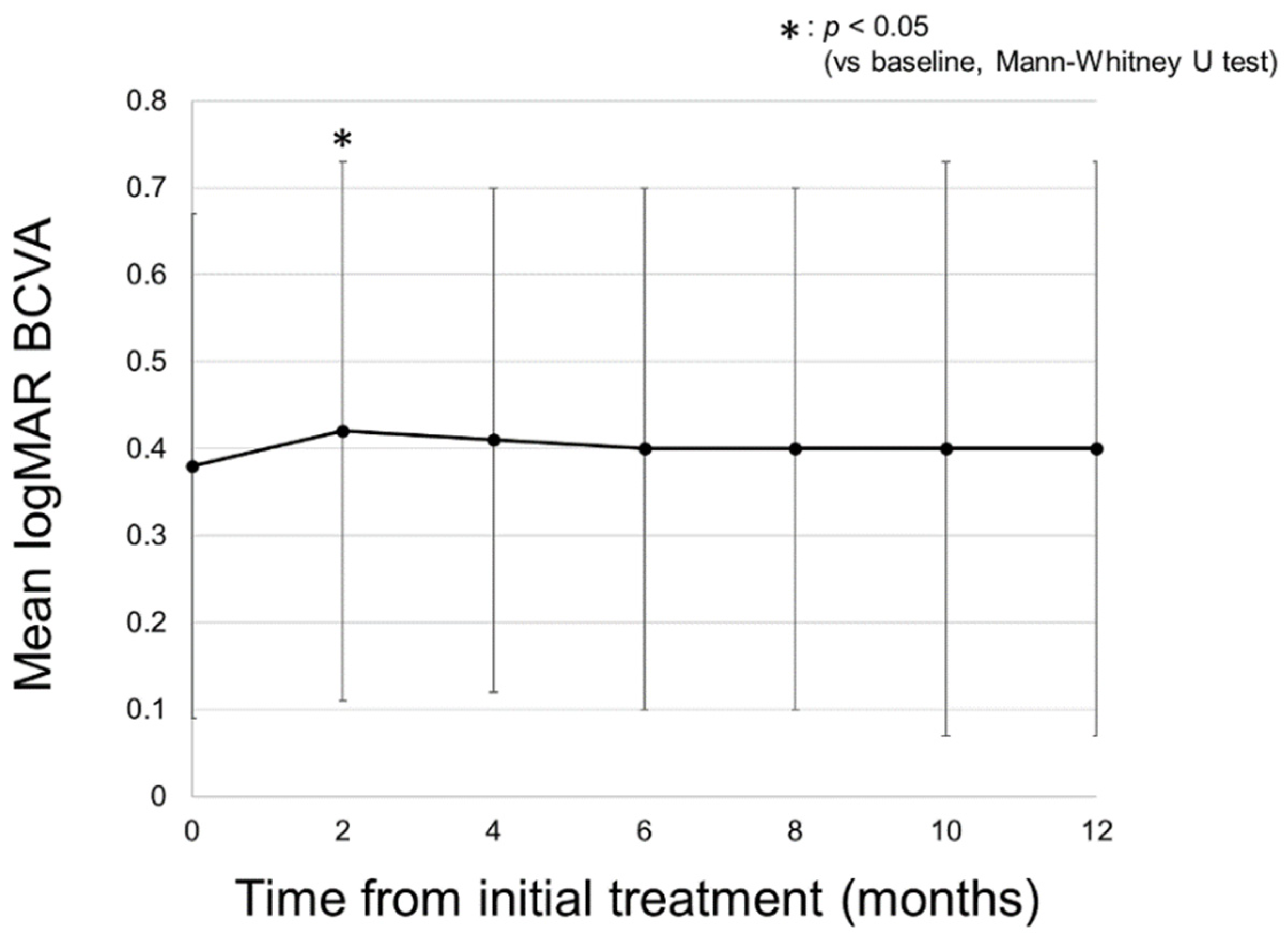
2.1. Changes in logMAR BCVA
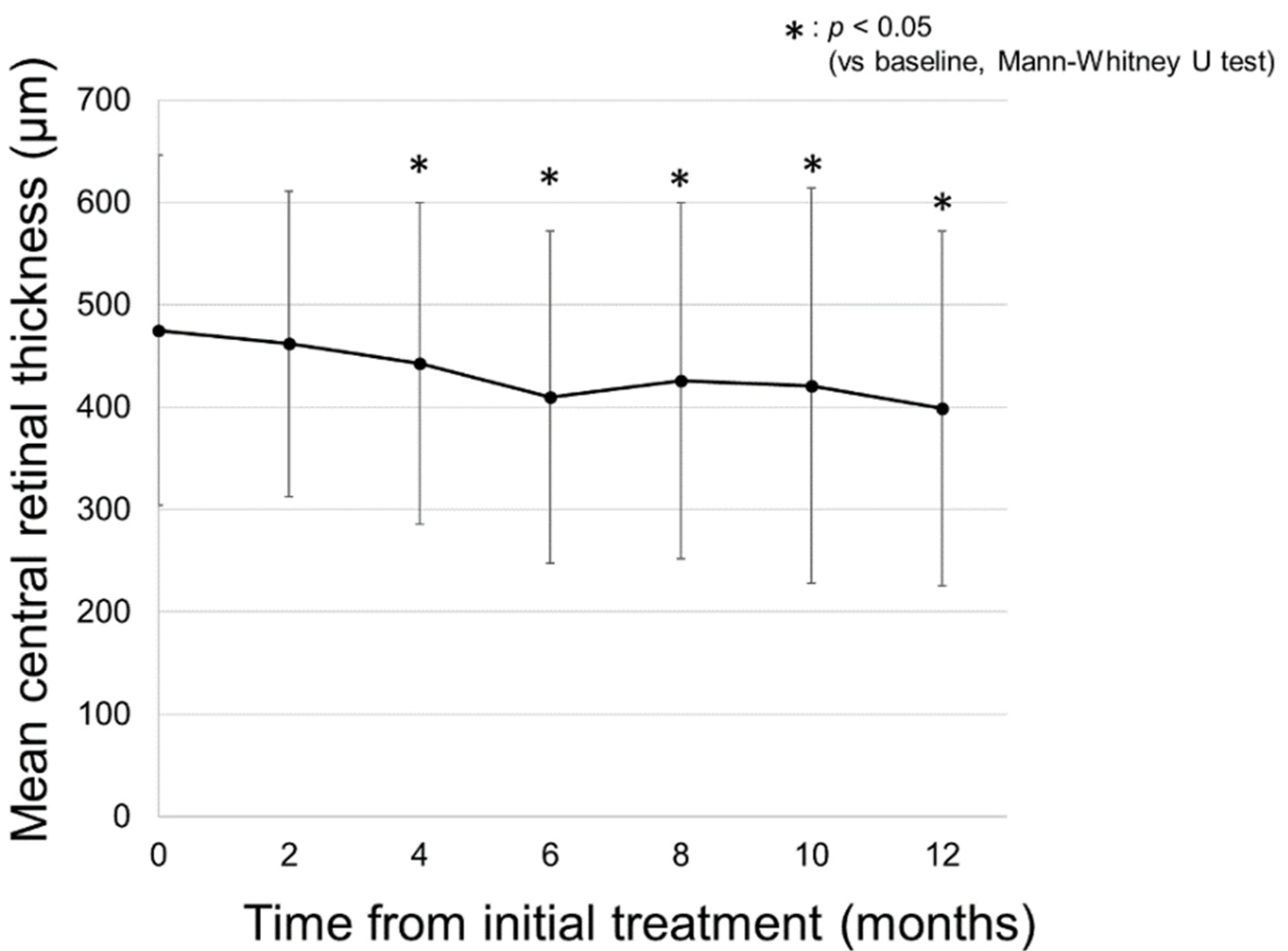
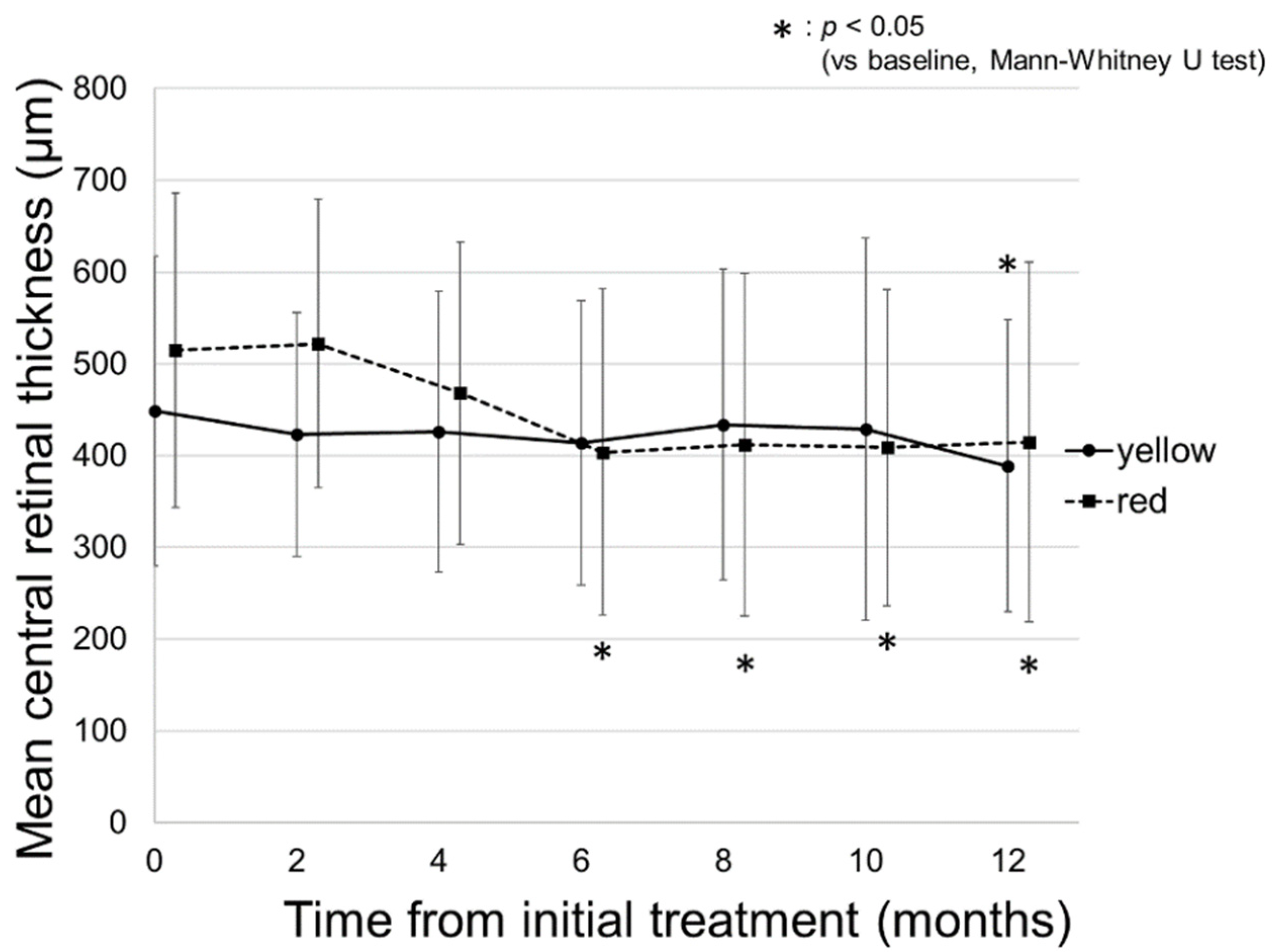
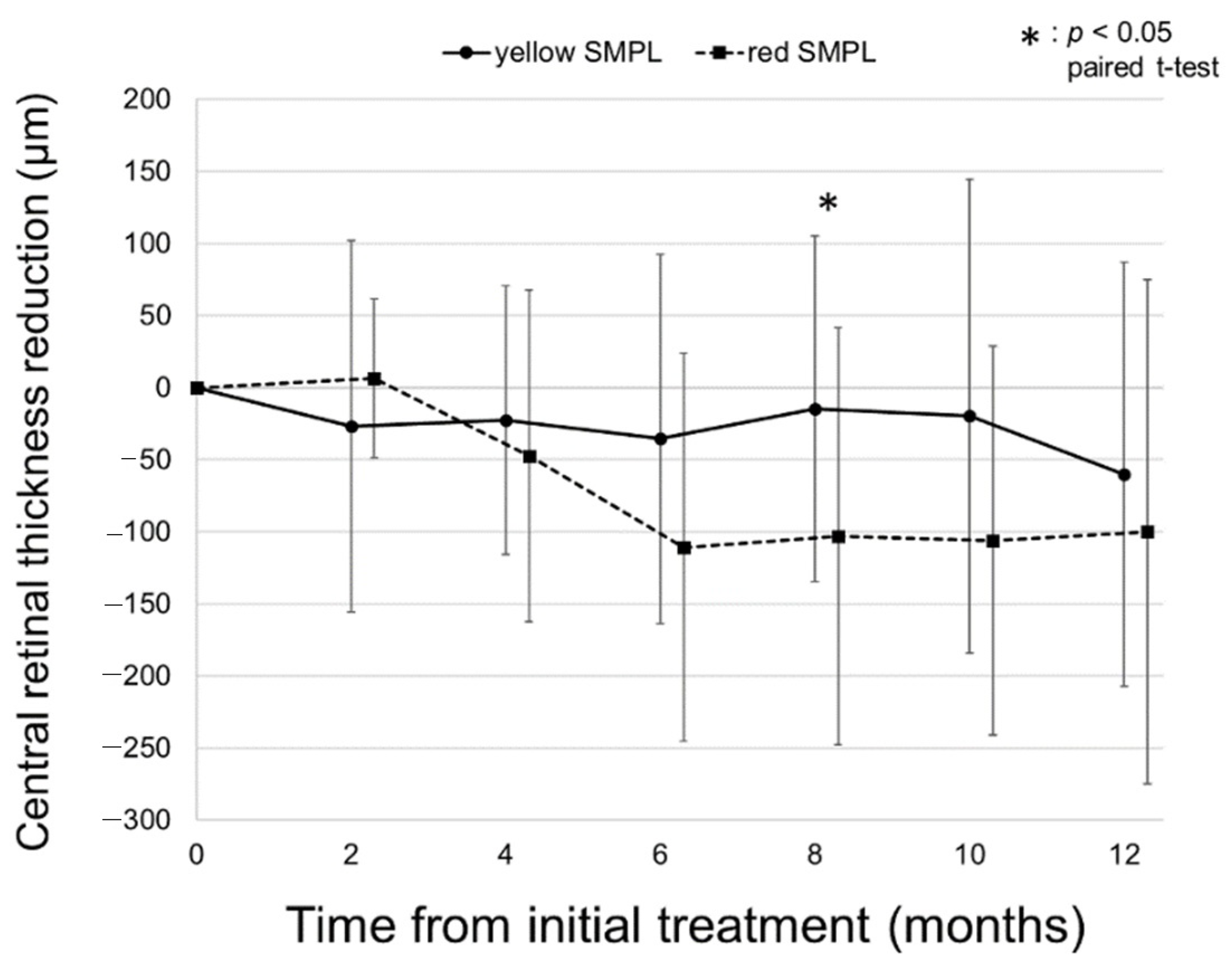
2.2. Changes in CRT on SD-OCT
2.3. Number of Total SMPL Treatments and Evaluation of the Safety
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. SMPL Treatment Protocol
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheung, N.; Mitchell, P.; Wong, T.Y. Diabetic retinopathy. Lancet 2010, 376, 124–136. [Google Scholar] [CrossRef]
- Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Early treatment diabetic retinopathy study research group. Arch. Ophthalmol. 1985, 103, 1796–1806. [CrossRef]
- Qi, H.-P.; Bi, S.; Wei, S.-Q.; Cui, H.; Zhao, J.-B. Intravitreal versus subtenon triamcinolone acetonide injection for diabetic macular edema: A systematic review and meta-analysis. Curr. Eye Res. 2012, 37, 1136–1147. [Google Scholar] [CrossRef] [PubMed]
- Boyer, D.S.; Nguyen, Q.D.; Brown, D.M.; Basu, K.; Ehrlich, J.S.; Ride and Rise Research Group. Outcomes with as-needed ranibizumab after initial monthly therapy: Long-Term outcomes of the phase III RIDE and RISE trials. Ophthalmology 2015, 122, 2504–2513.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korobelnik, J.-F.; Do, D.V.; Schmidt-Erfurth, U.; Boyer, D.S.; Holz, F.G.; Heier, J.S.; Midena, E.; Kaiser, P.; Terasaki, H.; Marcus, D.M.; et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology 2014, 121, 2247–2254. [Google Scholar] [CrossRef]
