Description of a PortableWireless Device for High-Frequency Body Temperature Acquisition and Analysis
Abstract
:1. Introduction
- Monitoring temperature in admitted patients. Temperature is normally measured every 8 to 12 hours. Common knowledge assumes that if the patient develops a fever, either it will persist until the next lecture, or the patient will be so sick to call the nurse, and the fever will be detected. Nevertheless, there are no empirical studies to back up this practice. A continuous monitoring of the patient's temperature can help detect intermittent fever bouts and unleash the consequent diagnostic and therapeutic interventions more objectively.
- Detecting fever in an outpatient setting. A common complaint in an outpatient clinic is the presence of fever. Fever often develops in the evening, and may not be confirmed during the visit to the clinic. Having the capability to record for a 24 or 48 hour period (“temperature Holter monitoring”) eliminates this problem and enables clinicians to arrive to more precise diagnosis.
- Detecting bacteremia as early as possible, eventually before the fever spike. The presence of bacteria in blood triggers the release of a number of cytokines that stimulate certain hypothalamic nucleii and start several physiologic measures aiming to rise the core temperature. The first of these mechanisms is a vasoconstriction of peripheral vessels, aiming to bypass the blood from the subcutaneous tissue to the deep tissues and therefore minimizing heat dissipation. This is reflected in an abrupt fall in peripheral temperature. Measuring simultaneously central and peripheral temperature has the potential to provide early signs of the development of bacteremia prior to the appearance of a full-blown fever. Furthermore, blood cultures would arguably be more sensitive in this setting than once the fever mechanisms have been unleashed.
- Providing new ways of categorizing fever. Classic fever patterns (i.e., “hectic”, “recurrent”, etc) are now considered obsolete by the research community, and are seldom used in clinical practice. New analytical techniques derived from complex time-series analysis (approximate entropy [6, 7], sample entropy [8], Lempel Ziv algorithm [9, 10], detrended fluctuation analysis [11]) have been shown useful to study and classify temperature, even in the absence of fever. For instance, it has been shown that there is a good correlation between physiological status and ApEn of the temperature profile in critically ill patients, and that ApEn is a prognostic marker as good as conventional scoring systems, with the advantage of being non-invasive and a continuous, rather than episodic, evaluation [12].
- Two functioning modes: Holter mode for long term ambulatory recordings, and real time mode.
- Real time wireless data transmission. Some devices need a cable (RS232, USB) to download the data.
- Standard Bluetooth radio interface. Other radio interfaces employed are not standard and therefore specific modules are necessary. Additionally, Bluetooth can be used directly in many mobile devices such as PDAs and phones.
- Enables patient movement. Even for admitted critically ill patients, some patient movement is necessary (surgery, X-Ray). Wireless data transmission can be resumed without data loss (internal buffer of up to 10 days) when wireless communication is out of range.
- Lightweight and small size. Portable device in contrast to other in-site monitors [21].
- High accuracy: 0.2°C. The accuracy found in other devices is usually lower [19]. Additionally, calibration with proper resistors can increase the accuracy, up to a threshold set by the probe accuracy.
- Signal processing based on signal entropy. Usually manufacturers only provide data editors as software tools.
- Two input channels. Comparative temperature analysis can be carried out.
- Non-invasive, comfortable. It can be applied to healthy subjects as control subjects, not only pathological subjects.
- Hot battery recharging. Batteries can be recharged by means of a mini USB connector, while in operation. This can increase the actual battery life indefinitely.
- High frequency. Readings are taken every minute, by averaging 60 measurements, one per second.
- Additionally, this device has enabled researchers to obtain important clinical results, as described in [12].
