Transforming Healthcare: A Comprehensive Review of Augmented and Virtual Reality Interventions
Abstract
1. Introduction
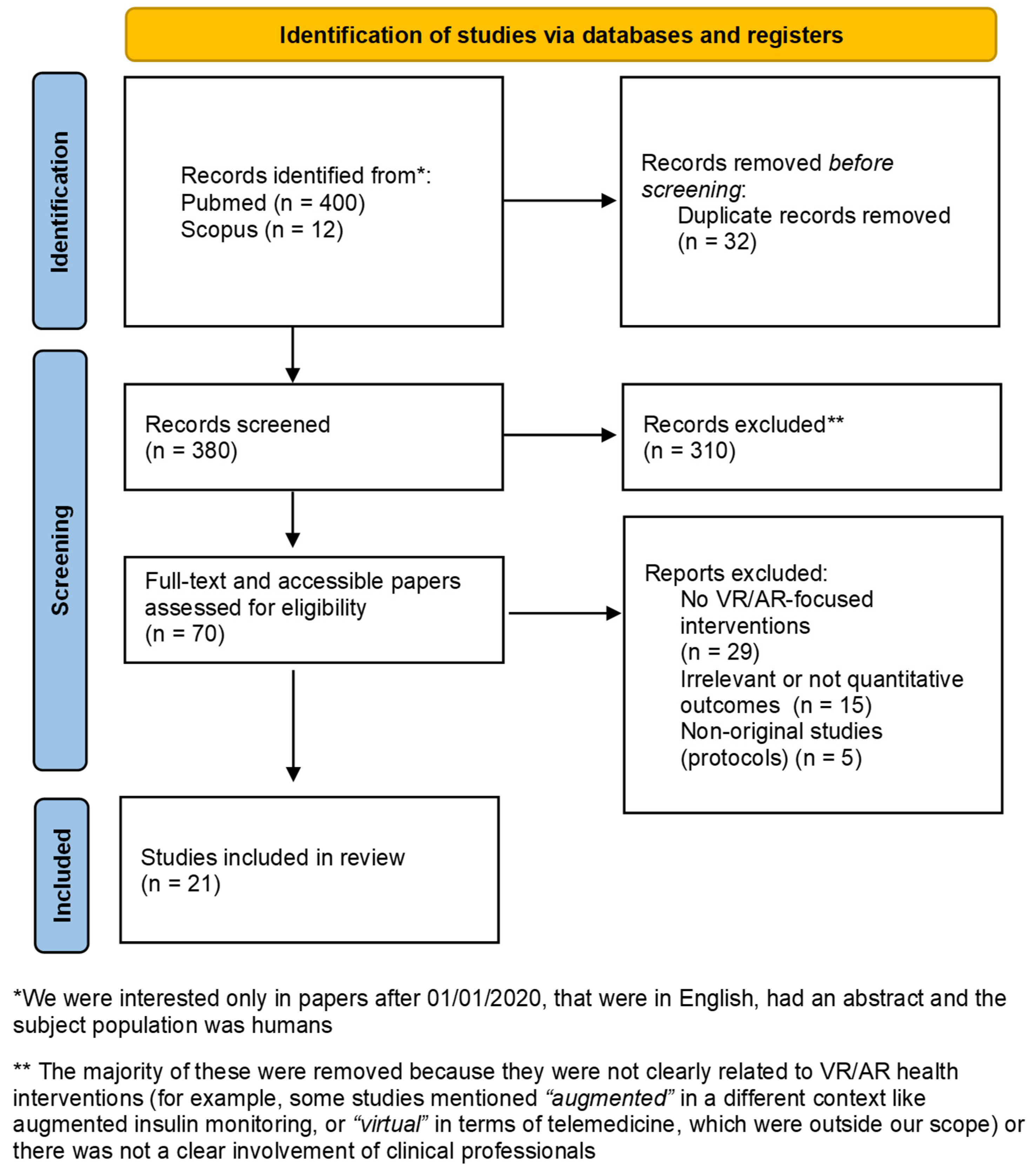
2. Methodology
3. Results
3.1. Literature Search Outcomes
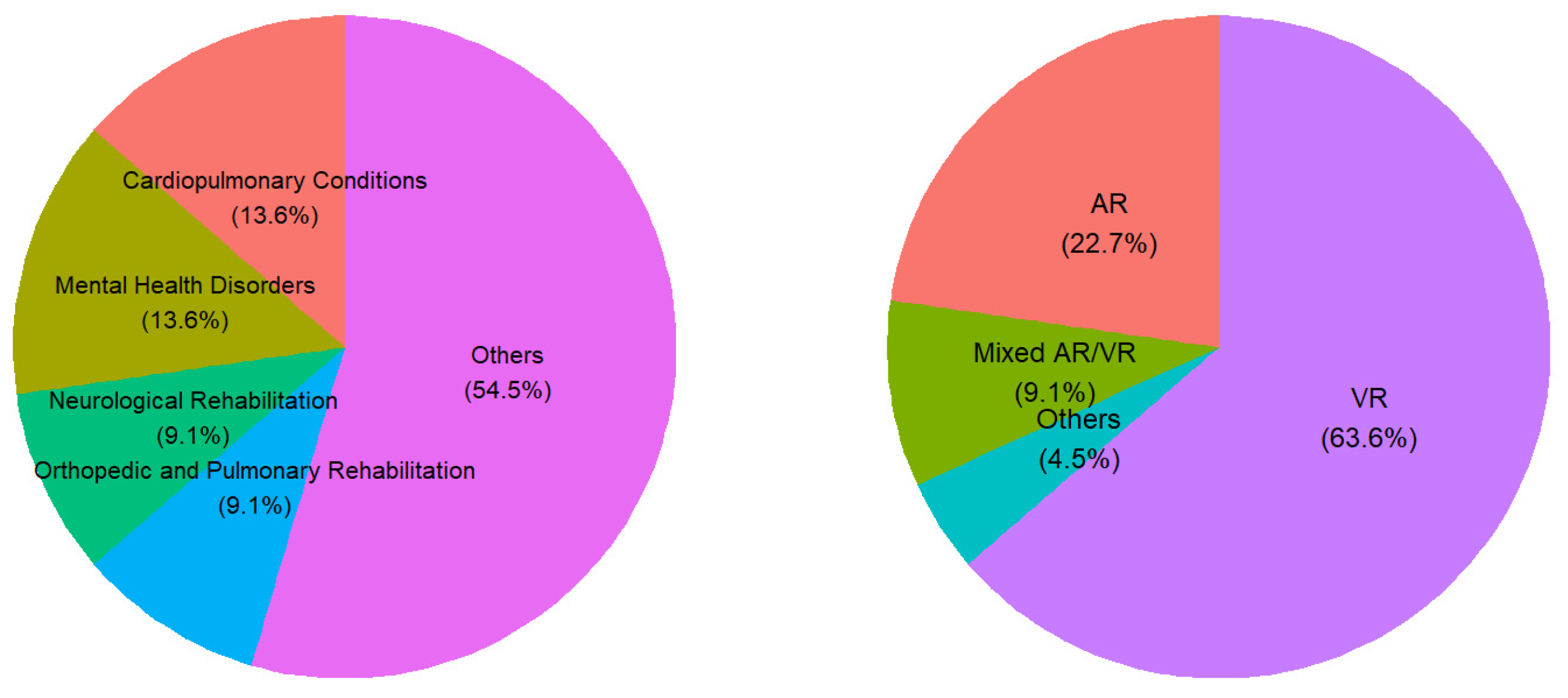
3.2. Characteristics of Included Studies
3.3. Quality Assessment
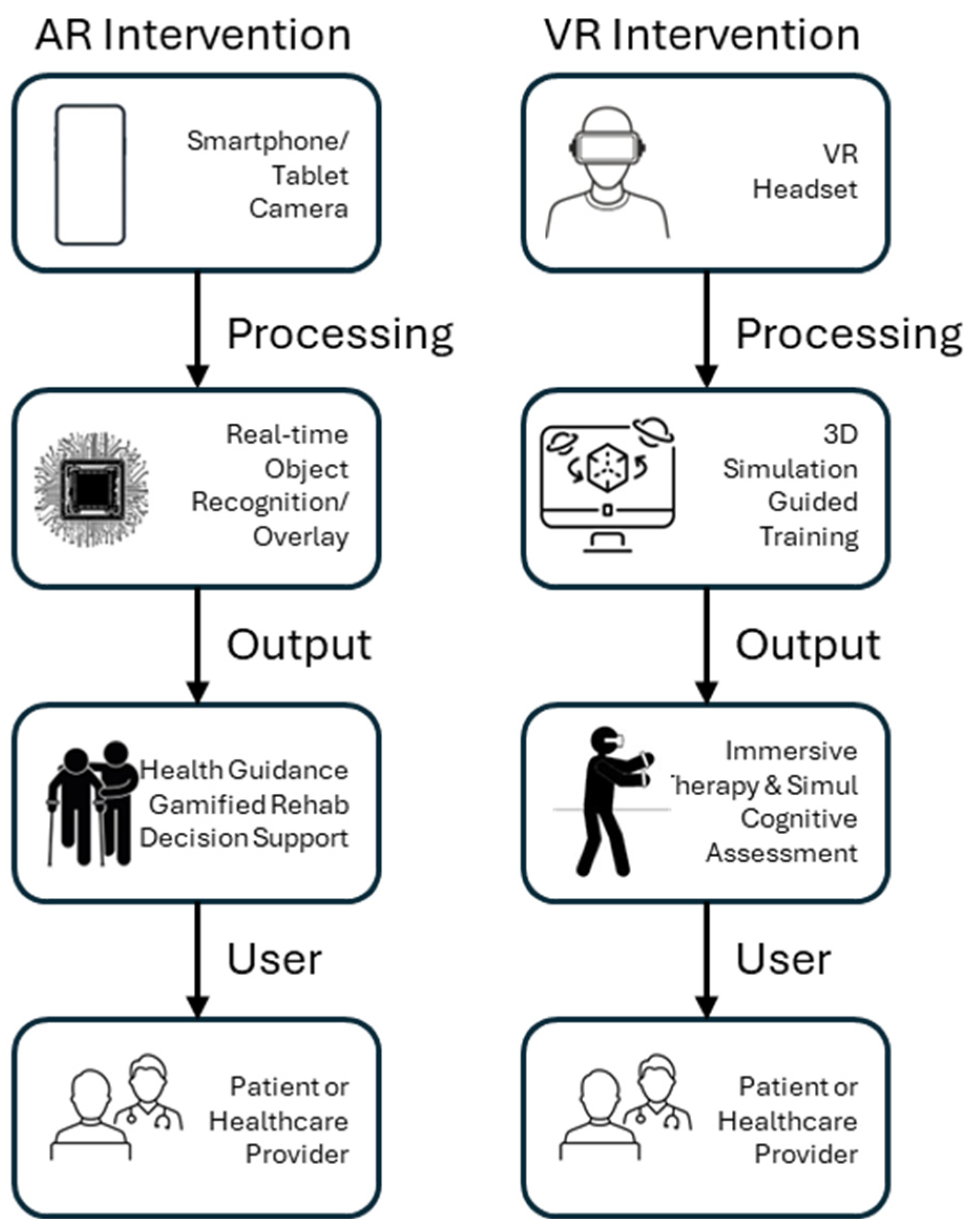
3.4. Main Intervention Features
3.5. Outcomes
3.6. Challenges with Using AR and VR Interventions
4. Discussion
4.1. Main Findings
4.2. Clinical Implications
4.3. Weaknesses of Included Studies
4.4. Technical and Usability Challenges
4.5. Recommendations
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Triantafyllidis, A.; Kondylakis, H.; Katehakis, D.; Kouroubali, A.; Alexiadis, A.; Segkouli, S.; Votis, K.; Tzovaras, D. Smartwatch interventions in healthcare: A systematic review of the literature. Int. J. Med. Inform. 2024, 44, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chirico, A.; Lucidi, F.; De Laurentiis, M.; Milanese, C.; Napoli, A.; Giordano, A. Virtual Reality in Health System: Beyond Entertainment. A Mini-Review on the Efficacy of VR During Cancer Treatment. J. Cell Physiol. 2016, 231, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Urlings, J.; Sezer, S.; Ter Laan, M.; Bartels, R.; Maal, T.; Boogaarts, J.; Henssen, D. The role and effectiveness of augmented reality in patient education: A systematic review of the literature. Patient Educ. Couns. 2022, 105, 1917–1927. [Google Scholar] [CrossRef]
- Sun, P.; Zhao, Y.; Men, J.; Ma, Z.R.; Jiang, H.Z.; Liu, C.Y.; Feng, W. Application of virtual and augmented reality technology in hip surgery: Systematic review. J. Med. Internet Res. 2023, 25, e37599. [Google Scholar] [CrossRef]
- Arjomandi Rad, A.; Vardanyan, R.; Thavarajasingam, S.G.; Zubarevich, A.; Van den Eynde, J.; Sá, M.P.B.; Zhigalov, K.; Sardiari Nia, P.; Ruhparwar, A.; Weymann, A. Extended, virtual and augmented reality in thoracic surgery: A systematic review. Interact. Cardiovasc. Thorac. Surg. 2022, 34, 201–211. [Google Scholar] [CrossRef]
- Detmer, F.J.; Hettig, J.; Schindele, D.; Schostak, M.; Hansen, C. Virtual and augmented reality systems for renal interventions: A systematic review. IEEE Rev. Biomed. Eng. 2017, 10, 78–94. [Google Scholar] [CrossRef] [PubMed]
- McCloskey, K.; Turlip, R.; Ahmad, H.S.; Ghenbot, Y.G.; Chauhan, D.; Yoon, J.W. Virtual and augmented reality in spine surgery: A systematic review. World Neurosurg. 2023, 173, 96–107. [Google Scholar] [CrossRef]
- Toledo-Peral, C.L.; Vega-Martínez, G.; Mercado-Gutiérrez, J.A.; Rodríguez-Reyes, G.; Vera-Hernández, A.; Leija-Salas, L.; Gutiérrez-Martínez, J. Virtual/augmented reality for rehabilitation applications using electromyography as control/biofeedback: Systematic literature review. Electronics 2022, 11, 2271. [Google Scholar] [CrossRef]
- Laghari, A.A.; Estrela, V.V.; Li, H.; Shoulin, Y.; Khan, A.A.; Anwar, M.S.; Wahab, A.; Bouraqia, K. Quality of experience assessment in virtual/augmented reality serious games for healthcare: A systematic literature review. Technol. Disabil. 2024, 36, 17–28. [Google Scholar] [CrossRef]
- Matthie, N.S.; Giordano, N.A.; Jenerette, C.M.; Magwood, G.S.; Leslie, S.L.; Northey, E.E.; Webster, C.I.; Sil, S. Use and efficacy of virtual, augmented, or mixed reality technology for chronic pain: A systematic review. Pain. Manag. 2022, 12, 859–878. [Google Scholar] [CrossRef] [PubMed]
- Lundin, R.M.; Yeap, Y.; Menkes, D.B. Adverse effects of virtual and augmented reality interventions in psychiatry: Systematic review. JMIR Ment. Health 2023, 10, e43240. [Google Scholar] [CrossRef]
- Nas, J.; Thannhauser, J.; Vart, P.; van Geuns, R.J.; Muijsers, H.E.C.; Mol, J.Q.; Aarts, G.W.A.; Konijnenberg, L.S.F.; Gommans, D.H.F.; Ahoud-Schoenmakers, S.G.A.M.; et al. Effect of face-to-face vs virtual reality training on cardiopulmonary resuscitation quality: A randomized clinical trial. JAMA Cardiol. 2020, 5, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Agrawal, S.; Peeta, S.; Benedyk, I. Safety and health perceptions of location-based augmented reality gaming app and their implications. Accid. Anal. Prev. 2021, 161, 106354. [Google Scholar] [CrossRef] [PubMed]