- Jackson, T.L.; Nicod, E.; Angelis, A.; Grimaccia, F.; Pringle, E.; Kanavos, P. Pars plana vitrectomy for diabetic macular edema: A systematic review, meta-analysis, and synthesis of safety literature. Retina 2017, 37, 886–895. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagenau, F.; Vogt, D.; Ziada, J.; Guenther, S.R.; Haritoglou, C.; Wolf, A.; Priglinger, S.G.; Schumann, R.G. Vitrectomy for diabetic macular edema: Optical coherence tomography criteria and pathology of the vitreomacular interface. Am. J. Ophthalmol. 2019, 200, 34–46. [Google Scholar] [CrossRef]
- Boyer, D.S.; Yoon, Y.H.; Belfort, R.; Bandello, F.; Maturi, R.K.; Augustin, A.J.; Li, X.-Y.; Cui, H.; Hashad, Y.; Whitcup, S.M. Three-Year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 2014, 121, 1904–1914. [Google Scholar] [CrossRef]
- Rosenblatt, A.; Udaondo, P.; Cunha-Vaz, J.; Sivaprasad, S.; Bandello, F.; Lanzetta, P.; Kodjikian, L.; Goldstein, M.; Habot-Wilner, Z.; Loewenstein, A. A collaborative retrospective study on the efficacy and safety of intravitreal dexamethasone implant (Ozurdex) in patients with diabetic macular edema: The european dme registry study. Ophthalmology 2020, 127, 377–393. [Google Scholar] [CrossRef] [Green Version]
- Bressler, S.B.; Glassman, A.R.; Almukhtar, T.; Bressler, N.M.; Ferris, F.; Googe, J.M.; Gupta, S.K.; Jampol, L.M.; Melia, M.; Wells, J.A. Five-Year outcomes of ranibizumab with prompt or deferred laser versus laser or triamcinolone plus deferred ranibizumab for diabetic macular edema. Am. J. Ophthalmol. 2016, 164, 57–68. [Google Scholar] [CrossRef] [Green Version]
- Friberg, T.R.; Karatza, E.C. The treatment of macular disease using a micropulsed and continuous wave 810-nm diode laser. Ophthalmology 1997, 104, 2030–2038. [Google Scholar] [CrossRef]
