1. Introduction
From a functional perspective, mobility can be described as the “capacity to move from one location to another independently” [
1]. This capacity characterizes the activity and participation of an individual within the community and can be facilitated or hindered by a variety of factors, including physical abilities, cognitive function, psychosocial aspects, and the external environment in which individuals operate [
2]. In the field of geriatric research, the mobility of older adults within the community is an area of increasing interest, given its profound impact on quality of life. Mobility is not only essential for accessing basic services but also has a positive impact on the mental and physical health of older adults [
3].
The geographical area that an individual covers in their daily routine is referred to as “living space” [
4] and has been considered a marker of physical and cognitive performance in community-dwelling older adults, as it reflects their capacity to move and interact within their environment, making it a critical determinant regarding quality of life [
5]. It can be conceptualized as a series of zones radiating from the individual’s residence, representing varying degrees of mobility and independence. This concept provides a comprehensive measure of functional mobility over time, capturing not only the physical distance traveled but also the frequency and regularity of movement across various spaces [
6] and includes travel by various means of transport [
7]. The concept of living space originated in 1985 by May, Nayak, and Isaacs in their publication “The Living Space Diary: A Measure of Mobility in Older Adults at Home” [
8], wherein they segmented living space into five concentric zones, starting with the bedroom and progressively extending to larger areas, including the rest of the house, surrounding grounds such as gardens, neighborhood blocks, and areas across busy streets. Years later, the “Living Space Questionnaire” was developed by Stalvey et al. in 1999 [
6], followed by the “Living Space Assessment (LSA)” created by Baker et al. at the University of Alabama at Birmingham (UAB) in 2003, which measures mobility across five concentric zones: outside the bedroom, outside the house, within the neighborhood, outside the neighborhood but within the town, and outside the town, over the past four weeks [
9]. The composite score ranges from 0 to 120, with higher scores indicative of greater mobility flexibility; thus, this measure can be seen as a predictor of morbidity, mortality, and healthcare utilization among the elderly population. Currently, studies have begun to utilize devices equipped with sensors to monitor and accurately measure living space, aiming to reflect the multidimensional nature of mobility [
10]. These devices exhibit significant potential due to their objectivity, reduced burden on participants, and capacity to provide prolonged observations over time [
11]. One selected instrument is GPS, which serves as a geographical indicator for describing an individual’s daily activities [
12].
The living space of older adults serves not only as a physical location of residence, but also reflects the environmental complexity they encounter [
13]. Community mobility within the living space is linked to risk behavior, particularly in relation to falls. The World Health Organization (WHO) defines a fall as an “event that causes a person to unintentionally rest on the ground, floor, or another lower level”.
The prevalence of falls among older adults is 26.5%, yet this figure may increase depending on the individual’s context [
14]. The most vulnerable group comprises adults aged 65 and older, with the risk escalating as age increases, especially in the presence of signs of frailty [
15]. According to recent studies, approximately one in four older adults experiences at least one fall each year. This not only increases the risk of physical injuries, but also contributes to a persistent fear of falling, which becomes a significant factor in increasing the likelihood of future falls. This fear negatively impacts mobility confidence, often disrupting gait, particularly in community settings where environmental challenges are common. The recurrent cycle of falls and fear highlights the importance of implementing preventive strategies that address both the physical and psychological factors associated with fall risk in older adults [
16].
Walking, as an essential motor function in daily life, constitutes a common link to activities of daily living and undergoes changes as we age. Trips are one of the most frequent causes of falls during walking and are associated with increased variability [
17] and decreased speed [
18] of walking, as well as observed changes in cadence [
19,
20], variability in stride length, swing phase duration, and double support [
20], all of which have been shown to be directly associated with an increased risk of falls. Regardless of whether the fall has resulted in injuries, this situation leads to a diminished functional capacity of the individual to perform daily activities, which consequently results in a reduction in mobility within the living space during the six months following the event [
21]. A decrease in living space is associated with frailty, fear of falling, fall risk, and mortality [
21,
22], among other factors, which significantly impact the health and well-being of older adults. Mobility within the living space during aging is compromised not only by intrinsic physiological issues, such as balance and gait disorders, neurological diseases, cognitive impairments, muscular weakness, depression, obesity, polypharmacy, and urinary incontinence, but also by other age-related factors that contribute to reduced mobility and increased fall risk [
23,
24,
25]. Demographic factors such as sex, age, low education level, and socioeconomic status [
23,
26] also play a significant role. When analyzed from a broader perspective, it encompasses other relevant multidimensional aspects, including those related to economic, material, and sociocultural factors [
27].
Due to the increasing importance of understanding living space in gerontological research, this study aims to examine the relationship between fall risk and living space. We asked whether it is possible to identify older people with and without a history of falls by using metrics that represent living space. Our hypothesis is that participants who do not have a history of falls have characteristics of greater living space, so they must be differentiated.
2. Related Work
Research has increasingly focused on the relationship between physical activity and living space mobility in older adults. The association between objectively measured physical activity and lifespace mobility demonstrates how wearable sensors, such as accelerometers and GPS devices, can provide accurate quantification of lifespace mobility [
28,
29], which is why its use has gained importance in the evaluation of daily mobility among older adults. Studies on the subject reveal that higher levels of physical activity are strongly associated with greater mobility in the living space, which contributes to greater autonomy and the ability to interact with various environmental zones [
28,
30]. These findings underscore the importance of promoting physical activity to reduce frailty and improve quality of life while highlighting the utility of sensor-based methods for continuous, objective measurements of both activity and living space mobility [
31,
32].
A group of researchers explored how GPS data can reveal information about the relationship between daily mobility and well-being in community-dwelling older adults, demonstrating that higher levels of daily mobility, as measured via GPS, are positively correlated with improved mental health and well-being, emphasizing the connection between environmental engagement and overall quality of life [
33]. This further strengthens the argument for encouraging greater mobility to improve the life outcomes of older adults. Additionally, wearable sensor technologies have expanded into living space mobility assessments. The development and validation of a mobility tracker prototype introduces a GPS recorder combined with an accelerometer to objectively monitor mobility patterns and activity levels in older adults. The device’s ability to track real-time movement and activity participation highlights its potential for geriatric research. Research highlights the importance of integrating sensor technologies into mobility studies, providing more accurate measures to inform interventions aimed at improving independence and reducing fall risks [
34,
35].
