Exploring Technology Acceptance of Healthcare Devices: The Moderating Role of Device Type and Generation
Abstract
1. Introduction
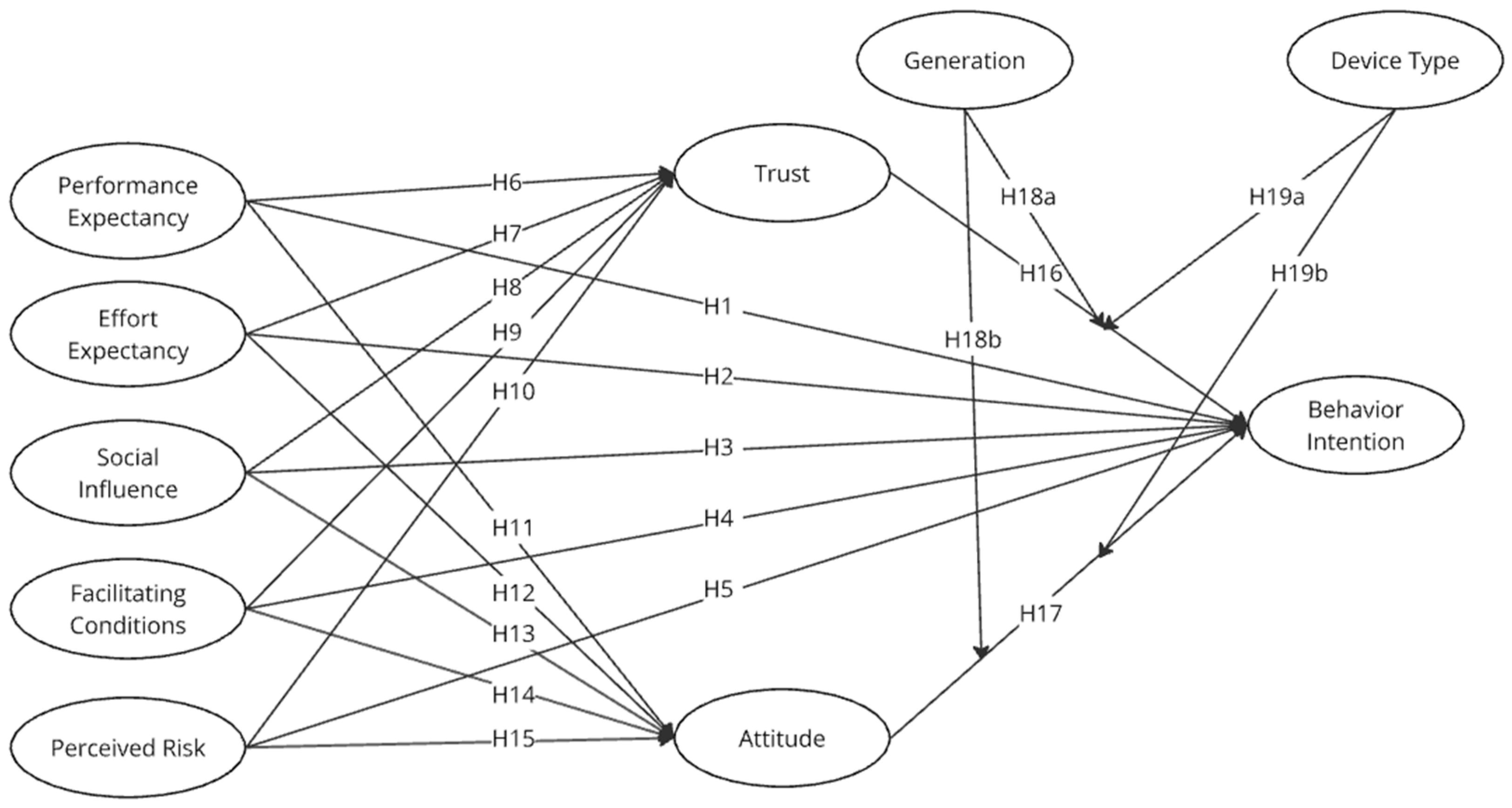
2. Literature Review
2.1. Technology Acceptance of Healthcare Devices
2.2. Trust
2.3. Attitude
2.4. Perceived Risk
2.5. The Role of Generation in Technology Acceptance
2.6. The Role of Device Types in Technology Acceptance
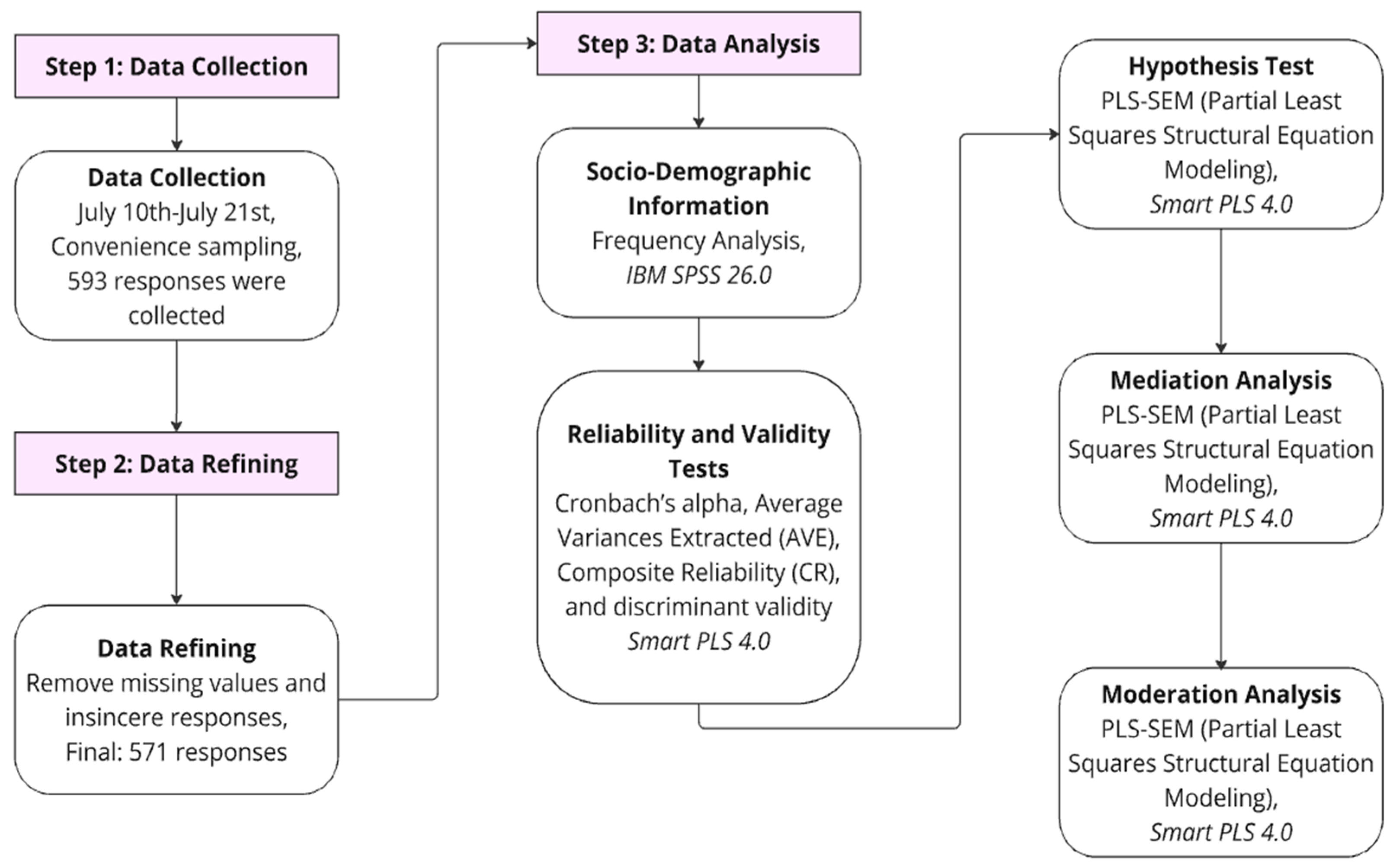
3. Methodology
4. Results
4.1. Demographic Information
4.2. Reliability and Validity Test
4.3. Hypotheses Testing Results
4.4. Mediation Effect Results
4.5. Moderation Effect Results
5. Discussion and Implications
5.1. Discussion
5.2. Theoretical Implications
5.3. Practical Implications
5.4. Limitations and Future Studies
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dal Mas, F.; Massaro, M.; Rippa, P.; Secundo, G. The Challenges of Digital Transformation in Healthcare: An Interdisciplinary Literature Review, Framework, and Future Research Agenda. Technovation 2023, 123, 102716. [Google Scholar] [CrossRef]
- Greengard, S. The Internet of Things; Revised and Update Edition; MIT Press: Cambridge, MA, USA, 2021; 296p. [Google Scholar]
- Zeadally, S.; Bello, O. Harnessing the Power of Internet of Things Based Connectivity to Improve Healthcare. Internet Things 2021, 14, 1–14. [Google Scholar] [CrossRef]
- Healthcare IoT—Worldwide|Statista Market Forecast. Available online: https://www.statista.com/outlook/tmo/internet-of-things/healthcare-iot/worldwide (accessed on 3 September 2024).
