Lumbar Sitting Behavior of Individuals with Low Back Pain: A Preliminary Study Using Extended Real-World Data
Abstract
1. Introduction
- Study 1: Verification of the sitting detection algorithm to characterize the lumbar sitting behavior, with a blinded assessor.
- Study 2: Day-long assessment of the sitting behaviors of individuals with sitting related low back discomfort and feature extraction with an exploration of participant experiences.
- Study 3: Case study application to individuals with clinical LBP.
2. Materials and Methods
2.1. Design and Participants
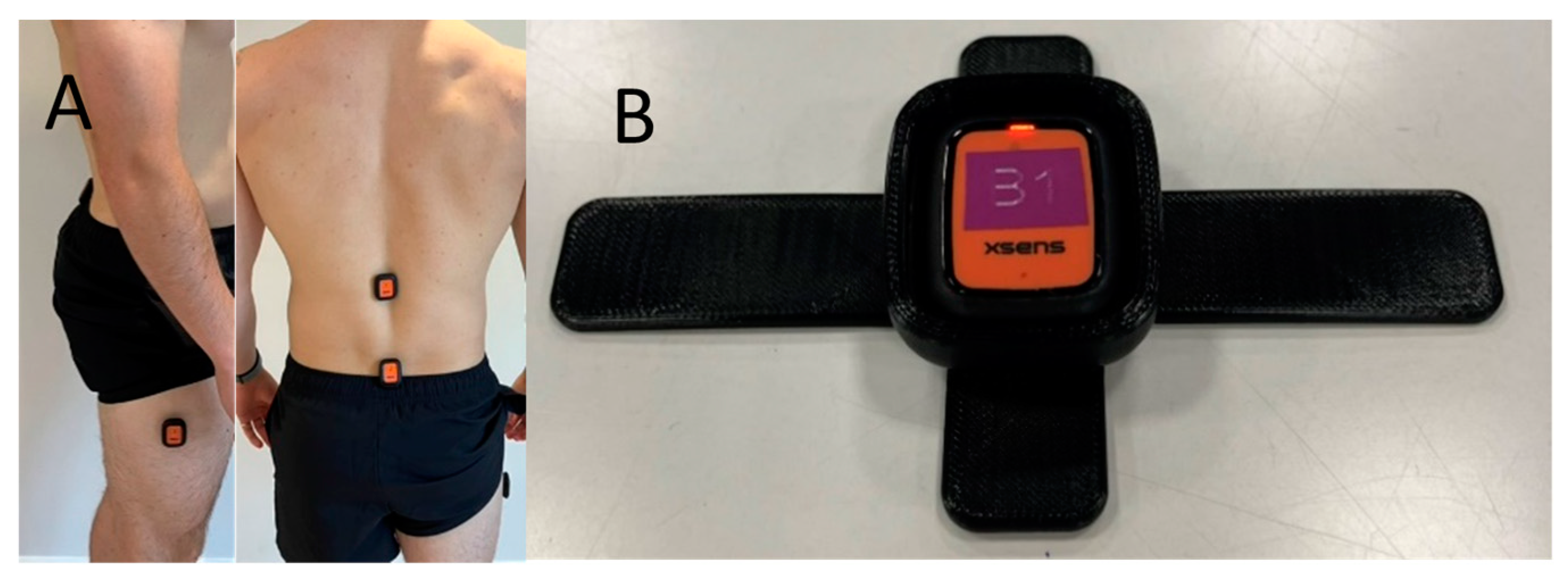
2.2. Sensor Placement and Data Processing
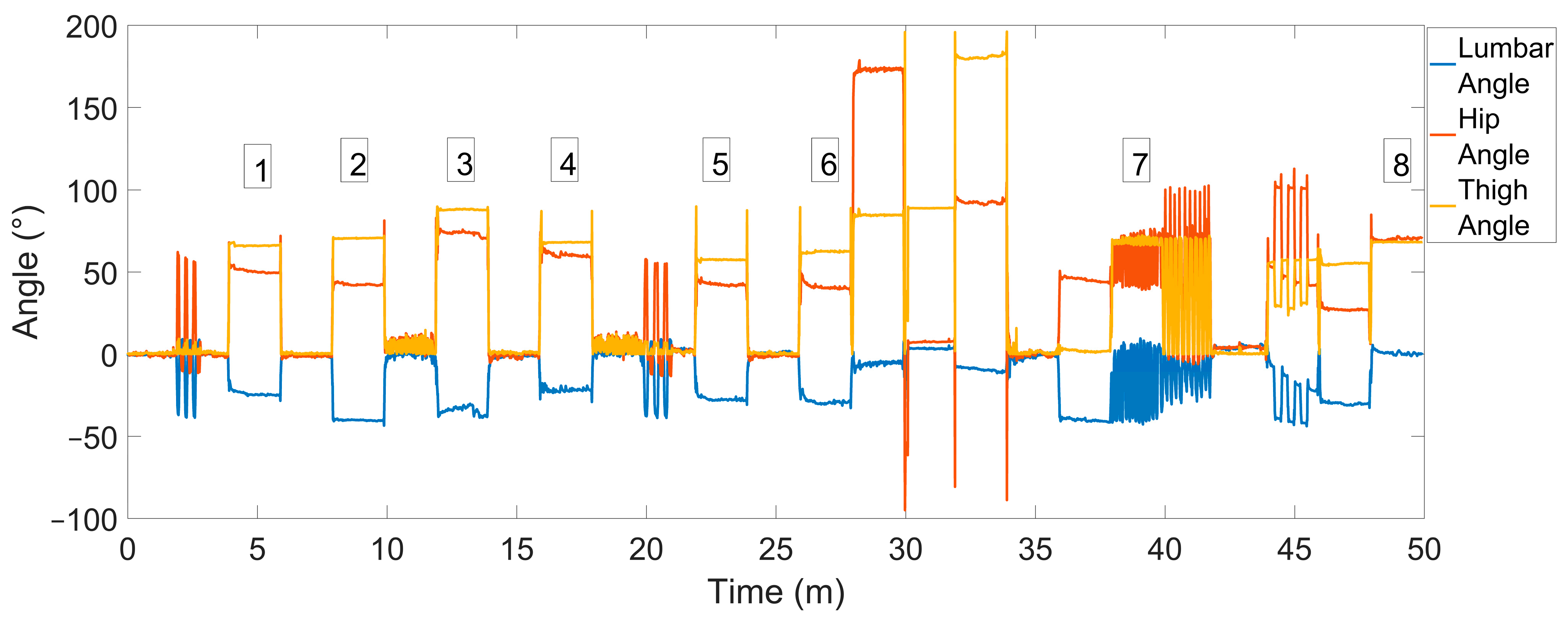
| Time | Activity | Period of Sitting (Figure 2) |
|---|---|---|
| 0–2 min | Standing | |
| 2–4 min | Flexion and extension cycles × 3 then standing | |
| 4–6 min | Sitting | 1 |
| 6–8 min | Standing | |
| 8–10 min | Slouched sitting | 2 |
| 10–12 min | Walking | |
| 12–14 min | Cross-legged sitting slouched—both legs on chair | 3 |
| 14–16 min | Standing | |
| 16–18 min | Cross-legged sitting erect—both legs on chair | 4 |
| 18–20 min | Walking | |
| 20–22 min | Flex and extension cycles × 3, then standing with pause | |
| 22–24 min | Sitting cross-legged, right over left | 5 |
| 24–26 min | Standing | |
| 26–28 min | Sitting cross-legged, left over right | 6 |
| 28–30 min | Prone lying | |
| 30–32 min | Supine lying | |
| 32–34 min | Supine lying with legs raised | |
| 34–36 min | Standing | |
| 36–38 min | Sustained forward bending | |
| 38–40 min | Highly variable sitting | 7 |
| 40–42 min | Sit to stand | |
| 42–44 min | Standing on one leg in the Trendelenburg posture, right | |
| 44–46 min | Full kneeling with head to floor, hold for 15 s, repeat × 3 | |
| 46–48 min | High stool sitting | |
| 48–50 min | Erect sitting | 8 |
3. Results
4. Materials and Methods
4.1. Design and Participants
4.2. Sensor Placement and Data Processing
4.3. Data Analysis
4.3.1. Focus Group
4.3.2. Visualization and Feature Extraction
5. Results
5.1. Focus Group
