The Difference in the Assessment of Knee Extension/Flexion Angles during Gait between Two Calibration Methods for Wearable Goniometer Sensors
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
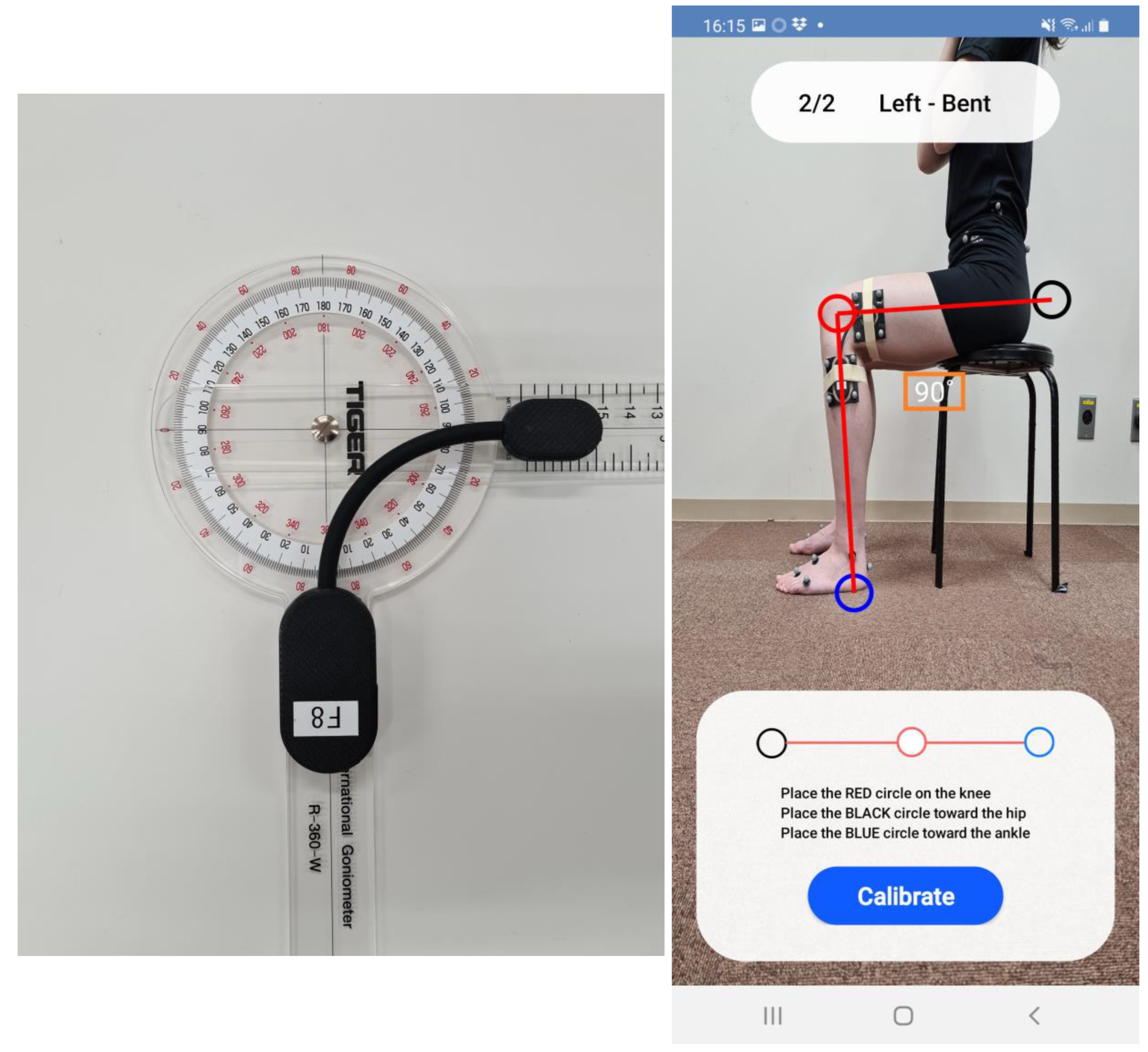
2.3. Knee Kinematics Analysis Using a Wearable Goniometer
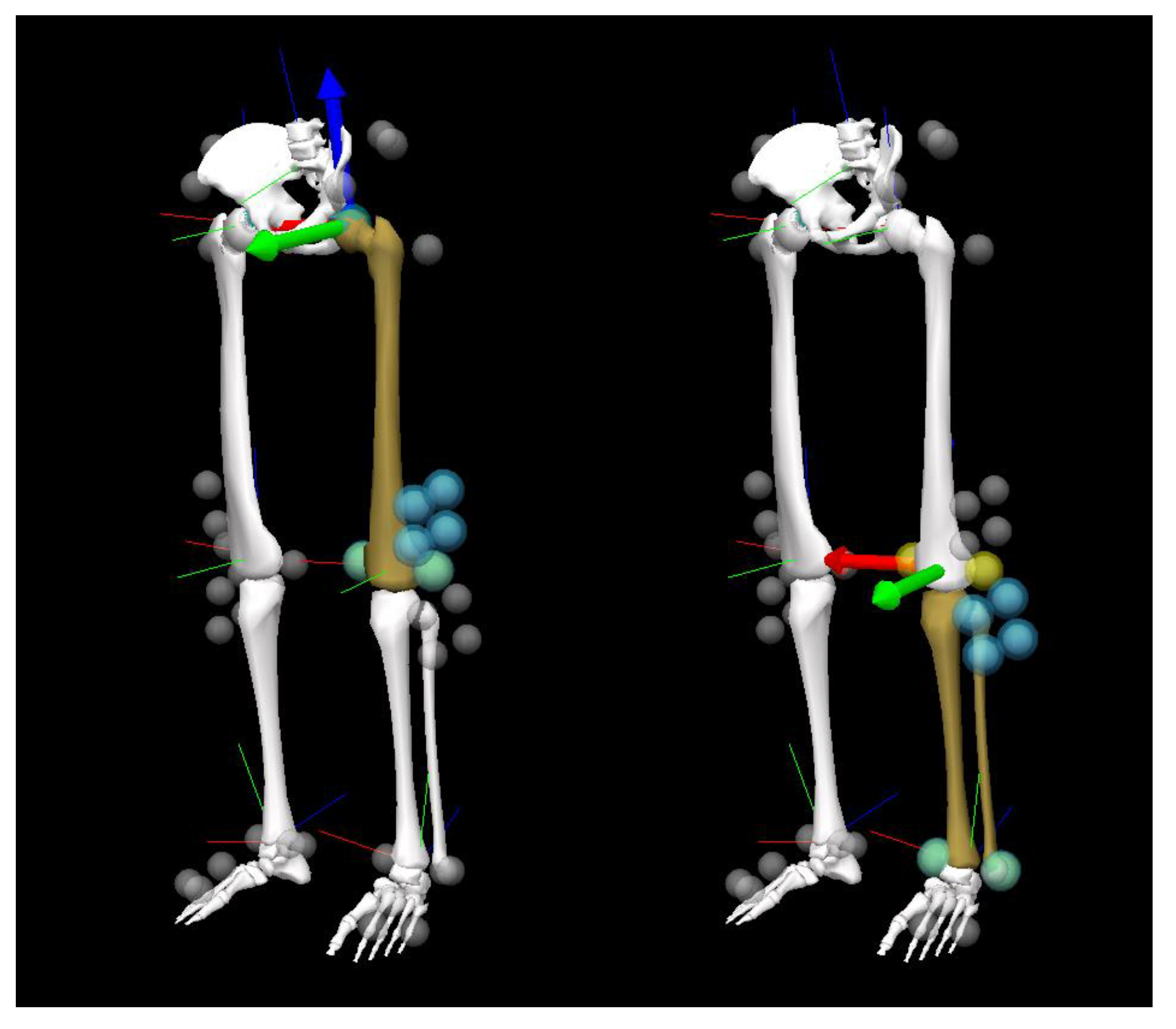
2.4. Knee Kinematics Analysis Using a Three-Dimensional Motion Analysis System
2.5. Data Analysis
2.6. Statistical Analysis
- CMC ≥ 0.95: excellent
- 0.95 > CMC ≥ 0.85: very good
- 0.85 > CMC ≥ 0.75: good
- 0.75 > CMC ≥ 0.65: moderate
- AE ≤ 2°: good accuracy
- 2 < AE ≤ 5°: acceptable accuracy
- 5° < AE ≤ 10°: tolerable accuracy
- AE > 10°: unacceptable accuracy
3. Results
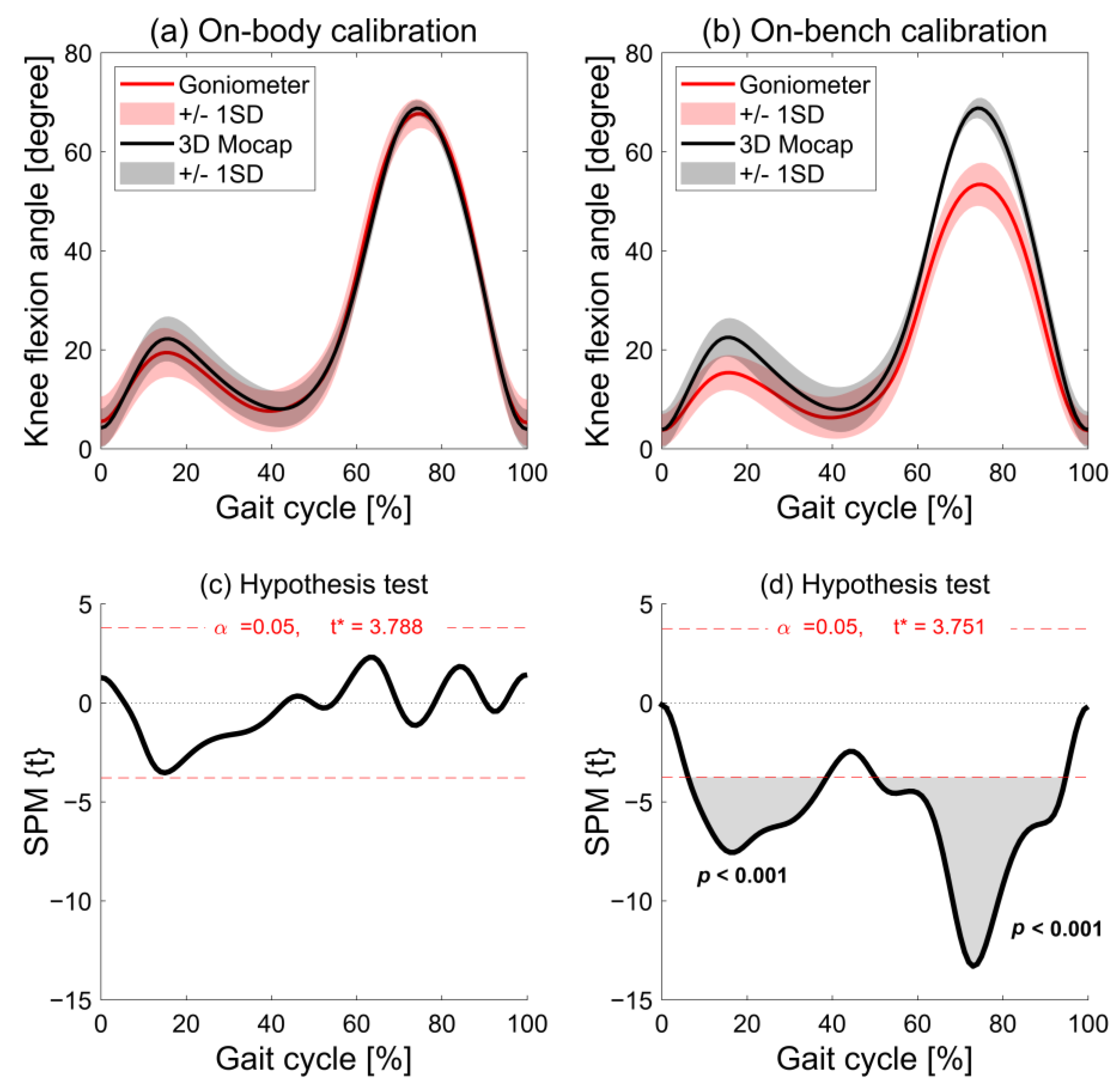
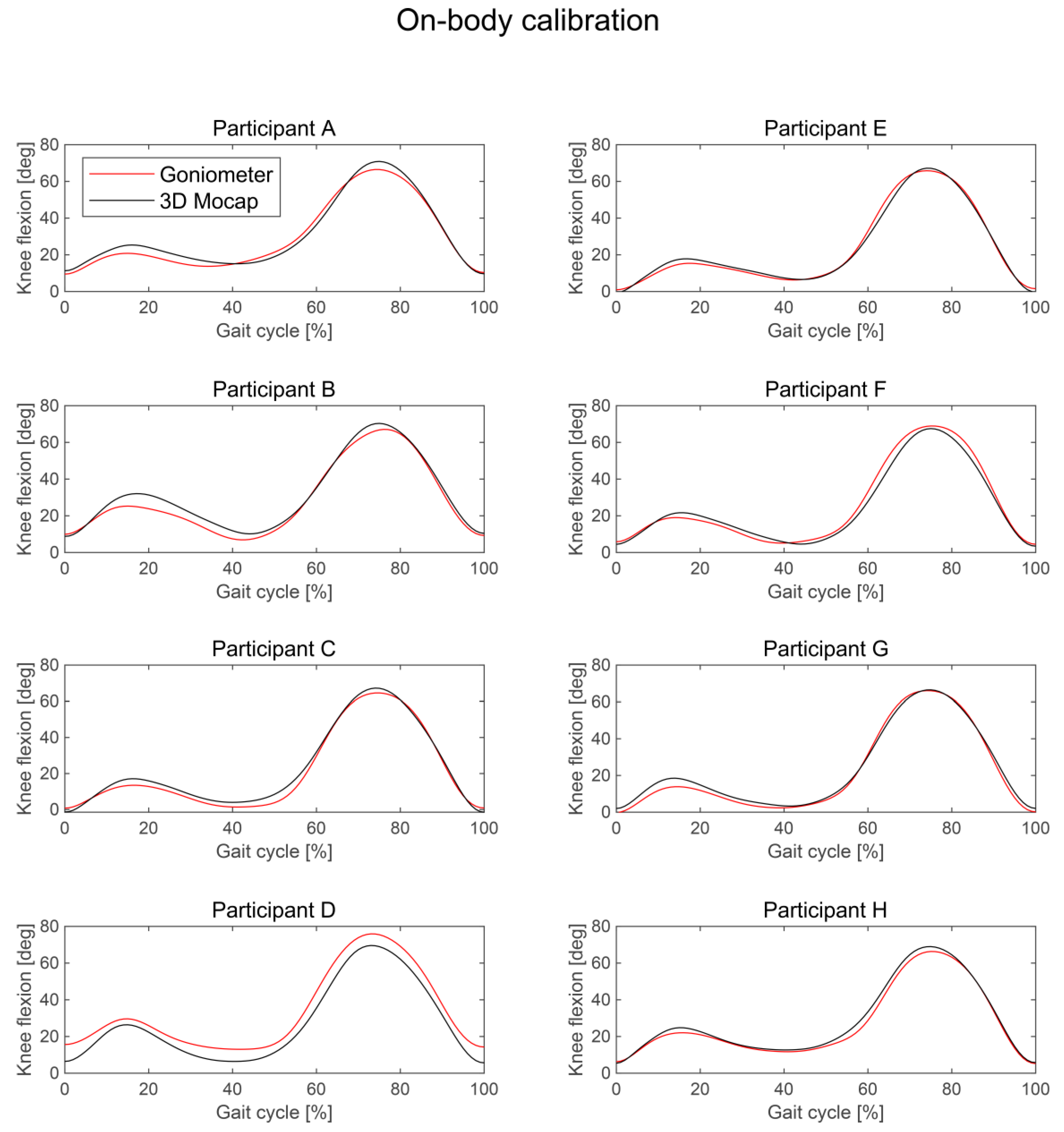
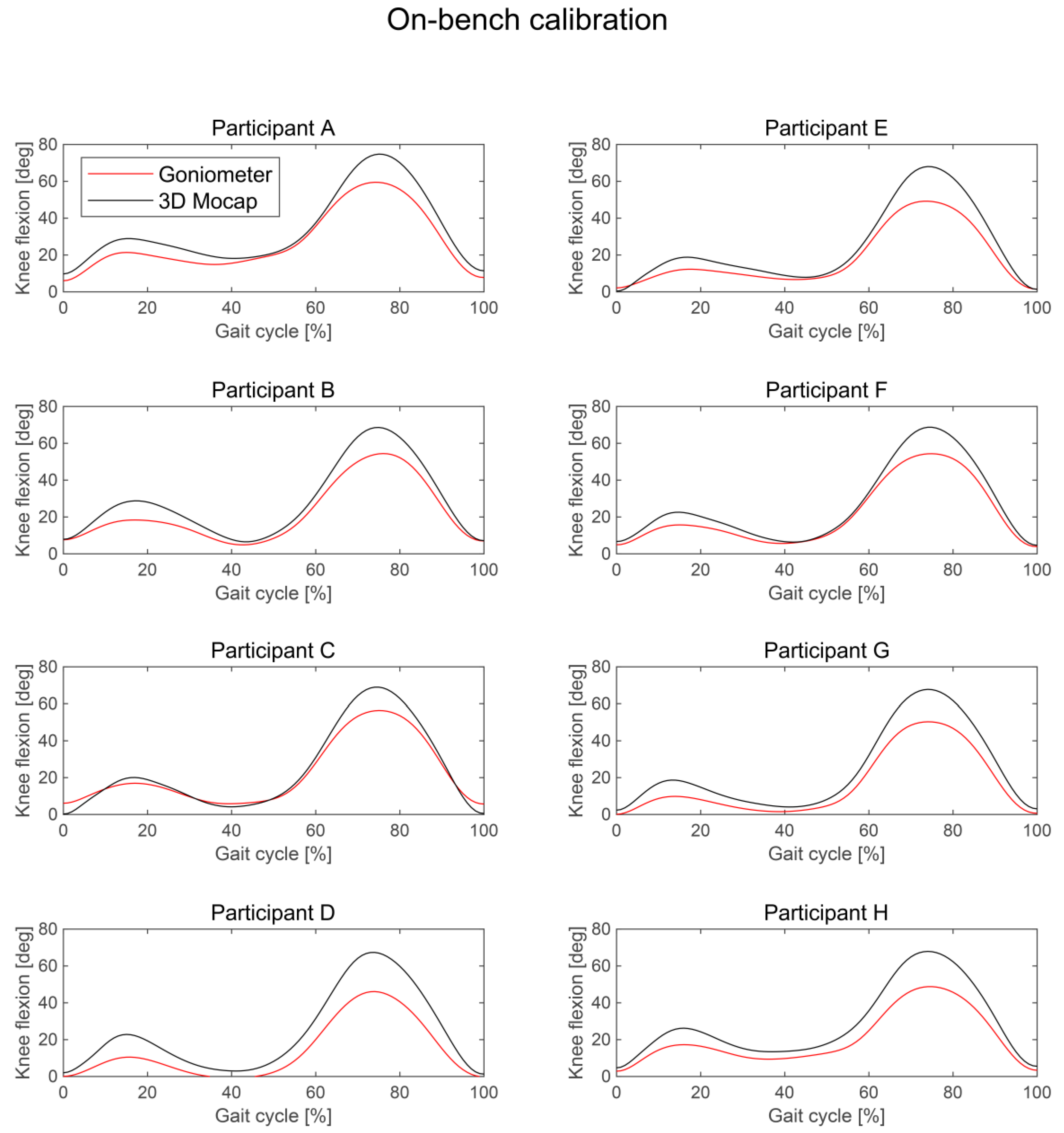
3.1. Waveform Similarity
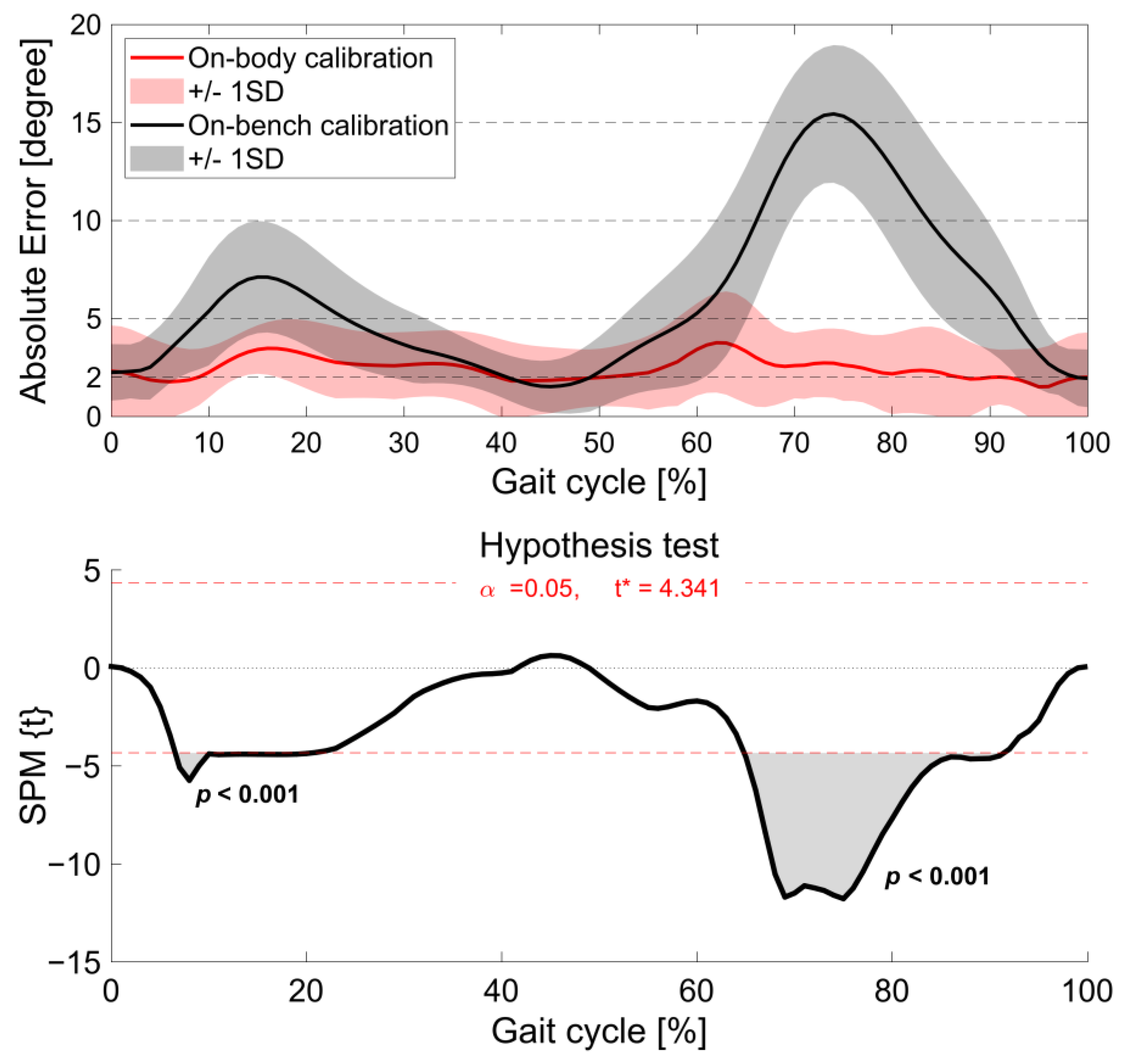
3.2. Absolute Errors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shafrin, J.; Sullivan, J.; Goldman, D.P.; Gill, T.M. The association between observed mobility and quality of life in the near elderly. PLoS ONE 2017, 12, e0182920. [Google Scholar] [CrossRef]
- Davis, J.C.; Bryan, S.; Li, L.C.; Best, J.R.; Hsu, C.L.; Gomez, C.; Vertes, K.A.; Liu-Ambrose, T. Mobility and cognition are associated with wellbeing and health related quality of life among older adults: A cross-sectional analysis of the Vancouver Falls Prevention Cohort. BMC Geriatr. 2015, 15, 75. [Google Scholar] [CrossRef]