- Jamil, F.; Ahmad, S.; Iqbal, N.; Kim, D.H. Towards a Remote Monitoring of Patient Vital Signs Based on IoT-Based Blockchain Integrity Management Platforms in Smart Hospitals. Sensors 2020, 20, 2195. [Google Scholar] [CrossRef]
- Deep, S.; Zheng, X.; Jolfaei, A.; Yu, D.; Ostovari, P.; Kashif Bashir, A. A Survey of Security and Privacy Issues in the Internet of Things from the Layered Context. Trans. Emerg. Telecommun. Technol. 2022, 33, e3935. [Google Scholar] [CrossRef]
- Ullah, M.; Hamayun, S.; Wahab, A.; Khan, S.U.; Qayum, M.; Ullah, A.; Rehman, M.U.; Mehreen, A.; Awan, U.A.; Naeem, M. Smart Technologies Used as Smart Tools in the Management of Cardiovascular Disease and Their Future Perspective. Curr. Probl. Cardiol. 2023, 48, 101922. [Google Scholar] [CrossRef]
- Wu, T.; Wu, F.; Qiu, C.; Redoute, J.M.; Yuce, M.R. A Rigid-Flex Wearable Health Monitoring Sensor Patch for IoT-Connected Healthcare Applications. IEEE Internet Things J. 2020, 7, 6932–6945. [Google Scholar] [CrossRef]
- Rashid, N.; Mortlock, T.; Al Faruque, M.A. Stress Detection Using Context-Aware Sensor Fusion from Wearable Devices. IEEE Internet Things J. 2023, 10, 14114–14127. [Google Scholar] [CrossRef]
- Pateraki, M.; Fysarakis, K.; Sakkalis, V.; Spanoudakis, G.; Varlamis, I.; Maniadakis, M.; Lourakis, M.; Ioannidis, S.; Cummins, N.; Schuller, B.; et al. Biosensors and Internet of Things in Smart Healthcare Applications: Challenges and Opportunities. Wearable Implant. Med. Devices 2020, 7, 25–53. [Google Scholar] [CrossRef]
- Pradhan, B.; Bhattacharyya, S.; Pal, K. IoT-Based Applications in Healthcare Devices. J. Healthc. Eng. 2021, 2021, 1–18. [Google Scholar] [CrossRef]
- Vasudevan, V.; Mohan, U.S.; Gounder, M.S. AI-Powered Internet of Medical Things for Monitoring Elderly Adults in Independent Living Environments. In Smart Healthcare Systems; Bhambri, P., Rashmi, S., Tran, T.A., Eds.; CRC Press: Boca Raton, FL, USA, 2024; pp. 289–303. [Google Scholar] [CrossRef]
- Dhagarra, D.; Goswami, M.; Kumar, G. Impact of Trust and Privacy Concerns on Technology Acceptance in Healthcare: An Indian Perspective. Int. J. Med. Inform. 2020, 141, 104164. [Google Scholar] [CrossRef]
- Liu, K.; Tao, D. The Roles of Trust, Personalization, Loss of Privacy, and Anthropomorphism in Public Acceptance of Smart Healthcare Services. Comput. Hum. Behav. 2022, 127, 107026. [Google Scholar] [CrossRef]
- Arfi, W.B.; Nasr, I.B.; Kondrateva, G.; Hikkerova, L. The Role of Trust in Intention to Use the IoT in EHealth: Application of the Modified UTAUT in a Consumer Context. Technol. Forecast. Soc. Change 2021, 167, 120688. [Google Scholar] [CrossRef]
- Alraja, M. Frontline Healthcare Providers’ Behavioural Intention to Internet of Things (IoT)-Enabled Healthcare Applications: A Gender-Based, Cross-Generational Study. Technol. Forecast. Soc. Change 2022, 174, 121256. [Google Scholar] [CrossRef]