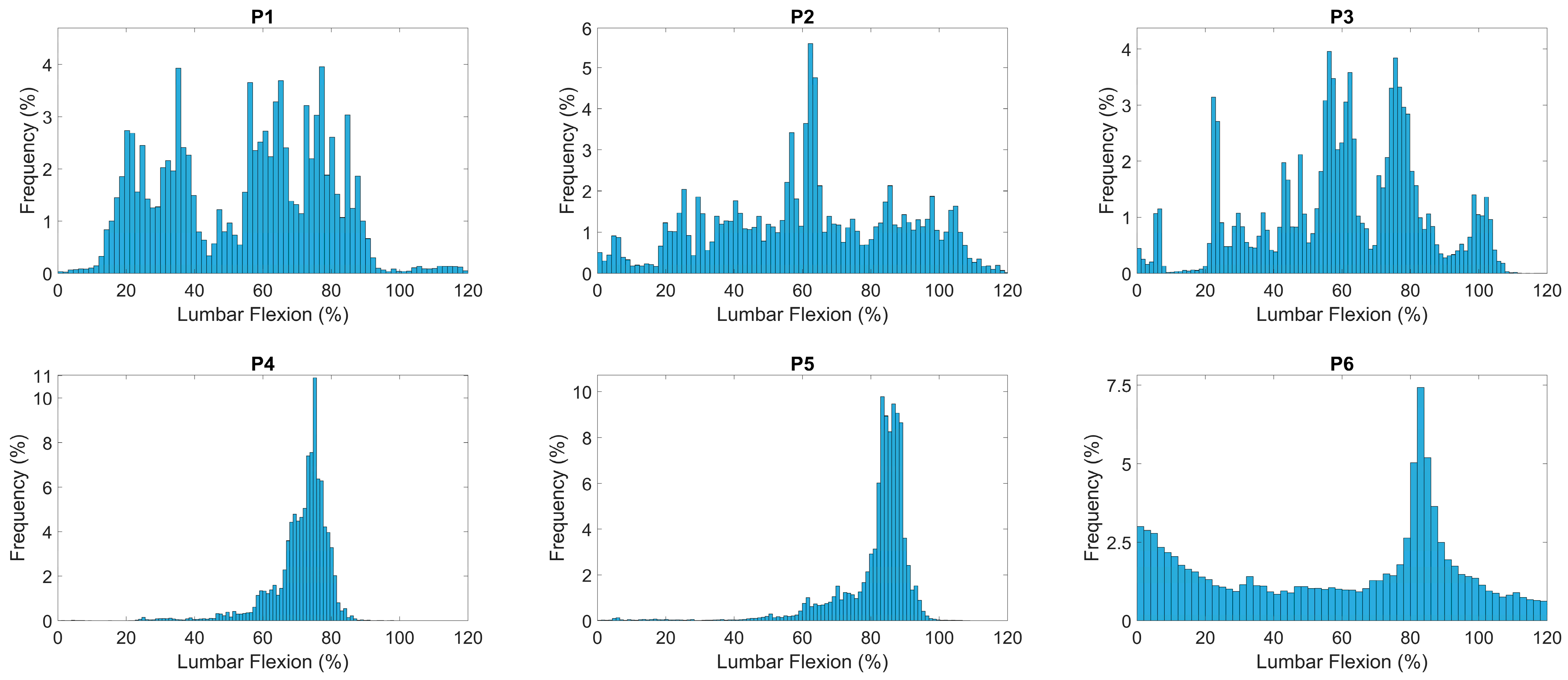
5.2. Visualization and Feature Engineering
6. Materials and Methods
6.1. Participants
6.2. Data Analysis
7. Results
8. Discussion
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- da Silva, T.; Mills, K.; Brown, B.T.; Pocovi, N.; de Campos, T.; Maher, C.; Hancock, M.J. Recurrence of low back pain is common: A prospective inception cohort study. J. Physiother. 2019, 65, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Hanna, F.; Daas, R.N.; El-Shareif, T.J.; Al-Marridi, H.H.; Al-Rojoub, Z.M.; Adegboye, O.A. The Relationship Between Sedentary Behavior, Back Pain, and Psychosocial Correlates Among University Employees. Front. Public Health 2019, 7, 80. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Kim, H.J.; Jeong, H.; Kim, H.; Chang, B.S.; Lee, C.K.; Yeom, J.S. Longer sitting time and low physical activity are closely associated with chronic low back pain in population over 50 years of age: A cross-sectional study using the sixth Korea National Health and Nutrition Examination Survey. Spine J. 2018, 18, 2051–2058. [Google Scholar] [CrossRef] [PubMed]
- Swain, C.T.V.; Pan, F.; Owen, P.J.; Schmidt, H.; Belavy, D.L. No consensus on causality of spine postures or physical exposure and low back pain: A systematic review of systematic reviews. J. Biomech. 2020, 102, 109312. [Google Scholar] [CrossRef]
- Zemp, R.; Fliesser, M.; Wippert, P.M.; Taylor, W.R.; Lorenzetti, S. Occupational sitting behavior and its relationship with back pain—A pilot study. App. Ergon. 2016, 56, 84–91. [Google Scholar] [CrossRef]
- Gupta, N.; Christiansen, C.S.; Hallman, D.M.; Korshøj, M.; Carneiro, I.G.; Holtermann, A. Is objectively measured sitting time associated with low back pain? A cross-sectional investigation in the NOMAD study. PLoS ONE 2015, 10, e0121159. [Google Scholar] [CrossRef]
- Womersley, L.; May, S. Sitting posture of subjects with postural backache. J. Manip. Physiol. Ther. 2006, 29, 213–218. [Google Scholar] [CrossRef]