- Dorin, G. Evolution of retinal laser therapy: Minimum intensity photocoagulation (MIP). Can the laser heal the retina without harming it? Semin. Ophthalmol. 2004, 19, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Laursen, M.L.; Moeller, F.; Sander, B.; Sjoelie, A.K. Subthreshold micropulse diode laser treatment in diabetic macular oedema. Br. J. Ophthalmol. 2004, 88, 1173–1179. [Google Scholar] [CrossRef]
- Luttrull, J.K.; Musch, D.; Mainster, M.A. Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular oedema. Br. J. Ophthalmol. 2005, 89, 74–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vujosevic, S.; Bottega, E.; Casciano, M.; Pilotto, E.; Convento, E.; Midena, E. Microperimetry and fundus autofluorescence in diabetic macular edema: Subthreshold micropulse diode laser versus modified early treatment diabetic retinopathy study laser photocoagulation. Retina 2010, 30, 908–916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luttrull, J.K.; Dorin, G. Subthreshold diode micropulse laser photocoagulation (SDM) as invisible retinal phototherapy for diabetic macular edema: A review. Curr. Diabetes Rev. 2012, 8, 274–284. [Google Scholar] [CrossRef] [Green Version]
- Luttrull, J.K.; Sinclair, S.H. Safety of transfoveal subthreshold diode micropulse laser for fovea-involving diabetic macular edema in eyes with good visual acuity. Retina 2014, 34, 2010–2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moisseiev, E.; Abbassi, S.; Thinda, S.; Yoon, J.; Yiu, G.; Morse, L.S. Subthreshold micropulse laser reduces anti-VEGF injection burden in patients with diabetic macular edema. Eur. J. Ophthalmol. 2017, 28, 68–73. [Google Scholar] [CrossRef] [Green Version]