- Ben Arfi, W.; Ben Nasr, I.; Khvatova, T.; Ben Zaied, Y. Understanding Acceptance of EHealthcare by IoT Natives and IoT Immigrants: An Integrated Model of UTAUT, Perceived Risk, and Financial Cost. Technol. Forecast. Soc. Change 2021, 163, 120437. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Al-rawashdeh, M.; Keikhosrokiani, P.; Belaton, B.; Alawida, M.; Zwiri, A. IoT Adoption and Application for Smart Healthcare: A Systematic Review. Sensors 2022, 22, 5377. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Fishbein, M.; Ajzen, I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research; Addison-Wesley: Reading, MA, USA, 1977; Volume 10, pp. 130–132. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. Extrinsic and Intrinsic Motivation to Use Computers in the Workplace. J. Appl. Soc. Psychol. 1992, 22, 1111–1132. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P. Assessing IT Usage: The Role of Prior Experience. MIS Q. 1995, 19, 561–570. [Google Scholar] [CrossRef]
- Thompson, R.L.; Higgins, C.A.; Howell, J.M. Personal Computing: Toward a Conceptual Model of Utilization. MIS Q. 1991, 15, 125–143. [Google Scholar] [CrossRef]
- Moore, G.C.; Benbasat, I. Development of an Instrument to Measure the Perceptions of Adopting an Information Technology Innovation. Inf. Syst. Res. 1991, 2, 192–222. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory. In The Health Psychology Reader; Chapter 6; Prentice-Hall: Hoboken, NJ, USA, 1986; pp. 94–106. [Google Scholar]
- Jena, R.K. Exploring Antecedents of Peoples’ Intentions to Use Smart Services in a Smart City Environment: An Extended UTAUT Model. J. Inf. Syst. 2022, 36, 133–149. [Google Scholar] [CrossRef]
- Popova, Y.; Zagulova, D. UTAUT Model for Smart City Concept Implementation: Use of Web Applications by Residents for Everyday Operations. Informatics 2022, 9, 27. [Google Scholar] [CrossRef]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding Consumer Acceptance of Healthcare Wearable Devices: An Integrated Model of UTAUT and TTF. Int. J. Med. Inform. 2020, 139, 104156. [Google Scholar] [CrossRef]
- Kang, H.J.; Han, J.; Kwon, G.H. The Acceptance Behavior of Smart Home Health Care Services in South Korea: An Integrated Model of UTAUT and TTF. Int. J. Environ. Res. Public Health 2022, 19, 13279. [Google Scholar] [CrossRef]
- Jim, J.R.; Hosain, M.T.; Mridha, M.F.; Kabir, M.M.; Shin, J. Toward Trustworthy Metaverse: Advancements and Challenges. IEEE Access 2023, 11, 118318–118347. [Google Scholar] [CrossRef]
- Makovi, K.; Sargsyan, A.; Li, W.; Bonnefon, J.F.; Rahwan, T. Trust within Human-Machine Collectives Depends on the Perceived Consensus about Cooperative Norms. Nat. Commun. 2023, 14, 3108. [Google Scholar] [CrossRef]
- Li, Q.; Zhang, X.; Seifert, J.P.; Zhong, H. Secure Mobile Payment via Trusted Computing. In Proceedings of the Third Asia-Pacific Trusted Infrastructure Technologies Conference, Wuhan, China, 21 November 2008. [Google Scholar] [CrossRef]
- Fotia, L.; Delicato, F.; Fortino, G. Trust in Edge-Based Internet of Things Architectures: State of the Art and Research Challenges. ACM Comput. Surv. 2023, 55, 1–34. [Google Scholar] [CrossRef]
- Namahoot, K.S.; Jantasri, V. Integration of UTAUT Model in Thailand Cashless Payment System Adoption: The Mediating Role of Perceived Risk and Trust. J. Sci. Technol. Policy Manag. 2023, 14, 634–658. [Google Scholar] [CrossRef]
- Li, C.; Wang, J.; Wang, S.; Zhang, Y. A Review of IoT Applications in Healthcare. Neurocomputing 2023, 565, 127017. [Google Scholar] [CrossRef]
- Jaime, F.J.; Muñoz, A.; Rodríguez-Gómez, F.; Jerez-Calero, A. Strengthening Privacy and Data Security in Biomedical Microelectromechanical Systems by IoT Communication Security and Protection in Smart Healthcare. Sensors 2023, 23, 8944. [Google Scholar] [CrossRef] [PubMed]
