Impact of Anatomical Placement on the Accuracy of Wearable Heart Rate Monitors During Rest and Various Exercise Intensities
Abstract
1. Introduction
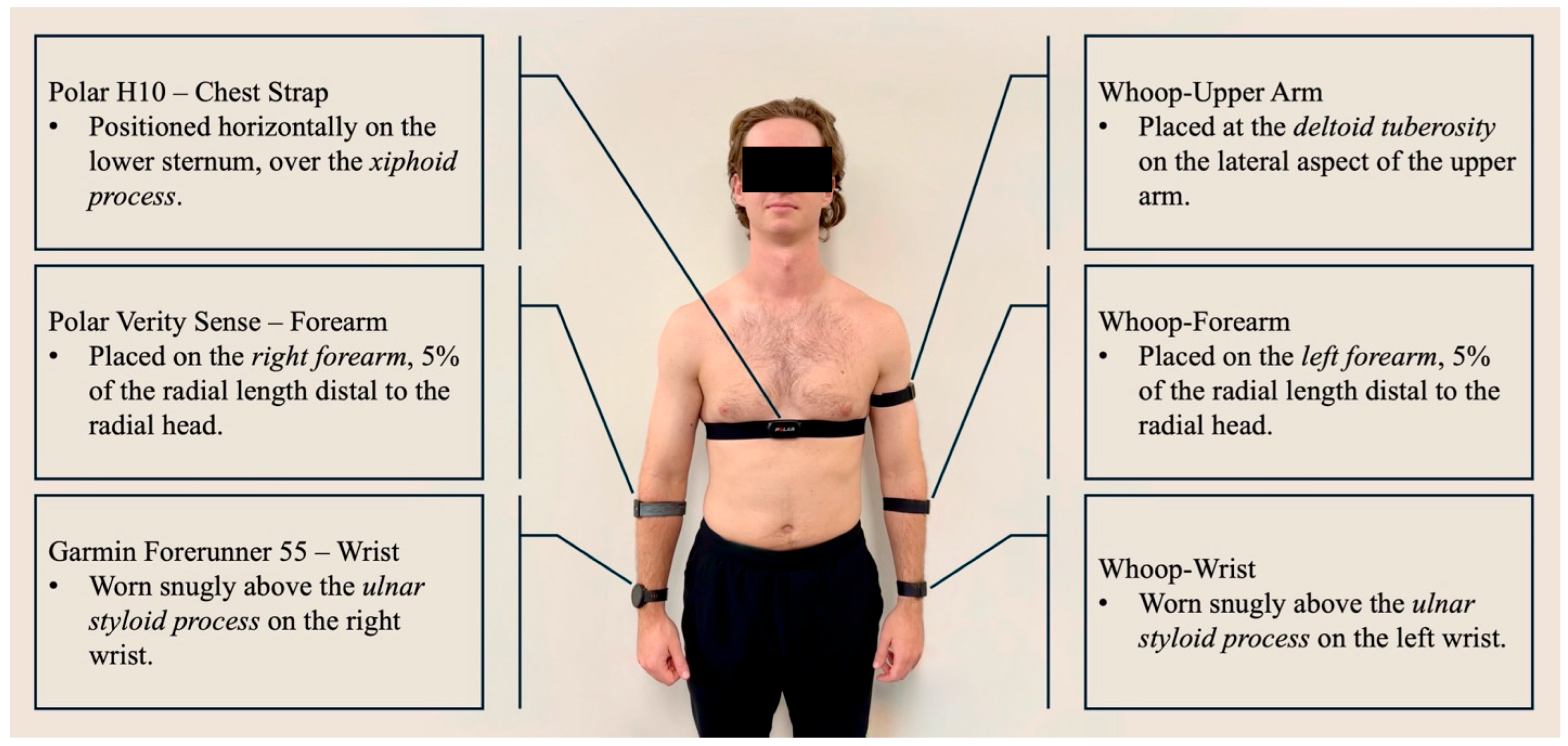
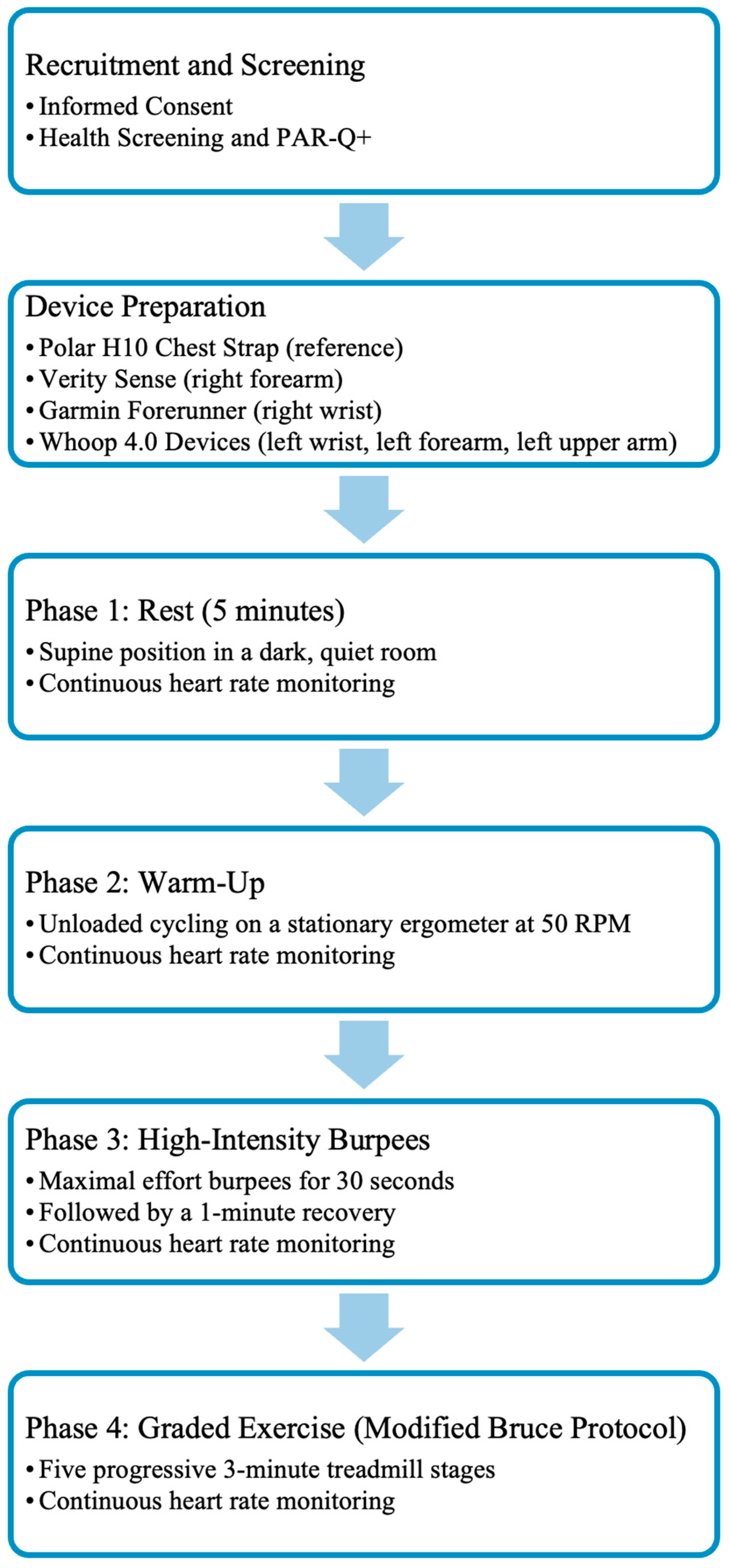
2. Methodology
2.1. Experimental Design
2.2. Participants
2.3. Statistical Analysis
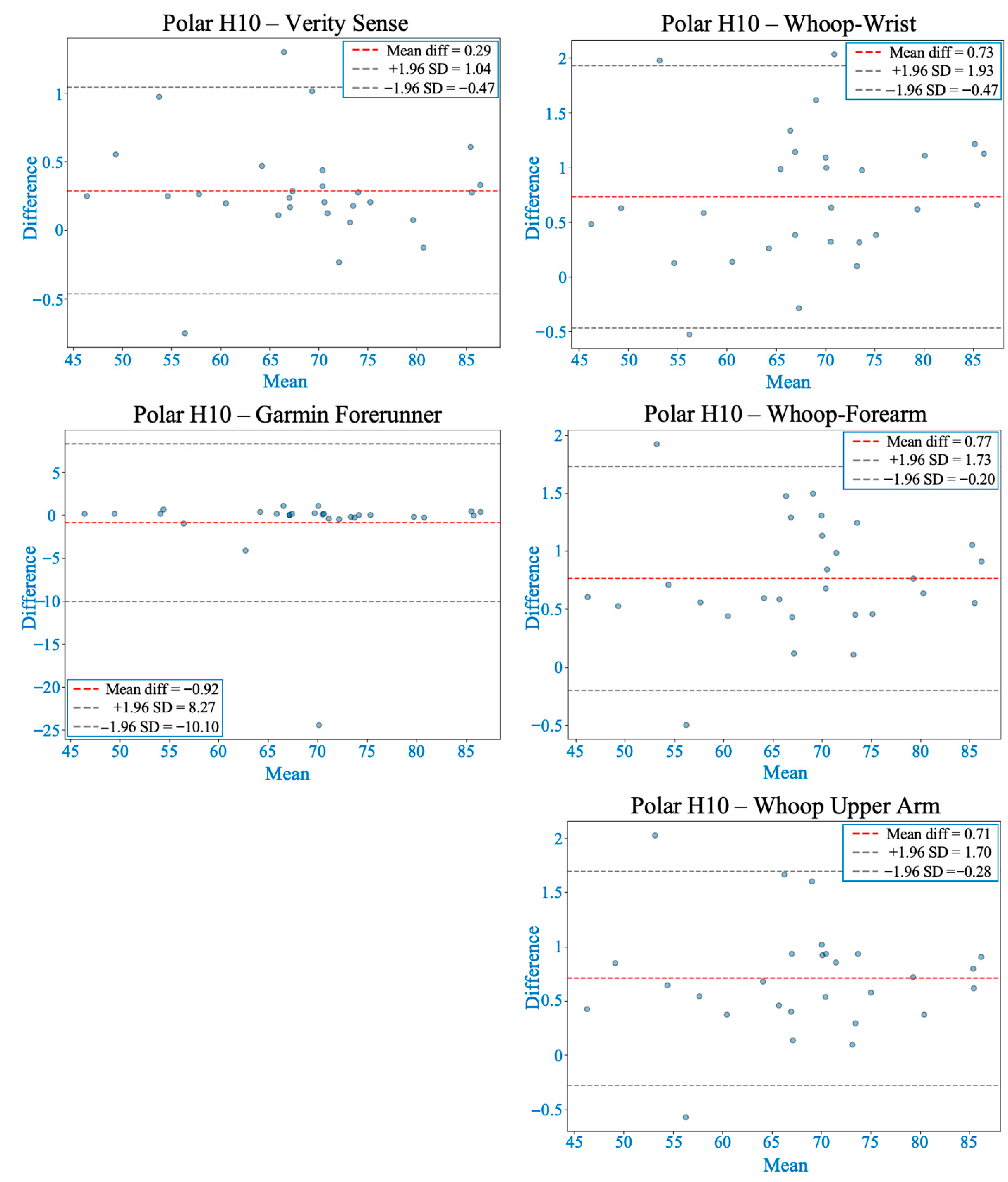
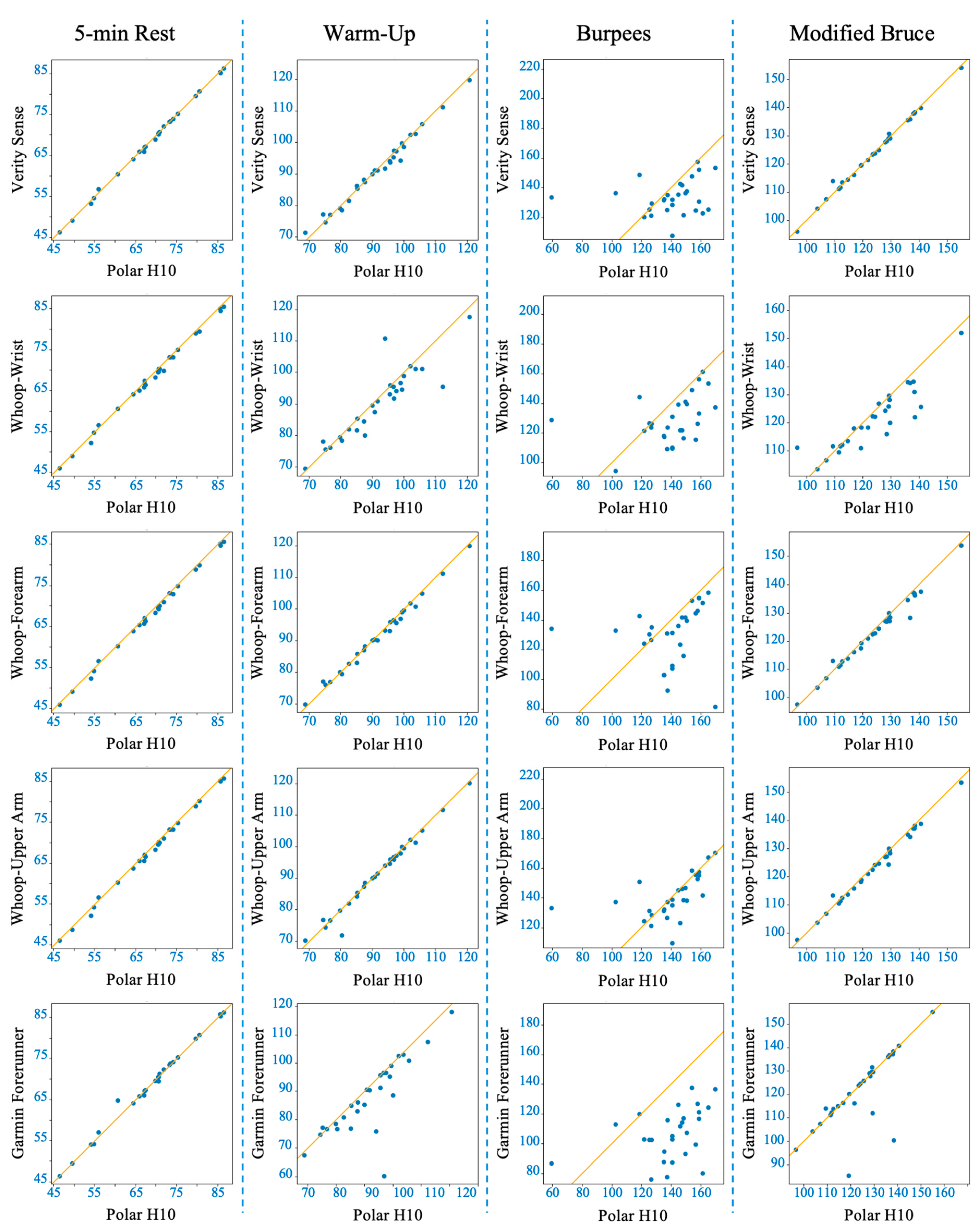
3. Results
3.1. During 5-Minute Rest
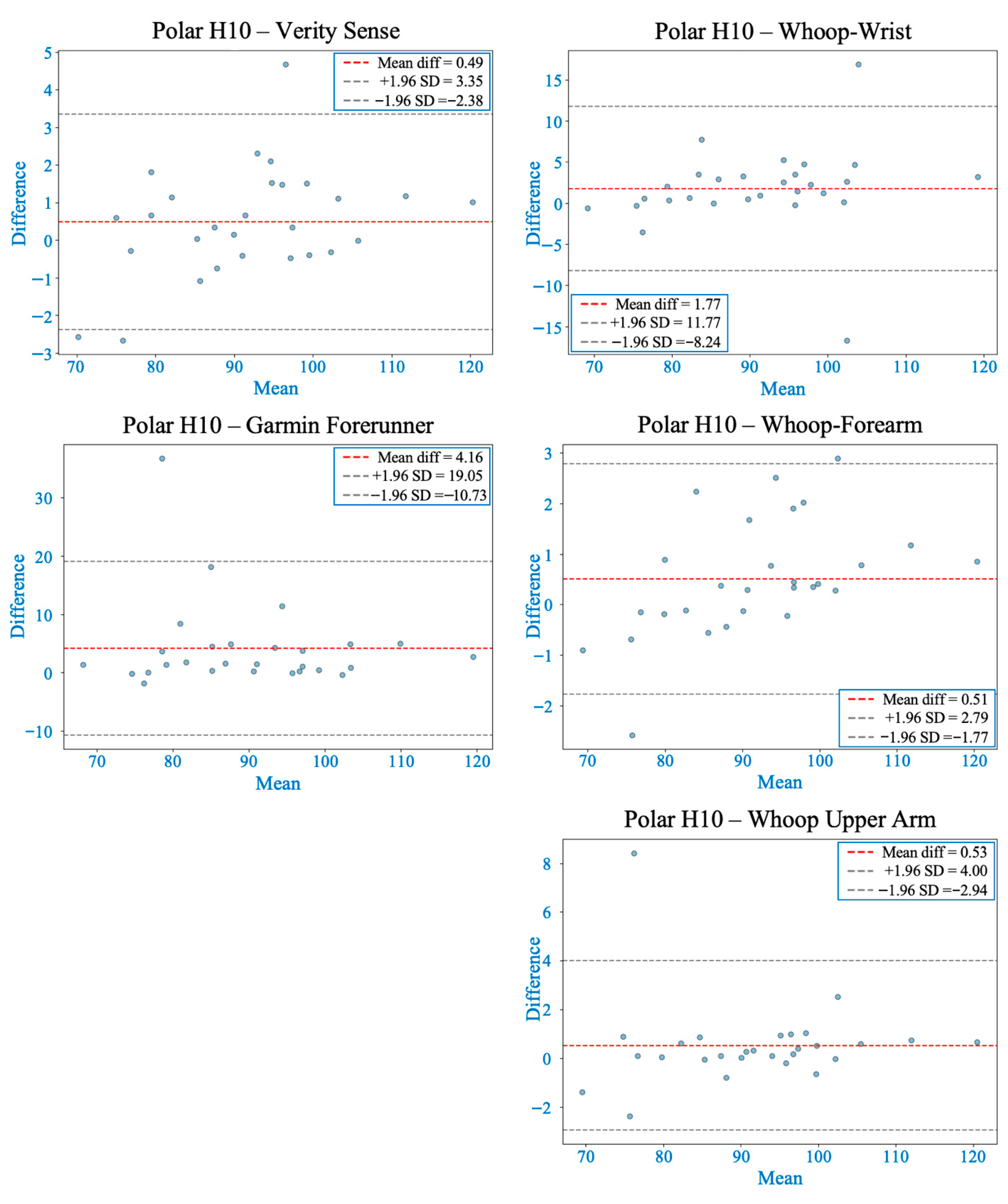
3.2. During 5-Minute Warm-Up
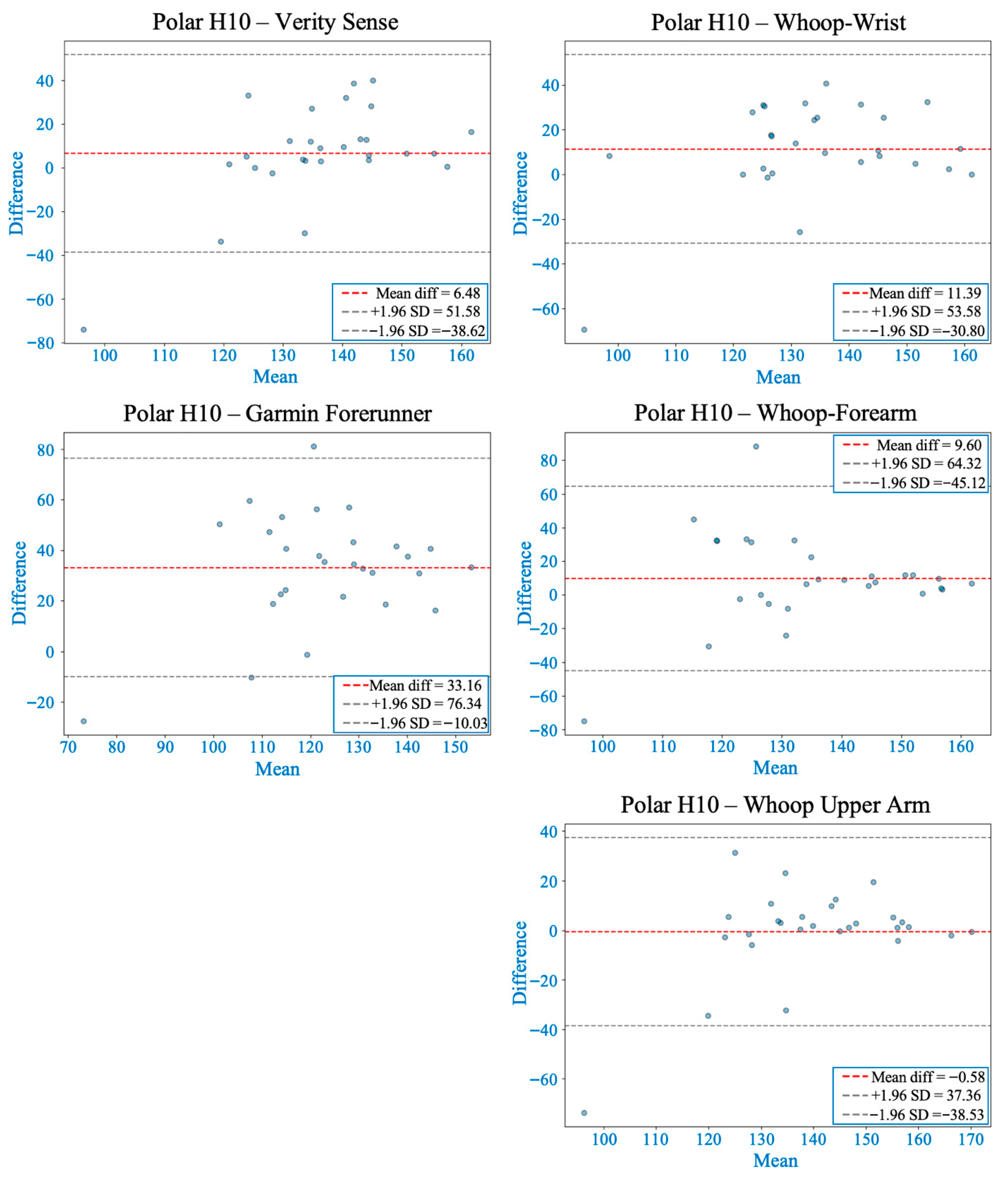
3.3. During 30-Second Burpees with 1-Minute Recovery
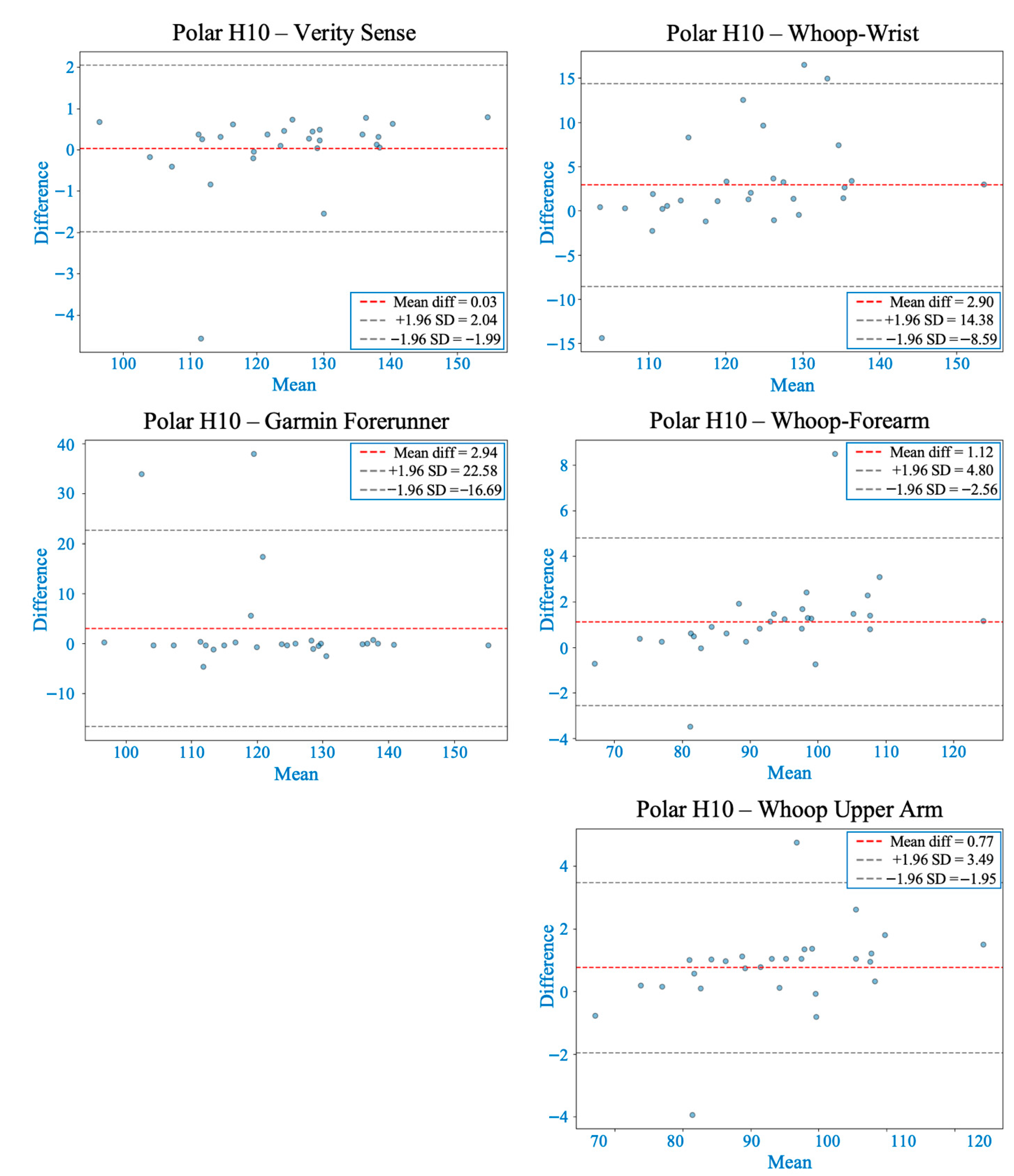
3.4. During Modified Bruce Graded Exercise Testing
4. Discussion
4.1. Accuracy Trends Across Activity Intensities
4.2. Physiological and Optical Mechanisms of Placement Differences
4.3. Inter-Device Differences: Optical Design and Signal Processing
4.4. Synthesis Across Activity Intensities
4.5. Impact of Anatomical Placement on Accuracy: Intra-Device (Whoop 4.0) Comparisons
5. Limitations
6. Practical Implications
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gajda, R.; Gajda, J.; Czuba, M.; Knechtle, B.; Drygas, W. Sports Heart Monitors as Reliable Diagnostic Tools for Training Control and Detecting Arrhythmias in Professional and Leisure-Time Endurance Athletes: An Expert Consensus Statement. Sports Med. 2024, 54, 1–21. [Google Scholar] [CrossRef]
- D’Souza, A.; Bucchi, A.; Johnsen, A.B.; Logantha, S.J.; Monfredi, O.; Yanni, J.; Prehar, S.; Hart, G.; Cartwright, E.; Wisloff, U.; et al. Exercise Training Reduces Resting Heart Rate via Downregulation of the Funny Channel HCN4. Nat. Commun. 2014, 5, 3775. [Google Scholar] [CrossRef] [PubMed]