- Ohkoshi, K.; Yamaguchi, T. Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. Am. J. Ophthalmol. 2010, 149, 133–139.e1. [Google Scholar] [CrossRef]
- Takatsuna, Y.; Yamamoto, S.; Nakamura, Y.; Tatsumi, T.; Arai, M.; Mitamura, Y. Long-Term therapeutic efficacy of the subthreshold micropulse diode laser photocoagulation for diabetic macular edema. Jpn. J. Ophthalmol. 2011, 55, 365–369. [Google Scholar] [CrossRef]
- Vujosevic, S.; Martini, F.; Longhin, E.; Convento, E.; Cavarzeran, F.; Midena, E. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: Morphologic and functional safety. Retina 2015, 35, 1594–1603. [Google Scholar] [CrossRef]
- Chang, D.B.; Luttrull, J.K. Comparison of subthreshold 577 and 810 nm micropulse laser effects on heat-shock protein activation kinetics: Implications for treatment efficacy and safety. Transl. Vis. Sci. Technol. 2020, 9, 23. [Google Scholar] [CrossRef]
- Vujosevic, S.; Frizziero, L.; Martini, F.; Bini, S.; Convento, E.; Cavarzeran, F.; Midena, E. Single retinal layer changes after subthreshold micropulse yellow laser in diabetic macular edema. Ophthalmic Surg. Lasers Imaging Retin. 2018, 49, e218–e225. [Google Scholar] [CrossRef] [Green Version]
- Vujosevic, S.; Gatti, V.; Muraca, A.; Brambilla, M.; Villani, E.; Nucci, P.; Rossetti, L.; De Cilla’, S. Optical coherence tomography angiography changes after subthreshold micropulse yellow laser in diabetic macular edema. Retina 2020, 40, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, K.; Ohkoshi, K.; Ohde, S.; Deshpande, G.A.; Ebihara, N.; Murakami, A. Comparative efficacy of pure yellow (577-nm) and 810-nm subthreshold micropulse laser photocoagulation combined with yellow (561–577-nm) direct photocoagulation for diabetic macular edema. Jpn. J. Ophthalmol. 