Comparison of Cervical Spine Kinematics and Clinical Neck Symptoms Between Mobile Device and Desktop Computer Use
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
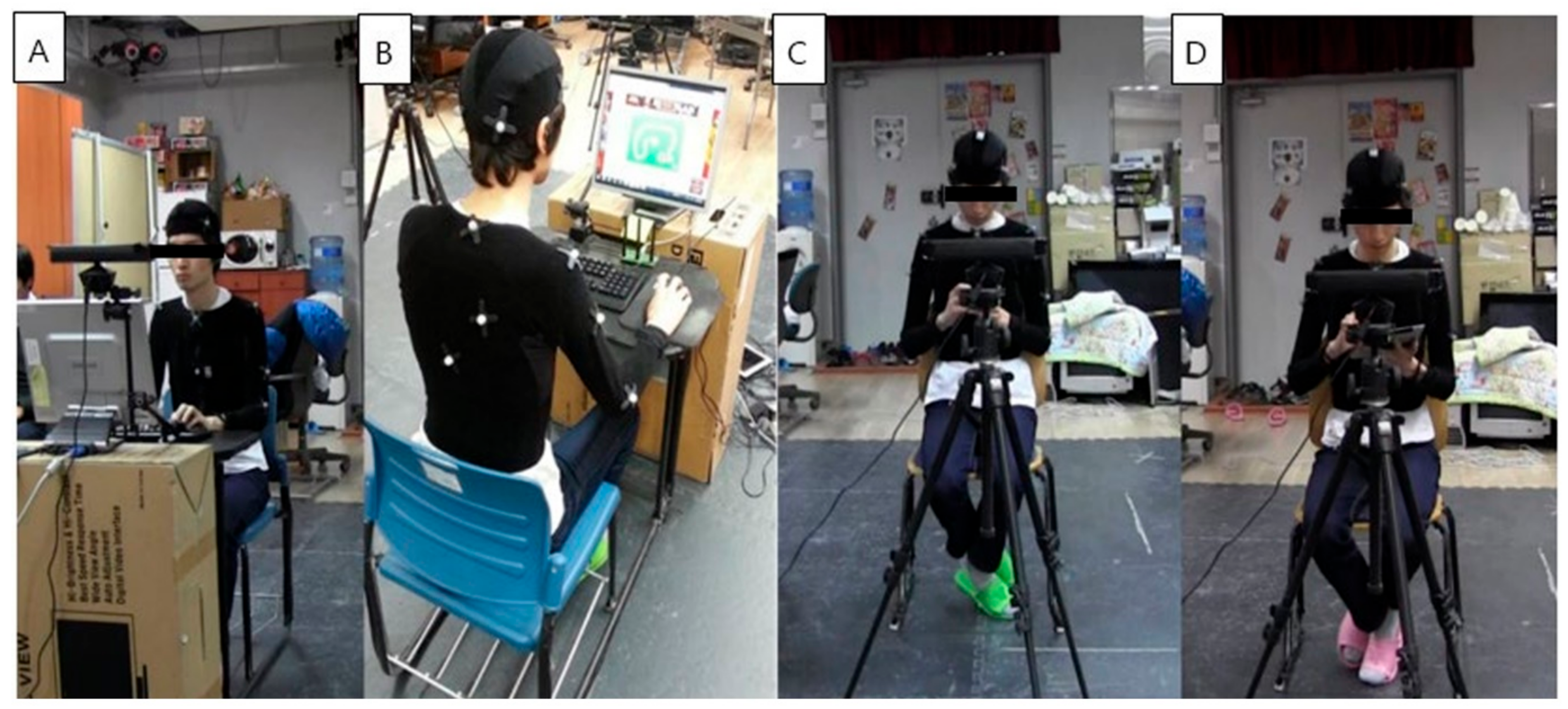
2.2. Experimental Protocols
2.3. Kinematic Analysis
2.3.1. Optical Motion Capture System
2.3.2. Data Analysis
2.3.3. Kinematic Variables
2.4. Clinical Variables
2.5. Statistical Analysis
3. Results
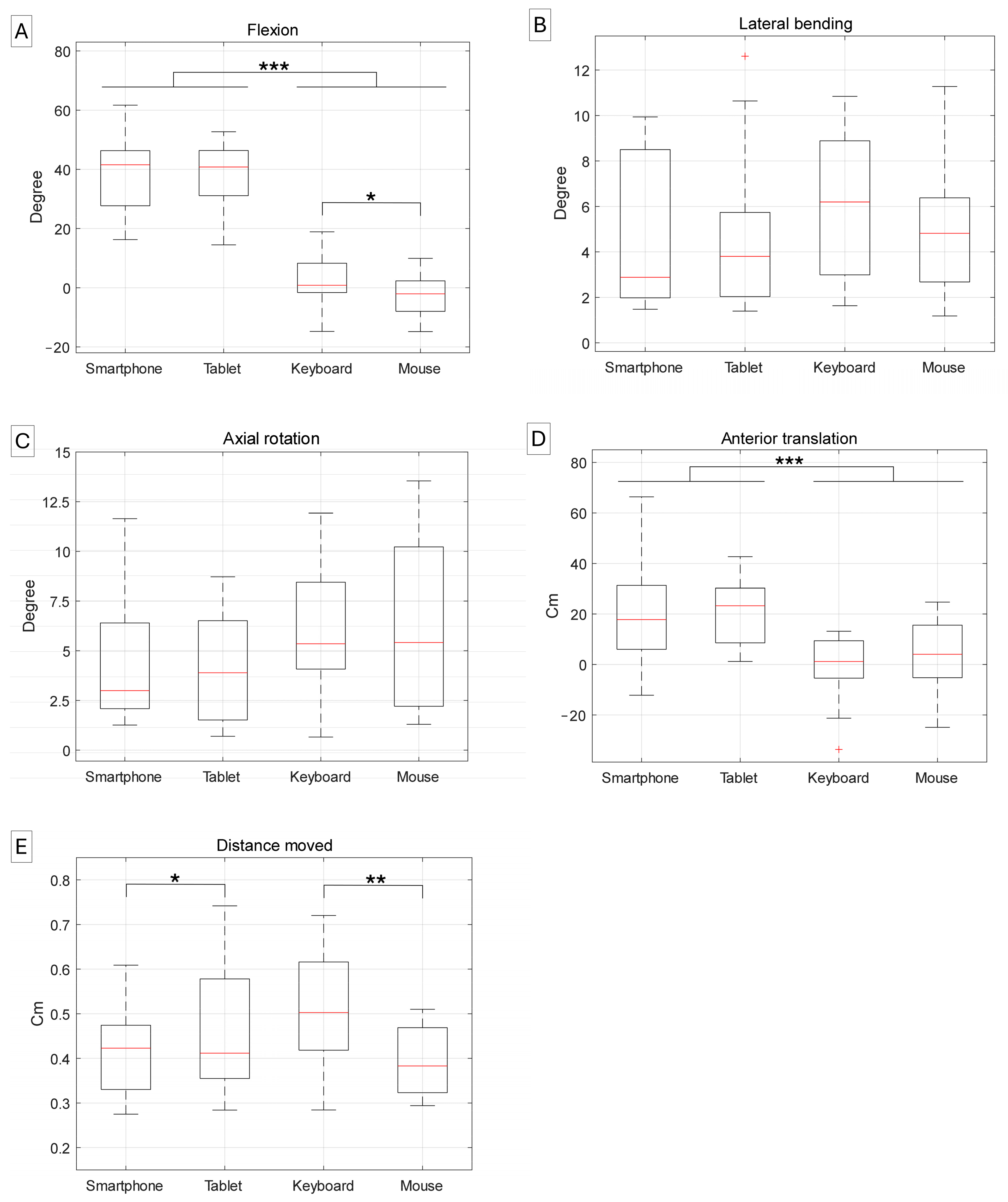
3.1. Kinematic Variables According to Task Type
3.2. Differences in Clinical Variables by Task Type
3.3. Differences in Clinical Variables by Kinematics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bergqvist, U.; Wolgast, E.; Nilsson, B.; Voss, M. Musculoskeletal disorders among visual display terminal workers: Individual, ergonomic, and work organizational factors. Ergonomics 1995, 38, 763–776. [Google Scholar] [CrossRef] [PubMed]
- Wærsted, M.; Hanvold, T.N.; Veiersted, K.B. Computer work and musculoskeletal disorders of the neck and upper extremity: A systematic review. BMC Musculoskelet. Disord. 2010, 11, 79. [Google Scholar] [CrossRef] [PubMed]
- Aaras, A.; Fostervold, K.I.; Ro, O.L.A.; Thoresen, M.; Larsen, S. Postural load during VDU work: A comparison between various work postures. Ergonomics 1997, 40, 1255–1268. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.B.; Banister, E.W. Musculoskeletal problems in VDT work: A review. Ergonomics 1994, 37, 1623–1648. [Google Scholar] [CrossRef]
- James, C.P.; Harburn, K.L.; Kramer, J.F. Cumulative trauma disorders in the upper extremities: Reliability of the postural and repetitive risk-factors index. Arch. Phys. Med. Rehabil. 1997, 78, 860–866. [Google Scholar] [CrossRef]
- Straker, L.; Jones, K.J.; Miller, J. A comparison of the postures assumed when using laptop computers and desktop computers. Appl. Ergon. 1997, 28, 263–268. [Google Scholar] [CrossRef]
- Yu, Z.; James, C.; Edwards, S.; Snodgrass, S.J. Differences in posture kinematics between using a tablet, a laptop, and a desktop computer in sitting and in standing. Work 2018, 61, 257–266. [Google Scholar] [CrossRef]
- Lee, R.; James, C.; Edwards, S.; Snodgrass, S.J. Differences in upper body posture between individuals with and without chronic idiopathic neck pain during computerised device use: A 3D motion analysis study. Gait Posture 2022, 95, 30–37. [Google Scholar] [CrossRef]