- Astfalck, R.G.; O’Sullivan, P.B.; Straker, L.M.; Smith, A.J.; Burnett, A.; Caneiro, J.P.; Dankaerts, W. Sitting postures and trunk muscle activity in adolescents with and without nonspecific chronic low back pain: An analysis based on subclassification. Spine 2010, 35, 1387–1395. [Google Scholar] [CrossRef]
- Misir, A.; Kizkapan, T.B.; Tas, S.K.; Yildiz, I.; Ozcamdalli, M.; Yetis, M. Lumbar spine posture and spinopelvic parameters change in various standing and sitting postures. Eur. Spine J. 2019, 28, 1072–1081. [Google Scholar] [CrossRef]
- Mitchell, T.; O’Sullivan, P.B.; Burnett, A.F.; Straker, L.; Smith, A. Regional differences in lumbar spinal posture and the influence of low back pain. BMC Musculoskelet. Disord. 2008, 9, 152. [Google Scholar] [CrossRef] [PubMed]
- Tüzün, C.; Yorulmaz, I.; Cindaş, A.; Vatan, S. Low back pain and posture. Clin. Rheumatol. 1999, 18, 308–312. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, D.E.; Callaghan, J.P. Spine posture and discomfort during prolonged simulated driving with self-selected lumbar support prominence. Hum. Factors 2015, 57, 976–987. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, D.; Callaghan, J.P. Does a break from sitting change biomechanical outcome measures or transient pain? A laboratory-based experimental study. Work 2023, 75, 553–566. [Google Scholar] [CrossRef] [PubMed]
- Morl, F.; Bradl, I. Lumbar posture and muscular activity while sitting during office work. J. Electromyogr. Kinesiol. 2013, 23, 362–368. [Google Scholar] [CrossRef]
- Cowin, J.; Nimphius, S.; Fell, J.; Culhane, P.; Schmidt, M. A proposed framework to describe movement variability within sporting tasks: A scoping review. Sports Med. Open 2022, 8, 85. [Google Scholar] [CrossRef]
- De Carvalho, D.; Greene, R.; Swab, M.; Godwin, M. Does objectively measured prolonged standing for desk work result in lower ratings of perceived low back pain than sitting? A systematic review and meta-analysis. Work 2020, 67, 431–440. [Google Scholar] [CrossRef]
- Zhu, J.; Liu, X.; Shi, Q.; He, T.; Sun, Z.; Guo, X.; Liu, W.; Sulaiman, O.B.; Dong, B.; Lee, C. Development trends and perspectives of future sensors and MEMS/NEMS. Micromachines 2019, 11, 7. [Google Scholar] [CrossRef]