- Pascual, K.; Fredman, A.; Naum, A.; Patil, C.; Sikka, N. Should mindfulness for health care workers go virtual? A mindfulness-based intervention using virtual reality and heart rate variability in the emergency department. Workplace Health Saf. 2023, 71, 188–194. [Google Scholar] [CrossRef]
- Menhas, R.; Qin, L.; Saqib, Z.A.; Younas, M. The association between COVID-19 preventive strategies, virtual reality exercise, use of fitness apps, physical and psychological health: Testing a structural equation moderation model. Front. Public Health 2023, 11, 1170645. [Google Scholar] [CrossRef]
- Wang, P.H.; Wang, Y.J.; Chen, Y.W.; Hsu, P.T.; Yang, Y.Y. An augmented reality (AR) app enhances the pulmonary function and feasibility of perioperative rehabilitation in patients undergoing orthopedic surgery. Int. J. Environ. Res. Public Health 2022, 20, 648. [Google Scholar] [CrossRef]
- Menna, G.; Kolias, A.; Esene, I.N.; Barthélemy, E.J.; Hoz, S.; Laeke, T.; Veiga Silva, A.C.; Longo-Calderón, G.M.; Baticulon, R.E.; Pérez Zabala, J.; et al. Reducing the gap in neurosurgical education in LMICs: A report of a non-profit educational program. World Neurosurg. 2024, 182, e792–e797. [Google Scholar] [CrossRef]
- Sun, W.N.; Hsieh, M.C.; Wang, W.F. Nurses’ knowledge and skills after use of an augmented reality app for advanced cardiac life support training: Randomized controlled trial. J. Med. Internet Res. 2024, 26, e57327. [Google Scholar] [CrossRef]
- Maggio, M.G.; Luca, A.; D’Agate, C.; Italia, M.; Calabrò, R.S.; Nicoletti, A. Feasibility and usability of a non-immersive virtual reality tele-cognitive app in cognitive rehabilitation of patients affected by Parkinson’s disease. Psychogeriatrics 2022, 22, 775–779. [Google Scholar] [CrossRef]
- Finkelstein, J.; Parvanova, I.; Huo, X. Feasibility of a virtual reality app to promote pulmonary rehabilitation. Stud. Health Technol. Inform. 2023, 302, 458–462. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.D.; Morse, A.; Barter, J.; Mammino, K.; Bay, A.A.; Prusin, T.; Hackney, M.E. Walk with me hybrid virtual/in-person walking for older adults with neurodegenerative disease. J. Vis. Exp. 2023, e62869. [Google Scholar] [CrossRef]
- Lacey, C.; Frampton, C.; Beaglehole, B. oVRcome—Self-guided virtual reality for specific phobias: A randomised controlled trial. Aust. N. Z. J. Psychiatry 2023, 57, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Kreidler, T.; Ochsenfahrt, A. Rehago—A home-based training app using virtual reality to improve functional performance of stroke patients with mirror therapy and gamification concept: A pilot study. Stud. Health Technol. Inform. 2022, 292, 91–95. [Google Scholar] [CrossRef]
- Bruni, F.; Mancuso, V.; Panigada, J.; Stramba-Badiale, M.; Cipresso, P.; Pedroli, E. Exploring how older adults experience semAPP, a 360° media-based tool for memory assessment: Qualitative study. JMIR Aging 2024, 7, e56796. [Google Scholar] [CrossRef]
- Guldager, J.D.; Kjær, S.L.; Lyk, P.; Dietrich, T.; Rundle-Thiele, S.; Majgaard, G.; Stock, C. User experiences with a virtual alcohol prevention simulation for Danish adolescents. Int. J. Environ. Res. Public Health 2020, 17, 6945. [Google Scholar] [CrossRef] [PubMed]
- Vinci, C.; Brandon, K.O.; Kleinjan, M.; Hernandez, L.M.; Sawyer, L.E.; Haneke, J.; Sutton, S.K.; Brandon, T.H. Augmented reality for smoking cessation: Development and usability study. JMIR Mhealth Uhealth 2020, 8, e21643. [Google Scholar] [CrossRef]
- Martinez-Millana, A.; Gomez-Noé, A.; Hartvigsen, G.; Michalsen, H.; Anke, A.; Stellander, M.; Dybwad, D.; Luzi, T.; Henriksen, A. Augmented reality-based exergames for persons with intellectual disability. Stud. Health Technol. Inform. 2024, 316, 1094–1095. [Google Scholar] [CrossRef]
- Blackmore, R.; Giles, C.; Tremain, H.; Kelly, R.; Foley, F.; Fletcher, K.; Nedeljkovic, M.; Wadley, G.; Seabrook, E.; Thomas, N. Examining the use of virtual reality to support mindfulness skills practice in mood and anxiety disorders: Mixed methods study. J. Med. Internet Res. 2024, 26, e45640. [Google Scholar] [CrossRef]
- Ucero-Lozano, R.; Pérez-Llanes, R.; López-Pina, J.A.; Cuesta-Barriuso, R. 180-degree immersive VR motion visualization in the treatment of haemophilic ankle arthropathy. Haemophilia 2023, 29, 282–289. [Google Scholar] [CrossRef]
