A Comprehensive Review of Elbow Exoskeletons: Classification by Structure, Actuation, and Sensing Technologies
Abstract
1. Introduction
2. Methodology
3. Anatomy of Human Elbow
3.1. Bones and Joint Structure
3.2. Muscles and Tendons
3.3. Ligaments
3.4. Movement, Range of Motion, and Force
4. Elbow Exoskeleton Application
4.1. Assistive Application
4.2. Rehabilitation Application
4.3. Augmentation Application
5. Elbow Exoskeleton Classification
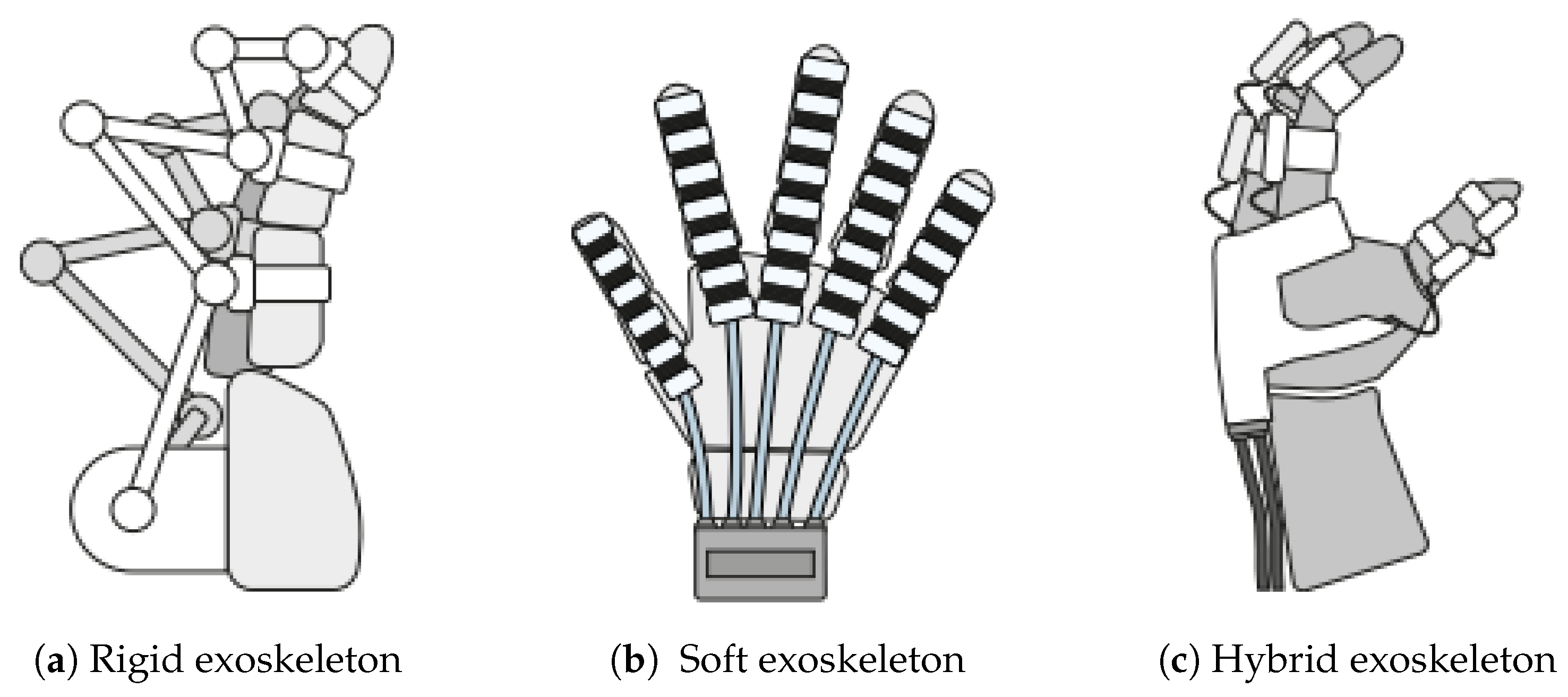
5.1. Rigid, Soft, and Hybrid Elbow Exoskeleton
5.2. Active and Passive Elbow Exoskeleton
6. Elbow Exoskeleton Actuation System
6.1. Pneumatic Actuator
6.2. Hydraulic Actuator
6.3. Cable-Based
6.4. Electric Actuator
6.5. Shape Memory Alloy
6.6. Variable Stiffness Actuator
6.7. Actuators Comparison
7. Elbow Exoskeleton Sensor Technologies
7.1. Force Sensor
7.2. Torque Sensor
7.3. EMG Sensor
7.4. IMU Sensor
7.5. Sensor Comparison
8. Existing Technologies of Elbow Exoskeleton

| Name | DoF | Application | Portability | Actuator | Sensor | Ref. |
|---|---|---|---|---|---|---|
| ExoSuit | FE | Assistive | Yes | TSA | Force Sensor, sEMG | [28] |
| Soft Elbow Exoskeleton | FE | Rehabilitation | Yes | Tendon-Sheath Actuator | sEMG, IMU | [2] |
| ULIX | FE, SP | Rehabilitation | No | Cable-Driven Actuator (Bowden Cable) | Position Sensor | [3] |
| Soft Exoskeleton | FE | Rehabilitation | Yes | Cable-Driven Actuator (Bowden Cable) | Force Sensor | [29] |
| Elbow Exoskeleton | FE | Assistive (Industrial Purposes) | Yes | Series Elastic Actuation | EMG Sensor | [32,33,34] |
| Elbow-sideWINDER | FE | Assistive (Industrial Purposes) | Yes | Cable-Driven Actuator (Bowden Cable) | Torque Sensor | [50] |
| Exoskeleton Arm | SP | Assistive | Yes | Cable-Driven Actuator (Bowden Cable) | Non Specified | [51] |
| Soft Wearable Exosuit | FE | Assistive | Yes | Cable-Driven Actuator (Bowden Cable) | Force Sensor | [30] |
| Exosuit | FE | Assistive | Yes | Cable-Driven Actuator (Bowden Cable) | IMU | [6] |
| NEUROExos | FE, SP | Rehabilitation | No | Electric Motor | Position, Torque Sensor | [52] |
| Elbow Exoskeleton | FE, SP | Rehabilitation | Yes | SMA | None Specified | [49] |
| Soft Elbow Exoskeleton | FE, SP | Assistive | No | Motor Tendon Actuator | Infrared Sensor | [31] |
| Carry | FE | Assistive (Industrial Purposes) | Yes | Pneumatic | Force Sensor | [39] |
| Soft Robotic Elbow Sleeve | FE | Assistive | Yes | Pneumatic | Force Sensor | [19] |
| Elbow Exoskeleton | FE | Experimental Purposes | No | TSA | Non Specified | [35] |
| Elbow Exoskeleton | FE, SP | Rehabilitation | No | VSA | Angle Sensor | [53] |
| DMLS-VSA Elbow Exoskeleton | FE | Rehabilitation | No | VSA | Force Sensor | [54] |
9. Design, Engineering, and Adoption Challenges of Elbow Exoskeleton
9.1. Design and Engineering Challenges