- van der Velden, R.M.J.; Verhaert, D.V.M.; Hermans, A.N.L.; Duncker, D.; Manninger, M.; Betz, K.; Gawalko, M.; Desteghe, L.; Pisters, R.; Hemels, M.; et al. The Photoplethysmography Dictionary: Practical Guidance on Signal Interpretation and Clinical Scenarios from TeleCheck-AF. Eur. Heart J. Digit. Health 2021, 2, 363–373. [Google Scholar] [CrossRef]
- Ponikowski, P.; Spoletini, I.; Coats, A.J.S.; Piepoli, M.F.; Rosano, G.M.C. Heart Rate and Blood Pressure Monitoring in Heart Failure. Eur. Heart J. Suppl. 2019, 21, M13–M16. [Google Scholar] [CrossRef] [PubMed]
- Hori, M.; Okamoto, H. Heart Rate as a Target of Treatment of Chronic Heart Failure. J. Cardiol. 2012, 60, 86–90. [Google Scholar] [CrossRef]
- Olshansky, B.; Ricci, F.; Fedorowski, A. Importance of Resting Heart Rate. Trends Cardiovasc. Med. 2023, 33, 502–515. [Google Scholar] [CrossRef]
- Giuliano, K.K. Improving Patient Safety through the Use of Nursing Surveillance. Biomed. Instrum. Technol. 2017, 51, 34–43. [Google Scholar] [CrossRef]
- Henneman, E.A.; Gawlinski, A.; Giuliano, K.K. Surveillance: A Strategy for Improving Patient Safety in Acute and Critical Care Units. Crit. Care Nurse 2012, 32, e9–e18. [Google Scholar] [CrossRef] [PubMed]
- Xintarakou, A.; Sousonis, V.; Asvestas, D.; Vardas, P.E.; Tzeis, S. Remote Cardiac Rhythm Monitoring in the Era of Smart Wearables: Present Assets and Future Perspectives. Front. Cardiovasc. Med. 2022, 9, 853614. [Google Scholar] [CrossRef]
- Varshney, J.P. Electrocardiography: Its Uses and Limitations. In Electrocardiography in Veterinary Medicine; Springer: Singapore, 2020; pp. 25–40. ISBN 978-981-15-3698-4. [Google Scholar]
- Yang, X.L.; Liu, G.Z.; Tong, Y.H.; Yan, H.; Xu, Z.; Chen, Q.; Liu, X.; Zhang, H.H.; Wang, H.B.; Tan, S.H. The history, hotspots, and trends of electrocardiogram. J. Geriatr. Cardiol. 2015, 12, 448–456. [Google Scholar] [CrossRef]