- Tomczyk, S.; Rahn, M.; Markwart, H.; Schmidt, S. A walk in the park? Examining the impact of app-based weather warnings on affective reactions and the search for information in a virtual city. Int. J. Environ. Res. Public Health 2021, 18, 8353. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Clinton, A.J.; Penka, J.; Gregory, M.E.; Sova, L.; Pfeil, S.; Patterson, J.; Maa, T. Smartphone-based virtual and augmented reality implicit association training (VARIAT) for reducing implicit biases toward patients among health care providers: App development and pilot testing. JMIR Serious Games 2024, 12, e51310. [Google Scholar] [CrossRef] [PubMed]
- Klemm, P.; Kleyer, A.; Tascilar, K.; Schuster, L.; Meinderink, T.; Steiger, F.; Lange, U.; Müller-Ladner, U.; Knitza, J.; Sewerin, P.; et al. A virtual reality–based app to educate health care professionals and medical students about inflammatory arthritis: Feasibility study. JMIR Serious Games 2021, 9, e23835. [Google Scholar] [CrossRef]
- Maples-Keller, J.L.; Bunnell, B.E.; Kim, S.J.; Rothbaum, B.O. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 2017, 25, 103–113. [Google Scholar] [CrossRef]
- Freeman, D.; Reeve, S.; Robinson, A.; Ehlers, A.; Clark, D.; Spanlang, B.; Slater, M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol. Med. 2018, 48, 2393–2400. [Google Scholar] [CrossRef] [PubMed]
- Birckhead, B.; Khalil, C.; Liu, X.; Conovitz, S.; Rizzo, A.; Danovitch, I.; Bullock, K.; Spiegel, B. Recommendations for methodology of virtual reality clinical trials in health care by an international working group. JMIR Ment. Health 2019, 6, e11973. [Google Scholar] [CrossRef]
- Garrett, B.; Taverner, T.; Gromala, D.; Tao, G.; Cordingley, E.; Sun, C. Virtual reality clinical research: Promises and challenges. JMIR Serious Games 2018, 6, e10839. [Google Scholar] [CrossRef]
- Trevi, R.; Chiappinotto, S.; Palese, A.; Galazzi, A. Virtual reality for cardiopulmonary resuscitation healthcare professionals training: A systematic review. J. Med. Syst. 2024, 48, 50. [Google Scholar] [CrossRef]
- Kondylakis, H.; Giglioli, I.A.C.; Katehakis, D.; Aldemir, H.; Zikas, P.; Papagiannakis, G.; Hors-Fraile, S.; González-Sanz, P.L.; Apostolakis, K.; Stephanidis, C.; et al. Stress Reduction in Perioperative Care: Feasibility Randomized Controlled Trial. J. Med. Internet Res. 2025, 27, e54049. [Google Scholar] [CrossRef]
- Kondylakis, H.; Giglioli, I.A.C.; Katehakis, D.G.; Aldemir, H.; Zikas, P.; Papagiannakis, G.; Hors-Fraile, S.; González-Sanz, P.L.; Apostolakis, K.C.; Stephanidis, C.; et al. A digital health intervention for stress and anxiety relief in perioperative care: Protocol for a feasibility randomized controlled trial. JMIR Res. Protoc. 2022, 11, e38536. [Google Scholar] [CrossRef]
- Roniotis, A.; Kondylakis, H.; Tsiknakis, M. Detection and Management of Depression in Cancer Patients Using Augmented Reality Technologies, Multimodal Signal Processing and Persuasive Interfaces. In Proceedings of the 2017 IEEE 30th International Symposium on Computer-Based Medical Systems (CBMS), Thessaloniki, Greece, 22–24 June 2017; pp. 751–752. [Google Scholar]
- Opriş, D.; Pintea, S.; García-Palacios, A.; Botella, C.; Szamosközi, Ş.; David, D. Virtual reality exposure therapy in anxiety disorders: A quantitative meta-analysis. Depress. Anxiety 2012, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 49, e160–e161. [Google Scholar] [CrossRef] [PubMed]
- Ehioghae, M.; Montoya, A.; Keshav, R.; Vippa, T.K.; Manuk-Hakobyan, H.; Hasoon, J.; Kaye, A.D.; Urits, I. Effectiveness of virtual reality–based rehabilitation interventions in improving postoperative outcomes for orthopedic surgery patients. Curr. Pain. Headache Rep. 2024, 28, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Pittara, M.; Matsangidou, M.; Pattichis, C.S. Virtual reality for pulmonary rehabilitation: Comprehensive review. JMIR Rehabil. Assist. Technol. 2023, 10, e47114. [Google Scholar] [CrossRef]
- Tsamitros, N.; Sebold, M.; Gutwinski, S.; Beck, A. Virtual reality-based treatment approaches in the field of substance use disorders. Curr. Addict. Rep. 2021, 8, 399–407. [Google Scholar] [CrossRef]