9.1.1. Actuator and Responsiveness
9.1.2. Comfort and Wearability
9.1.3. Weight and Device Placement
9.1.4. Safety and User Protection
9.1.5. Sensor Accuracy and Stability
9.1.6. Cost and Accessibility
9.1.7. Adjustability and Fit
9.1.8. Ease of Use and Setup
9.1.9. Design Appearance
9.2. Adoption and Real-World Implementation Challenges
9.2.1. Limited Long-Term Evidence and Field Validation
9.2.2. User Acceptability and Behavioral Resistance
9.2.3. Lack of Stakeholder Integration
9.2.4. Economic and Organizational Factors
10. Future Direction and Trends
10.1. Toward Fully Wearable and Portable System
10.2. Smart and Adaptive
10.3. Cost-Effective Manufacturing
11. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EMG | Electromyography |
| IMU | Inertial Measurement Unit |
| DOF | Degree of Freedom |
| UCL | Ulnar Collateral Ligament |
| RCL | Radial Collateral Ligament |
| WHO | World Health Organization |
| PLA | Polylactide |
| TSA | Twisted String Actuator |
| SMA | Shape memory alloy |
| sEMG | Surface Electromyography |
| SEA | Series elastic actuator |
| VSA | Variable Stiffness Actuator |
References
- Pehlivan, A.U.; Sergi, F.; Erwin, A.; Yozbatiran, N.; Francisco, G.E.; O’Malley, M.K. Design and Validation of the RiceWrist-S Exoskeleton for Robotic Rehabilitation after Incomplete Spinal Cord Injury. Robotica 2014, 32, 1415–1431. [Google Scholar] [CrossRef]
- Wu, Q.; Chen, Y. Adaptive cooperative control of a soft elbow rehabilitation exoskeleton based on improved joint torque estimation. Mech. Syst. Signal Process. 2023, 184, 109748. [Google Scholar] [CrossRef]
- Chen, T.; Casas, R.; Lum, P.S. An Elbow Exoskeleton for Upper Limb Rehabilitation With Series Elastic Actuator and Cable-Driven Differential. IEEE Trans. Robot. 2019, 35, 1464–1474. [Google Scholar] [CrossRef]
- Park, S.J.; Park, C.H. Suit-type Wearable Robot Powered by Shape-memory-alloy-based Fabric Muscle. Sci. Rep. 2019, 9, 9157. [Google Scholar] [CrossRef]
- Sambhav, R.; Jena, S.; Chatterjee, A.; Bhasin, S.; Santapuri, S.; Kumar, L.; Muthukrishnan, S.P.; Roy, S. An Integrated Dynamic Closed Loop Simulation Platform for Elbow Flexion Augmentation Using an Upper Limb Exosuit Model. Front. Robot. AI 2022, 9, 768841. [Google Scholar] [CrossRef]
- Missiroli, F.; Lotti, N.; Xiloyannis, M.; Sloot, L.H.; Riener, R.; Masia, L. Relationship Between Muscular Activity and Assistance Magnitude for a Myoelectric Model Based Controlled Exosuit. Front. Robot. AI 2020, 7, 595844. [Google Scholar] [CrossRef]
- Tiboni, M.; Borboni, A.; Vérité, F.; Bregoli, C.; Amici, C. Sensors and actuation technologies in exoskeletons: A review. Sensors 2022, 22, 884. [Google Scholar] [CrossRef] [PubMed]
- Gull, M.A.; Bai, S.; Bak, T. A Review on Design of Upper Limb Exoskeletons. Robotics 2020, 9, 16. [Google Scholar] [CrossRef]
