The Overlay, a New Solution for Volume Variations in the Residual Limb for Individuals with a Transtibial Amputation
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
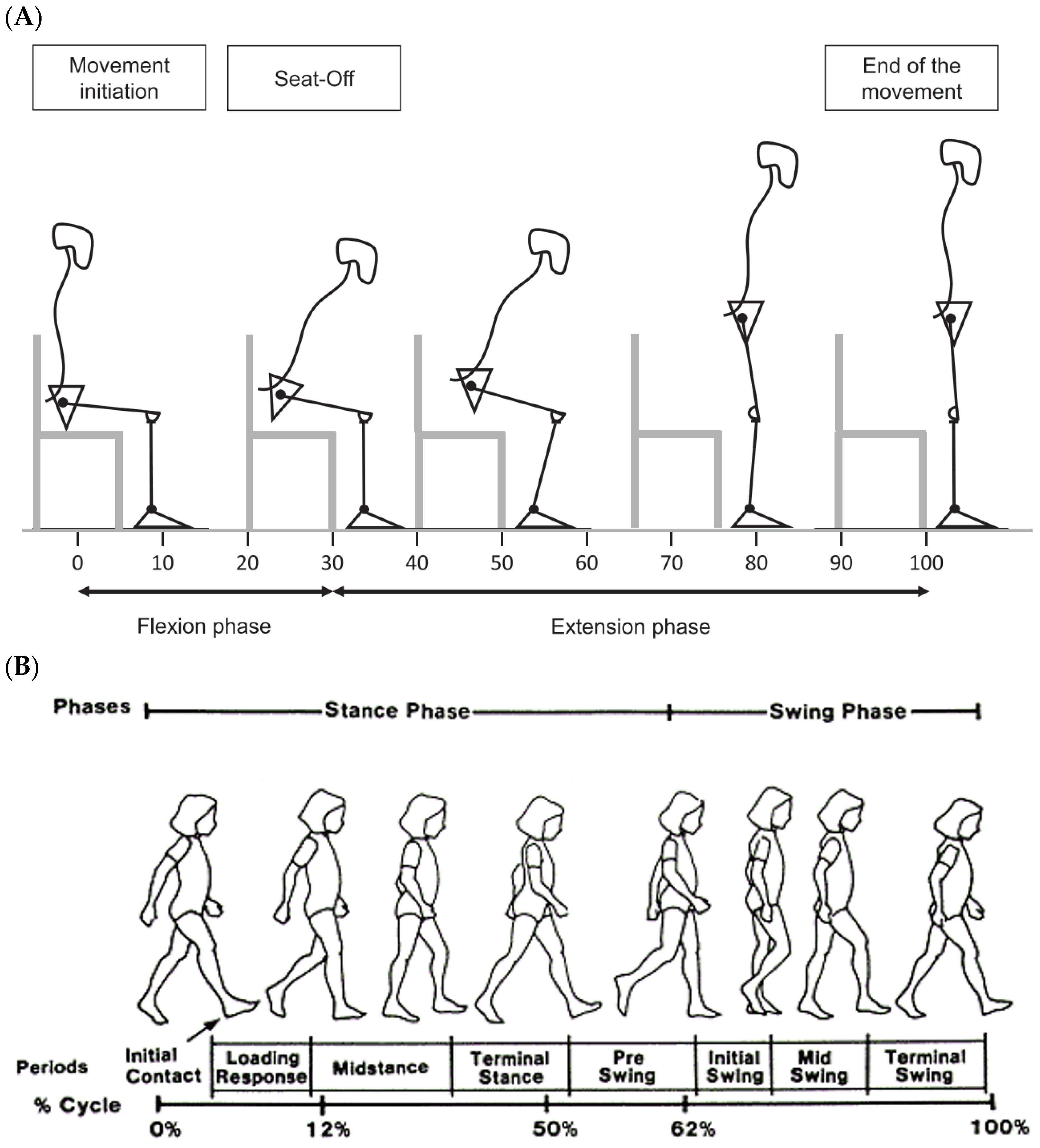
2.2. Protocol
2.3. Materials
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
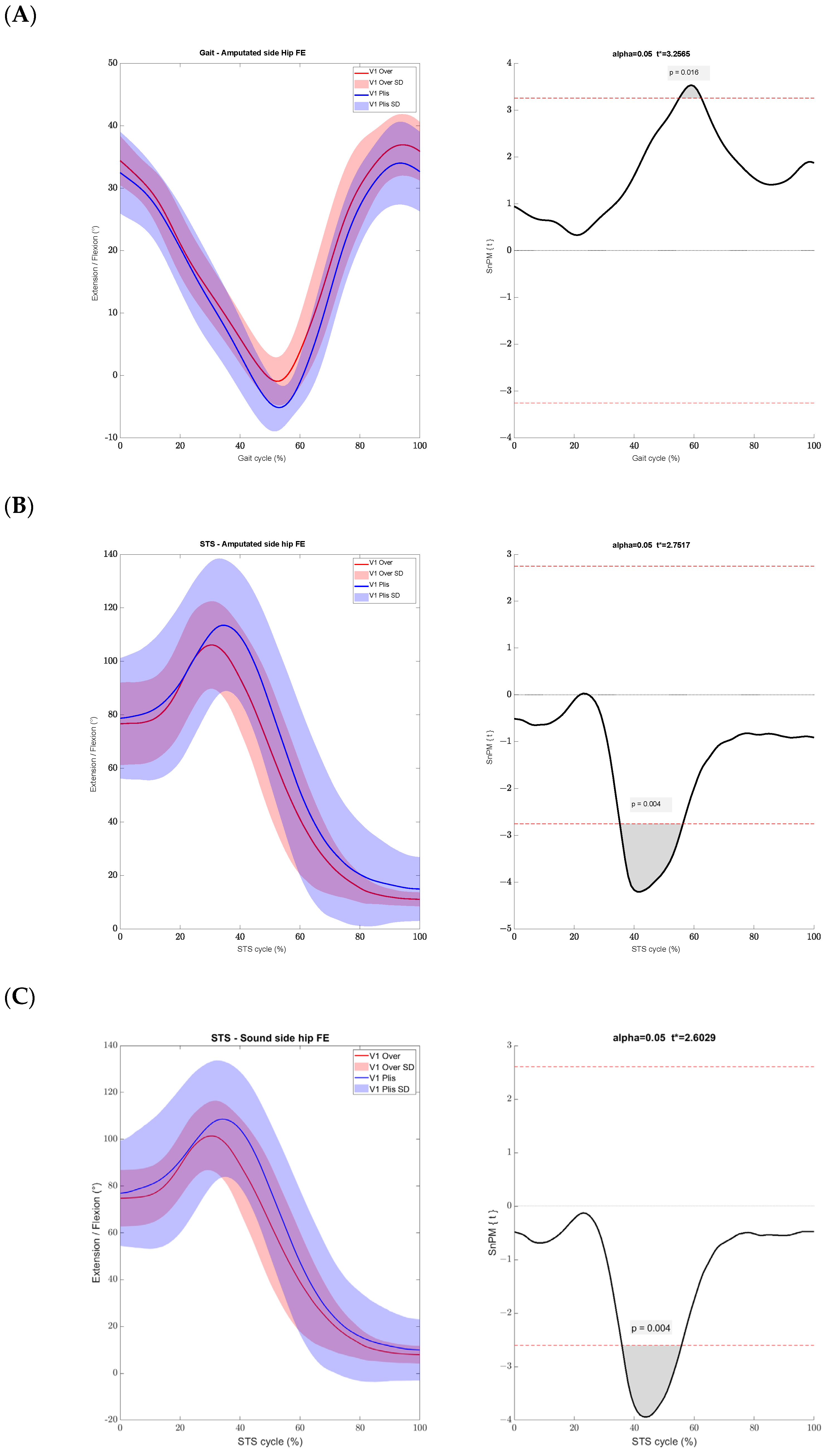
3.1. Comfortable Gait
3.2. 6MWT Task
3.3. Sit-to-Stand Task
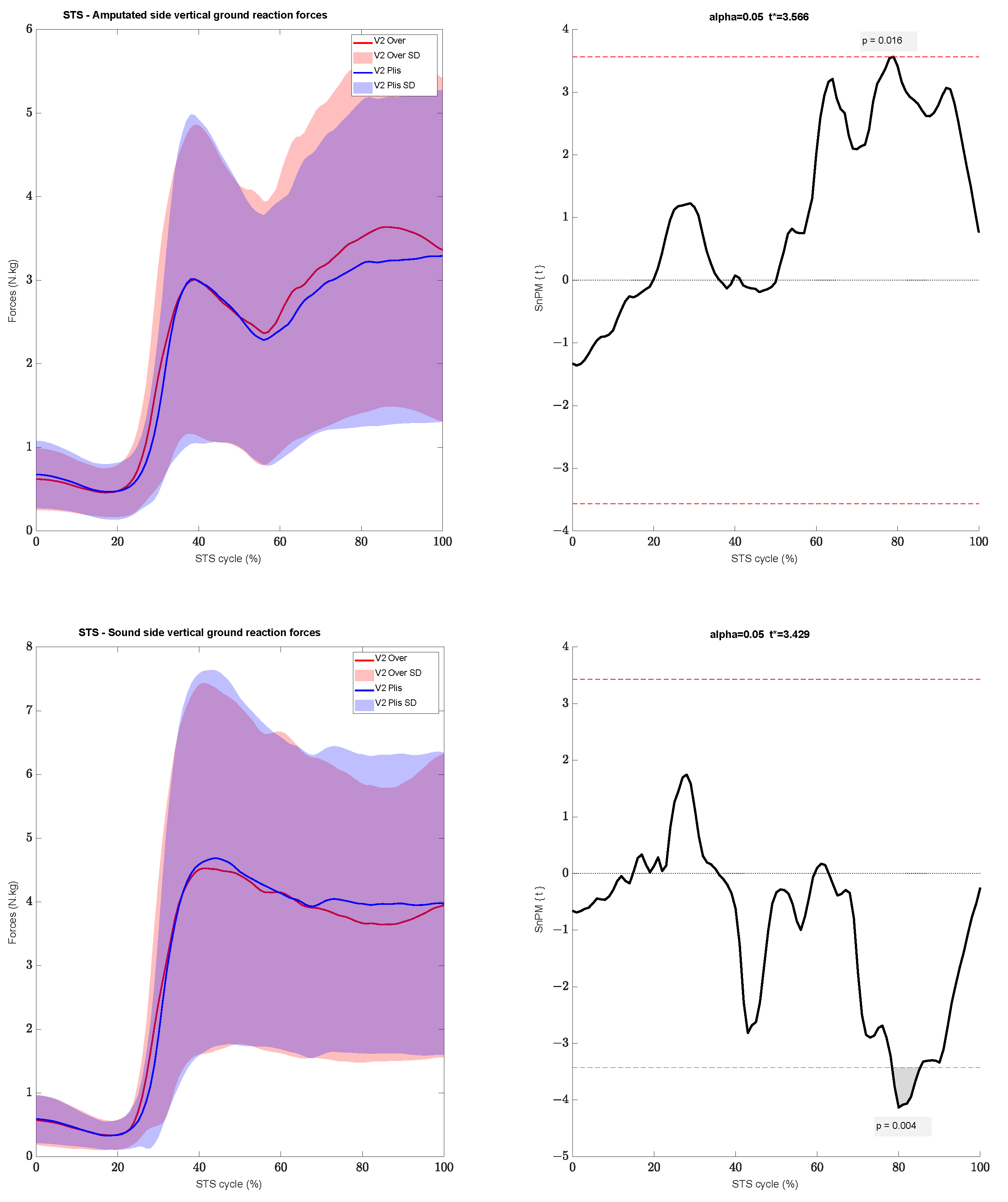
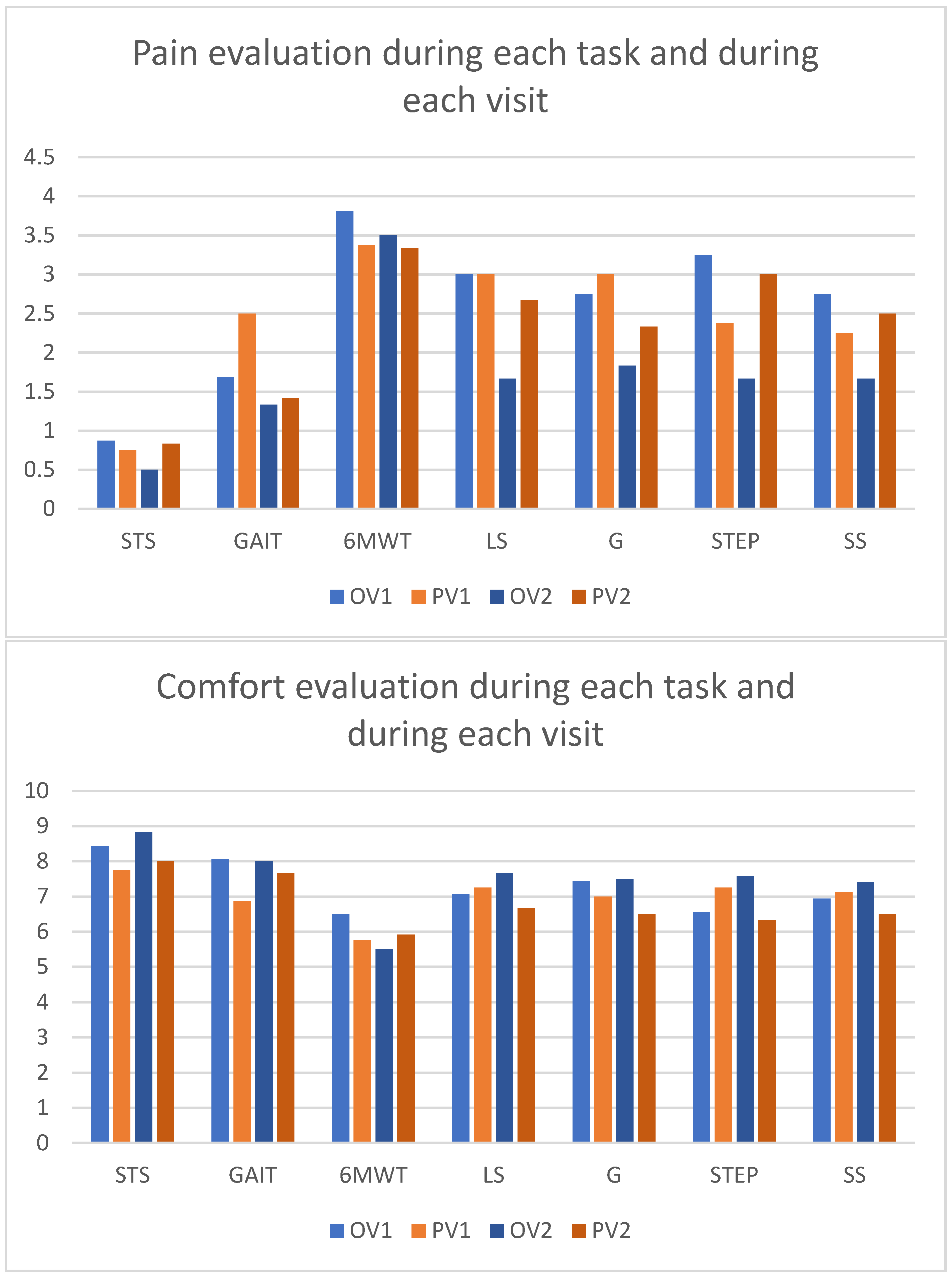
3.4. Pain, Comfort, and Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Inclusion | Exclusion |
|---|---|
| Be at least 18 years old | No stump injury |
| TTA | Underwent amputation at least 1 year ago |
| Activity level K2–K4 [17] | Harmony or thigh corset |
| Diameter of residual limb between 18–34 cm | Length of residual limb below knee at least 10 cm |
| At least 3 folds of variations during a day | 84 (±16) |
Appendix B. Instructions
References
- Imam, B.; Miller, W.C.; Finlayson, H.C.; Eng, J.J.; Jarus, T. Incidence of Lower Limb Amputation in Canada. Can. J. Public Health 2017, 108, e374–e380. [Google Scholar] [CrossRef] [PubMed]
- Grzebień, A.; Chabowski, M.; Malinowski, M.; Uchmanowicz, I.; Milan, M.; Janczak, D. Analysis of Selected Factors Determining Quality of Life in Patients after Lower Limb Amputation—A Review Article. Pol. J. Surg. 2017, 89, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.K.; Charan, M.; Kanagaraj, S. Trends and Challenges in Lower Limb Prosthesis. IEEE Potentials 2017, 36, 19–23. [Google Scholar] [CrossRef]