| Authors/Year | Title | Journal | Intervention Focus Summary |
|---|---|---|---|
| Nas et al., 2020 [13] | Effect of face-to-face vs virtual reality training on cardiopulmonary resuscitation quality: A randomized clinical trial. | JAMA Cardiology | Comparing VR-based CPR training to traditional face-to-face training for improving CPR skills. |
| Guo et al., 2021 [14] | Safety and health perceptions of location-based augmented reality gaming app and their implications. | Accident Analysis & Prevention | Investigating a location-based AR game (Pokémon GO) for its safety concerns and physical/mental health benefits. |
| Pascual et al., 2023 [15] | Should mindfulness for health care workers go virtual? A mindfulness-based intervention using virtual reality and heart rate variability in the emergency department. | Workplace Health & Safety | A VR-delivered mindfulness and biofeedback intervention to reduce stress in emergency department healthcare workers. |
| Menhas et al., 2023 [16] | The association between COVID-19 preventive strategies, virtual reality exercise, use of fitness apps, physical, and psychological health: Testing a structural equation moderation model. | Frontiers in Public Health | Examining relationships between VR exercise, fitness app use, and physical/mental health outcomes during COVID-19. |
| Wang et al., 2022 [17] | An augmented reality (AR) app enhances the pulmonary function and potency/feasibility of perioperative rehabilitation in patients undergoing orthopedic surgery. | International Journal of Environmental Research and Public Health | Using an AR mobile app to improve pulmonary function as part of pre- and post-operative rehab for orthopedic surgery patients. |
| Menna et al., 2024 [18] | Reducing the gap in neurosurgical education in LMICs: A report of a non-profit educational program. | World Neurosurgery | Implementing AR/VR-enhanced neurosurgical training to improve surgical education in low-resource settings. |
| Sun et al., 2024 [19] | Nurses’ knowledge and skills after use of an augmented reality app for advanced cardiac life support training: Randomized controlled trial. | Journal of Medical Internet Research | Evaluating an AR training app for nurses to improve Advanced Cardiac Life Support (ACLS) skills. |
| Maggio et al., 2022 [20] | Feasibility and usability of a non-immersive virtual reality tele-cognitive app in cognitive rehabilitation of patients affected by Parkinson’s disease. | Psychogeriatrics | Testing a home-based, non-immersive VR cognitive rehabilitation app for patients with Parkinson’s disease. |
| Finkelstein et al., 2023 [21] | Feasibility of a virtual reality app to promote pulmonary rehabilitation. | Studies in Health Technology & Informatics | Assessing the usability and acceptance of a VR application designed to support pulmonary rehabilitation exercises. |
| Wells et al., 2023 [22] | Walk with me hybrid virtual/in-person walking for older adults with neurodegenerative disease. | Journal of Visualized Experiments | A combined virtual reality and in-person group walking program for older adults with neurodegenerative conditions. |
| Lacey et al., 2023 [23] | oVRcome—Self-guided virtual reality for specific phobias: A randomised controlled trial. | Australian & New Zealand J. Psychiatry | A self-guided VR exposure therapy app (“oVRcome”) for treating specific phobias (fear of flying, heights, etc.). |
| Chen et al., 2022 [24] | Rehago—A home-based training app using virtual reality to improve functional performance of stroke patients with mirror therapy and gamification concept: A pilot study. | Studies in Health Technology & Informatics | A home-based VR rehabilitation app (“Rehago”) incorporating mirror therapy and game elements for stroke recovery. |
| Bruni et al., 2024 [25] | Exploring how older adults experience semAPP, a 360° media-based tool for memory assessment: Qualitative study. | JMIR Aging | User experience with “semAPP,” a 360° AR/VR application for assessing memory in older adults. |
| Guldager et al., 2020 [26] | User experiences with a virtual alcohol prevention simulation for Danish adolescents. | Int. Journal of Environ. Res. Public Health | Adolescents’ engagement with a VR simulation designed to educate and prevent underage alcohol use. |