- Yoshimura, N.; Iidaka, T.; Horii, C.; Mure, K.; Muraki, S.; Oka, H.; Kawaguchi, H.; Akune, T.; Ishibashi, H.; Ohe, T.; et al. Epidemiology of locomotive syndrome using updated clinical decision limits: 6-year follow-ups of the ROAD study. J. Bone Miner. Metab. 2022, 40, 623–635. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, W.; Kobayashi, Y.; Inoue, K.; Horie, M.; Yoshihara, K.; Ooie, T. Kinematic characteristics during gait in frail older women identified by principal component analysis. Sci. Rep. 2022, 12, 1676. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, A.; Katsuhira, J.; Watanabe, M.; Fujii, T.; Yoshimoto, T.; Oka, H.; Matsudaira, K. Relationship between the locomotive syndrome and kinetic and kinematic parameters during static standing and level walking. Gait Posture 2022, 93, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Ishida, T.; Kataoka, Y.; Takeda, R.; Tadano, S.; Suzuki, T.; Nakamura, K.; Nakata, A.; Osuka, S.; Yamada, S.; et al. Evaluation of gait characteristics in subjects with locomotive syndrome using wearable gait sensors. BMC Musculoskelet. Disord. 2022, 23, 457. [Google Scholar] [CrossRef] [PubMed]
- Ino, T.; Samukawa, M.; Ishida, T.; Wada, N.; Koshino, Y.; Kasahara, S.; Tohyama, H. Validity of AI-Based Gait Analysis for Simultaneous Measurement of Bilateral Lower Limb Kinematics Using a Single Video Camera. Sensors 2023, 23, 9799. [Google Scholar] [CrossRef] [PubMed]
- Stenum, J.; Rossi, C.; Roemmich, R.T. Two-dimensional video-based analysis of human gait using pose estimation. PLoS Comput. Biol. 2021, 17, e1008935. [Google Scholar] [CrossRef]
- Ota, M.; Tateuchi, H.; Hashiguchi, T.; Ichihashi, N. Verification of validity of gait analysis systems during treadmill walking and running using human pose tracking algorithm. Gait Posture 2021, 85, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Zago, M.; Luzzago, M.; Marangoni, T.; De Cecco, M.; Tarabini, M.; Galli, M. 3D Tracking of Human Motion Using Visual Skeletonization and Stereoscopic Vision. Front. Bioeng. Biotechnol. 2020, 8, 181. [Google Scholar] [CrossRef]
