Reliability of Ultrasound Measurements of the Median Nerve in Asymptomatic Subjects Using a Handheld Device
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Subjects
2.3. Instruments and Operators
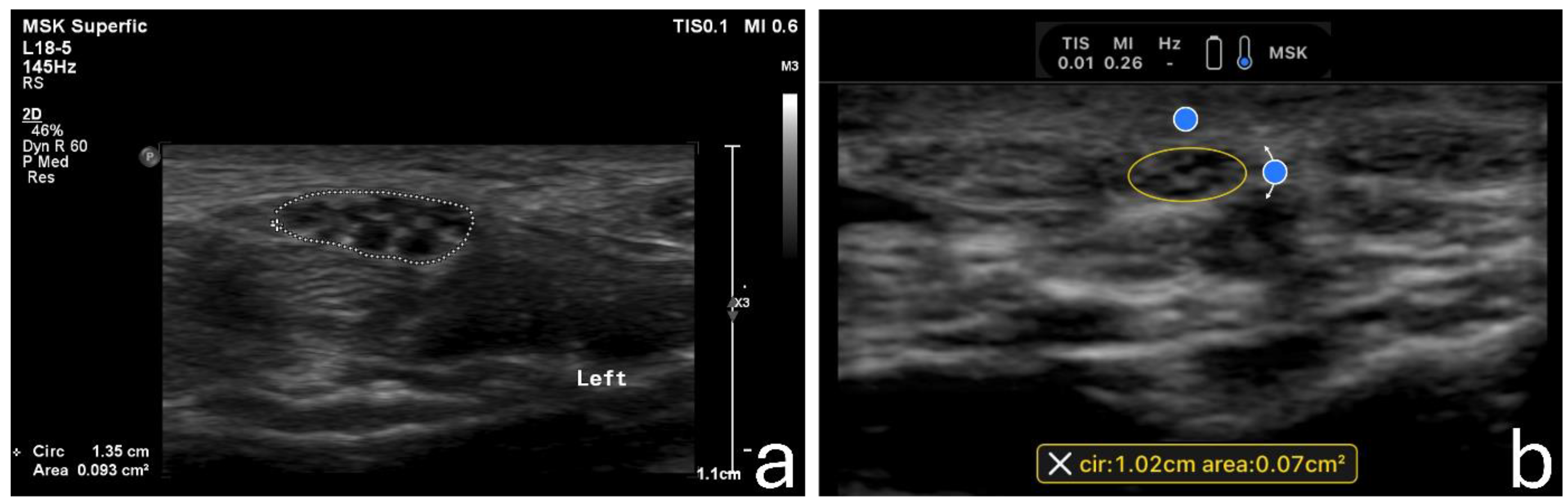
2.4. Image Acquisition
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roomizadeh, P.; Eftekharsadat, B.; Abedini, A.; Ranjbar-Kiyakalayeh, S.; Yousefi, N.; Ebadi, S.; Babaei-Ghazani, A. Ultrasonographic Assessment of Carpal Tunnel Syndrome Severity: A Systematic Review and Meta-Analysis. Am. J. Phys. Med. Rehabil. 2019, 98, 373–381. [Google Scholar] [CrossRef]
- Lin, T.-Y.; Chang, K.-V.; Wu, W.-T.; Özçakar, L. Ultrasonography for the Diagnosis of Carpal Tunnel Syndrome: An Umbrella Review. J. Neurol. 2022, 269, 4663–4675. [Google Scholar] [CrossRef]
- Bueno-Gracia, E.; Malo-Urriés, M.; Ruiz-de-Escudero-Zapico, A.; Rodríguez-Marco, S.; Jiménez-del-Barrio, S.; Shacklock, M.; Estébanez-de-Miguel, E.; Tricás-Moreno, J.M. Reliability of Measurement of the Carpal Tunnel and Median Nerve in Asymptomatic Subjects with Ultrasound. Musculoskelet. Sci. Pract. 2017, 32, 17–22. [Google Scholar] [CrossRef]
- Fowler, J.R.; Hirsch, D.; Kruse, K. The Reliability of Ultrasound Measurements of the Median Nerve at the Carpal Tunnel Inlet. J. Hand Surg. Am. 2015, 40, 1992–1995. [Google Scholar] [CrossRef]
- Fowler, J.R.; Gaughan, J.P.; Ilyas, A.M. The Sensitivity and Specificity of Ultrasound for the Diagnosis of Carpal Tunnel Syndrome: A Meta-Analysis. Clin. Orthop. Relat. Res. 2011, 469, 1089–1094. [Google Scholar] [CrossRef]
- Zaki, H.A.; Shaban, E.; Salem, W.; Bilal, F.; Fayed, M.; Hendy, M.; Abdelrahim, M.G.; Masood, M.; Shallik, N.A. A Comparative Analysis between Ultrasound and Electromyographic and Nerve Conduction Studies in Diagnosing Carpal Tunnel Syndrome (CTS): A Systematic Review and Meta-Analysis. Cureus 2022, 14, e30476. [Google Scholar] [CrossRef]