| Vinci et al., 2020 [27] | Augmented reality for smoking cessation: Development and usability study. | JMIR mHealth and uHealth | Development and user testing of an AR-based application to support smokers in quitting (cue exposure therapy). |
| Martinez-Millana et al., 2024 [28] | Augmented reality-based exergames for persons with intellectual disability. | Studies in Health Technology & Informatics | Introducing AR “exergames” (exercise games) to encourage physical activity among people with intellectual disabilities. |
| Blackmore et al., 2024 [29] | Examining the use of virtual reality to support mindfulness skills practice in mood and anxiety disorders: Mixed methods study. | Journal of Medical Internet Research | Using VR environments to facilitate mindfulness meditation practice for individuals with anxiety and mood disorders. |
| Ucero-Lozano et al., 2023 [30] | 180-degree immersive VR motion visualization in the treatment of haemophilic ankle arthropathy. | Haemophilia | Applying immersive 180° virtual reality visualizations of movement to help manage pain and improve joint mobility in hemophilia. |
| Tomczyk et al., 2021 [31] | A walk in the park? Examining the impact of app-based weather warnings on affective reactions and the search for information in a virtual city. | Int. Journal of Environ. Res. Public Health | Simulating emergency weather alerts in VR to study users’ emotional responses and information-seeking behavior. |
| Shen et al., 2024 [32] | Smartphone-Based Virtual and Augmented Reality Implicit Association Training (VARIAT) for Reducing Implicit Biases Toward Patients Among Health Care Providers: App Development and Pilot Testing | JMIR Serious Games | Develop and evaluate the preliminary efficacy of VARIAT to reduce implicit biases among Medicaid providers. |
| Klemm et al., 2021 [33] | A virtual reality–based app to educate health care professionals and medical students about inflammatory arthritis: feasibility study | JMIR Serious Games | Educate health care professionals and medical students about inflammatory arthritis. |
| Study | EPHPP Criteria | Global Rating | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Selection Bias | Study Design | Confounders | Blinding | Data Collection | Withdrawal–Dropouts | Intervention Integrity | Analyses | ||
| Nas et al., 2020 [13] | M | M | S | W | S | M | N/A | S | M |
| Guo et al., 2021 [14] | M | M | M | W | M | N/A | N/A | S | M |
| Pascual et al., 2023 [15] | M | S | M | W | S | M | M | S | M |
| Menhas et al., 2023 [16] | M | M | M | W | M | N/A | N/A | S | M |
| Wang et al., 2022 [17] | M | M | M | W | S | M | S | M | M |
| Menna et al., 2024 [18] | M | W | W | N/A | M | N/A | M | M | W |
| Sun et al., 2024 [19] | M | S | M | W | S | S | S | S | M |
| Maggio et al., 2022 [20] | M | W | W | N/A | S | S | M | M | W |
| Finkelstein et al., 2023 [21] | M | W | W | N/A | S | S | S | M | W |
| Wells et al., 2023 [22] | M | W | W | N/A | S | S | S | M | W |
| Lacey et al., 2023 [23] | M | W | W | N/A | S | S | M | M | W |
| Chen et al., 2022 [24] | M | W | W | N/A | S | S | M | M | W |
| Bruni et al., 2024 [25] | M | W | W | N/A | S | S | M | M | W |
| Guldager et al., 2020 [26] | M | W | W | N/A | S | S | M | M | W |
| Vinci et al., 2020 [27] | M | W | W | N/A | S | S | M | M | W |
| Martinez-Millana et al., 2024 [28] | M | W | W | N/A | M | N/A | S | W | S |
| Blackmore et al., 2024 [29] | M | M | W | N/A | S | S | M | M | M |
| Ucero-Lozano et al., 2023 [30] | M | W | W | N/A | S | S | M | M | W |
| Tomczyk et al., 2021 [31] | M | M | S | N/A | S | S | S | S | S |
| Shen et al., 2024 [32] | M | W | W | N/A | M | S | S | M | W |
| Klemm et al., 2021 [33] | M | W | W | N/A | M | S | S | M | W |
| Study | Target Disease/Condition | AR/VR Device Used | Intervention Target | Additional Devices/Tools | Main Features of the Intervention |
|---|---|---|---|---|---|
| Nas et al., 2020 [13] | Cardiopulmonary resuscitation | VR headset | CPR training quality | None | Immersive VR CPR training with feedback on compression depth and rate. |