- Viswakumar, A.; Rajagopalan, V.; Ray, T.; Gottipati, P.; Parimi, C. Development of a Robust, Simple, and Affordable Human Gait Analysis System Using Bottom-Up Pose Estimation With a Smartphone Camera. Front. Physiol. 2021, 12, 784865. [Google Scholar] [CrossRef]
- Brodie, M.A.D.; Coppens, M.J.M.; Lord, S.R.; Lovell, N.H.; Gschwind, Y.J.; Redmond, S.J.; Del Rosario, M.B.; Wang, K.; Sturnieks, D.L.; Persiani, M.; et al. Wearable pendant device monitoring using new wavelet-based methods shows daily life and laboratory gaits are different. Med. Biol. Eng. Comput. 2016, 54, 663–674. [Google Scholar] [CrossRef]
- Picerno, P.; Iosa, M.; D’Souza, C.; Benedetti, M.G.; Paolucci, S.; Morone, G. Wearable inertial sensors for human movement analysis: A five-year update. Expert Rev. Med. Devices 2021, 18, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Trojaniello, D.; Ravaschio, A.; Hausdorff, J.M.; Cereatti, A. Comparative assessment of different methods for the estimation of gait temporal parameters using a single inertial sensor: Application to elderly, post-stroke, Parkinson’s disease and Huntington’s disease subjects. Gait Posture 2015, 42, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Favre, J.; Jolles, B.M.; Aissaoui, R.; Aminian, K. Ambulatory measurement of 3D knee joint angle. J. Biomech. 2008, 41, 1029–1035. [Google Scholar] [CrossRef]