- Kincaid, B.L.; An, K.N. Elbow joint biomechanics for preclinical evaluation of total elbow prostheses. J. Biomech. 2013, 46, 2331–2341. [Google Scholar] [CrossRef]
- Perrelli, M.; Lago, F.; Garofalo, S.; Bruno, L.; Mundo, D.; Carbone, G. A critical review and systematic design approach for innovative upper-limb rehabilitation devices. Robot. Auton. Syst. 2025, 183, 104835. [Google Scholar] [CrossRef]
- Javed, O.; Maldonado, K.A.; Ashmyan, R. Anatomy, Shoulder and Upper Limb, Muscles. 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482410/ (accessed on 18 May 2015).
- Olsen, B.S.; Michael, T.V.; Søjbjerg, J.O.; Helmig, P.; Sneppen, O. Lateral collateral ligament of the elbow joint: Anatomy and kinematics. J. Shoulder Elb. Surg. 1996, 5, 103–112. [Google Scholar] [CrossRef]
- Dragusanu, M.; Guinet, N.; Suthar, B.; Baldi, T.L.; Prattichizzo, D.; Malvezzi, M. A 3 Degrees-of-Freedom Lightweight Flexible Twisted String Actuators (TSAs)-Based Exoskeleton for Wrist Rehabilitation. IEEE Robot. Autom. Lett. 2025, 10, 6520–6527. [Google Scholar] [CrossRef]
- Eastman, J.; White, H.; Evans, J.; Augsburger, S.; Wallace, J.; Riley, S.; Iwinski, H. What is the minimum torque required to obtain passive elbow end range of motion? Gait Posture 2022, 93, 235–239. [Google Scholar] [CrossRef]
- Anam, K.; Al-Jumaily, A.A. Active Exoskeleton Control Systems: State of the Art. Procedia Eng. 2012, 41, 988–994. [Google Scholar] [CrossRef]
- Bardi, E.; Gandolla, M.; Braghin, F.; Resta, F.; Pedrocchi, A.L.G.; Ambrosini, E. Upper limb soft robotic wearable devices: A systematic review. J. Neuroeng. Rehabil. 2022, 19, 87. [Google Scholar] [CrossRef] [PubMed]
- Thøgersen, M.B.; Mohammadi, M.; Gull, M.A.; Bengtson, S.H.; Kobbelgaard, F.V.; Bentsen, B.; Khan, B.Y.; Severinsen, K.E.; Bai, S.; Bak, T.; et al. User Based Development and Test of the EXOTIC Exoskeleton: Empowering Individuals with Tetraplegia Using a Compact, Versatile, 5-DoF Upper Limb Exoskeleton Controlled through Intelligent Semi-Automated Shared Tongue Control. Sensors 2022, 22, 6919. [Google Scholar] [CrossRef]
- Guatibonza, A.; Solaque, L.; Velasco, A.; Peñuela, L. Assistive Robotics for Upper Limb Physical Rehabilitation: A Systematic Review and Future Prospects. Chin. J. Mech. Eng. 2024, 37, 69. [Google Scholar] [CrossRef]
- Koh, T.H.; Cheng, N.; Yap, H.K.; Yeow, C.H. Design of a Soft Robotic Elbow Sleeve with Passive and Intent-Controlled Actuation. Front. Neurosci. 2017, 11, 597. [Google Scholar] [CrossRef]
- Waheed, Z.A.; Humaidi, A.J.; Sadiq, M.E.; Al-Qassar, A.A.; Hasan, A.F.; Al-Dujaili, A.Q.; Ajel, A.R.; Abbas, S.J. Control of Elbow Rehabilitation System Based on Optimal-Tuned Backstepping Sliding Mode Controller. J. Eng. Sci. Technol. 2023, 18, 584–603. [Google Scholar]