- Vermunicht, P.; Makayed, K.; Meysman, P.; Laukens, K.; Knaepen, L.; Vervoort, Y.; De Bliek, E.; Hens, W.; Van Craenenbroeck, E.; Desteghe, L.; et al. Validation of Polar H10 chest strap and Fitbit Inspire 2 tracker for measuring continuous heart rate in cardiac patients: Impact of artefact removal algorithm. Europace 2023, 25, euad122.550. [Google Scholar] [CrossRef]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195–202. [Google Scholar] [CrossRef]
- Tamura, T.; Maeda, Y.; Sekine, M.; Yoshida, M. Wearable Photoplethysmographic Sensors—Past and Present. Electronics 2014, 3, 282–302. [Google Scholar] [CrossRef]
- Gilgen-Ammann, R.; Schweizer, T.; Wyss, T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur. J. Appl. Physiol. 2019, 119, 1525–1532. [Google Scholar] [CrossRef]
- Schaffarczyk, M.; Rogers, B.; Reer, R.; Gronwald, T. Validity of the Polar H10 Sensor for Heart Rate Variability Analysis during Resting State and Incremental Exercise in Recreational Men and Women. Sensors 2022, 22, 6536. [Google Scholar] [CrossRef]
- Li, X.; Song, Y.; Wang, H.; Su, X.; Wang, M.; Li, J.; Ren, Z.; Zhong, D.; Huang, Z. Evaluation of Measurement Accuracy of Wearable Devices for Heart Rate Variability. iScience 2023, 26, 108128. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, Z.; Wei, X. Monitoring Heart and Respiratory Rates at Radial Artery Based on PPG. Optik 2013, 124, 3954–3956. [Google Scholar] [CrossRef]
- Kavsaoğlu, A.R.; Polat, K.; Hariharan, M. Non-Invasive Prediction of Hemoglobin Level Using Machine Learning Techniques with the PPG Signal’s Characteristic Features. Appl. Soft Comput. 2015, 37, 983–991. [Google Scholar] [CrossRef]
- Rhee, S.; Yang, B.H.; Asada, H.H. Artifact-Resistant Power-Efficient Design of Finger-Ring Plethysmographic Sensors. IEEE Trans. Biomed. Eng. 2001, 48, 795–805. [Google Scholar] [CrossRef]