- Takeda, R.; Tadano, S.; Natorigawa, A.; Todoh, M.; Yoshinari, S. Gait posture estimation using wearable acceleration and gyro sensors. J. Biomech. 2009, 42, 2486–2494. [Google Scholar] [CrossRef] [PubMed]
- Nazarahari, M.; Noamani, A.; Ahmadian, N.; Rouhani, H. Sensor-to-body calibration procedure for clinical motion analysis of lower limb using magnetic and inertial measurement units. J. Biomech. 2019, 85, 224–229. [Google Scholar] [CrossRef]
- Shull, P.B.; Jirattigalachote, W.; Hunt, M.A.; Cutkosky, M.R.; Delp, S.L. Quantified self and human movement: A review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture 2014, 40, 11–19. [Google Scholar] [CrossRef]
- Takeda, R.; Lisco, G.; Fujisawa, T.; Gastaldi, L.; Tohyama, H.; Tadano, S. Drift removal for improving the accuracy of gait parameters using wearable sensor systems. Sensors 2014, 14, 23230–23247. [Google Scholar] [CrossRef]
- Kettelkamp, D.B.; Johnson, R.J.; Smidt, G.L.; Chao, E.Y.; Walker, M. An electrogoniometric study of knee motion in normal gait. J. Bone Joint Surg. Am. 1970, 52, 775–790. [Google Scholar] [CrossRef]
- Rivera, B.; Cano, C.; Luis, I.; Elias, D.A. A 3D-Printed Knee Wearable Goniometer with a Mobile-App Interface for Measuring Range of Motion and Monitoring Activities. Sensors 2022, 22, 763. [Google Scholar] [CrossRef]
- Ishida, T.; Samukawa, M. Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle. Sensors 2023, 23, 3266. [Google Scholar] [CrossRef]
- de Oliveira Sato, T.; Hansson, G.-Å.; Coury, H.J.C.G. Goniometer crosstalk compensation for knee joint applications. Sensors 2010, 10, 9994–10005. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.A.R.; Pinskerova, V. The movement of the normal tibio-femoral joint. J. Biomech. 2005, 38, 197–208. [Google Scholar] [CrossRef]