- Rahman, M.H.; Rahman, M.J.; Cristobal, O.L.; Saad, M.; Kenné, J.P.; Archambault, P.S. Development of a whole arm wearable robotic exoskeleton for rehabilitation and to assist upper limb movements. Robotica 2015, 33, 19–39. [Google Scholar] [CrossRef]
- Butler, T.; Gillette, J.C. Exoskeletons Used as a PPE for Injury Prevention. Prof. Saf. 2019, 64, 32–37. [Google Scholar]
- Nnaji, C.; Okpala, I.; Gambatese, J.; Jin, Z. Controlling safety and health challenges intrinsic in exoskeleton use in construction. Saf. Sci. 2023, 157, 105943. [Google Scholar] [CrossRef]
- Butler, T.; Wisner, D. Exoskeleton Technology: Making Workers Safer and More Productive, Vol. All Days, Professional Development Conference and Exposition. 2017. Available online: https://onepetro.org/ASSPPDCE/proceedings-pdf/ASSE17/All-ASSE17/ASSE-17-579/1233834/asse-17-579.pdf (accessed on 1 March 2025).
- Proud, J.K.; Lai, D.T.H.; Mudie, K.L.; Carstairs, G.L.; Billing, D.C.; Garofolini, A.; Begg, R.K. Exoskeleton Application to Military Manual Handling Tasks. Hum. Factors 2022, 64, 527–554. [Google Scholar] [CrossRef] [PubMed]
- Taal, S.R.; Sankai, Y. Practical Design of Full Body Exoskeletons - Stretching the Limits of Weight and Power. In Proceedings of the Third International Conference on Biomedical Electronics and Devices, Barcelona, Spain, 11–14 February 2010; SciTePress—Science and Technology Publications: Setúbal, Portugal, 2010; pp. 133–138. [Google Scholar] [CrossRef][Green Version]
- Achilli, G.M.; Amici, C.; Dragusanu, M.; Gobbo, M.; Logozzo, S.; Malvezzi, M.; Tiboni, M.; Valigi, M.C. Soft, Rigid, and Hybrid Robotic Exoskeletons for Hand Rehabilitation: Roadmap with Impairment-Oriented Rationale for Devices Design and Selection. Appl. Sci. 2023, 13, 11287. [Google Scholar] [CrossRef]
- Hosseini, M.; Meattini, R.; San-Millan, A.; Palli, G.; Melchiorri, C.; Paik, J. A sEMG-Driven Soft ExoSuit Based on Twisted String Actuators for Elbow Assistive Applications. IEEE Robot. Autom. Lett. 2020, 5, 4094–4101. [Google Scholar] [CrossRef]
- Wei, W.; Qu, Z.; Wang, W.; Zhang, P.; Hao, F. Design on the Bowden Cable-Driven Upper Limb Soft Exoskeleton. Appl. Bionics Biomech. 2018, 2018, 1925694. [Google Scholar] [CrossRef]
- Xiloyannis, M.; Annese, E.; Canesi, M.; Kodiyan, A.; Bicchi, A.; Micera, S.; Ajoudani, A.; Masia, L. Design and Validation of a Modular One-To-Many Actuator for a Soft Wearable Exosuit. Front. Neurorobot. 2019, 13, 39. [Google Scholar] [CrossRef]
- Ismail, R.; Ariyanto, M.; Perkasa, I.A.; Adirianto, R.; Putri, F.T.; Glowacz, A.; Caesarendra, W. Soft Elbow Exoskeleton for Upper Limb Assistance Incorporating Dual Motor-Tendon Actuator. Electronics 2019, 8, 1184. [Google Scholar] [CrossRef]
- Mobedi, E.; Kim, W.; Momi, E.D.; Tsagarakis, N.G.; Ajoudani, A. A Soft Assistive Device for Elbow Effort-Compensation. In Proceedings of the 2021 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Prague, Czech Republic, 27 September–1 October 2021; pp. 9540–9547. [Google Scholar] [CrossRef]