2014, 59, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Gawęcki, M. Micropulse laser treatment of retinal diseases. J. Clin. Med. 2019, 8, 242. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.; Ai, P.; Ai, Z.; Xu, G. Subthreshold diode micropulse laser versus conventional laser photocoagulation monotherapy or combined with anti-VEGF therapy for diabetic macular edema: A Bayesian network meta-analysis. Biomed. Pharmacother. 2018, 97, 293–299. [Google Scholar] [CrossRef]
- Akkaya, S.; Acikalin, B.; Dogan, Y.E.; Coban, F. Subthreshold micropulse laser versus intravitreal anti-VEGF for diabetic macular edema patients with relatively better visual acuity. Int. J. Ophthalmol. 2020, 13, 1606–1611. [Google Scholar] [CrossRef] [PubMed]
- Al-Barki, A.; Al-Hijji, L.; High, R.; Schatz, P.; Do, D.; Nguyen, Q.D.; Luttrull, J.K.; Kozak, I. Comparison of short-pulse subthreshold (532 nm) and infrared micropulse (810 nm) macular laser for diabetic macular edema. Sci. Rep. 2021, 11, 14. [Google Scholar] [CrossRef]
- Valera-Cornejo, D.A.; García-Roa, M.; Quiroz-Mendoza, J.; Arias-Gómez, A.; Ramírez-Neria, P.; Villalpando-Gómez, Y.; Romero-Morales, V.; García-Franco, R. Micropulse laser in patients with refractory and treatment-naïve center–involved diabetic macular edema: Short terms visual and anatomic outcomes. Ther. Adv. Ophthalmol. 2021, 13, 2515841420979112. [Google Scholar] [CrossRef] [PubMed]