| Guo et al., 2021 [14] | General health/safety awareness | AR mobile app (Pokémon GO) | Health behavior and safety perception | Smartphone GPS | Location-based gameplay, physical activity encouragement, and safety perception analysis. |
| Pascual et al., 2023 [15] | Stress and Anxiety | VR Headset | Mental Well-being of Healthcare Workers | None | Guided mindfulness and relaxation exercises; immersive calming environments; stress reduction techniques. |
| Menhas et al., 2023 [16] | General Health | VR Fitness System | Physical Activity During COVID-19 | Fitness Apps | Virtual exercise programs, real-time coaching, integration with fitness tracking apps, and social engagement features. |
| Wang et al., 2022 [17] | Post-Orthopedic Surgery | AR Mobile App | Pulmonary Rehabilitation | Smartphone | AR-guided breathing exercises, personalized rehabilitation plans, progress monitoring, and patient education materials. |
| Menna et al., 2024 [18] | Neurosurgery Training | Mixed AR/VR | Surgical Skill Development | Smartphone/Tablet | Simulated surgical procedures; interactive 3D anatomy models; real-time feedback; collaborative training sessions. |
| Sun et al., 2024 [19] | Cardiac Emergencies | AR Headset | Advanced Life Support Skills | None | AR simulations of emergency scenarios, step-by-step procedural guidance, performance analytics, and team co-ordination drills. |
| Maggio et al., 2022 [20] | Parkinson’s Disease | Non-immersive VR | Cognitive Function Enhancement | Tablet | Cognitive exercises tailored for Parkinson’s patients; memory and attention tasks; adaptive difficulty levels. |
| Finkelstein et al., 2023 [21] | Chronic Pulmonary Conditions | VR System | Pulmonary Function Improvement | Smartphone App | Virtual pulmonary rehabilitation sessions, breathing exercises, patient education, and remote monitoring by clinicians. |
| Wells et al., 2023 [22] | Neurodegenerative Diseases | VR Headset | Mobility and Physical Activity | Sensors | Combined virtual and real-world walking programs, motion tracking, balance training, and personalized exercise routines. |
| Lacey et al., 2023 [23] | Specific Phobias | VR Headset | Phobia Treatment | Mobile App | Self-guided VR exposure therapy, customizable scenarios, anxiety management techniques, and progress tracking. |
| Chen et al., 2022 [24] | Stroke Recovery | VR Headset | Motor Function Rehabilitation | Sensors | Home-based VR exercises for stroke patients; real-time feedback; adaptive difficulty; integration with telehealth services. |
| Bruni et al., 2024 [25] | Memory Impairment | AR/VR Headset | Cognitive Assessment | Mobile App | Interactive memory assessment tools, real-time performance analysis, and personalized cognitive training plans. |
| Guldager et al., 2020 [26] | Alcohol Abuse Prevention | VR Headset | Adolescent Education | None | Simulated scenarios to educate on alcohol risks, decision-making exercises, and peer-pressure resistance training. |
| Vinci et al., 2020 [27] | Smoking Addiction | AR Mobile App | Smoking Cessation Support | Smartphone | AR-based cue exposure therapy to reduce cravings, personalized quit plans, progress tracking, and support community access. |
| Martinez-Millana et al., 2024 [28] | Intellectual Disabilities | AR Application | Physical Activity Engagement | Tablet/Smartphone | Interactive exergames to promote fitness, adaptive difficulty, social engagement features, and real-time feedback. |
| Blackmore et al., 2024 [29] | Mood and Anxiety Disorders | VR Headset | Mental Health Improvement | VR Mindfulness App | Guided mindfulness practices in a virtual setting, immersive calming environments, and stress and anxiety reduction techniques. |
| Ucero-Lozano et al., 2023 [30] | Hemophilia-Related Joint Issues | VR Headset | Pain Management and Mobility | Sensors | VR visualization techniques for pain management, joint mobility exercises, real-time feedback, and patient education. |
| Tomczyk et al., 2021 [31] | Public Safety | VR Simulation | Emergency Preparedness | Smartphone App | Virtual scenarios to assess responses to weather warnings, decision-making exercises, and public safety education. |