- De Marchis, C.; Ranaldi, S.; Varrecchia, T.; Serrao, M.; Castiglia, S.F.; Tatarelli, A.; Ranavolo, A.; Draicchio, F.; Lacquaniti, F.; Conforto, S. Characterizing the Gait of People with Different Types of Amputation and Prosthetic Components through Multimodal Measurements: A Methodological Perspective. Front. Rehabil. Sci. 2022, 3, 804746. [Google Scholar] [CrossRef] [PubMed]
- Miramand, L.; Moisan, G.; Richard, V.; McFadyen, B.J.; Turcot, K. Whole Body Movement Strategies during Sit-to-Stand and Stair Ascent in Individuals with a Lower Limb Amputation: A Systematic Review. Clin. Biomech. 2022, 100, 105811. [Google Scholar] [CrossRef] [PubMed]
- Hashimto, A.H.; Kobayashi, T.; Gao, F. The Effect of Transverse Prosthetic Alignment Changes on Socket Reaction Moments during Gait in Individuals with Transtibial Amputation. Gait Posture 2018, 65, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Orendurff, M.S.; Boone, D.A. Effect of Alignment Changes on Socket Reaction Moments during Gait in Transfemoral and Knee-Disarticulation Prostheses: Case Series. J. Biomech. 2013, 46, 2539–2545. [Google Scholar] [CrossRef] [PubMed]
- Gailey, R.; Allen, K.; Castles, J.; Kucharik, J.; Roeder, M. Review of Secondary Physical Conditions Associated with Lower-Limb Amputation and Long-Term Prosthesis Use. J. Rehabil. Res. Dev. 2008, 45, 15–30. [Google Scholar] [CrossRef]