The dynamic relationship between physical activity and life-space mobility is further explored in objectively measured physical activity and changes in life-space mobility among older people. Using accelerometers and GPS devices, a study reveals that increased physical activity is associated with expanded living space, leading to greater functional independence. In contrast, decreases in activity levels result in a contraction of living space, emphasizing the need to maintain activity levels to preserve mobility and quality of life [
36]. Wearable sensors have also been used to quantify real-world mobility patterns, as discussed in Quantifying Free-Living Community Mobility in Healthy Older Adults Using Wearable Sensors. In another study, researchers capture detailed information about how older adults move in their communities, revealing the advantages of wearable technologies to continuously monitor mobility without the limitations of laboratory environments [
37]. These findings suggest that wearable sensors offer an unobtrusive but accurate means of assessing mobility, informing interventions aimed at preserving physical function in older populations [
37].
A more comprehensive approach to understanding mobility is presented in Predictors of Real-Life Mobility in Community-Dwelling Older Adults, which explores both individual-level determinants and external factors, such as neighborhood walkability and social engagement. One study suggests that effective interventions to improve mobility must consider both personal and environmental influences, reflecting the complexity of mobility patterns in older adults [
38]. On the other hand, another study reveals that older adults who carry out higher levels of physical activity tend to move in areas of larger living spaces, which is indicative of greater autonomy. This research emphasizes the importance of promoting physical activity as a means to maintain or improve the mobility of the living space, directly contributing to the well-being and independence of older adults [
32].
Community Mobility Positioning System Indicators and Future Health Outcomes Among Older Adults shows that GPS-derived mobility indicators predict future health outcomes, such as physical decline and hospitalization rates. Research results demonstrated that the utility of monitoring community mobility can inform early interventions aimed at preserving health and improving outcomes in aging populations [
39]. The use of GPS watches to monitor mobility in the living space highlights the relationship between this mobility and the health characteristics of older adults who use devices with global positioning systems.
Research links reduced mobility in the living space with negative health indicators, such as decreased physical function and increased risk of falls, showing the value of GPS technology in providing real-time assessments of mobility and health in older adults [
40]. The challenges and opportunities of using GPS to track mobility patterns in older adults with dementia were explored in a GPS-based study to understand the outdoor mobility patterns of older adults with dementia [
41]. This research highlights the reduced outdoor mobility of people with dementia and suggests that GPS-based monitoring can help healthcare providers assess decreased mobility and implement timely interventions.
On the other hand, one study pointed out discrepancies between objective GPS data and self-reported mobility measures. This study emphasizes the importance of integrating objective tools such as GPS to complement self-reported data, leading to a more comprehensive understanding of life-space mobility and its implications for health outcomes, particularly in relation to falls [
42]. Generating GPS activity spaces that shed light on the mobility habits of older adults further investigates the value of GPS data in creating “activity spaces” that provide detailed information about how older adults navigate their environments. Other research emphasizes that these activity spaces offer more accurate real-world movement data compared to traditional self-reports, highlighting the importance of leveraging technology for mobility assessments [
12].
Despite the increasing use of sensor-based technologies to assess mobility, research that explores a broader range of physical functions and overall functioning within the context of living space mobility remains lacking. Most studies tend to focus on isolated aspects, such as walking speed or step count, rather than investigating how multiple physical factors interact to influence mobility in various environments. Expanding the scope of these investigations is essential to gain a more complete understanding of how living space mobility is affected by the complex interplay of physical and environmental factors. Additionally, integrating data from different sources, such as GPS and accelerometers, provides a more holistic view of mobility patterns. GPS data enable precise tracking of geographic movement and distance, while accelerometers provide detailed information on activity intensity and gait quality. This combination is crucial for understanding life-space mobility and its relationship to falls, as it offers insights into the spatial and physical dimensions of mobility, leading to improved fall-prevention strategies. However, there is still a significant gap in the literature on the combined use of sensor-based data to explore how various physical and environmental factors interact in shaping living space mobility. Our study seeks to fill this gap by integrating data from GPS, accelerometers, and other functional measures to provide a more complete perspective of mobility in older adults. By addressing this gap, our work seeks to contribute to the deepening of how these factors jointly influence fall risk, complementing with new knowledge that can inform more effective fall prevention interventions and mobility support strategies.
3. Materials and Methods
3.1. Participant Recruitment and Eligibility Criteria
A total of 129 older adults from the Metropolitan Region of Santiago, Chile, were included regardless of their socioeconomic level (see
Table 1 for the description of the dataset). The recruitment process was adjusted to ethical guidelines, granting each participant written informed consent previously approved by the Scientific Bioethics Committee of the Central University of Chile (reference project 48/2022). Participants were recruited over a six-month period (August 2023–January 2024) through a stratified recruitment process in primary care centers and local communities. Recruitment efforts included advertisements in health centers and community networks inviting men and women aged 65 years and older to participate. Eligibility criteria required that participants were free of fatigue or breathing difficulties at the time of assessment. Older adults with chronic conditions such as hypertension or diabetes were included as long as their conditions were under medical control. However, people with cognitive impairment that could make it difficult to understand informed consent or follow simple instructions were excluded. The sampling method used was non-probabilistic convenience sampling, intended to guarantee a representative sample of diverse origins, socioeconomic levels, and health states.
Falls were identified through a combination of self-reported history and clinical assessment. During the baseline interview, participants reported any falls they had experienced in the past 12 months. When available, medical records were reviewed to corroborate reported falls. A fall was considered to be that defined by the WHO in 2021 as an “event which results in a person coming to rest inadvertently on the ground or floor or other lower level”. Based on this definition, participants were classified into two groups: those who had a history of falls and those who did not.