- Mobedi, E.; Kim, W.; Leonori, M.; Tsagarakis, N.G.; Ajoudani, A. Design and Control of an Assistive Device for Elbow Effort-Compensation. IEEE/ASME Trans. Mechatronics 2023, 28, 3446–3457. [Google Scholar] [CrossRef]
- Mobedi, E.; Hjorth, S.; Kim, W.; De Momi, E.; Tsagarakis, N.G.; Ajoudani, A. A Power-Aware Control Strategy for an Elbow Effort-Compensation Device. IEEE Robot. Autom. Lett. 2023, 8, 4330–4337. [Google Scholar] [CrossRef]
- Popov, D.; Gaponov, I.; Ryu, J. A preliminary study on a twisted strings-based elbow exoskeleton. In Proceedings of the IEEE World Haptics Conference Proceedings, Daejeon, Republic of Korea, 14–17 April 2013; pp. 473–484. [Google Scholar] [CrossRef]
- Kim, Y.G.; Little, K.; Noronha, B.; Xiloyannis, M.; Masia, L.; Accoto, D. A voice activated bi-articular exosuit for upper limb assistance during lifting tasks. Robot. Comput.-Integr. Manuf. 2020, 66, 101995. [Google Scholar] [CrossRef]
- Paterna, M.; Gisolo, S.M.; Benedictis, C.D.; Muscolo, G.G.; Ferraresi, C. A passive upper-limb exoskeleton for industrial application based on pneumatic artificial muscles. Mech. Sci. 2022, 13, 387–398. [Google Scholar] [CrossRef]
- Huysamen, K.; Bosch, T.; de Looze, M.; Stadler, K.S.; Graf, E.; O’Sullivan, L.W. Evaluation of a passive exoskeleton for static upper limb activities. Appl. Ergon. 2018, 70, 148–155. [Google Scholar] [PubMed]
- Nassour, J.; Zhao, G.; Grimmer, M. Soft pneumatic elbow exoskeleton reduces the muscle activity, metabolic cost and fatigue during holding and carrying of loads. Sci. Rep. 2021, 11, 12556. [Google Scholar] [CrossRef]
- Lee, D.; Song, B.; Park, S.Y.; Baek, Y.S. Development and Control of an Electro-Hydraulic Actuator System for an Exoskeleton Robot. Appl. Sci. 2019, 9, 4295. [Google Scholar] [CrossRef]
- Palli, G.; Hosseini, M.; Melchiorri, C. Experimental Evaluation of Guided Twisted Actuation. IFAC-PapersOnLine 2016, 49, 380–385. [Google Scholar] [CrossRef]
- Kapsalyamov, A.; Hussain, S.; Jamwal, P.K. State of the Art Assistive Powered Upper Limb Exoskeletons for Elderly. IEEE Access 2017, 8, 178991–179001. [Google Scholar] [CrossRef]
- Park, S.J.; Choi, K.; Rodrigue, H.; Park, C.H. Fabric muscle with a cooling acceleration structure for upper limb assistance soft exosuits. Sci. Rep. 2022, 12, 11398. [Google Scholar] [CrossRef]
- Liu, Y.; Guo, S.; Hirata, H.; Ishihara, H.; Tamiya, T. Development of a powered variable-stiffness exoskeleton device for elbow rehabilitation. Biomed. Microdevices 2018, 20, 64. [Google Scholar] [CrossRef]
- Cestari, M.; Sanz-Merodio, D.; Arevalo, J.C.; Garcia, E. An Adjustable Compliant Joint for Lower-Limb Exoskeletons. IEEE/ASME Trans. Mechatronics 2015, 20, 889–898. [Google Scholar] [CrossRef]