- Sanders, J.E.; Cagle, J.C.; Allyn, K.J.; Harrison, D.S.; Ciol, M.A. How Do Walking, Standing, and Resting Influence Transtibial Amputee Residual Limb Fluid Volume? J. Rehabil. Res. Dev. 2014, 51, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.E.; Fatone, S. Residual Limb Volume Change: Systematic Review of Measurement and Management. J. Rehabil. Res. Dev. 2011, 48, 949. [Google Scholar] [CrossRef]
- Sanders, J.E.; Youngblood, R.T.; Hafner, B.J.; Ciol, M.A.; Allyn, K.J.; Gardner, D.; Cagle, J.C.; Redd, C.B.; Dietrich, C.R. Residual Limb Fluid Volume Change and Volume Accommodation. Prosthet. Orthot. Int. 2018, 42, 415–427. [Google Scholar] [CrossRef] [PubMed]
- Youngblood, R.T.; Hafner, B.J.; Allyn, K.J.; Cagle, J.C.; Hinrichs, P.; Redd, C.; Vamos, A.C.; Ciol, M.A.; Bean, N.; Sanders, J.E. Effects of Activity Intensity, Time, and Intermittent Doffing on Daily Limb Fluid Volume Change in People with Transtibial Amputation. Prosthet. Orthot. Int. 2019, 43, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Klenow, T.; Schulz, J. Adjustable-Volume Prosthetic Sockets: Market Overview and Value Propositions. Can. Prosthet. Orthot. J. 2021, 4, 17. [Google Scholar] [CrossRef] [PubMed]
- Dillingham, T.; Kenia, J.; Shofer, F.; Marschalek, J. A Prospective Assessment of an Adjustable, Immediate Fit, Transtibial Prosthesis. PM&R 2019, 11, 1210–1217. [Google Scholar] [CrossRef]
- Seo, J.; Lee, H.; Seo, D.W.; Lee, D.; Kwon, O.; Kwak, M.K.; Lee, K.H. A Prosthetic Socket with Active Volume Compensation for Amputated Lower Limb. Sensors 2021, 21, 407. [Google Scholar] [CrossRef] [PubMed]
- Pirouzi, G.; Abu Osman, N.A.; Oshkour, A.A.; Ali, S.; Gholizadeh, H.; Wan Abas, W.A.B. Development of an Air Pneumatic Suspension System for Transtibial Prostheses. Sensors 2014, 14, 16754–16765. [Google Scholar] [CrossRef] [PubMed]