- Nardelli, M.; Vanello, N.; Galperti, G.; Greco, A.; Scilingo, E.P. Assessing the Quality of Heart Rate Variability Estimated from Wrist and Finger PPG: A Novel Approach Based on Cross-Mapping Method. Sensors 2020, 20, 3156. [Google Scholar] [CrossRef]
- Yokoyama, K.; Hayashi, E.; Ito, H.; Kawahara, Y. Estimation of Heart Rate Variability from Heart Rate Measured with Wristwatch-Type Heart Rate Monitor. Electron. Commun. Jpn. 2022, 105, e12351. [Google Scholar] [CrossRef]
- Adams, T.; Wagner, S.; Baldinger, M.; Zellhuber, I.; Weber, M.; Nass, D.; Surges, R. Accurate Detection of Heart Rate Using In-Ear Photoplethysmography in a Clinical Setting. Front. Digit. Health 2022, 4, 909519. [Google Scholar] [CrossRef]
- Ferlini, A.; Montanari, A.; Min, C.; Li, H.; Sassi, U.; Kawsar, F. In-Ear PPG for Vital Signs. IEEE Pervasive Comput. 2022, 21, 65–74. [Google Scholar] [CrossRef]
- Sim, J.K.; Ahn, B.; Doh, I. A Contact-Force Regulated Photoplethysmography (PPG) Platform. AIP Adv. 2018, 8, 045210. [Google Scholar] [CrossRef]
- Hsiu, H.; Hsu, C.L.; Wu, T.L. Effects of Different Contacting Pressure on the Transfer Function between Finger Photoplethysmographic and Radial Blood Pressure Waveforms. Proc. Inst. Mech. Eng. H 2011, 225, 575–583. [Google Scholar] [CrossRef]
- Grabovskis, A.; Marcinkevics, Z.; Rubins, U.; Kviesis-Kipge, E. Effect of Probe Contact Pressure on the Photoplethysmographic Assessment of Conduit Artery Stiffness. J. Biomed. Opt. 2013, 18, 027004. [Google Scholar] [CrossRef]
- Scardulla, F.; D’Acquisto, L.; Colombarini, R.; Hu, S.; Pasta, S.; Bellavia, D. A Study on the Effect of Contact Pressure during Physical Activity on Photoplethysmographic Heart Rate Measurements. Sensors 2020, 20, 5052. [Google Scholar] [CrossRef]