- Habbal, A.; Ali, M.K.; Abuzaraida, M.A. Artificial Intelligence Trust, Risk and Security Management (AI TRiSM): Frameworks, Applications, Challenges and Future Research Directions. Expert Syst. Appl. 2024, 240, 122442. [Google Scholar] [CrossRef]
- Pentikäinen, K. Attitudes towards English Accents Title: Attitudes towards English Accents: A Comparison of Finnish Lower and Upper Secondary Students. Commun. Monogr. 2023, 84, 385–405. [Google Scholar]
- Wang, J.; Kim, H.-S. Visualizing the Landscape of Home IoT Research: A Bibliometric Analysis Using VOSviewer. Sensors 2023, 23, 3086. [Google Scholar] [CrossRef]
- Almazroi, A.A. An Empirical Investigation of Factors Influencing the Adoption of Internet of Things Services by End-Users. Arab. J. Sci. Eng. 2023, 48, 1641–1659. [Google Scholar] [CrossRef]
- Zin, K.S.L.T.; Kim, S.; Kim, H.-S.; Feyissa, I.F. A Study on Technology Acceptance of Digital Healthcare among Older Korean Adults Using Extended Tam (Extended Technology Acceptance Model). Adm. Sci. 2023, 13, 42. [Google Scholar] [CrossRef]
- Rahman, M.; Sciara, G.C. Travel Attitudes, the Built Environment and Travel Behavior Relationships: Causal Insights from Social Psychology Theories. Transp. Policy 2022, 123, 44–54. [Google Scholar] [CrossRef]
- Fishman, J.; Yang, C.; Mandell, D. Attitude Theory and Measurement in Implementation Science: A Secondary Review of Empirical Studies and Opportunities for Advancement. Implement. Sci. 2021, 16, 87. [Google Scholar] [CrossRef]
- Likert, R. A Technique for the Measurement of Attitudes. Arch. Psychol. 1932, 22, 55. [Google Scholar]
- Widyanto, H.A.; Kusumawardani, K.A.; Yohanes, H. Safety First: Extending UTAUT to Better Predict Mobile Payment Adoption by Incorporating Perceived Security, Perceived Risk and Trust. J. Sci. Technol. Policy Manag. 2022, 13, 952–973. [Google Scholar] [CrossRef]
- Featherman, M.S.; Pavlou, P.A. Predicting E-Services Adoption: A Perceived Risk Facets Perspective. Int. J. Hum. Comput. Stud. 2003, 59, 451–474. [Google Scholar] [CrossRef]
- Pentz, C.D.; du Preez, R.; Swiegers, L. To Bu(Y) or Not to Bu(Y): Perceived Risk Barriers to Online Shopping among South African Generation Y Consumers. Cogent Bus. Manag. 2020, 7, 1827813. [Google Scholar] [CrossRef]
- Dash, A.; Sahoo, A.K. Exploring Patient’s Intention towards e-Health Consultation Using an Extended UTAUT Model. J. Enabling Technol. 2022, 16, 266–279. [Google Scholar] [CrossRef]
- Gupta, S.; Kamboj, S.; Bag, S. Role of Risks in the Development of Responsible Artificial Intelligence in the Digital Healthcare Domain. Inf. Syst. Front. 2023, 25, 2257–2274. [Google Scholar] [CrossRef]
- Sugiarto, B.A.T.; Kahmad, D.; Huriani, Y. Gen Zers’ Stances on The Religion Role in Human Salvation | Sugiarto | Jaqfi: Jurnal Aqidah Dan Filsafat Islam. Jaqfi J. Aqidah Filsafat Islam 2022, 7, 135–152. [Google Scholar] [CrossRef]
- Lissitsa, S.; Laor, T. Baby Boomers, Generation X and Generation Y: Identifying Generational Differences in Effects of Personality Traits in on-Demand Radio Use. Technol. Soc. 2021, 64, 101526. [Google Scholar] [CrossRef]
- Determann, L. Healthy Data Protection. Michigan Technol. Law Rev. 2019, 26, 229–278. [Google Scholar] [CrossRef]