3.2. Use of Smartphones for Mobility Monitoring
Mobility within the community was monitored using two systems: global positioning system (GPS) and using an accelerometer, both incorporated into a smartphone. The GPS provided estimates of life-space mobility metrics, while the accelerometer captured spatiotemporal parameters of gait and motor control. Smartphones, equipped with sensors such as accelerometers, gyroscopes, magnetometers, and GPS, serve as valuable, low-cost, and accessible tools for assessing mobility in older adults. The accuracy and reliability of smartphones equipped with MEMS-based inertial sensors, including the accelerometer and gyroscope found in devices such as the Samsung Galaxy A14, have been demonstrated in controlled laboratory tests. Studies have validated the performance of these sensors in various motion tracking applications, showing that they provide comparable accuracy to more advanced systems like motion capture devices [
43]. Studies show that the accelerometer and gyroscope in modern smartphones provide valid and reliable data for estimating motion with comparable accuracy to standard systems, such as the Vicon MX motion capture system [
44]. The studies show acceptable accuracy in measuring movement and orientation, making them viable for non-clinical applications such as gait analysis and fall prediction [
44,
45]. The GPS sampling rate was set to one data point per minute, which provided sufficient detail to track spatial movement patterns. The accelerometer, on the other hand, recorded data at a rate of 50 Hz (50 data points per second), which is adequate for capturing detailed gait dynamics. The mobile phone was securely placed on the participant’s torso, specifically between the T5 and T10 vertebral levels, using an adjustable harness to ensure stability and continuous contact with the individual’s body throughout the assessment (see
Figure 1). This anatomical location was chosen due to its proximity to the center of mass of the body, providing a more representative measure of trunk balance and control during movement. Placing the phone in this area also ensures that the device does not interfere with the body’s natural movements during the assessment, providing comfort to the subject without compromising the accuracy of the data. This level of precision in device placement is critical for replicability by ensuring that the data collected accurately reflect the participant’s mobility and motor control. Each participant was monitored for approximately 8 h until they went to sleep.
The measurements began at a community center located within the participants’ residential municipality. From this starting point, each participant moved freely toward their home or other destinations, using their preferred mode of transportation (walking, by car, by bus, etc.). This approach allowed us to capture mobility in real-life conditions, reflecting their daily routines without imposing restrictions on their routes or activities.
3.3. Life-Space Mobility
Participants were instructed to follow their usual daily routines on the day they were assessed for community mobility. This approach was taken to ensure that the mobility data collected reflected authentic real-world behaviors and movement patterns. Although the observation period was limited to a single day, this method aimed to capture the typical mobility of participants within their community environment. To maintain the validity of the data, the assessments were rescheduled in case of unfavorable weather conditions, such as rain, which could have influenced the participants’ behavior. This precaution helped minimize deviations from their usual activities, ensuring a more accurate reflection of their mobility patterns. Participants were thoroughly briefed to adhere to their normal schedules, avoiding any variations, such as adding or omitting activities, to ensure that their daily living space and interactions were authentically captured. By emphasizing the importance of maintaining their usual routines, this study sought to provide a realistic assessment of life-space mobility in older adults within their natural community environments.
3.4. GPS Data Processing
Python’s Scikit-Mobility library was used to perform a detailed analysis of participants’ movement trajectories based on GPS (latitude and longitude) time series data. This tool allowed the visualization of movement routes, the identification of stopping places throughout the day, and the detection of the home location of each subject. Additionally, the time spent in each identified location was calculated. This information was then used to analyze acceleration patterns outside the home, providing a comprehensive understanding of subjects’ mobility and spatiotemporal behaviors within their daily environments.
Scikit-Mobility is an advanced Python library designed specifically for mobility data manipulation and analysis. It allows the study of various aspects of human movement through a specialized set of tools [
46]. One of its key features is the TrajDataFrame class, which extends the functionality of Pandas DataFrame by integrating spatial and temporal coordinates. This allows specific operations on trajectories, such as filtering by time or location or calculating distances between points. The library also includes visualization functions for mapping trajectories, making it easier to interpret mobility patterns. In addition, Scikit-Mobility incorporates algorithms to detect locations where people stay for significant periods, allowing points of interest or repetitive behavior patterns to be identified. As shown in
Figure 1, diamonds of different colors represent various stages in an individual’s trajectory, providing information about mobility behaviors and daily routines.
Daily Mobility Plot
The daily mobility of each participant was visually represented by a series of colored bars, each of them corresponding to different places visited throughout the day (see
Figure 2). These color-coded bars illustrate both the duration and sequence of stays at various points of interest, offering a clear overview of participants’ daily movement patterns, including time thresholds and geographic radius considerations. The beginning of each bar indicates the time of arrival at a location, while the end marks the departure, creating a chronological visualization of mobility across geographic spaces. This graph highlights not only the frequency and regularity of visits to specific places, but also the spatial and temporal distribution of each individual’s activities throughout the day. In
Figure 2, the pink rectangle represents the time spent inside the participant’s house, while the other colored rectangles (brown, white, green) mean different places visited. From this visualization, we identified the spatiotemporal windows corresponding to the periods in which participants moved outside their homes. To accurately generate these stays, several key parameters were defined. First, the stop radius factor, which determines the distance within which a location is classified as a “stay”; secondly, the minimum duration necessary to define a stop, which in this study was set at 15 min; and finally, the spatial radius, which represents the distance used to group nearby points. In this analysis, we used a radius of 100 m and a minimum stop duration of 15 min to identify significant stays. These parameters were carefully selected to capture relevant movements without introducing unnecessary noise on short trips or brief stops. The choice of a 100 m radius is justified by its proven suitability for capturing daily movements, especially in densely populated urban areas. This value strikes a balance between precision and functionality in detecting points of interest within mobility patterns [
46,
47]. Similarly, the 15 min stop duration was selected to filter out brief interruptions and focus on the most meaningful activities. Previous studies have employed similar thresholds to capture significant stays that reflect important human behaviors, such as visiting a commercial establishment or resting in a park [
48,
49].
3.5. Location Clustering
The location clustering function within the library enables the grouping of locations based on their spatial proximity, making it useful for identifying areas with high mobility density or geographic patterns of interest. This is achieved using the Density-Based Spatial Clustering of Applications with Noise (DBSCAN) algorithm, which clusters points based on density. Key parameters for this process include the maximum distance, which defines the maximum distance in kilometers for considering points within the same cluster, and the minimum number of samples required to form a cluster.