- Nixon, M.A.; McCallum, B.C.; Fright, W.R.; Price, N.B. The effect of metals and interfering fields on electromagnetic trackers. Presence 1998, 7, 204–218. [Google Scholar] [CrossRef]
- Milne, A.D.; Chess, D.G.; Johnson, J.A.; King, G.J. Accuracy of an electromagnetic tracking device: A study of the optimal range and metal interference. J. Biomech. 1996, 29, 791–793. [Google Scholar] [CrossRef]
- Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Plamondon, A. Effect of local magnetic field disturbances on inertial measurement units accuracy. Appl. Ergon. 2017, 63, 123–132. [Google Scholar] [CrossRef] [PubMed]
- McClintock, F.; Callaway, A.; Clark, C.; Williams, J. Assessing the Impact of Sensor Orientation on Accelerometer-Derived Angles: A Systematic Analysis and Proposed Error Reduction. App. Sci. 2024, 14, 842. [Google Scholar] [CrossRef]
- Williams, J.M.; Frey, M.; Breen, A.; De Carvalho, D. Systematic analysis of different low-pass filter cut-off frequencies on lumbar spine kinematics data and the impact on the agreement between accelerometers and an optoelectronic system. J. Biomech. 2022, 145, 111395. [Google Scholar] [CrossRef] [PubMed]
- Mingels, S.; Dankaerts, W.; van Etten, L.; Bruckers, L.; Granitzer, M. Lower spinal postural variability during laptop-work in subjects with cervicogenic headache compared to healthy controls. Sci. Rep. 2021, 11, 5159. [Google Scholar] [CrossRef]
- Dunk, N.M.; Callaghan, J.P. Lumbar spine movement patterns during prolonged sitting differentiate low back pain developers from matched asymptomatic controls. Work 2010, 35, 3–14. [Google Scholar] [CrossRef]
- Waddell, C.; Newton, M.; Henderson, I.; Somerville, D.; Main, C. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993, 52, 157–168. [Google Scholar] [CrossRef]
- Roland, M.; Fairbank, J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef]
- Wong, W.Y.; Wong, M.S. Detecting spinal posture change in sitting positions with tri-axial accelerometers. Gait Posture 2008, 27, 168–171. [Google Scholar] [CrossRef]