- Wang, J.; Fan, S.; Alexandridis, A.; Han, K.; Jeon, G.; Zilic, Z.; Pang, Y. A Multistage Blockchain-Based Secure and Trustworthy Smart Healthcare System Using ECG Characteristic. IEEE Internet Things Mag. 2021, 4, 48–58. [Google Scholar] [CrossRef]
- Agárdi, I.; Alt, M.A. Do Digital Natives Use Mobile Payment Differently than Digital Immigrants? A Comparative Study between Generation X and Z. Electron. Commer. Res. 2022, 24, 1463–1490. [Google Scholar] [CrossRef]
- Bhalla, R.; Tiwari, P.; Chowdhary, N. Digital Natives Leading the World: Paragons and Values of Generation Z. In Generation Z Marketing and Management in Tourism and Hospitality: The Future of the Industry, 1st ed.; Stylos, N., Rahimi, R., Okumus, B., Williams, S., Eds.; Springer International Publishing: Cham, Switzerland, 2021; Volume 1, pp. 3–23. [Google Scholar] [CrossRef]
- Babu, A.S.; Yashika, K.P.; Nishaan Kushalappa, K.S.; Adiga, A.; Raj, S.B.; Mrudula, N.; Meghana, S.; Chandana, K.B.; Jayachandran, R. NeuroPredict: A Comprehensive Approach for Alzheimer’s Disease Prediction and Development of a Medical Assisting Kit. In Proceedings of the 2023 International Conference on Recent Advances in Science and Engineering Technology (ICRASET), B G Nagara, India, 23–24 November 2023. [Google Scholar] [CrossRef]
- Mohan, B.; Virender; Gupta, R.K.; Pombeiro AJ, L.; Solovev, A.A.; Singh, G. Advancements in Metal-Organic, Enzymatic, and Nanocomposite Platforms for Wireless Sensors of the Next Generation. Adv. Funct. Mater. 2024, 1, 2405231. [Google Scholar] [CrossRef]
- Natarajan, T.; Balasubramanian, S.A.; Kasilingam, D.L. The Moderating Role of Device Type and Age of Users on the Intention to Use Mobile Shopping Applications. Technol. Soc. 2018, 53, 79–90. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult GT, M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. An Introduction to Structural Equation Modeling. In Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2021; Volume 1, pp. 1–29. [Google Scholar] [CrossRef]
- Hulland, J. Use of Partial Least Squares (PLS) in Strategic Management Research: A Review of Four Recent Studies. Strateg. Manag. J. 1999, 20, 195–204. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y. On the Evaluation of Structural Equation Models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Kim, T.H.; Kim, H.-S. Delivery App Understanding and Acceptance among Food Tech Customers Using the Modified Technology Acceptance Model. J. Tour. Sci. 2016, 40, 127–144. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Rana, N.P.; Jeyaraj, A.; Clement, M.; Williams, M.D. Re-Examining the Unified Theory of Acceptance and Use of Technology (UTAUT): Towards a Revised Theoretical Model. Inf. Syst. Front. 2019, 21, 719–734. [Google Scholar] [CrossRef]
- Chawla, D.; Joshi, H. Role of Mediator in Examining the Influence of Antecedents of Mobile Wallet Adoption on Attitude and Intention. Glob. Bus. Rev. 2023, 24, 609–625. [Google Scholar] [CrossRef]
- Pavlou, P.A. Consumer Acceptance of Electronic Commerce: Integrating Trust and Risk with the Technology Acceptance Model. Int. J. Electron. Commer. 2003, 7, 101–134. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Kim, J. An Extended Technology Acceptance Model in Behavioral Intention toward Hotel Tablet Apps with Moderating Effects of Gender and Age. Int. J. Contemp. Hosp. Manag. 2016, 28, 1535–1553. [Google Scholar] [CrossRef]