- Rykkje, A.; Carlsen, J.F.; Nielsen, M.B. Hand-Held Ultrasound Devices Compared with High-End Ultrasound Systems: A Systematic Review. Diagnostics 2019, 9, 61. [Google Scholar] [CrossRef]
- Alfuraih, A.M.; Alqarni, M.A.; Alhuthaili, H.S.; Mubaraki, M.Y.; Alotaibi, N.N.; Almusalim, F.M. Reproducibility and Feasibility of a Handheld Ultrasound Device Compared to a Standard Ultrasound Machine in Muscle Thickness Measurements. Australas. J. Ultrasound Med. 2023, 26, 13–20. [Google Scholar] [CrossRef]
- Alfuraih, A.M.; Alrashed, A.I.; Almazyad, S.O.; Alsaadi, M.J. Abdominal Aorta Measurements by a Handheld Ultrasound Device Compared with a Conventional Cart-Based Ultrasound Machine. Ann. Saudi Med. 2021, 41, 376–382. [Google Scholar] [CrossRef]
- Falkowski, A.L.; Jacobson, J.A.; Freehill, M.T.; Kalia, V. Hand-Held Portable versus Conventional Cart-Based Ultrasound in Musculoskeletal Imaging. Orthop. J. Sports Med. 2020, 8, 2325967119901017. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Measuring Agreement in Method Comparison Studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef]
- Zardi, E.M.; Franceschetti, E.; Giorgi, C.; Palumbo, A.; Franceschi, F. Accuracy and Performance of a New Handheld Ultrasound Machine with Wireless System. Sci. Rep. 2019, 9, 14599. [Google Scholar] [CrossRef]
- Alemán, L.; Berná, J.D.; Reus, M.; Martínez, F.; Doménech-Ratto, G.; Campos, M. Reproducibility of Sonographic Measurements of the Median Nerve. J. Ultrasound Med. 2008, 27, 193–197. [Google Scholar] [CrossRef]
- Ngaage, L.M.; Casey, P.M.; Giladi, A.M. Utility of Ultrasound for Identifying Median Nerve Changes Indicative of Acute Carpal Tunnel Syndrome after Distal Radius Fracture. J. Hand Surg. Glob. Online 2023, 5, 430–434. [Google Scholar] [CrossRef]