- Eltayeb, S.; Staal, J.B.; Kennes, J.; Lamberts, P.H.; de Bie, R.A. Prevalence of complaints of arm, neck and shoulder among computer office workers and psychometric evaluation of a risk factor questionnaire. BMC Musculoskelet. Disord. 2007, 8, 68. [Google Scholar] [CrossRef]
- Johnston, V.; Souvlis, T.; Jimmieson, N.L.; Jull, G. Associations between individual and workplace risk factors for self-reported neck pain and disability among female office workers. Appl. Ergon. 2008, 39, 171–182. [Google Scholar] [CrossRef]
- Global Smartphone User Penetration Forecast by 88 Countries: 2007 to 2028. Available online: https://www.techinsights.com/ko/node/54486 (accessed on 30 October 2024).
- Sarraf, F.; Varmazyar, S. Comparing the effect of the posture of using smartphones on head and neck angles among college students. Ergonomics 2022, 65, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Hansraj, K.K. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg. Technol. Int. 2014, 25, 277–279. [Google Scholar] [PubMed]
- Lee, S.; Kang, H.; Shin, G. Head flexion angle while using a smartphone. Ergonomics 2015, 58, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Kietrys, D.M.; Gerg, M.J.; Dropkin, J.; Gold, J.E. Mobile input device type, texting style and screen size influence upper extremity and trapezius muscle activity, and cervical posture while texting. Appl. Ergon. 2015, 50, 98–104. [Google Scholar] [CrossRef]
- Xie, Y.F.; Szeto, G.; Madeleine, P.; Tsang, S. Spinal kinematics during smartphone texting—A comparison between young adults with and without chronic neck-shoulder pain. Appl. Ergon. 2018, 68, 160–168. [Google Scholar] [CrossRef]
- Berolo, S.; Wells, R.P.; Amick, B.C., III. Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: A preliminary study in a Canadian university population. Appl. Ergon. 2011, 42, 371–378. [Google Scholar] [CrossRef]
- AlAbdulwahab, S.S.; Kachanathu, S.J.; AlMotairi, M.S. Smartphone use addiction can cause neck disability. Musculoskelet. Care 2017, 15, 1–3. [Google Scholar] [CrossRef]
- Almhdawi, K.A.; Mathiowetz, V.; Al-Hourani, Z.; Khader, Y.; Kanaan, S.F.; Alhasan, M. Musculoskeletal pain symptoms among allied health professions’ students: Prevalence rates and associated factors. J. Back Musculoskelet. Rehabil. 2017, 30, 1291–1301. [Google Scholar] [CrossRef]
- Zhuang, L.; Wang, L.; Xu, D.; Wang, Z.; Liang, R. Association between excessive smartphone use and cervical disc degeneration in young patients suffering from chronic neck pain. J. Orthop. Sci. 2021, 26, 110–115. [Google Scholar] [CrossRef]