- Dillon, M.P.; Major, M.J.; Kaluf, B.; Balasanov, Y.; Fatone, S. Predict the Medicare Functional Classification Level (K-Level) Using the Amputee Mobility Predictor in People with Unilateral Transfemoral and Transtibial Amputation: A Pilot Study. Prosthet. Orthot. Int. 2018, 42, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, T.; Bellmann, M.; Proebsting, E.; Blumentritt, S. Effects of Adaptation to a Functionally New Prosthetic Lower-Limb Component. JPO J. Prosthet. Orthot. 2014, 26, 134–143. [Google Scholar] [CrossRef]
- Kammin, E.J. The 6-Minute Walk Test: Indications and Guidelines for Use in Outpatient Practices. J. Nurse Pract. 2022, 18, 608–610. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB Recommendation on Definitions of Joint Coordinate System of Various Joints for the Reporting of Human Joint Motion—Part I: Ankle, Hip, and Spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Moisan, G.; Miramand, L.; Younesian, H.; Legrand, T.; Turcot, K. Assessment of Biomechanical Deficits in Individuals with a Trans-Tibial Amputation during Level Gait Using One-Dimensional Statistical Parametric Mapping. Gait Posture 2021, 87, 130–135. [Google Scholar] [CrossRef]
- Turcot, K.; Armand, S.; Fritschy, D.; Hoffmeyer, P.; Suvà, D. Sit-to-Stand Alterations in Advanced Knee Osteoarthritis. Gait Posture 2012, 36, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Burnfield, J. Gait Analysis: Normal and Pathological Function. J. Pediatr. Orthop. 1992, 12, 815. [Google Scholar] [CrossRef]