- Hong, K.R.; Hwang, I.W.; Kim, H.J.; Yang, S.H.; Lee, J.M. Apple Watch 6 vs. Galaxy Watch 4: A Validity Study of Step-Count Estimation in Daily Activities. Sensors 2024, 24, 4658. [Google Scholar] [CrossRef]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: A systematic review. BMC Musculoskel. Disord. 2019, 20, 55. [Google Scholar] [CrossRef]
- Bergman, J.H.M.; McGregor, A.H. Body-worn sensor design: What do patients and clinicians want? Ann. Biomed. Eng. 2011, 39, 2299–2312. [Google Scholar] [CrossRef] [PubMed]
- Dankaerts, W.; O’Sullivan, P.; Burnett, A.; Straker, L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine 2006, 31, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Casas, A.S.; Patino, M.S.; Camargo, D.M. Association between the sitting posture and back pain in college students. Rev. Univ. Ind. Santander Salud 2016, 48, 446–454. [Google Scholar] [CrossRef]
- Ippersiel, P.; Robbins, S.; Preuss, R. Movement variability in adults with low back pain during sit-to-stand-to-sit. Clin. Biomech. 2018, 58, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Ringheim, I.; Indahl, A.; Roeleveld, K. Reduced muscle activity variability in lumbar extensor muscles during sustained sitting in individuals with chronic low back pain. PLoS ONE 2019, 14, e0213778. [Google Scholar] [CrossRef]
- Oliosi, E.; Júlio, A.; Probst, P.; Silva, L.; Vilas-Boas, J.P.; Pinheiro, A.R.; Gamboa, H. Exploring the Real-Time Variability and Complexity of Sitting Patterns in Office Workers with Non-Specific Chronic Spinal Pain and Pain-Free Individuals. Sensors 2024, 24, 4750. [Google Scholar] [CrossRef]
- Stefanakis, M.; Luo, J.; Pollintine, P.; Dolan, P.; Adams, M.A. ISSLS Prize winner: Mechanical influences in progressive intervertebral disc degeneration. Spine 2014, 39, 1365–1372. [Google Scholar] [CrossRef]
- Greene, R.; Frey, M.; Attarsharghi, S.; Snow, J.C.; Barrett, M.; De Carvalho, D. Transient perceived back pain induced by prolonged sitting in a backless office chair: Are biomechanical factors involved? Ergonomics 2019, 62, 1415–1425. [Google Scholar] [CrossRef]