- Khan, M.R.; Ambati, T. Musculoskeletal pain symptoms in users performing smartphone texting: A preliminary study on institute environment. Int. J. Ind. Ergon. 2022, 90, 103325. [Google Scholar] [CrossRef]
- Sahu, M.; Gnana Sundari, K.; David, A. Recent Ergonomic Interventions and Evaluations on Laptop, Smartphones and Desktop Computer Users. In Advances in Industrial Automation and Smart Manufacturing: Select Proceedings of ICAIASM 2019, Proceedings of the International Conference on Advances in Industrial Automation and Smart Manufacturing (ICAIASM) 2019, Nandyal, India, 26–27 July 2019; Springer: Berlin/Heidelberg, Germany, 2021; pp. 207–224. [Google Scholar]
- Sengupta, A.; Grabiner, S.; Kothari, P.; Martinez, G. Ergonomic Aspects of Personal Digital Assistant (PDA) and Laptop Use. In Proceedings of the 6th International Scientific Conference on Prevention of Work-Related Musculoskeletal Disorders, PREMUS, Boston, MA, USA, 27–30 August 2007. [Google Scholar]
- Douglas, E.C.; Gallagher, K.M. The influence of a semi-reclined seated posture on head and neck kinematics and muscle activity while reading a tablet computer. Appl. Ergon. 2017, 60, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Young, J.G.; Trudeau, M.; Odell, D.; Marinelli, K.; Dennerlein, J.T. Touch-screen tablet user configurations and case-supported tilt affect head and neck flexion angles. Work 2012, 41, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Guzman, J.; Haldeman, S.; Carroll, L.J.; Carragee, E.J.; Hurwitz, E.L.; Peloso, P.; Nordin, M.; Cassidy, J.D.; Holm, L.W.; Côté, P. Clinical practice implications of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Eur. Spine J. 2008, 17, 199–213. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Walton, D.M.; Bobos, P.; Lomotan, M.; Carlesso, L. A qualitative description of chronic neck pain has implications for outcome assessment and classification. Open J. Orthop. 2016, 10, 746. [Google Scholar] [CrossRef]
- Plug-In Gait Reference Guide—Vicon Documentation. Available online: https://help.vicon.com/download/attachments/11378719/Plug-in%20Gait%20Reference%20Guide.pdf (accessed on 30 October 2024).
- Straker, L.; Skoss, R.; Burnett, A.; Burgess-Limerick, R. Effect of visual display height on modelled upper and lower cervical gravitational moment, muscle capacity and relative strain. Ergonomics 2009, 52, 204–221. [Google Scholar] [CrossRef]