- Çera, G.; Pagria, I.; Khan, K.A.; Muaremi, L. Mobile Banking Usage and Gamification: The Moderating Effect of Generational Cohorts. J. Syst. Inf. Technol. 2020, 22, 243–263. [Google Scholar] [CrossRef]
- Ho, D.H.; Kim, S.; Lee, B.-H.; Jeon, B.; Kim, H.-S. Exploring User Perceptions of a Radar Sensor-Based Smart Healthcare Device for Heart Rate and Breathing Rate Monitoring through Interviews. J. Ind. Innov. 2024, 40, 82–95. [Google Scholar] [CrossRef]
- Shin, J.; Kim, H.-S. Understanding Consumption Behavior on Mobile Grocery Shopping: An Application of the Extended Unfied Theory of Acceptance and Use of Technology (UTAUT2). J. Ind. Innov. 2024, 40, 1–13. [Google Scholar] [CrossRef]
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Gender | Male | 287 | 49.6 |
| Female | 292 | 50.4 | |
| Generation | Under 20 | 17 | 2.9 |
| 20s | 303 | 52.4 | |
| 30s | 189 | 32.6 | |
| Over 40 | 70 | 12.1 | |
| Nationality | Korean | 17 | 2.9 |
| Indonesian | 302 | 52.2 | |
| Vietnamese | 68 | 11.7 | |
| Chinese | 190 | 32.8 | |
| Others | 2 | 0.4 | |
| Education Level | High school graduate and below | 50 | 8.6 |
| 3-year college | 86 | 14.9 | |
| Bachelor’s degree | 352 | 60.8 | |
| Postgraduate | 91 | 15.7 | |
| Monthly Income | Less than USD 1000 | 130 | 22.5 |
| USD 1000~1999 | 279 | 48.1 | |
| USD 2000~2999 | 130 | 22.5 | |
| Over USD 3000 | 40 | 6.9 | |
| Marital Status | Not married | 229 | 39.5 |
| Married | 250 | 43.2 | |
| Divorced | 100 | 17.3 | |
| Household # | 1 (living alone) | 120 | 20.7 |
| 2 | 143 | 24.7 | |
| 3 | 156 | 27.0 | |
| More than 4 | 160 | 27.6 |
| Constructs | Items | Factor Loading | CR | AVE | Cronbach’s Alpha |
|---|---|---|---|---|---|
| Performance Expectancy | PE1 | 0.882 | 0.821 | 0.732 | 0.816 |
| PE2 | 0.818 | ||||
| PE3 | 0.865 | ||||
| Effort Expectancy | EE1 | 0.897 | 0.831 | 0.747 | 0.830 |
| EE2 | 0.856 | ||||
| EE3 | 0.838 | ||||
| Social Influence | SI1 | 0.862 | 0.793 | 0.704 | 0.790 |
| SI2 | 0.808 | ||||
| SI3 | 0.847 | ||||
| Facilitating Conditions | FC1 | 0.872 | 0.792 | 0.704 | 0.789 |
| FC2 | 0.817 | ||||
| FC3 | 0.826 | ||||
| Perceived Risk | CI1 | 0.810 | 0.777 | 0.688 | 0.774 |
| CI2 | 0.835 | ||||
| CI3 | 0.843 | ||||
| Trust | T1 | 0.868 | 0.827 | 0.656 | 0.824 |
| T2 | 0.778 | ||||
| T3 | 0.783 | ||||
| T4 | 0.806 | ||||
| Attitude | Att1 | 0.884 | 0.782 | 0.695 | 0.779 |
| Att2 | 0.765 | ||||
| Att3 | 0.848 | ||||
| Behavioral Intention | BI1 | 0.855 | 0.829 | 0.657 | 0.825 |
| BI2 | 0.760 | ||||
| BI3 | 0.789 | ||||
| BI4 | 0.835 |
| Att | BI | EE | FC | PE | PR | SI | T | |
|---|---|---|---|---|---|---|---|---|
| Att | 0.834 | |||||||
| BI | 0.791 | 0.811 | ||||||
| EE | 0.733 | 0.735 | 0.864 | |||||
| FC | 0.753 | 0.779 | 0.771 | 0.839 | ||||
| PE | 0.735 | 0.743 | 0.769 | 0.753 | 0.855 | |||
| PR | 0.704 | 0.764 | 0.678 | 0.719 | 0.680 | 0.829 | ||
| SI | 0.725 | 0.793 | 0.716 | 0.765 | 0.749 | 0.744 | 0.839 | |
| T | 0.795 | 0.799 | 0.761 | 0.789 | 0.777 | 0.728 | 0.779 | 0.810 |
| Path | Path Coefficient (β) | Standard Deviation | t-Value | p-Value | Result | |
|---|---|---|---|---|---|---|
| H1 | PE -> BI | 0.034 | 0.036 | 0.964 | 0.335 | Not Supported |
| H2 | EE -> BI | 0.050 | 0.036 | 1.408 | 0.159 | Not Supported |
| H3 | SI -> BI | 0.194 | 0.045 | 4.350 | <0.001 | Supported |
| H4 | FC -> BI | 0.129 | 0.033 | 3.848 | <0.001 | Supported |