| Sitting Region | Duration (min) | Mean Lumbar Flexion (°) | Mean Lumbar Flexion (%) | Standard Deviation (°) | Known Sitting Position | Sitting Identified by Algorithm |
|---|---|---|---|---|---|---|
| 1 | 1.99 | 23.95 | 64.70 | 1.49 | Normal sitting | Yes |
| 2 | 1.99 | 40.04 | 108.20 | 1.59 | Slouched sitting | Yes |
| 3 | 2.01 | 33.57 | 90.71 | 3.99 | Double cross-legged sitting slouched | Yes |
| 4 | 2.01 | 21.75 | 58.78 | 1.20 | Double cross-legged sitting erect | Yes |
| 5 | 1.90 | 27.41 | 74.08 | 0.81 | Single cross-legged sitting ankle to knee | No (Thigh angle < 60°) |
| 6 | 1.94 | 28.79 | 77.79 | 1.93 | Single cross-legged sitting normal | Yes |
| 7 | 1.95 | 17.80 | 48.09 | 19.19 | Slouched and erect sitting cycles | Yes |
| 8 | 1.97 | 0.68 | 1.83 | 1.50 | Erect sitting | Yes |
| P | No. of Sitting Windows | Mean Sitting Window Duration (min) (SD) | Weighted Average Posture for the Day (%Flexion) | Average Posture for the Day (%Flexion) | Variability of Postures through Day (%Flexion) | Average Fidgeting through Day (%Flexion) | Weighted Average SLPE | Average SLPE | Variability of SLPE through Day |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 | 4.11 (3.27) | 54.78 (23.60) | 60.67 | 18.25 | 6.18 | 125.19 | 35.51 | 21.11 |
| 2 | 22 | 6.44 (6.47) | 60.94 (26.54) | 59.05 | 24.99 | 11.12 | 319.69 | 40.78 | 161.17 |
| 3 | 20 | 9.84 (7.90) | 60.23 (23.91) | 68.14 | 21.33 | 6.87 | 505.98 | 117.76 | 84.01 |
| 4 | 33 | 2.40 (1.68) | 70.91 (8.93) | 71.61 | 5.86 | 4.90 | 669.50 | 50.07 | 41.55 |
| 5 | 22 | 4.66 (5.97) | 81.34 (11.67) | 81.01 | 7.97 | 10.06 | 746.10 | 48.70 | 76.21 |
| 6 | 37 | 6.02 (5.03) | 61.86 (37.34) | 51.37 | 28.13 | 28.48 | 366.97 | 17.38 | 29.53 |
| Characteristic | Pt1 | Pt2 |
|---|---|---|
| Sex | M | F |
| Age (years) | 53 | 35 |
| Height (m) | 1.71 | 1.81 |
| Weight (kg) | 85 | 86 |
| Duration (years) | 10 | 0.75 |
| VAS (average) | 54 | 18 |
| VAS (worst) | 63 | 42 |
| FABQ | 46 | 29 |
| RMDQ | 8 | 8 |