- Dyrby, C.O.; Andriacchi, T.P. Secondary motions of the knee during weight bearing and non-weight bearing activities. J. Orthop. Res. 2004, 22, 794–800. [Google Scholar] [CrossRef]
- Shuai, Z.; Dong, A.; Liu, H.; Cui, Y. Reliability and Validity of an Inertial Measurement System to Quantify Lower Extremity Joint Angle in Functional Movements. Sensors 2022, 22, 863. [Google Scholar] [CrossRef]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef]
- Bessone, V.; Höschele, N.; Schwirtz, A.; Seiberl, W. Validation of a new inertial measurement unit system based on different dynamic movements for future in-field applications. Sports Biomech. 2022, 21, 685–700. [Google Scholar] [CrossRef] [PubMed]
- Fleiss, J.L. The Design and Analysis of Clinical Experiments; Wiley: Hoboken, NJ, USA, 1986. [Google Scholar]
- Asano, T.; Akagi, M.; Nakamura, T. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: In vivo analysis using a biplanar image-matching technique. J. Arthroplast. 2005, 20, 1060–1067. [Google Scholar] [CrossRef]
- Ishida, T.; Samukawa, M.; Endo, D.; Kasahara, S.; Tohyama, H. Effects of Changing Center of Pressure Position on Knee and Ankle Extensor Moments During Double-Leg Squatting. J. Sports Sci. Med. 2022, 21, 341–346. [Google Scholar] [CrossRef]
- Bell, A.L.; Brand, R.A.; Pedersen, D.R. Prediction of hip joint centre location from external landmarks. Hum. Mov. Sci. 1989, 8, 3–16. [Google Scholar] [CrossRef]
- Grood, E.S.; Suntay, W.J. A joint coordinate system for the clinical description of three-dimensional motions: Application to the knee. J. Biomech. Eng. 1983, 105, 136–144. [Google Scholar] [CrossRef]