- Liu, L.; Hong, Z.; Penzlin, B.; Misgeld, B.J.E.; Ngo, C.; Bergmann, L.; Leonhardt, S. Low Impedance-Guaranteed Gain-Scheduled GESO for Torque-Controlled VSA With Application of Exoskeleton-Assisted Sit-to-Stand. IEEE/ASME Trans. Mechatronics 2021, 26, 2080–2091. [Google Scholar] [CrossRef]
- Kim, J.H.; Shim, M.; Ahn, D.H.; Son, B.J.; Kim, S.Y.; Kim, D.Y.; Baek, Y.S.; Cho, B.K. Design of a Knee Exoskeleton Using Foot Pressure and Knee Torque Sensors. Int. J. Adv. Robot. Syst. 2015, 12, 112. [Google Scholar] [CrossRef]
- Neťuková, S.; Bejtic, M.; Malá, C.; Horáková, L.; Kutílek, P.; Kauler, J.; Krupička, R. Lower Limb Exoskeleton Sensors: State-of-the-Art. Sensors 2022, 22, 9091. [Google Scholar] [CrossRef]
- Copaci, D.; Martin, F.; Moreno, L.; Blanco, D. SMA Based Elbow Exoskeleton for Rehabilitation Therapy and Patient Evaluation. IEEE Access 2019, 7, 31473–31484. [Google Scholar] [CrossRef]
- Park, D.; Natali, C.D.; Sposito, M.; Caldwell, D.G.; Ortiz, J. Elbow-sideWINDER (Elbow-side Wearable INDustrial Ergonomic Robot): Design, control, and validation of a novel elbow exoskeleton. Front. Neurorobot. 2023, 17, 1168213. [Google Scholar] [CrossRef]
- Dežman, M.; Asfour, T.; Ude, A.; Gams, A. Exoskeleton Arm Pronation/Supination Assistance Mechanism With A Guided Double Rod System. In Proceedings of the 2019 IEEE-RAS 19th International Conference on Humanoid Robots (Humanoids), Toronto, ON, Canada, 15–17 October 2019; pp. 559–564. [Google Scholar] [CrossRef]
- Vitiello, N.; Lenzi, T.; Roccella, S.; De Rossi, S.M.; Cattin, E.; Giovacchini, F.; Vecchi, F.; Carrozza, M.C. NEUROExos: A Powered Elbow Exoskeleton for Physical Rehabilitation. IEEE Trans. Robot. 2013, 29, 220–235. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, F.; Fu, Y. A cable-driven elbow exoskeleton with variable stiffness actuator for upper limb rehabilitation. Robotica 2025, 43, 662–679. [Google Scholar] [CrossRef]
- Zhang, M.; Li, H.; Shi, K.; Song, A. Design, Modeling, and Control of a Variable Stiffness Actuator With Dual-Motor Load Sharing for Elbow Exoskeletons. IEEE/ASME Trans. Mechatronics 2025, 1–11. [Google Scholar] [CrossRef]
- Gull, M.A.; Thoegersen, M.; Bengtson, S.H.; Mohammadi, M.; Andreasen Struijk, L.N.; Moeslund, T.B.; Bak, T.; Bai, S. A 4-DOF Upper Limb Exoskeleton for Physical Assistance: Design, Modeling, Control and Performance Evaluation. Appl. Sci. 2021, 11, 5865. [Google Scholar] [CrossRef]
- Kim, B.; Deshpande, A.D. An upper-body rehabilitation exoskeleton Harmony with an anatomical shoulder mechanism: Design, modeling, control, and performance evaluation. Int. J. Robot. Res. 2017, 36, 414–435. [Google Scholar] [CrossRef]