3.6. Mobility Metrics
The following life-space mobility variables were calculated using GPS data to provide a comprehensive view of spatial and temporal mobility patterns among the participants. These metrics offer valuable insights into both the geographical extent and behavioral characteristics of movement, both of which are for understanding life-space mobility.
Activity Space (km2):
This refers to the geographical area in which a person conducts their daily activities or regularly travels [
11]. It is represented by the Minimum Convex Polygon (MCP), which is the smallest convex shape that encloses all the GPS points. The area of the MCP is calculated as
where
are the coordinates of the GPS points. In the code, this was converted from square meters to square kilometers.
SDE Compactness: SDE compactness measures how concentrated or dispersed a person’s movements are within their activity space. This measure can provide information on the efficiency and distribution of mobility in a specific area [
50].
This is computed using the Standard Deviational Ellipse (SDE), which represents the spread of movement. Compactness is calculated as
where
is the area of the ellipse and
is the perimeter of the minimum convex polygon.
Minimum Convex Polygon: The term minimum convex polygon refers to the geometric shape that minimally encloses all points, representing the mobility of older adults within their activity space. This polygon can be used to delineate the maximum area covered by daily activities of an older adult [
4]. Its area,
, is computed as described in the
Section 4.1.1.
Number of Visited Places: Refers to the count of distinct locations visited by an older adult within a specified time period, which can be an indicator of their mobility and social activity [
11]. It is calculated by identifying clusters of GPS points using the DBSCAN algorithm and counting the number of clusters.
Time Outside of Home (hours): The total number of hours that an older adult spends outside their habitual residence can be a significant indicator of their level of activity and community participation [
4]. The time spent outside the home is calculated by summing the time intervals during which the individual is located outside their home. If
is the time outside for each visit:
Maximum Distance (km): The term maximum distance refers to the farthest distance an older adult has traveled from their habitual residence as part of their daily mobility [
11]. It is calculated using the geodesic distance formula between the home location and the farthest point, as follows:
Straight-Line Distance: This is the sum of the straight-line distances between consecutive points [
51], calculated as
where
represents the geodesic distance between consecutive points.
Turning Radius: This metric provides insights into the smoothness and continuity of an individual’s movement patterns. A smaller turning radius may indicate frequent changes in direction, often associated with navigation through confined spaces or complex environments. In contrast, a larger turning radius typically suggests smoother, more direct paths, often seen in open or less complex environments. In studies of older adults, a smaller turning radius could indicate cautious or hesitant movement, which might be linked to fear of falling or difficulties in spatial navigation [
52]. It is calculated by evaluating the angles between consecutive trip segments and the radius of curvature, as follows:
where
l is the distance between two points, and
is the angle of turning.
K Radius of Gyration: A measure used to describe the dispersion of an individual’s movements from a central point, usually their home or another significant location. It calculates the average distance of all the points visited from this central location, providing an understanding of the extent of an individual’s mobility within their community. A larger radius of gyration suggests that the individual regularly moves over a broader area, indicating higher mobility and possibly greater independence [
53]. It is computed as
where
is the distance of the
i-th point from the center of mass (usually the home location) and
is the average distance.
3.7. Accelerometer Data Processing
A Butterworth band-pass filter was applied to the acceleration signals on all three axes of the accelerometer, with low and high cut-off frequencies of 0.5 Hz and 20 Hz, respectively. This filter is effective in eliminating high-frequency noise while retaining the signal components relevant to human gait.
Subsequently, the ‘find_peaks’ function from ‘scipy.signal’ was used to detect peaks in the filtered signals. A minimum distance between consecutive peaks was set, calculated as half of the sampling frequency (fs/2) to avoid false detection caused by small fluctuations in the signal. Additionally, a minimum peak height threshold was defined, set to 0.5 to reduce the detection of peaks originating from residual noise. Peak identification enabled the calculation of various gait characteristics such as the number of steps, cadence, mean step time, step time variability, regularity, and step symmetry.
To exclusively detect and analyze the gait sections within the 8 h accelerometer data, specific inclusion criteria were implemented to identify walking episodes and exclude movements not relevant to gait analysis. First, a speed threshold of less than 5 km/h was set to exclude movements conducted via other modes of transportation, such as cars, buses, or public transit, thus focusing the analysis on gait activities.
Additionally, to ensure the continuity of the gait episodes, the acceleration signal was required to contain at least 30 consecutive peaks, representing detected steps. With the established threshold, brief or incomplete movements that do not reflect sustained gait patterns were excluded. On the other hand, the duration of the gait sections varied across participants, as it depended on their unique mobility patterns and movements throughout the study period. For each gait variable (such as cadence, mean step time, step time variability, regularity, and step symmetry) the average of all walking records that met these criteria was calculated and analyzed.
Gait Characteristics (Accelerometer Metrics)
In this study, an average step length of 0.7 m was used as a constant for all participants. This value is widely recognized in the literature as a standard approximation for step length in older adults during regular walking conditions. Research has shown that the average step length for healthy adults typically ranges between 0.65 and 0.75 m depending on factors such as height, gait speed, and age [
54,
55]. Given the variability in step length due to individual characteristics, using 0.7 m as an average provides a reasonable estimate for analyzing walking patterns in older populations. Studies have also demonstrated that fixed step length values are commonly employed in gait analysis when direct measurement is not feasible or when individual-specific data are unavailable [
56,
57]. This approach ensures consistency in the estimation of walking speed and total distance traveled, allowing for a reliable comparison of gait parameters across participants.