| Shen et al., 2024 [32] | Implicit Bias in Healthcare | Smartphone-based VR and AR | Bias Reduction Training for Health Professionals | Smartphone | Interactive VR/AR implicit association modules; case-based training on race, socioeconomic status, and LGBTQ+ bias; accessible through standard smartphones; user feedback and knowledge assessments. |
| Klemm et al., 2021 [33] | Inflammatory Arthritis | VR Headset | Medical Education (HCPs and Students) | VR-compatible smartphone | Immersive 3D simulation of arthritis patient experience; visual exploration of joint inflammation; educational modules on disease understanding and empathy building. |
| Study | Study Design | Participants | Age (Mean/Range) | Follow-Up Duration | Outcome Measures | Statistically Significant Outcomes |
|---|---|---|---|---|---|---|
| Nas et al., 2020 [13] | Randomized Clinical Trial | 381 | 26 years | Immediate | CPR quality | Significantly improved exercise capacity (mean increase in peak oxygen uptake: 2.2 mL/kg/min; 95% CI: 1.4–3.0; p < 0.001) and quality of life (mean increase in SF-36 physical component score: 4.0 points; 95% CI: 2.3–5.7; p < 0.001) compared to usual care. |
| Guo et al., 2021 [14] | Survey-Based Study | N/A | Adults (varied ages) | Cross-sectional | Physical activity, safety perceptions | Mixed results on safety behaviors and physical activity. Improvements in physical health (β = 0.34, p < 0.001), psychological health (β = 0.29, p < 0.001), and overall wellbeing (β = 0.31, p < 0.001). |
| Pascual et al., 2023 [15] | Randomized Clinical Trial | 45 | Adults | Immediate | Stress, heart rate variability | Significant anxiety/stress reduction, statistical significance not clearly tested. Weak positive correlation (0.157, p < 0.01) between ordinal session number and intrasession HRV progress. |
| Menhas et al., 2023 [16] | Cross-sectional Study | 2795 | Adults | Cross-sectional | Physical and psychological health | COVID-19 preventive strategies positively influenced virtual reality exercise (β = 0.385, p < 0.001). Virtual reality exercise positively affected physical health (β = 0.159, p < 0.001) and psychological health (β = 0.122, p < 0.001). Fitness app usage moderated these relationships, enhancing the positive effects. |
| Wang et al., 2022 [17] | Prospective Comparative Study | 66 | Adults | Prospective duration | Pulmonary outcomes | Improved pulmonary rehabilitation outcomes, statistical significance was not clearly tested. |
| Menna et al., 2024 [18] | Educational Validation Study | 168 | Medical trainees | Single session | Educational effectiveness, usability | High usability and educational effectiveness. In this study, 86% found the cadaver-free hybrid training system intuitive, and 83% agreed that the combination of mental training, augmented reality, and hands-on simulation effectively bridged the gap between theoretical knowledge and practical skills. |
| Sun et al., 2024 [19] | Randomized Controlled Trial | 102 | Nurses | Immediate | Cardiac life support skills | Significant improvement in ACLS skills. The AR group also reported high motivation (mean score: 141.65 ± 19.25) and usability (System Usability Scale score: 90.47 ± 11.91), with low cognitive load (mean score: 15.42 ± 5.76). |
| Maggio et al., 2022 [20] | Randomized Controlled Trial | 16 | 58.4 years | 6 weeks | Cognitive performance (Parkinson’s disease) | Significant cognitive improvement. The GAS score recorded at the end of the study (65.6 ± 4.2) was significantly higher than at baseline (38.5 ± 2.4; p-value < 0.001). |
| Finkelstein et al., 2023 [21] | Pilot Feasibility Study | 9 | Adults | Pilot period | Pulmonary outcomes | Statistically significant increase in patient knowledge (mean score increase from 7.2 to 7.9; p < 0.04), with a high usability score (System Usability Scale: 95.8). |
| Wells et al., 2023 [22] | Comparative Study | 40 | Older adults | Study duration | Physical and mental health | Improved physical and psychological health outcomes, statistical significance was not clearly tested. |
| Lacey et al., 2023 [23] | Randomized Controlled Trial | 126 | 18–64 years | 6 weeks | Severity of specific phobias | Significantly greater reduction in specific phobia severity scores (mean change: −20.53 ± 8.24) compared to the waitlist control group (−12.31 ± 10.66), with an effect size of 0.86 (p < 0.001). |