| Aggravating Factors | Sitting Standing Walking | Sitting Standing |
| P | Sitting Windows | No. of Sitting Windows | Mean Sitting Window Duration (min) | Weighted Average Posture for the Day (%Flexion) | Average Posture for the Day (%Flexion) | Variability of Postures through Day (%Flexion) | Average Fidgeting through Day (%Flexion) | Weighted Average SLPE | Average SLPE | Variability of SLPE |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Overall | 27 | 4.82 | 70.67 | 60.10 | 25.21 | 9.94 | 268.32 | 80.37 | 98.83 |
| Painful | 3 | 7.26 | 61.86 | 57.28 | 24.28 | 21.46 | 70.82 | 135 | 162.21 | |
| Pain Free | 24 | 4.52 | 72.26 | 60.44 | 25.24 | 8.51 | 216.77 | 73.55 | 85.33 | |
| 2 | Overall | 27 | 7.14 | 86.54 | 85.11 | 9.74 | 3.52 | 1745.8 | 324.37 | 330.64 |
| Painful | 6 | 8.91 | 83.56 | 86.42 | 8.03 | 3.93 | 271.79 | 302.11 | 308.97 | |
| Pain Free | 21 | 6.63 | 87.23 | 84.73 | 10.16 | 3.41 | 1761.60 | 330.74 | 336.31 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McClintock, F.A.; Callaway, A.J.; Clark, C.J.; Alqhtani, R.S.; Williams, J.M. Lumbar Sitting Behavior of Individuals with Low Back Pain: A Preliminary Study Using Extended Real-World Data. Sensors 2024, 24, 6751. https://doi.org/10.3390/s24206751
McClintock FA, Callaway AJ, Clark CJ, Alqhtani RS, Williams JM. Lumbar Sitting Behavior of Individuals with Low Back Pain: A Preliminary Study Using Extended Real-World Data. Sensors. 2024; 24(20):6751. https://doi.org/10.3390/s24206751
Chicago/Turabian StyleMcClintock, Frederick A., Andrew J. Callaway, Carol J. Clark, Raee S. Alqhtani, and Jonathan M. Williams. 2024. "Lumbar Sitting Behavior of Individuals with Low Back Pain: A Preliminary Study Using Extended Real-World Data" Sensors 24, no. 20: 6751. https://doi.org/10.3390/s24206751
APA StyleMcClintock, F. A., Callaway, A. J., Clark, C. J., Alqhtani, R. S., & Williams, J. M. (2024). Lumbar Sitting Behavior of Individuals with Low Back Pain: A Preliminary Study Using Extended Real-World Data. Sensors, 24(20), 6751. https://doi.org/10.3390/s24206751