Step count calculation is a key element for gait pattern analysis and was based on the detection of peaks in the vertical acceleration signal. The use of spike detection in acceleration signals is a well-established technique in gait analysis. Previous studies have shown that identifying peaks in the vertical acceleration signal is a reliable and valid method for detecting steps, particularly in free-living conditions and with wearable devices such as smartphones and accelerometers [
58,
59]. While it may seem simplistic, peak detection is very effective due to the repetitive and cyclical nature of walking, where each step generates a distinct peak in the acceleration signal. This method has been widely used in clinical and research settings as it provides accurate step count estimates, especially when combined with filtering techniques such as the Butterworth filter to reduce noise and eliminate false detections [
60,
61]. Furthermore, other step-derived variables such as step time variability, regularity, and symmetry, are also well-supported in the literature as indicators of gait stability and fall risk. These variables, derived from step intervals and accelerometer data, have been shown to correlate with balance control and fall risk in older adults [
54,
62]. Therefore, by combining a standardized step length with peak detection for step counting, and subsequently deriving additional gait metrics, this study employs a validated approach that strikes a balance between simplicity, practicality, and accuracy in both controlled and free-living environments. Additionally, the use of the inverse of the standard deviation of step time as a measure of step regularity is also well-supported in the literature. Studies have shown that this metric provides a reliable and simple quantification of step rhythm coherence, reflecting variability in the gait cycle. For example, several studies [
54,
62] used the inverse of the standard deviation of step time to evaluate gait stability, which demonstrated its usefulness in identifying individuals at higher risk of falls due to irregular stepping patterns. Although step regularity is often derived using autocorrelation procedures, particularly in studies that focus on variations between strides and the periodicity of gait signals [
63], the inverse of the standard deviation remains a widely accepted and simpler, computationally efficient, and interpretable alternative, especially in large data sets or free-living conditions. This method allows a balance between simplicity and reliability, providing a meaningful measure of gait consistency that correlates with other indicators of gait stability, such as symmetry and gait variability.
3.8. Mobility and Gait Metrics
The inclusion of both life-space mobility and gait characteristics as features in this study is essential for providing a comprehensive analysis of mobility patterns in older adults and their association with fall risk. Life-space mobility metrics, such as time spent outside the home, number of places visited, radius of gyration, and maximum distance traveled, capture an individual’s spatial behavior and their interaction with the environment. These metrics are particularly important because reduced life-space mobility has been linked to increased frailty, social isolation, and a higher likelihood of falls [
64,
65]. By analyzing these variables, we can better understand how participants’ engagement with their surroundings influences their physical activity levels and overall fall risk. In addition, gait characteristics such as step count, walking speed, stride regularity, and step symmetry provide critical insights into the biomechanical aspects of mobility. Gait has been extensively studied as a predictor of falls, with irregularities in gait patterns often indicating underlying motor or balance impairments [
62,
66]. Features such as step time variability and RMS acceleration help capture not only the consistency of movement but also the stability of the gait cycle, which are crucial indicators of an individual’s functional mobility and fall risk [
67,
68]. By combining both life-space mobility and gait characteristics, this study is able to capture both the environmental and physical dimensions of mobility, offering a more holistic approach to fall risk prediction. This comprehensive set of features allows for a better understanding of the interplay between spatial behavior and motor control, thus improving the accuracy of the models used to classify fall risk in older adults.
3.9. Classification Between Fallers and Non-Fallers
Using mobility metrics and machine learning algorithms, we assessed the ability to differentiate behavioral patterns between older adults with and without a history of falls in the past year. To achieve this, we employed Support Vector Machines (SVMs), Random Forest (RF), and K-Nearest Neighbors (KNN) algorithms. The selection of these algorithms was based on their complementary strengths in handling diverse data types and their proven effectiveness in classification tasks, particularly within the domain of gait analysis and fall risk prediction.
SVM is renowned for its robustness in high-dimensional feature spaces and performs particularly well with small sample sizes, making it an ideal choice for our dataset, which consists of a limited number of participants relative to the feature space [
69,
70]. Furthermore, studies have demonstrated that SVM classifiers exhibit high generalizability in automatic fall detection, achieving up to 93% accuracy in distinguishing falls from normal daily activities [
71]. KNN, on the other hand, is a simple yet powerful instance-based learning algorithm that performs well in scenarios where the decision boundaries are complex or non-linear. KNN’s ability to adapt locally to the structure of the data makes it a natural choice when the relationship between features and labels may vary across different regions of the feature space [
72,
73]. KNN has shown high performance in classifying gait patterns, with reported accuracy rates of up to 94% [
74].
Finally, Random Forest (RF) was chosen for its strong performance in handling noisy and high-dimensional data, thanks to its ensemble nature and ability to mitigate overfitting through bootstrapping and random feature selection [
75]. RF has been widely applied in fall detection and gait analysis studies, consistently demonstrating high accuracy. In a recent study, RF achieved 91.3% accuracy in predicting fall risk using gait data [
76].
By selecting these three algorithms, we aimed to leverage their respective advantages to improve the robustness and accuracy of our fall risk classification model. To implement the algorithms, the Python Scikit-learn library was used, which provides simple and efficient tools for data analysis and modeling, including classification, regression, clustering, and dimensionality reduction algorithms.
In this study, three classification models were implemented: Random Forest, K-Nearest Neighbors, and Support Vector Machines, to differentiate between the groups of “people who have experienced falls” and “people who have not experienced falls”. To optimize the performance of each model, an exhaustive hyperparameter search was conducted using GridSearchCV. For Random Forest, combinations of hyperparameters were explored, including the number of trees (n_estimators) set at 100, 200, and 300; maximum tree depths (max_depth) of 2 and 3; minimum number of samples required to split an internal node (min_samples_split) of 2 and 5; minimum number of samples required at a leaf node (min_samples_leaf) of 3 and 4; and the number of features to consider when looking for the best split (max_features) as ‘sqrt’ and ‘log2’. For the K-Nearest Neighbors model, values of n_neighbors from 1 to 10 were evaluated, with weight functions (weights) ‘uniform’ and ‘distance’, and distance metrics ‘Euclidean’ and ‘Manhattan’. Regarding Support Vector Machines, values of the penalty parameter C of 0.1, 1, and 10 were tested; values of gamma of 1, 0.1, and 0.01; and different kernel functions: ‘rbf’, ‘poly’, and ‘sigmoid’. Cross-validation was performed using Leave-One-Out Cross-Validation (LOOCV), and the f1_macro metric was used to evaluate performance during hyperparameter tuning. The data were divided into training and test sets in a proportion of 70% and 30%, respectively, applying standard normalization and missing value imputation through a pipeline that included SimpleImputer and StandardScaler. To evaluate the final performance of the models, classification reports and ROC curves were generated, using the area under the curve (AUC) as the main metric.