- Trempe, C.L.; Mainster, M.A.; Pomerantzeff, O.; Avila, M.P.; Jalkh, A.E.; Weiter, J.J.; McMeel, J.W.; Schepens, C.L. Macular photocoagulation. Optimal wavelength selection. Ophthalmology 1982, 89, 721–728. [Google Scholar] [CrossRef]
- Mainster, M.A. Wavelength selection in macular photocoagulation. Ophthalmology 1986, 93, 952–958. [Google Scholar] [CrossRef]
- Singh, A.D. Ocular phototherapy. Eye 2013, 27, 190–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| All Patients (n = 43) | Yellow SMPL (n = 26) | Red SMPL (n = 17) | p Value (Yellow vs. Red) | |
|---|---|---|---|---|
| Age | 66.0 ± 10.1 | 65.3 ± 11.4 | 67.1 ± 7.9 | 0.97 |
| Gender Male (%) | 29(67.4%) | 18(69.2%) | 11(64.7%) | 0.76 |
| Duration of DM (months) | 121 ± 100 | 134 ± 106 | 100 ± 90 | 0.28 |
| Hb A1c (%) | 7.0 ± 1.2 | 7.0 ± 1.4 | 6.9 ± 0.8 | 0.82 |
| Mean BCVA | 0.38 ± 0.29 | 0.40 ± 0.33 | 0.35 ± 0.22 | 0.96 |
| Mean CRT | 475 ± 171 | 449 ± 169 | 515 ± 171 | 0.19 |
| Treatment-naïve eye (%) | 14(32.6%) | 8(30.8%) | 6(35.3%) | 0.76 |
| Variables | β-Coefficient | p-Value |
|---|---|---|
| Age | −1.3 × 10−4 | 0.98 |
| Male gender | −0.04 | 0.64 |
| Baseline logMAR BCVA | 0.77 | 1.0 × 10−5 |
| Baseline CRT | −8.6 × 10−5 | 0.73 |
| HbA1c | 0.067 | 0.055 |
| Duration of DM | 1.4 × 10−5 | 0.97 |
| Past treatment history for DME | 0.02 | 0.78 |
| SMPL (yellow: 0, red: 1) | −0.07 | 0.42 |
| Variables | β-Coefficient | p-Value |
|---|---|---|
| Age | −0.39 | 0.88 |
| Male gender | −20.5 | 0.70 |
| Baseline logMAR BCVA | 154.1 | 0.10 |
| Baseline CRT | 0.47 | 3.4 × 10−3 |
| HbA1c | −1.4 | 0.94 |
| Duration of DM | −0.13 | 0.62 |
| Past treatment history for DME | 51.9 | 0.33 |
| SMPL (yellow: 0, red: 1) | 1.0 | 0.98 |
| All Patients (n = 43) | Yellow SMPL (n = 26) | Red SMPL (n = 17) | p Value (Yellow vs. Red) | |