| Chen et al., 2022 [24] | Pilot Study | 48 | Adults | 6 weeks | Functional outcomes post-stroke | Ιmprovements in functional independence (mean FIM score increase of 5.54 points) and quality of life (mean EQ5D-5L score increase of 7.13 points) after a 6-week intervention. |
| Bruni et al., 2024 [25] | Feasibility Study | 34 | Older adults (60+) | Single session | Cognitive/memory assessment | Effective cognitive assessment, statistical significance was not clearly tested. |
| Guldager et al., 2020 [26] | Randomized Controlled Trial | 31 | Adolescents (16–18) | Single session | Alcohol risk perception | Improved awareness and risk perception, statistical significance was not clearly tested. |
| Vinci et al., 2020 [27] | Randomized Controlled Trial | 50 | Adults (average 34) | 8 weeks | Smoking abstinence, cravings | Significant craving reduction, improved abstinence. Εxposure to smoking-related augmented reality images elicited a significantly higher urge to smoke (median = 4.58, SD = 3.49) compared to neutral images (median = 1.42, SD = 3.01), with a Wilcoxon signed-rank test yielding Z = −2.14, p = 0.03, and a large effect size (Cohen’s d = 0.70). |
| Martinez-Millana et al., 2024 [28] | Feasibility Study | 24 | Young adults (18–30) | 4 weeks | Physical activity levels | Increased physical activity. Statistical significance was not clearly tested. |
| Blackmore et al., 2024 [29] | Randomized Controlled Trial | 45 | Adults (18–60) | 8 weeks | Anxiety and depression symptoms | Improved mood, reduced anxiety. Mean curiosity and decentering increased significantly (Cohen d = 1.3 and 1.51, respectively; p < 0.001). Negative affect on the Positive and Negative Affect Schedule (Cohen d = 0.62; p = 0.003) and State–Trait Anxiety Inventory Y-1 state anxiety (Cohen d = 0.84; p < 0.001) significantly reduced. |
| Ucero-Lozano et al., 2023 [30] | Feasibility Study | 14 | Adults (30–50) | Single session | Joint mobility, pain management | Improved mobility, reduced pain. Statistically significant differences in joint state (F = 51.38; η2p = 0.63), pressure pain threshold of the lateral malleolus (F = 12.34; η2p = 0.29), and range of motion (F = 11.7; η2p = 0.28). |
| Tomczyk et al., 2021 [31] | Quasi-experimental 2 × 2 × 2 factorial design | 276 | Adults (17–83) | Single session | Momentary anxiety | Participants who received a warning message and were confronted with a thunderstorm showed the highest increase in momentary anxiety (video: +0.67, vignette: +0.58; both p < 0.001), which predicted information seeking intentions (β = 0.46, p < 0.001). |
| Shen et al., 2024 [32] | Pilot Pre–Post Study | 18 Medicaid Providers | Not reported; adult professionals | Single session | Training reaction, affective knowledge, skill-based knowledge | Significant improvement in LGBTQ+ bias-related knowledge (Cohen d = 0.72; 95% CI −1.38 to −0.04). |
| Klemm et al., 2021 [33] | Feasibility Study | 125 (HCPs and medical students) | Adults (18–70) | Single session | Knowledge and attitude changes toward arthritis | Reported improvements in attitudes and empathy, but the statistical significance was not clearly tested. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrakis, A.; Koumakis, L.; Kazantzaki, E.; Kondylakis, H. Transforming Healthcare: A Comprehensive Review of Augmented and Virtual Reality Interventions. Sensors 2025, 25, 3748. https://doi.org/10.3390/s25123748
Petrakis A, Koumakis L, Kazantzaki E, Kondylakis H. Transforming Healthcare: A Comprehensive Review of Augmented and Virtual Reality Interventions. Sensors. 2025; 25(12):3748. https://doi.org/10.3390/s25123748
Chicago/Turabian StylePetrakis, Aristeidis, Lefteris Koumakis, Eleni Kazantzaki, and Haridimos Kondylakis. 2025. "Transforming Healthcare: A Comprehensive Review of Augmented and Virtual Reality Interventions" Sensors 25, no. 12: 3748. https://doi.org/10.3390/s25123748
APA StylePetrakis, A., Koumakis, L., Kazantzaki, E., & Kondylakis, H. (2025). Transforming Healthcare: A Comprehensive Review of Augmented and Virtual Reality Interventions. Sensors, 25(12), 3748. https://doi.org/10.3390/s25123748