- Ng, A.J.T.; Chandrasekaran, R.; Prakash, A.; Mogali, S.R. A Systematic Review: Normative Reference Values of the Median Nerve Cross-Sectional Area Using Ultrasonography in Healthy Individuals. Sci. Rep. 2022, 12, 9217. [Google Scholar] [CrossRef]
- Duncan, I.; Sullivan, P.; Lomas, F. Sonography in the Diagnosis of Carpal Tunnel Syndrome. Am. J. Roentgenol. 1999, 173, 681–684. [Google Scholar] [CrossRef]
- Asbeutah, A.; Dashti, M.; AlMajran, A.; Ghayyath, A. Sonographic Measurement of Cross-Sectional Area of the Median Nerve in Academic Dentists Without Symptoms or Signs of Carpal Tunnel Syndrome. J. Diagn. Med. Sonogr. 2018, 35, 105–111. [Google Scholar] [CrossRef]
- Karahan, A.Y.; Arslan, S.; Ordahan, B.; Bakdik, S.; Ekiz, T. Superb Microvascular Imaging of the Median Nerve in Carpal Tunnel Syndrome: An Electrodiagnostic and Ultrasonographic Study. J. Ultrasound Med. 2018, 37, 2855–2861. [Google Scholar] [CrossRef]
- Endo, T.; Matsui, Y.; Kawamura, D.; Urita, A.; Momma, D.; Ota, M.; Shibayama, H.; Iwai, T.; Nishida, M.; Iwasaki, N. Diagnostic Utility of Superb Microvascular Imaging and Power Doppler Ultrasonography for Visualizing Enriched Microvascular Flow in Patients with Carpal Tunnel Syndrome. Front. Neurol. 2022, 13, 832569. [Google Scholar] [CrossRef] [PubMed]
- Gitto, S.; Messina, C.; Chianca, V.; Tuscano, B.; Lazzara, A.; Corazza, A.; Pedone, L.; Albano, D.; Sconfienza, L.M. Superb Microvascular Imaging (SMI) in the Evaluation of Musculoskeletal Disorders: A Systematic Review. Radiol. Med. 2020, 125, 481–490. [Google Scholar] [CrossRef] [PubMed]
| EPIQ 7, Philips Healthcare | Butterfly iQ, Butterfly Network Inc. | |
|---|---|---|