|---|---|---|---|---|
| Mean laser power (mW) | 269 ± 57 | 228 ± 19 | 327 ± 41 | <1.0 × 10−6 |
| Mean number of laser spots | 99.7 ± 9.8 | 102.1 ± 10.0 | 96.3 ± 8.6 | 1.0 × 10−5 |
| Mean (Median) number of total SMPL treatment | 5.1 ± 1.1 (6.0) | 5.1 ± 1.1 (5.0) | 5.2 ± 1.1 (6.0) | 0.48 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kikushima, W.; Shijo, T.; Furuhata, Y.; Sakurada, Y.; Kashiwagi, K. Comparison of the 1-Year Visual and Anatomical Outcomes between Subthreshold Red (670 nm) and Yellow (577 nm) Micro-Pulse Laser Treatment for Diabetic Macular Edema. Pharmaceuticals 2021, 14, 1100. https://doi.org/10.3390/ph14111100
Kikushima W, Shijo T, Furuhata Y, Sakurada Y, Kashiwagi K. Comparison of the 1-Year Visual and Anatomical Outcomes between Subthreshold Red (670 nm) and Yellow (577 nm) Micro-Pulse Laser Treatment for Diabetic Macular Edema. Pharmaceuticals. 2021; 14(11):1100. https://doi.org/10.3390/ph14111100
Chicago/Turabian StyleKikushima, Wataru, Taiyo Shijo, Yukiko Furuhata, Yoichi Sakurada, and Kenji Kashiwagi. 2021. "Comparison of the 1-Year Visual and Anatomical Outcomes between Subthreshold Red (670 nm) and Yellow (577 nm) Micro-Pulse Laser Treatment for Diabetic Macular Edema" Pharmaceuticals 14, no. 11: 1100. https://doi.org/10.3390/ph14111100
APA StyleKikushima, W., Shijo, T., Furuhata, Y., Sakurada, Y., & Kashiwagi, K. (2021). Comparison of the 1-Year Visual and Anatomical Outcomes between Subthreshold Red (670 nm) and Yellow (577 nm) Micro-Pulse Laser Treatment for Diabetic Macular Edema. Pharmaceuticals, 14(11), 1100. https://doi.org/10.3390/ph14111100