- Giavarina, D. Understanding Bland Altman Analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Ludbrook, J. Linear Regression Analysis for Comparing Two Measurers or Methods of Measurement: But Which Regression? Clin. Exp. Pharmacol. Physiol. 2010, 37, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Sekine, M.; Tamura, T. Relationship between Measurement Site and Motion Artifacts in Wearable Reflected Photoplethysmography. J. Med. Syst. 2011, 35, 969–976. [Google Scholar] [CrossRef]
- Allen, J. Photoplethysmography and Its Application in Clinical Physiological Measurement. Physiol. Meas. 2007, 28, R1–R39. [Google Scholar] [CrossRef]
- Khong, W.L.; Mariappan, M.; Chong, C.S. Contact and Non-Contact Heart Beat Rate Measurement Techniques: Challenges and Issues. Pertanika J. Sci. Technol. 2021, 29, 1707–1732. [Google Scholar] [CrossRef]
- Elgendi, M. On the Analysis of Fingertip Photoplethysmogram Signals. Curr. Cardiol. Rev. 2012, 8, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Secomb, T.W. Hemodynamics. Compr. Physiol. 2016, 6, 975–1003. [Google Scholar] [CrossRef]
- Charlton, P.H.; Marozas, V.; Mejía-Mejía, E.; Kyriacou, P.A.; Mant, J. Determinants of photoplethysmography signal quality at the wrist. PLoS Digit. Health 2025, 4, e0000585. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Seok, H.S.; Kim, S.S.; Shin, H. Photoplethysmogram Analysis and Applications: An Integrative Review. Front. Physiol. 2022, 12, 808451. [Google Scholar] [CrossRef]
- Wang, Z.; Cheng, S.; Fukuda, K.; Hu, W.; Xu, X.; Someya, T. Flexible Near-Infrared Organic Photodetectors for Emergent Wearable Applications. Wearable Electron. 2024, 1, 53–77. [Google Scholar] [CrossRef]
- Liu, J.; Yan, B.P.; Dai, W.X.; Ding, X.R.; Zhang, Y.T.; Zhao, N. Multi-Wavelength Photoplethysmography Method for Skin Arterial Pulse Extraction. Biomed. Opt. Express 2016, 7, 4313–4326. [Google Scholar] [CrossRef]