- Cole, G.K.; Nigg, B.M.; Ronsky, J.L.; Yeadon, M.R. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: A standardization proposal. J. Biomech. Eng. 1993, 115, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Cutti, A.G.; Cappello, A. A new formulation of the coefficient of multiple correlation to assess the similarity of waveforms measured synchronously by different motion analysis protocols. Gait Posture 2010, 31, 540–542. [Google Scholar] [CrossRef] [PubMed]
- Pataky, T.C.; Vanrenterghem, J.; Robinson, M.A. Zero- vs. one-dimensional, parametric vs. non-parametric, and confidence interval vs. hypothesis testing procedures in one-dimensional biomechanical trajectory analysis. J. Biomech. 2015, 48, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Cutti, A.G.; Garofalo, P.; Raggi, M.; Heijboer, M.; Cappello, A.; Davalli, A. First in vivo assessment of “Outwalk”: A novel protocol for clinical gait analysis based on inertial and magnetic sensors. Med. Biol. Eng. Comput. 2010, 48, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Hart, H.F.; Culvenor, A.G.; Collins, N.J.; Ackland, D.C.; Cowan, S.M.; Machotka, Z.; Crossley, K.M. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 597–612. [Google Scholar] [CrossRef]
- Mills, K.; Hunt, M.A.; Ferber, R. Biomechanical deviations during level walking associated with knee osteoarthritis: A systematic review and meta-analysis. Arthritis Care Res. 2013, 65, 1643–1665. [Google Scholar] [CrossRef]
- Winter, D.A. Foot trajectory in human gait: A precise and multifactorial motor control task. Phys. Ther. 1992, 72, 45–53; discussion 54–56. [Google Scholar] [CrossRef] [PubMed]