- Xie, Y.; Szeto, G.P.; Dai, J.; Madeleine, P. A comparison of muscle activity in using touchscreen smartphone among young people with and without chronic neck–shoulder pain. Ergonomics 2016, 59, 61–72. [Google Scholar] [CrossRef]
- Bland, J.H.; Boushey, D.R. Anatomy and physiology of the cervical spine. In Seminars in Arthritis and Rheumatism; WB Saunders: Philadelphia, PA, USA, 1990; Volume 20, pp. 1–20. [Google Scholar]
- Tang, Z.; Jin, X.; Wu, Y.; Ma, J.; Xia, D.; Dong, Y.; Yang, C. Ergonomic evaluation of the effects of forearm conditions and body postures on trapezius muscle activity during smartphone texting. Int. J. Ind. Ergon. 2021, 82, 103085. [Google Scholar] [CrossRef]
- Mousavi-Khatir, R.; Talebian, S.; Toosizadeh, N.; Olyaei, G.R.; Maroufi, N. The effect of static neck flexion on mechanical and neuromuscular behaviors of the cervical spine. J. Biomech. 2018, 72, 152–158. [Google Scholar] [CrossRef]
- Szeto, G.P.Y.; Straker, L.M.; O’Sullivan, P.B. EMG median frequency changes in the neck–shoulder stabilizers of symptomatic office workers when challenged by different physical stressors. J. Electromyogr. Kinesiol. 2005, 15, 544–555. [Google Scholar] [CrossRef]
- Evans, G. Identifying and treating the causes of neck pain. Med. Clin. N. Am. 2014, 98, 645–661. [Google Scholar] [CrossRef]
- Nakphet, N.; Chaikumarn, M.; Janwantanakul, P. Effect of different types of rest-break interventions on neck and shoulder muscle activity, perceived discomfort and productivity in symptomatic VDU operators: A randomized controlled trial. Int. J. Occup. Saf. Ergon. 2014, 20, 339–353. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Park, S.M.; Kim, S.Y.; Hyeong, J.H.; Roh, J.R. Changes in Biomechanical Factors Depending on Smartphone Usage Configurations. J. Ergon. Soc. Korea. 2024, 43, 365–378. [Google Scholar] [CrossRef]
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef] [PubMed]
- March, L.M.; Brnabic, A.J.; Skinner, J.C.; Schwarz, J.M.; Finnegan, T.; Druce, J.; Brooks, P.M. Musculoskeletal disability among elderly people in the community. Med. J. Aust. 1998, 168, 439–442. [Google Scholar] [CrossRef][Green Version]
- Joch, M.; Döhring, F.R.; Maurer, L.K.; Müller, H. Inference statistical analysis of continuous data based on confidence bands—Traditional and new approaches. Behav. Res. Methods 2019, 51, 1244–1257. [Google Scholar] [CrossRef]

| Mobile Device | Desktop Computer | ||||||
|---|---|---|---|---|---|---|---|
| Smartphone | Tablet | Total | Keyboard | Mouse | Total | p-Value | |