2. Device Description
2.1. Temperature Sensors
2.2. Thermistor Amplifier
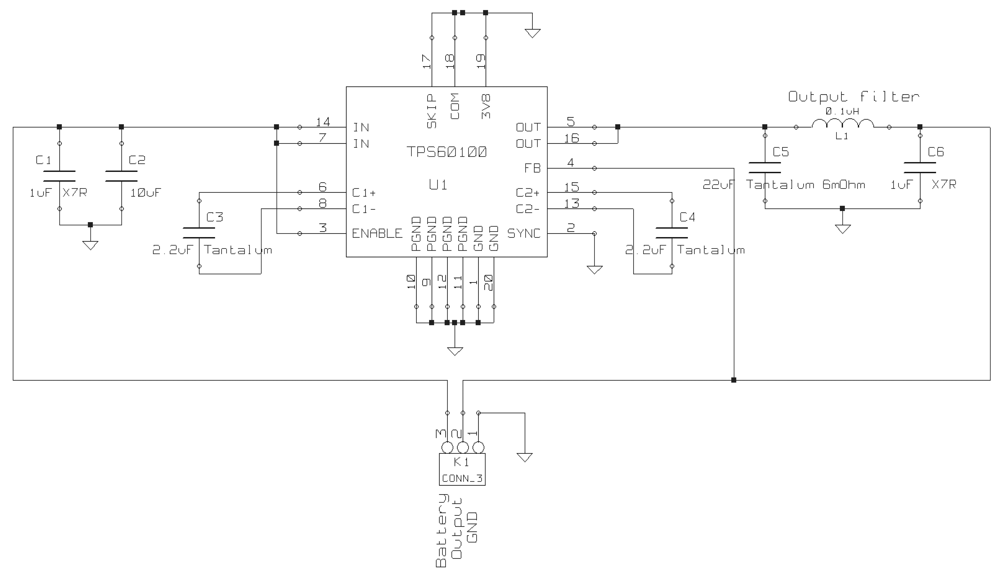
2.3. Power Source
- They deliver much closer to their rated capacity. Battery life is defined for 2,700 mAh rechargeable batteries, although current capacities, especially for disposable batteries, are even higher.
- They stay at about 1.2 V for most of their discharge cycle, high enough to feed most of the current available the step-up DC-DC converters.
- They are less expensive than alkaline or Li-ion batteries.
- Chargers are readily available. TherCom includes a Mini-USB connector and a charging circuit for in-place battery recharging from USB power [23].
- They can be recharged hundreds of times (minimum 500 cycles guaranteed).
- Off-the-shelf parts. Potential users are very familiar with this type of batteries.
- Can be recharged indefinitely at low current rates (lower than 120 mA) without damaging the batteries.
- Switch off external circuits when not needed. I/O pins are used to power the thermistor amplifier and the voltage references.
- The microcontroller periodically goes to sleep and the watchdog timer awakes it for temperature sampling.
- Clock the microcontroller at a lower frequency.
- Configure unused pin ports as outputs.
2.4. Voltage References
2.5. CPU
- High performance 8 bit RISC CPU.
- 40 MHz/10 MIPs sustained operation.
- 2.0 to 5.5 V operation.
- Flash, SRAM and EEPROM memory. One of the restrictions in embedded systems is the amount of memory available. This memory shortage is usually overcome by using additional external memories (such as microSD cards). However, body temperature measurement does not require high sampling rates and therefore small memories suffice to store all the data for long periods.
- Digital and analog ports. Digital ports are used to control external LEDs, power the amplifiers and the voltage references. Analog ports are used to acquire thermistor voltage, input ADC voltage references, and monitor batteries level.
- 4 timers.
- Up to 25 mA sink/source pin capability. Digital outputs power the amplifiers during sampling and the rest of the time remain in high impedance to save battery power. This sink/source capability is sufficient for the amplifiers and voltage references.
- Up to 16 analog channels. 2 analog channels are used for each thermistor, 2 channels as the ADC voltage references, 1 channel to monitor battery level, and another channel to monitor recharging block. Devices with 12 and 16 ADC channels are available in this family. Resolution of the converter is 10 bits, and the measurement range is 10° C. That gives a resolution of 0.01 °C per count, better than the accuracy of the sensors. Sample and hold circuit is included in the ADC.
- Up to 25 Ksps.
- Full-duplex asynchronous or half-duplex synchronous addressable USART. Serial interface is employed to communicate with the Bluetooth module.
- Programmable low voltage detect.
- Watchdog timer.
- In-System Programming Method.
2.6. ADC
- Configure pin as analog input.
- Select channel.
- Enable ADC module.
- Start conversion.
- Wait for the conversion to be completed.
- Read the result.
2.7. Bluetooth Module
2.8. Firmware
- Bluetooth module control. A high priority periodical interrupt polls module to read commands from the host computer (set device name, start acquisition, configure mode, get battery level, set date, set time, and retrieve data from memory). It also sends data to the host computer with the format: Date (yyyy-mm-dd), time (hh:mm:ss) and the two temperature samples (float values with two decimal digits). All the fields are separated by tabs. Temperatures are computed according to preprogrammed calibration curves.
- Off-line data acquisition in Holter mode. Bluetooth module is switched off to save power and enable the device to function for up to 10 days. A low priority interrupt samples the two channels every second. The device is in sleep mode for 90% of the time. It is awaken 10 ms before ADC inputs are sampled to get stable values. When 60 samples have been acquired, the mean is computed and stored in EEPROM with the format described above. All data are downloaded to the host computer afterwards, once the recording ends by restarting the device.