- Ino, T.; Ohkoshi, Y.; Maeda, T.; Kawakami, K.; Suzuki, S.; Tohyama, H. Side-to-side differences of three-dimensional knee kinematics during walking by normal subjects. J. Phys. Ther. Sci. 2015, 27, 1803–1807. [Google Scholar] [CrossRef]
- Huddleston, J.; Alaiti, A.; Goldvasser, D.; Scarborough, D.; Freiberg, A.; Rubash, H.; Malchau, H.; Harris, W.; Krebs, D. Ambulatory measurement of knee motion and physical activity: Preliminary evaluation of a smart activity monitor. J. Neuroeng. Rehabil. 2006, 3, 21. [Google Scholar] [CrossRef] [PubMed]
- Chiba, H.; Ebihara, S.; Tomita, N.; Sasaki, H.; Butler, J.P. Differential gait kinematics between fallers and non-fallers in community-dwelling elderly people. Geriatr. Gerontol. Int. 2005, 5, 127–134. [Google Scholar] [CrossRef]
- Barrett, R.S.; Mills, P.M.; Begg, R.K. A systematic review of the effect of ageing and falls history on minimum foot clearance characteristics during level walking. Gait Posture 2010, 32, 429–435. [Google Scholar] [CrossRef]

| Advantage | Disadvantage |
|---|---|
Easy to use
| Less accuracy
|
| Real-time visual biofeedback | Single or double axes (no 3D analysis) |
| No recording volume limitations | Mainly used for knee joint |
| Long time use (low power consumption, no drift) | No positional data |
| Less expensive (or cheap) | Requires attachment for sensors to body |
| Coefficient of Multiple Correlations | ||
|---|---|---|
| Participant | On-Body Calibration | On-Bench Calibration |
| A | 0.990 | 0.956 |
| B | 0.991 | 0.957 |
| C | 0.996 | 0.983 |
| D | 0.977 | 0.905 |
| E | 0.998 | 0.949 |
| F | 0.994 | 0.972 |
| G | 0.997 | 0.949 |
| H | 0.996 | 0.916 |
| I | 0.997 | 0.992 |
| J | 0.998 | 0.983 |
| Mean | 0.993 (0.007) | 0.956 (0.029) |
| Mean Absolute Errors (SD) [min, max] | ||