The ROC curves were generated using the test datasets following the split into training and test sets, without retraining the models on the samples used in the ROC curve analysis. This methodology ensures that the AUC calculation accurately reflects the model’s performance on the validation set.
5. Discussion
The primary objective of this study was to assess whether machine learning models could effectively distinguish between older adults with and without a history of falls using mobility metrics derived from GPS and accelerometer data. By employing three machine learning algorithms (Random Forest, Support Vector Machine, and K-Nearest Neighbors) we sought to explore how life-space mobility and gait patterns could predict fall risk in older adults. This study addressed a gap in the literature by demonstrating that the combination of sensor-based metrics, such as GPS and accelerometers, enhances classification performance compared to using individual data sources alone.
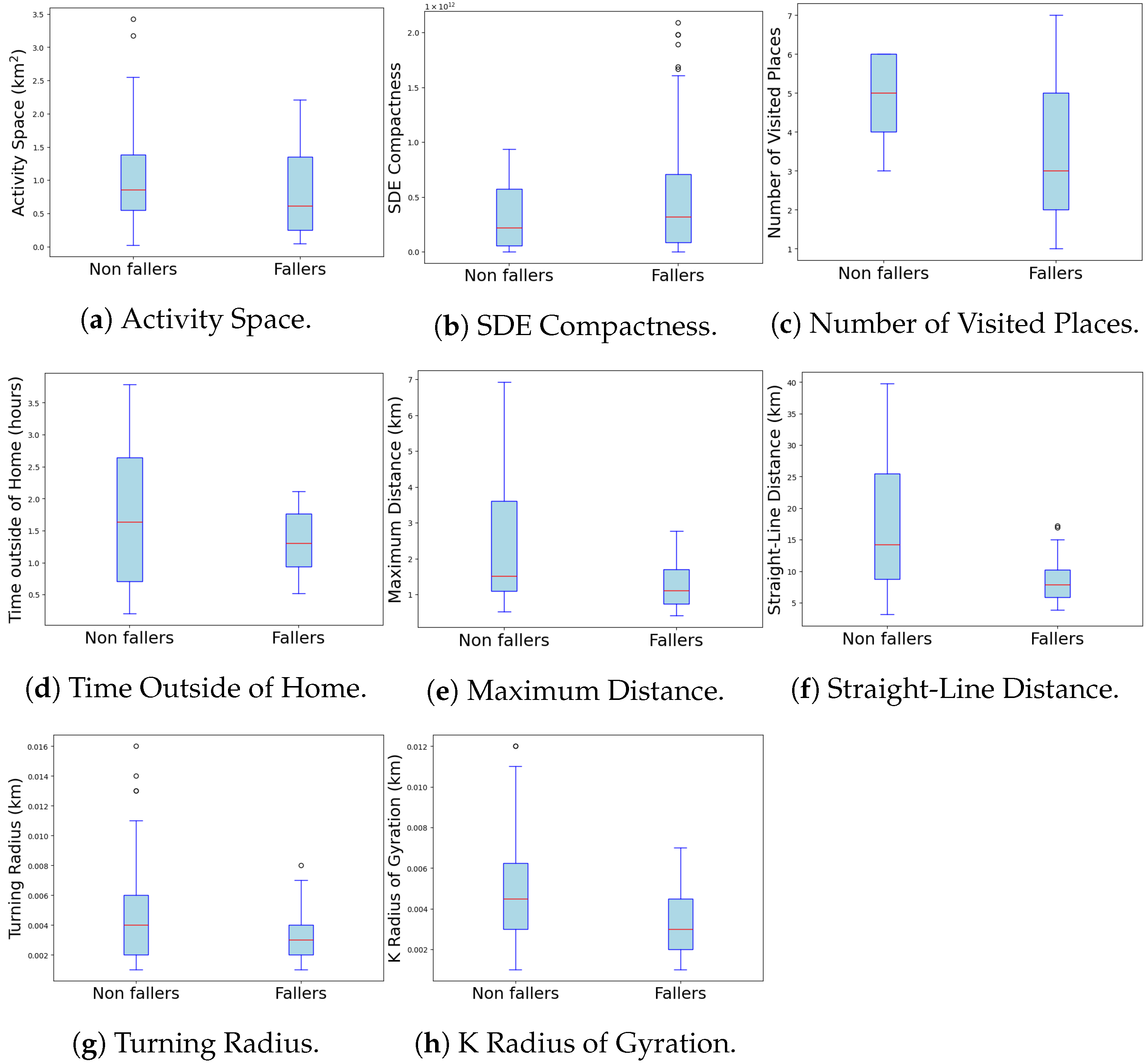
Our results indicated significant differences in several key metrics, underscoring the relevance of these measures for fall risk prediction. For instance, the “Activity Space” metric showed substantial differences between non-fallers and fallers (see
Table 2 and
Figure 3a), as did the “Maximum Distance Traveled” (see
Figure 3e). These findings suggest that non-fallers tend to have greater mobility within their life space, potentially reflecting better functional mobility. Similarly, gait metrics, such as mean step time and step time variability, revealed slower and more variable gait patterns in the group of individuals who experienced falls, consistent with a less stable gait in those with a history of falls (see
Figure 4b,c).