- Real time data acquisition. Functionality is similar to that of Holter mode, except that the Bluetooth module is not switched off, and when the mean is computed, resulting data are both stored in memory and transmitted to the host computer. Storing data in memory in real time mode enables the device to download lost data in case communication between host computer and TherCom was interrupted (for example, because of device out of range due to monitored patient displacement).
- Power control. In order to save battery power, peripherals are switched off during most of the time. They are only active when a temperature sample is acquired. Additionally, microcontroller is in sleep mode until watchdog timer periodically throws an interrupt to awake it. Then, one digital output is set active to power the thermistor amplifier and the voltage references. Both temperature channels are then measured, peripherals are switched off, and the microcontroller enters sleep mode again until next cycle. In offline mode, the Bluetooth module is also disabled.
2.9. Physical Features
2.10. Calibration
2.11. Software Application
2.12. Tools Used
3. Results and Discussion
- It provides a real-time, wireless monitorization of temperature. This may be useful both in patients admitted to a critical care unit and in relatively independent patients admitted to a general ward (and able to move freely).
- It provides two channels, thus allowing for a central and a peripheral temperature reading. This offers a good insight both on the thermoregulatory system and on the general perfusion status. Arguably, measuring the central/peripheral gradient will allow for an early detection of an impending haemodynamic deterioration or bacteraemia.
- Recording the lectures on a memory allows for its use as a temperature Holter device. This may be extremely useful in patients attending an outpatient clinic because of occasional fever bouts, not confirmed during the physical exam.
- It provides a complexity analysis of the temperature profile. ApEn has proved to have prognostic implications on survival of critical patients (reference), and could also be useful in the differential diagnosis of certain diseases.
4. Conclusion
References and Notes
- Varela, M.; Jimenez, L.; Farina, R. Complexity analysis of the temperature curve: new information from body temperature. Eur. J. Appl. Physiol. 2003, 3-4, 230–237. [Google Scholar]
- Varela, M.; Calvo, M.; Chana, M.; Gomez-Mestre, I.; Asensio, R.; Galdos, P. Clinical implications of temperature curve complexity in critically ill patients. Crit. Care Med. 2005, 12, 2764–2771. [Google Scholar]
- Varela, M.; Churruca, J.; Gonzalez, A.; Martin, A.; Ode, J.; Galdos, P. Temperature curve complexity predicts survival in critically ill patients. Am. J. Respir. Crit. Care Med. 2006, 3, 290–298. [Google Scholar]
- Boudoulas, H.; Schaal, S.; Lewis, R. P.; Robinson, J. Superiority of 24-hour outpatient monitoring over multi-stage exercise testing for the evaluation of syncope. 1979, 103–108. [Google Scholar]
- Hansen, T.; Jeppesen, J.; Rasmussen, S.; Ibsen, H.; Torp-Pedersen, C. Ambulatory blood pressure and mortality: a population-based study. Hypertension 2005, 4, 499–504. [Google Scholar]
- Pincus, S. M.; Gladstone, I. M.; Ehrenkranz, R. A. A regularity statistic for medical data analysis. J Clin Monit 1991, 7, 335–345. [Google Scholar]
- Hornero, R.; Aboy, M.; Abasolo, D.; McNames, J.; Goldstein, B. Interpretation of approximate entropy: analysis of intracranial pressure approximate entropy during acute intracranial hypertension. IEEE Trans. Biomed. Eng. 2005, 10, 1671–1680. [Google Scholar]
- Aboy, M.; Cuesta-Frau, D.; Austin, D.; Mico-Tormos, P. Characterization of Sample Entropy in the Context of Biomedical Signal Analysis. 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2007; pp. 5942–5945. [Google Scholar]
- Lempel, A.; Ziv, J. On the complexity of finite sequences. IEEE Trans. Inform. Theory 1976, 22, 75–81. [Google Scholar]
- Aboy, M.; Hornero, R.; Abasolo, D.; Alvarez, D. Interpretation of the lempel-ziv complexity measure in the context of biomedical signal analysis. IEEE Trans. Biomed. Eng. 2006, 11, 2282–2288. [Google Scholar]
- Peng, C.-K.; Buldyrev, S. V.; Havlin, S.; Simons, M.; Stanley, H. E.; Goldberger, A. L. Mosaic organization of DNA nucleotides. Phys. Rev. E 1994, 49, 1685–1689. [Google Scholar]