- Popov, D.; Gaponov, I.; Ryu, J. Bidirectional Elbow Exoskeleton Based on Twisted-String Actuators. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS) Proceedings, Tokyo, Japan, 3–7 November 2013; pp. 5853–5858. [Google Scholar] [CrossRef]
- Botti, L.; Bacchetta, A.; Oliva, M.; Melloni, R. Exoskeletons at Work: Opportunities, Suggestions for Implementation and Future Research Needs. In Human Aspects of Advanced Manufacturing, Proceedings of the AHFE International Conference; Karwowski, W., Trzcielinski, S., Eds.; AHFE Open Access: Orlando, FL, USA, 2023; Volume 80. [Google Scholar] [CrossRef]
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodriguez-Guerrero, C.; et al. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef] [PubMed]
- Turchetti, G.; Vitiello, N.; Trieste, L.; Romiti, S.; Geisler, E.; Micera, S. Why Effectiveness of Robot-Mediated Neurorehabilitation Does Not Necessarily Influence Its Adoption. IEEE Rev. Biomed. Eng. 2014, 7, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Östlund, B.; Malvezzi, M.; Frennert, S.; Funk, M.; Gonzalez-Vargas, J.; Baur, K.; Alimisis, D.; Thorsteinsson, F.; Alonso-Cepeda, A.; Fau, G.; et al. Interactive robots for health in Europe: Technology readiness and adoption potential. Front. Public Health 2023, 11, 979225. [Google Scholar] [CrossRef]
- Dragusanu, M.; Troisi, D.; Suthar, B.; Prattichizzo, D.; Malvezzi, M. Development of a Soft Actuated Glove Based on Twisted String Actuators for Hand Rehabilitation. In Proceedings of the 2024 10th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), Heidelberg, Germany, 1–4 September 2024; pp. 1702–1708. [Google Scholar] [CrossRef]
- Dragusanu, M.; Troisi, D.; Suthar, B.; Hussain, I.; Prattichizzo, D.; Malvezzi, M. MGlove-TS: A modular soft glove based on twisted string actuators and flexible structures. Mechatronics 2024, 98, 103141. [Google Scholar] [CrossRef]
- Dragusanu, M. Hand/Wrist Exoskeleton. In Design of Soft–Rigid Devices for Rehabilitative and Assistive Robotics; Springer Nature: Cham, Switzerland, 2025; pp. 21–96. [Google Scholar] [CrossRef]
- Dragusanu, M.; Saeed, A.; Guinet, N.; Troisi, D.; Prattichizzo, D.; Malvezzi, M. Development of the Modular Finger Elements of an Actuated Glove for Hand Rehabilitation. In Advances in Italian Mechanism Science; Quaglia, G., Boschetti, G., Carbone, G., Eds.; Springer Nature: Cham, Switzerland, 2024; pp. 563–570. [Google Scholar] [CrossRef]
- Tomo, T.P.; Somlor, S.; Schmitz, A.; Jamone, L.; Huang, W.; Kristanto, H.; Sugano, S. Design and Characterization of a Three-Axis Hall Effect-Based Soft Skin Sensor. Sensors 2016, 16, 491. [Google Scholar] [CrossRef]
- Ray, T.; Choi, J.; Reeder, J.; Lee, S.P.; Aranyosi, A.J.; Ghaffari, R.; Rogers, J.A. Soft, skin-interfaced wearable systems for sports science and analytics. Curr. Opin. Biomed. Eng. 2019, 9, 47–56. [Google Scholar] [CrossRef]
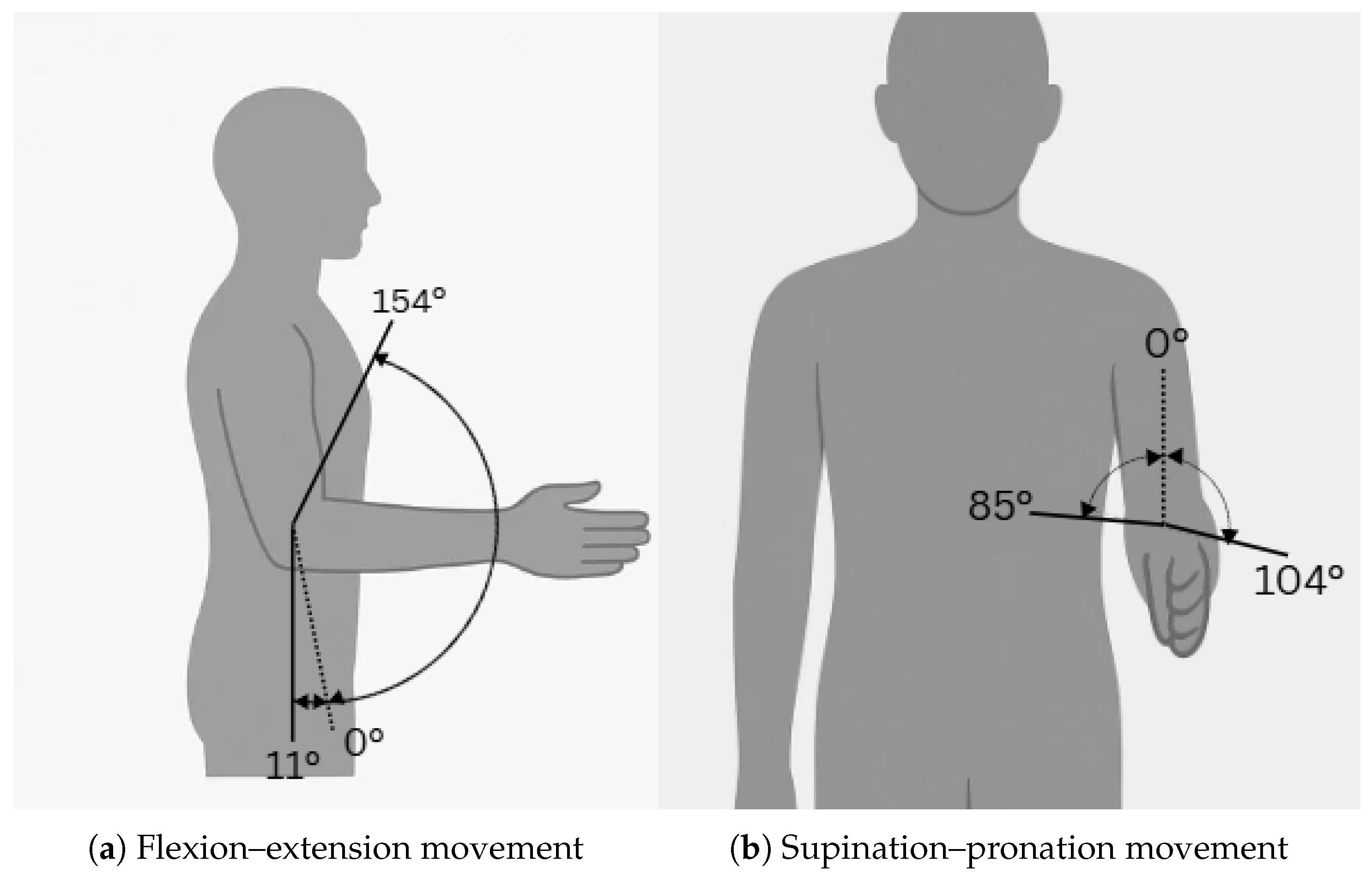