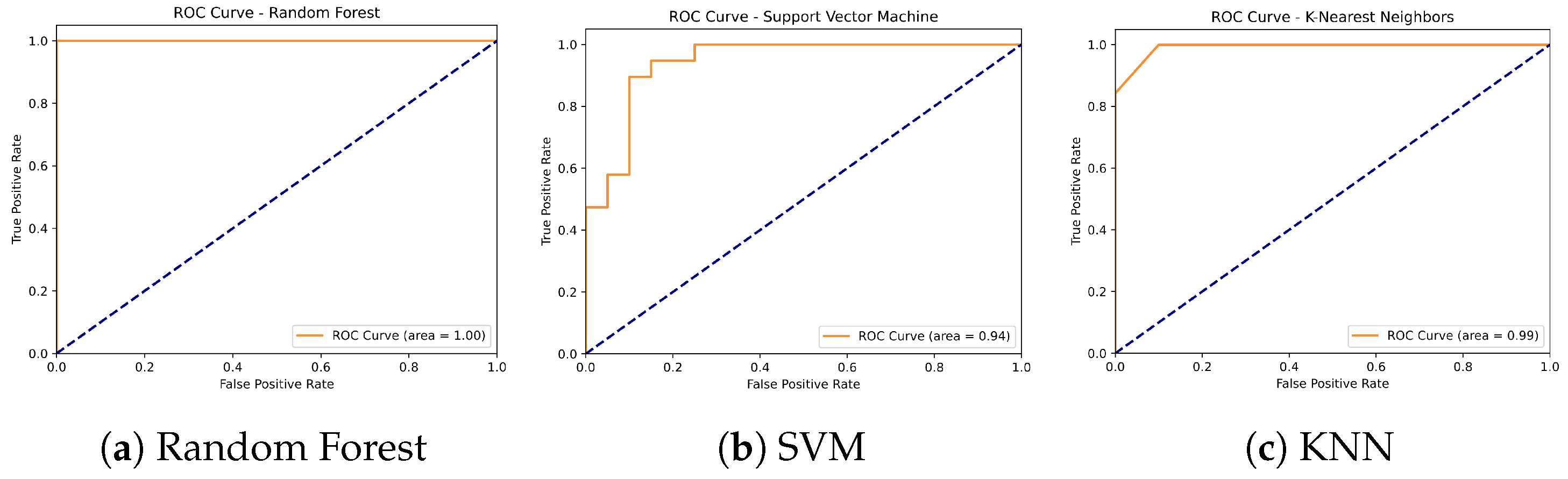
Furthermore, models that combined GPS and accelerometer data outperformed those based on either data source alone. The Random Forest model achieved the highest accuracy at 97%, closely followed by SVM at 95%, while KNN showed lower performance with an accuracy of 87% (see
Table 6 and
Figure 7). These findings are consistent with previous research [
78], which demonstrated that machine learning models like Random Forest and SVM are highly effective in predicting fall risk when using wearable sensors for gait and movement analysis; similarly, [
79] found that combining accelerometer data with machine learning algorithms improved fall risk classification accuracy in older adults.
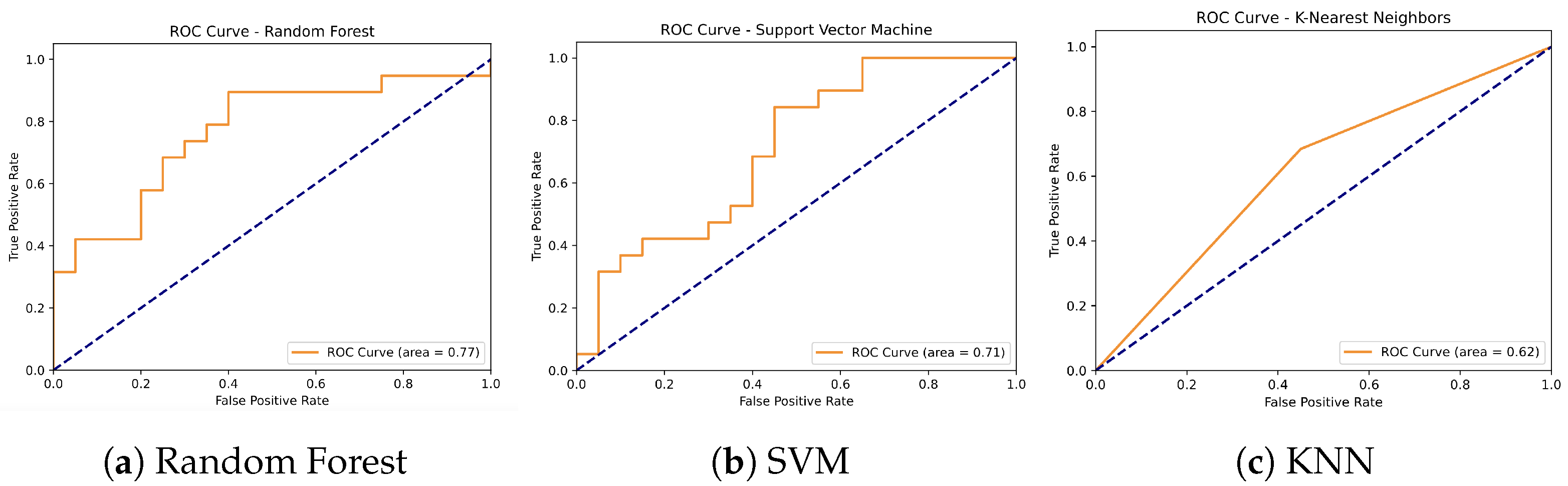
In contrast, models based solely on GPS data yielded lower accuracies, with Random Forest achieving 74% and SVM and KNN reaching 67% and 62%, respectively (see
Table 4 and
Figure 5). While these results suggest that GPS data alone provide valuable information about life-space mobility, it is the combination of GPS and accelerometer data that produces the most robust predictions, reinforcing the importance of integrating both data sources for fall risk assessment. Additionally, classification models based solely on accelerometer data also showed strong results: Random Forest again achieved the highest accuracy at 95%, followed by SVM and KNN with 90%. These findings demonstrate the utility of gait characteristics captured by accelerometers for predicting fall risk, while also highlighting that adding GPS metrics offers greater refinement and enhances the predictive power of the models (see
Table 5 and
Figure 6).
Previous research has often relied heavily on accelerometer data to classify fallers and non-fallers. For example, a study [
80] demonstrated that accelerometer-based models could achieve high accuracy in detecting fall risk, with results reaching up to 90% precision. However, this study did not incorporate life-space mobility metrics, such as activity space derived from GPS data. This limits the approach to movement characteristics captured by accelerometers without considering spatial mobility patterns that reflect the overall functional capacity of older adults. In contrast, this study adds to the existing literature by demonstrating that the combination of life-space mobility metrics with gait characteristics results in significantly improved classification outcomes. The inclusion of GPS data, as demonstrated in this work, adds an important dimension to understanding fall risk, particularly by capturing variations in daily movement patterns that reflect an individual’s functional capacity. Another study [
81] emphasized that older adults with restricted life-space mobility are at greater risk of falling, corroborating the findings of this study, which showed that fallers exhibited significantly smaller activity spaces and shorter maximum distances traveled compared to non-fallers. Integrating these GPS-derived metrics into machine learning models, as demonstrated here, strengthens the case for using life-space variables to assess fall risk in community-dwelling older adults.