| H5 | PR -> BI | 0.169 | 0.038 | 4.450 | <0.001 | Supported |
| H6 | PE -> T | 0.220 | 0.037 | 5.971 | <0.001 | Supported |
| H7 | EE -> T | 0.164 | 0.037 | 4.466 | <0.001 | Supported |
| H8 | SI -> T | 0.215 | 0.038 | 5.613 | <0.001 | Supported |
| H9 | FC -> T | 0.232 | 0.038 | 6.029 | <0.001 | Supported |
| H10 | PR -> T | 0.141 | 0.035 | 3.969 | <0.001 | Supported |
| H11 | PE -> Att | 0.194 | 0.041 | 4.732 | <0.001 | Supported |
| H12 | EE -> Att | 0.189 | 0.038 | 4.982 | <0.001 | Supported |
| H13 | SI -> Att | 0.137 | 0.040 | 3.439 | <0.001 | Supported |
| H14 | FC -> Att | 0.228 | 0.037 | 6.211 | <0.001 | Supported |
| H15 | PR -> Att | 0.178 | 0.035 | 5.115 | <0.001 | Supported |
| H16 | Att -> BI | 0.312 | 0.049 | 6.296 | <0.001 | Supported |
| H17 | T -> BI | 0.100 | 0.049 | 2.036 | 0.042 | Supported |
| Paths | Total Effect | Direct Effect | Indirect Effect | 95% CI | Mediation Effect | |||
|---|---|---|---|---|---|---|---|---|
| β | β | p-Value | β | p-Value | Lower | Upper | ||
| PE -> Att -> BI | 0.083 | 0.034 | 0.335 | 0.060 | <0.001 | 0.031 | 0.095 | Full mediation effect |
| EE -> Att -> BI | 0.075 | 0.050 | 0.159 | 0.059 | <0.001 | 0.034 | 0.088 | Full mediation effect |
| SI -> Att -> BI | 0.064 | 0.194 | <0.001 | 0.043 | 0.003 | 0.018 | 0.073 | Partial mediation effect |
| FC -> Att -> BI | 0.094 | 0.129 | <0.001 | 0.071 | <0.001 | 0.041 | 0.105 | Partial mediation effect |
| PR -> Att -> BI | 0.070 | 0.169 | <0.001 | 0.055 | <0.001 | 0.029 | 0.085 | Partial mediation effect |
| PE -> T -> BI | 0.083 | 0.034 | 0.335 | 0.022 | 0.054 | 0.001 | 0.046 | No mediation effect |
| EE -> T -> BI | 0.094 | 0.050 | 0.159 | 0.016 | 0.063 | 0.001 | 0.036 | No mediation effect |
| SI -> T -> BI | 0.064 | 0.194 | <0.001 | 0.022 | 0.063 | 0.001 | 0.046 | No mediation effect |
| FC -> T -> BI | 0.094 | 0.129 | <0.001 | 0.023 | 0.055 | 0.001 | 0.048 | No mediation effect |
| PR -> T -> BI | 0.070 | 0.169 | <0.001 | 0.014 | 0.089 | 0.001 | 0.033 | No mediation effect |
| Paths | Standard Deviation | Standard Deviation | t-Value | p-Value | Result |
|---|---|---|---|---|---|
| Generation x Att -> BI | −0.297 | 0.059 | 4.984 | <0.001 | Supported |
| Generation x T -> BI | 0.285 | 0.062 | 4.609 | <0.001 | Supported |
| Device Type x Att -> BI | 0.052 | 0.065 | 0.803 | 0.422 | Not Supported |
| Device Type x T -> BI | −0.138 | 0.066 | 2.099 | 0.036 | Supported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Zhong, Y.; Wang, J.; Kim, H.-S. Exploring Technology Acceptance of Healthcare Devices: The Moderating Role of Device Type and Generation. Sensors 2024, 24, 7921. https://doi.org/10.3390/s24247921
Kim S, Zhong Y, Wang J, Kim H-S. Exploring Technology Acceptance of Healthcare Devices: The Moderating Role of Device Type and Generation. Sensors. 2024; 24(24):7921. https://doi.org/10.3390/s24247921
Chicago/Turabian StyleKim, Seieun, Yinai Zhong, Jue Wang, and Hak-Seon Kim. 2024. "Exploring Technology Acceptance of Healthcare Devices: The Moderating Role of Device Type and Generation" Sensors 24, no. 24: 7921. https://doi.org/10.3390/s24247921
APA StyleKim, S., Zhong, Y., Wang, J., & Kim, H.-S. (2024). Exploring Technology Acceptance of Healthcare Devices: The Moderating Role of Device Type and Generation. Sensors, 24(24), 7921. https://doi.org/10.3390/s24247921