- Pataky, T.C.; Vanrenterghem, J.; Robinson, M.A. Zero- vs. One-Dimensional, Parametric vs. Non-Parametric, and Confidence Interval vs. Hypothesis Testing Procedures in One-Dimensional Biomechanical Trajectory Analysis. J. Biomech. 2015, 48, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, E.C.; Nederhand, M.J.; Rietman, J.S. Adaptation Strategies of the Lower Extremities of Patients with a Transtibial or Transfemoral Amputation during Level Walking: A Systematic Review. Arch. Phys. Med. Rehabil. 2011, 92, 1311–1325. [Google Scholar] [CrossRef] [PubMed]
- Özyürek, S.; Demirbüken, I.; Angin, S. Altered Movement Strategies in Sit-to-Stand Task in Persons with Transtibial Amputation. Prosthet. Orthot. Int. 2014, 38, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, V.; Gailey, R.; Gaunaurd, I.; Gailey, R.; O’Toole, C. Weight Distribution Symmetry during the Sit-to-Stand Movement of Unilateral Transtibial Amputees. Ergonomics 2011, 54, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Gailey, R.; Kristal, A.; Lucarevic, J.; Harris, S.; Applegate, B.; Gaunaurd, I. The Development and Internal Consistency of the Comprehensive Lower Limb Amputee Socket Survey in Active Lower Limb Amputees. Prosthet. Orthot. Int. 2019, 43, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.E.; Redd, C.B.; Cagle, J.C.; Hafner, B.J.; Gardner, D.; Allyn, K.J.; Harrison, D.S.; Ciol, M.A. Preliminary Evaluation of a Novel Bladder-Liner for Facilitating Residual Limb Fluid Volume Recovery without Doffing. J. Rehabil. Res. Dev. 2016, 53, 1107–1120. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.E.; Youngblood, R.T.; Hafner, B.J.; Cagle, J.C.; McLean, J.B.; Redd, C.B.; Dietrich, C.R.; Ciol, M.A.; Allyn, K.J. Effects of Socket Size on Metrics of Socket Fit in Trans-Tibial Prosthesis Users. Med. Eng. Phys. 2017, 44, 32–43. [Google Scholar] [CrossRef]

| Characteristics | |
|---|---|
| Gender | 3 Females–5 Males |
| Etiology | 3 Traumatic–4 Medical |
| Age | 56 (±10) |
| Height (m) | 1.70 (±0.1) |
| Weight (kg) | 84 (±16) |
| Time since amputation (year) | 13 (±9) |
| Number of folds | 5 (±2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badaire, P.; Robert, M.T.; Turcot, K. The Overlay, a New Solution for Volume Variations in the Residual Limb for Individuals with a Transtibial Amputation. Sensors 2024, 24, 4744. https://doi.org/10.3390/s24144744
Badaire P, Robert MT, Turcot K. The Overlay, a New Solution for Volume Variations in the Residual Limb for Individuals with a Transtibial Amputation. Sensors. 2024; 24(14):4744. https://doi.org/10.3390/s24144744
Chicago/Turabian StyleBadaire, Pierre, Maxime T. Robert, and Katia Turcot. 2024. "The Overlay, a New Solution for Volume Variations in the Residual Limb for Individuals with a Transtibial Amputation" Sensors 24, no. 14: 4744. https://doi.org/10.3390/s24144744
APA StyleBadaire, P., Robert, M. T., & Turcot, K. (2024). The Overlay, a New Solution for Volume Variations in the Residual Limb for Individuals with a Transtibial Amputation. Sensors, 24(14), 4744. https://doi.org/10.3390/s24144744