- Lee, J.; Kim, M.; Park, H.K.; Kim, I.Y. Motion Artifact Reduction in Wearable Photoplethysmography Based on Multi-Channel Sensors with Multiple Wavelengths. Sensors 2020, 20, 1493. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Pi, Z.; Liu, B. TROIKA: A General Framework for Heart Rate Monitoring Using Wrist-Type Photoplethysmographic Signals during Intensive Physical Exercise. IEEE Trans. Biomed. Eng. 2015, 62, 522–531. [Google Scholar] [CrossRef]
- Fine, J.; Branan, K.L.; Rodriguez, A.J.; Boonya-Ananta, T.; Ajmal; Ramella-Roman, J.C.; McShane, M.J.; Coté, G.L. Sources of Inaccuracy in Photoplethysmography for Continuous Cardiovascular Monitoring. Biosensors 2021, 11, 126. [Google Scholar] [CrossRef] [PubMed]
| Age (years) | 23.75 ± 1.11 |
| Height (cm) | 171.50 ± 8.00 |
| Weight (kg) | 71.74 ± 8.92 |
| Body Mass Index (kg/m2) | 24.36 ± 2.44 |
| Body Fat Percentage (%) | 21.99 ± 6.79 |
| Device | Rest | Warm-Up | Burpees | Modified Bruce |
|---|---|---|---|---|
| Verity Sense | 1.57 ± 0.77% | 3.87 ± 1.92% | 16.32 ± 23.65% | 1.89 ± 1.21% |
| Garmin Forerunner | 2.11 ± 1.49% | 6.88 ± 6.95% | 25.48 ± 11.18% | 4.29 ± 6.76% |
| Whoop-upper arm | 2.50 ± 0.87% | 2.91 ± 2.21% | 12.07 ± 24.26% | 1.92 ± 1.15% |
| Whoop-forearm | 2.81 ± 0.87% | 3.51 ± 1.96% | 17.75 ± 24.87% | 2.55 ± 3.28% |
| Whoop-wrist | 2.93 ± 1.02% | 5.59 ± 4.57% | 17.23 ± 21.51% | 5.95 ± 5.03% |
| Activity | Device | Mean Bias (bpm) | 95% Limits of Agreement (LOA, bpm) | Proportional Bias | Systematic Bias |
|---|---|---|---|---|---|
| Rest | Verity Sense | 0.29 | −0.47 to 1.04 | No | No |
| Garmin Forerunner | −0.92 | −10.10 to 8.27 | No | No | |
| Whoop-upper arm | 0.71 | −0.28 to 1.70 | No | No | |
| Whoop-forearm | 0.77 | −0.20 to 1.73 | No | No | |
| Whoop-wrist | 0.73 | −0.47 to 1.93 | No | No | |
| Warm-Up | Verity Sense | 0.49 | −2.38 to 3.35 | No | No |
| Garmin Forerunner | 4.16 | −10.73 to 19.05 | No | No | |
| Whoop-upper arm | 0.53 | −2.94 to 4.00 | No | No | |
| Whoop-forearm | 0.51 | −1.77 to 2.79 | Yes | Yes | |