| Discomfort | 40.0 (29.8,50.1) | 36.5 (26.3,46.7) | 39.1 (30.4–47.8) | 30.7 (20.3,41.0) a | 37.0 (26.6,47.3) a | 33.0 (24.3–41.7) | 0.036 * |
| Pain | 37.4 (25.5,49.3) | 36.3 (24.4,48.2) | 37.5 (29.3–45.6) | 24.7 (15.2,34.2) | 27.2 (17.7,36.7) | 25.3 (17.2–33.5) | 0.002 * |
| Tension | 49.6 (37.4,61.7) | 45.0 (32.8,57.2) | 47.6 (38.3–57.0) | 35.3 (25.6,45.0) | 38.2 (28.4,47.8) | 36.3 (27.0–45.6) | <0.001 * |
| Fatigue | 47.8 (37.2,58.4) | 51.4 (40.8,62.0) | 49.6 (40.4–58.8) | 33.9 (22.1,45.6) a | 42.8 (31.1,54.5) a | 38.3 (29.2–47.5) | 0.005 * |
| Discomfort | Pain | Tension | Fatigue | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ß | SE | p-Value | ß | SE | p-Value | ß | SE | p-Value | ß | SE | p-Value | |
| Flexion | 0.146 | 0.065 | 0.031 * | 0.224 | 0.092 | 0.019 * | 0.209 | 0.077 | 0.010 * | 0.261 | 0.089 | 0.006 * |
| Lateral bending | −0.065 | 0.575 | 0.910 | −0.063 | 0.773 | 0.936 | 0.325 | 0.688 | 0.639 | 0.037 | 0.782 | 0.962 |
| Axial rotation | 0.640 | 0.460 | 0.171 | 0.675 | 0.642 | 0.299 | 0.120 | 0.567 | 0.833 | 0.715 | 0.645 | 0.274 |
| Anterior translation | 0.263 | 0.088 | 0.005 * | 0.358 | 0.122 | 0.005 * | 0.281 | 0.105 | 0.011 * | 0.289 | 0.124 | 0.024 * |
| Distance moved | −2.361 | 15.353 | 0.879 | 31.364 | 20.431 | 0.132 | 18.900 | 0.139 | 0.305 | −2.202 | 21.060 | 0.917 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, M.W.; Seong, M.Y.; Song, Y.S.; Youn, K.; Yang, K.Y.; Lee, J.; Chung, S.G.; Kim, K. Comparison of Cervical Spine Kinematics and Clinical Neck Symptoms Between Mobile Device and Desktop Computer Use. Sensors 2025, 25, 1438. https://doi.org/10.3390/s25051438
Park MW, Seong MY, Song YS, Youn K, Yang KY, Lee J, Chung SG, Kim K. Comparison of Cervical Spine Kinematics and Clinical Neck Symptoms Between Mobile Device and Desktop Computer Use. Sensors. 2025; 25(5):1438. https://doi.org/10.3390/s25051438
Chicago/Turabian StylePark, Myung Woo, Min Yong Seong, Young Seop Song, Kibum Youn, Kyung Yong Yang, Jehee Lee, Sun Gun Chung, and Keewon Kim. 2025. "Comparison of Cervical Spine Kinematics and Clinical Neck Symptoms Between Mobile Device and Desktop Computer Use" Sensors 25, no. 5: 1438. https://doi.org/10.3390/s25051438
APA StylePark, M. W., Seong, M. Y., Song, Y. S., Youn, K., Yang, K. Y., Lee, J., Chung, S. G., & Kim, K. (2025). Comparison of Cervical Spine Kinematics and Clinical Neck Symptoms Between Mobile Device and Desktop Computer Use. Sensors, 25(5), 1438. https://doi.org/10.3390/s25051438