- Cuesta-Frau, D.; Varela, M.; Miró, P.; Galdós, P.; Abásolo, D.; Hornero, R.; Aboy, M. Predicting survival in critical patients by use of body temperature regularity measurement based on approximate entropy. Medical and Biological Engineering and Computing 2007, 45, 671–678. [Google Scholar]
- Coulic, V.; Novikov, V.; Devriendt, J.; Gillet, C.; Bodson, A.; DeKoster, E. Use of a Temperature Gradient Measuring Device in Monitoring of Diabetic and Critically Ill Patients. 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2007; pp. 3508–3511. [Google Scholar]
- Mohy-Ud-Din, Z.; Woo, S.; Lee, J. H.; Lee, S.; Young, P. S.; Won, C.; Cho, J. H. Wireless Skin Temperature Sensing Patch. IEEE International Conference on Multisensor Fusion and Integration for Intelligent Systems; 2008; pp. 258–260. [Google Scholar]
- Wong, C.; Chang, K. Development of a Portable Multi–functional Patient Monitor. 22nd Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2000; pp. 2611–2614. [Google Scholar]
- Chien, R.; Tai, C. A New Wireless-Type Physiological Signal Measuring System Using a PDA and the Bluetooth Technology. IEEE International Conference on Industrial Technology; 2006; pp. 119–120. [Google Scholar]
- Bor-Shing, L.; Bor-Shyh, L.; Nai-Kuan, C.; Fok-Ching, C.; Sao-Jie, C. RTWPMS: A Real-Time Wireless Physiological Monitoring System. IEEE Transactions on Information Technology in Biomedicine 2006, 10, 647–656. [Google Scholar]
- Chihashi, F.; Sankai, Y. Development of a Portable Vital Sensing System for Home Telemedicine. 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2007; pp. 5872–5877. [Google Scholar]
- SpectrumTecnologiesInc. Watchdog Dataloggers. 2008. http://www.specmeters.com/clearance/index.html.
- MSRElectronicsGmbH. Dataloggers and measuring instruments. 2008. http://www.msr.ch/en/.
- Philips. SureSigns VM8. 2008. http://www.healthcare.philips.com/.
- AdvancedIndustrialSystemsInc. Temperature vs. resistance table YSI 400 series probes. 2008. http://www.advindsys.com/ApNotes/YSI400SeriesProbesRvsT.htm.
- Sherman, L. Charge Your Battery Faster By Using an USB Port. Power Electronics Technology 2004, 34–40. [Google Scholar]
- Microchip. PICMicro Power Managed Tips'n Tricks. 2003. www.microchip.com.
- RFSolutionsLtd. Linkmatik bluetooth transceiver. 2007. www.rfsolutions.co.uk.
- Montgomery, D. C.; Runter, G. Applied statistics and probability for engineers; New York; John Wiley and Sons. D.L., 1994. [Google Scholar]
- Varela, M.; Cuesta-Frau, D.; Madrid, J.; Churruca, J.; Miro, P.; Ruiz, R.; Martinez, C. Holter monitoring of central and peripheral temperature: possible uses and feasibility study in outpatient settings. Journal of Clinical Monitoring and Computing 2009, 23, 209–216. [Google Scholar]




| Specification | Result |
|---|---|
| Inputs | 2 channels thermistor |
| Temperature range | 31 °C to 41 °C |
| Characterizations | Steinhart-Hart, YSI-400 |
| Temperature accuracy | ± 0.2 °C |
| Temperature resolution | 0.01 °C |
| Measurement interval | 1 minute |
| Data logging | Up to 10 days |
| Averaging | 60 samples/minute |
| Probe connection | Universal 2-way male connector |
| Communications | Bluetooth interface |
| Battery | 2xNiMH AA rechargeable |
| Size | 90 ×63 × 28mm |
| Weight | 250 g |
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Cuesta-Frau, D.; Varela, M.; Aboy, M.; Miró-Martínez, P. Description of a PortableWireless Device for High-Frequency Body Temperature Acquisition and Analysis. Sensors 2009, 9, 7648-7663. https://doi.org/10.3390/s91007648
Cuesta-Frau D, Varela M, Aboy M, Miró-Martínez P. Description of a PortableWireless Device for High-Frequency Body Temperature Acquisition and Analysis. Sensors. 2009; 9(10):7648-7663. https://doi.org/10.3390/s91007648
Chicago/Turabian StyleCuesta-Frau, David, Manuel Varela, Mateo Aboy, and Pau Miró-Martínez. 2009. "Description of a PortableWireless Device for High-Frequency Body Temperature Acquisition and Analysis" Sensors 9, no. 10: 7648-7663. https://doi.org/10.3390/s91007648
APA StyleCuesta-Frau, D., Varela, M., Aboy, M., & Miró-Martínez, P. (2009). Description of a PortableWireless Device for High-Frequency Body Temperature Acquisition and Analysis. Sensors, 9(10), 7648-7663. https://doi.org/10.3390/s91007648