| Whoop-wrist | 1.77 | −8.23 to 11.77 | No | No | |
| Burpees | Verity Sense | 6.48 | −38.62 to 51.58 | Yes | Yes |
| Garmin Forerunner | 33.16 | −10.03 to 76.34 | No | No | |
| Whoop-upper arm | −0.58 | −38.53 to 37.36 | Yes | Yes | |
| Whoop-forearm | 9.60 | −45.12 to 64.32 | No | No | |
| Whoop-wrist | 11.39 | −30.80 to 53.58 | No | No | |
| Modified Bruce Protocol | Verity Sense | 0.03 | −1.99 to 2.04 | No | No |
| Garmin Forerunner | 2.94 | −16.69 to 22.57 | No | No | |
| Whoop-upper arm | 0.77 | −1.95 to 3.49 | Yes | No | |
| Whoop-forearm | 1.12 | −2.56 to 4.80 | Yes | Yes | |
| Whoop-wrist | 2.90 | −8.59 to 14.38 | Yes | Yes |
| Device | Rest | Warm-Up | Burpees | Modified Bruce |
|---|---|---|---|---|
| Verity Sense | 0.9990 | 0.9912 | 0.1343 | 0.9968 |
| Garmin Forerunner | 0.9961 | 0.7677 | 0.1521 | 0.7323 |
| Whoop-upper arm | 0.9964 | 0.9879 | 0.4605 | 0.9922 |
| Whoop-forearm | 0.9960 | 0.9940 | 0.1021 | 0.1021 |
| Whoop-wrist | 0.9956 | 0.8910 | 0.3100 | 0.8514 |
| Activity | Device | Slope (95% CI) | Intercept (95% CI) | Proportional Bias | Systematic Bias |
|---|---|---|---|---|---|
| Rest | Verity Sense | 1.0026 (0.988–1.017) | −0.46 (−1.45–0.52) | No | No |
| Garmin Forerunner | 0.9940 (0.960–1.028) | 0.46 (−1.93–2.85) | No | No | |
| Whoop-upper arm | 0.9999 (0.981–1.019) | −0.71 (−2.04–0.62) | No | No | |
| Whoop-forearm | 0.9957 (0.977–1.014) | −0.47 (−1.78–0.83) | No | No | |
| Whoop-wrist | 0.9881 (0.965–1.011) | 0.09 (−1.50–1.68) | No | No | |
| Warm-Up | Verity Sense | 0.9542 (0.911–0.997) | 3.73 (−0.25–7.71) | Yes | No |
| Garmin Forerunner | 1.1054 (0.834–1.377) | −13.86 (−31.9–4.1) | No | No | |
| Whoop-upper arm | 1.0008 (0.943–1.059) | −0.60 (−6.0–4.8) | No | No | |
| Whoop-forearm | 0.9507 (0.919–0.982) | 4.03 (1.10–6.96) | Yes | Yes | |
| Whoop-wrist | 0.9311 (0.769–1.093) | 4.57 (−10.3–19.4) | No | No | |