| Motion | ROM (Degrees) | Torque (Nm) | Reference |
|---|---|---|---|
| Flexion | 0°–154° | ∼2.7 | [10,14] |
| Extension | 0°–154° | ∼2.7 | [10,14] |
| Pronation | 0°–85° | ∼0.06 | [10,13] |
| Supination | 0°–104° | ∼0.06 | [10,13] |
| Actuator Type | Power Density | Control Precision | Weight | Portability | Compliance |
|---|---|---|---|---|---|
| Pneumatic | Medium | Moderate | Low | Low (requires compressor) | High (air compressibility) |
| Hydraulic | High | High | High (fluid + hardware) | Low (bulky pump/reservoir) | Low (fluid incompressibility) |
| Bowden Cable-Driven | Medium | Moderate to High | Low (motor remote) | High | Medium (some compliance) |
| TSA | Low to Medium | Moderate | Very Low | High | High (soft, compliant) |
| Electric (Motors) | High | High | Medium to High | High | Low to Medium |
| SMA | Low | Low to Moderate | Very Low | High | High (material properties) |
| VSA | Medium to High | High (stiffness and position control) | Medium (due to added stiffness mechanism) | Medium (depends on design) | High (adjustable stiffness improves compliance) |
| Category | Force Sensor | Torque Sensor | EMG Sensor | IMU |
|---|---|---|---|---|
| Measured Quantity | Linear force | Rotational force (torque) | Muscle activation (bioelectrical signal) | Orientation, acceleration, angular velocity |
| Advantages | Simple integration, ensures safety | Precise joint control, real-time feedback | Captures user intent, supports voluntary control | Compact, good for motion tracking |
| Disadvantages | May lack motion detail | Adds bulk, needs careful calibration | Noisy signals, affected by skin/electrode contact | Drift over time, limited accuracy alone |
| Common Applications | Load monitoring | Joint torque measurement | Intent detection in rehabilitation | Gait and arm motion analysis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Supriyono, C.S.A.; Dragusanu, M.; Malvezzi, M. A Comprehensive Review of Elbow Exoskeletons: Classification by Structure, Actuation, and Sensing Technologies. Sensors 2025, 25, 4263. https://doi.org/10.3390/s25144263
Supriyono CSA, Dragusanu M, Malvezzi M. A Comprehensive Review of Elbow Exoskeletons: Classification by Structure, Actuation, and Sensing Technologies. Sensors. 2025; 25(14):4263. https://doi.org/10.3390/s25144263
Chicago/Turabian StyleSupriyono, Callista Shekar Ayu, Mihai Dragusanu, and Monica Malvezzi. 2025. "A Comprehensive Review of Elbow Exoskeletons: Classification by Structure, Actuation, and Sensing Technologies" Sensors 25, no. 14: 4263. https://doi.org/10.3390/s25144263
APA StyleSupriyono, C. S. A., Dragusanu, M., & Malvezzi, M. (2025). A Comprehensive Review of Elbow Exoskeletons: Classification by Structure, Actuation, and Sensing Technologies. Sensors, 25(14), 4263. https://doi.org/10.3390/s25144263