Using GPS metrics in combination with gait characteristics provides a more comprehensive assessment of fall risk. Non-fallers exhibited larger life-space metrics, including greater activity space and maximum distance traveled, which aligns with previous studies suggesting that reduced mobility is associated with a higher risk of falls. Additionally, gait metrics such as step time variability and harmonic ratio showed significant differences between fallers and non-fallers, reinforcing the importance of stable and rhythmic movement patterns in fall prevention. These findings are consistent with those of Weiss et al. (2013) [
78], who found that algorithms such as Random Forest and SVM, when applied to wearable sensor data (e.g., accelerometers), were highly effective in predicting fall risk among older adults. However, this study demonstrates that combining GPS and accelerometer data further improves prediction outcomes.
Interestingly, while some metrics showed significant differences between fallers and non-fallers, others, such as step symmetry, did not. This may suggest that certain gait characteristics, like symmetry, may not be as relevant for distinguishing fallers from non-fallers or could reflect limitations in the sample size or sensitivity of measurement tools. This finding highlights the need for further studies exploring which gait characteristics are most predictive of fall risk. Moreover, differences in recall rates between fallers and non-fallers suggest that while the models are good at identifying non-fallers, there is room for improvement in accurately detecting fallers. This observation aligns with the findings obtained in a study [
79] in which it was noted that although accelerometer data with machine learning algorithms, improved fall risk classification accuracy, accurately detecting fallers remains challenging, particularly in individuals with more restricted life-space mobility.
Despite the significant findings, this study presents several limitations that should be considered when interpreting the results. One major limitation is the sample size. Although this study included 129 older adults, this number may not be large enough to capture the full variability of gait and mobility metrics within this population. A larger sample size could improve the generalizability of the results and allow for more detailed analyses, such as stratification by age groups or comorbidities, which was not feasible in this study due to the limited number of subjects. Additionally, the mobility and gait data were collected over a single day of observation. While participants were asked to maintain their normal daily routine, this approach may not adequately capture fluctuations in mobility patterns that occur over the course of a week or different seasons. Future studies should consider collecting data over more extended periods to better reflect variability in older adults’ mobility and their environment. Another consideration is the use of a fixed step length estimation (0.7 m) to calculate walking speed and total distance traveled. While this value is consistent with previous studies and provides a reasonable approximation for the population studied, individual step length was not measured for each participant, which may have introduced estimation errors in the walking speed analysis. In future research, it would be beneficial to incorporate personalized step length measurements or use more advanced sensors capable of estimating this value in real time. Moreover, the use of peak detection in accelerometer signals for step counting, while widely accepted in the field of biomechanics, may not adequately capture steps occurring in unusual conditions or during abrupt changes in direction. This could limit the precision in identifying irregular gait patterns in individuals at high risk of falls. A combination of detection methods, such as using gyroscopes alongside accelerometers, could enhance accuracy in future research.
The use of machine learning algorithms, although powerful, also comes with certain limitations. While Random Forest offers high classification accuracy, the use of this algorithm implies the need for a larger amount of data to improve its generalization capability. Since machine learning algorithms tend to be sensitive to the quality and quantity of data, future research should include larger and more diverse datasets to validate the findings of this study. Additionally, hyperparameter tuning techniques were not explored, which could have further optimized the models’ performance. Moreover, this study did not address multicollinearity in the mobility and gait metrics used to train the classification models. The presence of multicollinearity could affect the interpretation of the individual contributions of variables in the model and bias the results. Future studies should employ techniques such as Principal Component Analysis (PCA) or the removal of highly correlated variables to enhance model stability and interpretability. Finally, the definition of the group of non-fallers, based exclusively on the absence of fall events in the 12 months preceding the assessment, represents another limitation. While this definition is consistent with the literature and allows for an initial classification, it does not guarantee that individuals classified as “non-faller” will not experience a fall shortly after measurement. Given that falls can be unpredictable events, the fact that a person did not fall in the previous year does not eliminate the possibility of a future fall. This introduces uncertainty into the participant categorization, and future studies should consider longitudinal follow-up to more accurately capture fall risk over the long term, providing a better understanding of the factors that may predispose an individual to fall in the period following the initial assessment.
Turning back to the findings, this study makes several contributions to the field of mobility and fall risk prediction in older adults by integrating novel metrics from GPS and accelerometer data. First, our work expands on previous research by providing a detailed analysis of life-space mobility and gait patterns using the combined use of these two sensor modalities. By tracking community mobility with GPS and examining gait characteristics using accelerometer data, we were able to develop a more comprehensive model for predicting fall risk. This combination of spatial and temporal data has not been widely explored in the existing literature and allows for a richer understanding of how environmental factors and motor control intersect in the context of aging. Additionally, our study presents strong classification results for distinguishing between older adults with and without a history of falls, using machine learning algorithms such as Random Forest, K-Nearest Neighbors, and Support Vector Machines. Lastly, future research could focus on extending the temporal scope of this study by lengthening the observation period beyond a single day and collecting data across various environmental contexts. This approach would provide a more nuanced understanding of how mobility behaviors fluctuate over time and under different environmental conditions. Additionally, the findings of this study could inspire the development of intelligent wearable devices capable of real-time monitoring of gait and movement patterns, sending immediate alerts to caregivers or family members when high fall-risk patterns are detected. Such devices could employ advanced anomaly detection algorithms to identify sudden changes in the user’s mobility or stability. Furthermore, these data could be integrated into personalized rehabilitation programs, dynamically adjusting physical and therapeutic activities according to the user’s abilities and monitoring their progress. This would enable more effective and safer rehabilitation for individuals who have fallen or are at high risk of falling. In the long term, implementing AI-based predictive models could also aid in estimating future fall risk, facilitating early preventive interventions such as targeted exercise programs, home modifications, or adjustments in medical treatments to mitigate risk factors.