| Burpees | Verity Sense | 0.1230 (−0.08–0.33) | 116.19 (89.0–143.4) | No | Yes |
| Garmin Forerunner | 0.5303 (0.23–0.83) | 32.55 (−9.9–75.0) | Yes | No | |
| Whoop-upper arm | 0.4546 (0.23–0.68) | 76.87 (44.5–109.3) | Yes | Yes | |
| Whoop-forearm | 0.4259 (0.04–0.81) | 70.71 (14.7–126.7) | Yes | Yes | |
| Whoop-wrist | 0.4446 (0.17–0.72) | 66.30 (28.3–104.3) | Yes | Yes | |
| Modified Bruce Protocol | Verity Sense | 0.9787 (0.950–1.008) | 2.62 (−1.0–6.2) | No | No |
| Garmin Forerunner | 0.7936 (0.65–0.94) | 22.73 (4.8–40.7) | Yes | Yes | |
| Whoop-upper arm | 0.9568 (0.92–0.99) | 4.60 (−0.0–9.2) | Yes | No | |
| Whoop-forearm | 0.9358 (0.89–0.98) | 6.86 (0.9–12.8) | Yes | Yes | |
| Whoop-wrist | 0.7936 (0.65–0.94) | 22.73 (4.8–40.7) | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Moghaddam, M.; Collins, J.P.; Gardner, C.E.; Rabel, M.C. Impact of Anatomical Placement on the Accuracy of Wearable Heart Rate Monitors During Rest and Various Exercise Intensities. Sensors 2026, 26, 176. https://doi.org/10.3390/s26010176
Moghaddam M, Collins JP, Gardner CE, Rabel MC. Impact of Anatomical Placement on the Accuracy of Wearable Heart Rate Monitors During Rest and Various Exercise Intensities. Sensors. 2026; 26(1):176. https://doi.org/10.3390/s26010176
Chicago/Turabian StyleMoghaddam, Masoud, James P. Collins, Caroline E. Gardner, and Michael C. Rabel. 2026. "Impact of Anatomical Placement on the Accuracy of Wearable Heart Rate Monitors During Rest and Various Exercise Intensities" Sensors 26, no. 1: 176. https://doi.org/10.3390/s26010176
APA StyleMoghaddam, M., Collins, J. P., Gardner, C. E., & Rabel, M. C. (2026). Impact of Anatomical Placement on the Accuracy of Wearable Heart Rate Monitors During Rest and Various Exercise Intensities. Sensors, 26(1), 176. https://doi.org/10.3390/s26010176