|---|---|---|
| Participant | On-Body Calibration | On-Bench Calibration |
| A | 2.5 (1.3) [0.03, 4.7] | 6.4 (4.1) [0.9, 15.5] |
| B | 2.9 (2.1) [0.02, 7.5] | 6.2 (4.0) [0.1, 14.7] |
| C | 2.2 (1.3) [0.07, 5.2] | 3.7 (3.5) [0.001, 12.7] |
| D | 6.2 (1.6) [3.2, 9.5] | 9.9 (5.9) [1.5, 21.3] |
| E | 1.4 (1.1) [0.01, 4.9] | 6.3 (5.4) [0.1, 14.4] |
| F | 2.5 (1.6) [0.03, 6.9] | 4.9 (3.9) [0. 2, 14.4) |
| G | 1.9 (1.3) [0.004, 4.8] | 7.6 (4.6) [2.2, 17.4] |
| H | 1.7 (1.3) [0.02, 4.7] | 8.3 (5.2) [1.8, 19.2] |
| I | 2.0 (1.2) [0.06, 4.4] | 2.7 (2.4) [0.01, 9.5] |
| J | 1.1 (0.8) [0.01, 3.3] | 3.5 (3.4) [0.001, 11.9] |
| Mean | 2.4 (1.4) | 6.0 (4.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishida, T.; Samukawa, M. The Difference in the Assessment of Knee Extension/Flexion Angles during Gait between Two Calibration Methods for Wearable Goniometer Sensors. Sensors 2024, 24, 2092. https://doi.org/10.3390/s24072092
Ishida T, Samukawa M. The Difference in the Assessment of Knee Extension/Flexion Angles during Gait between Two Calibration Methods for Wearable Goniometer Sensors. Sensors. 2024; 24(7):2092. https://doi.org/10.3390/s24072092
Chicago/Turabian StyleIshida, Tomoya, and Mina Samukawa. 2024. "The Difference in the Assessment of Knee Extension/Flexion Angles during Gait between Two Calibration Methods for Wearable Goniometer Sensors" Sensors 24, no. 7: 2092. https://doi.org/10.3390/s24072092
APA StyleIshida, T., & Samukawa, M. (2024). The Difference in the Assessment of Knee Extension/Flexion Angles during Gait between Two Calibration Methods for Wearable Goniometer Sensors. Sensors, 24(7), 2092. https://doi.org/10.3390/s24072092