| Transducer technology | Broadband 288 piezoelectric elements | 9000 = element Capacitive Micromachined Ultrasonic Transducer (CMUT) |
| Transducer type | Linear transducer | Multi-modal 2-D array |
| Frequency range (MHz) | 18–5 | 10–1 |
| Weight (kg) | 104.3 | 0.3 |
| Dimensions (mm) | 606 × 1500 × 1009 | 163 × 56 × 35 |
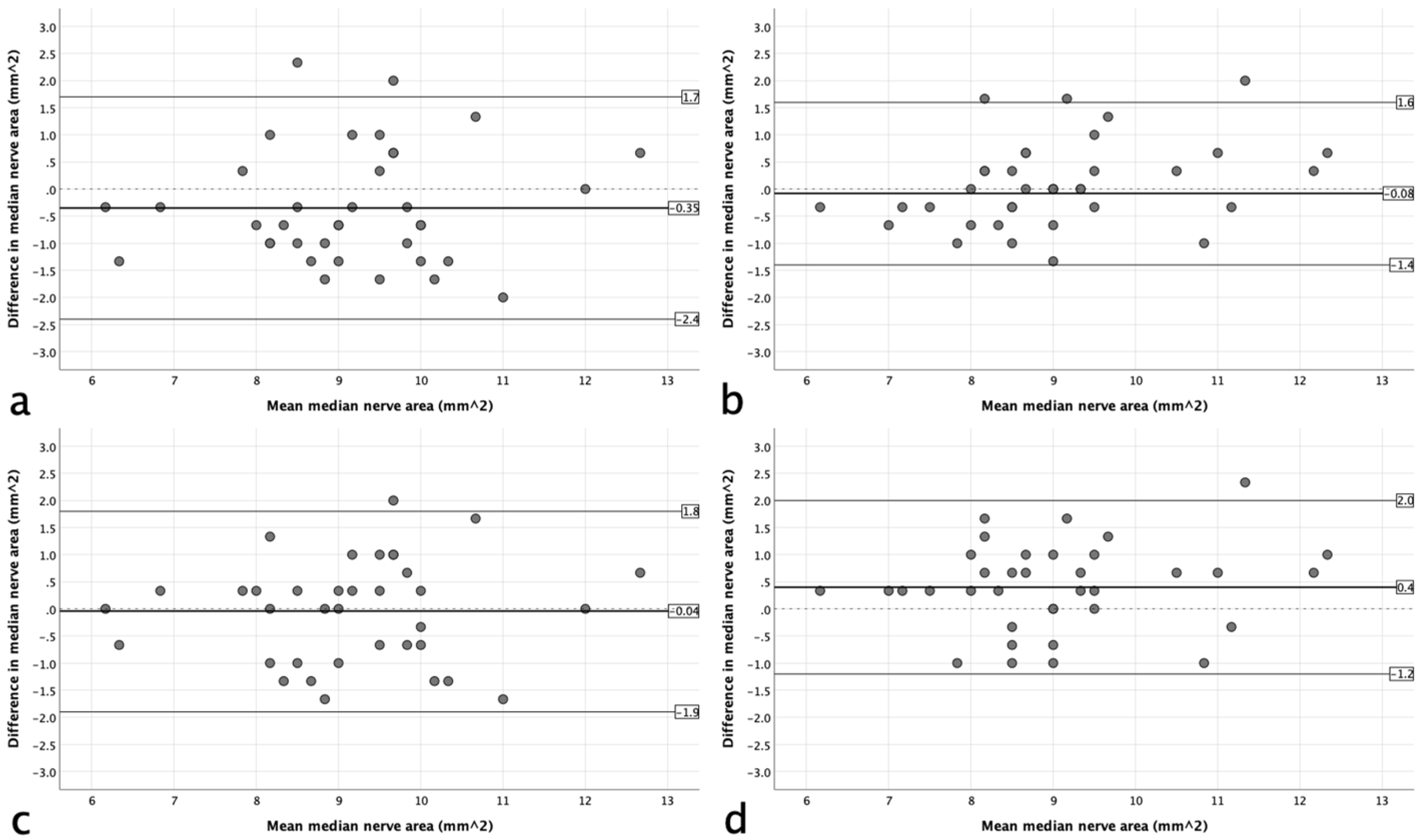
| Standard (Tracing) (SD) | Standard (Ellipse) (SD) | Handheld (SD) | Handheld versus Standard (Tracing) | Handheld versus Standard (Ellipse) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference (%) | Upper and Lower 95% LoAs | p-Value * | Mean Difference (%) | Upper and Lower 95% LoAs | p-Value * | ||||
| Right | 8.9 ± 1.4 | 9.3 ± 1.4 | 9.3 ± 1.3 | 0.35 (3.8%) | −2.4, 1.7 | 0.026 | 0.04 (0.5%) | −1.9, 1.8 | 0.386 |
| Left | 9.0 ± 1.5 | 9.4 ± 1.4 | 9.0 ± 1.3 | 0.08 (0.9%) | −1.4, 1.6 | 0.265 | −0.4 (−4.4%) | −1.2, 2.0 | 0.002 |
| Right | Left | |||||
|---|---|---|---|---|---|---|
| Standard (Tracing) | Standard (Ellipse) | Handheld | Standard (Tracing) | Standard (Ellipse) | Handheld | |
| Operator A reproducibility | 0.901 (0.830, 0.946) | 0.894 (0.815, 0.943) | 0.906 (0.838, 0.948) | 0.921 (0.864, 0.957) | 0.916 (0.855, 0.954) | 0.926 (0.873, 0.960) |
| Operator B reproducibility | 0.703 (0.128, 0.920) | - | 0.539 (0.478, 0.880) | 0.801 (0.391, 0.947) | - | 0.841 (0.542, 0.957) |
| Inter-operator reproducibility | 0.572 (0.283, 0.884) | - | 0.714 (0.150, 0.930) | 0.505 (0.297, 0.574) | - | 0.674 (0.099, 0.915) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfuraih, A.M.; Aldahlawi, R.H.; Habib, Y.S.; Alhowimel, A.S.; Bedewi, M.A. Reliability of Ultrasound Measurements of the Median Nerve in Asymptomatic Subjects Using a Handheld Device. Sensors 2024, 24, 3444. https://doi.org/10.3390/s24113444
Alfuraih AM, Aldahlawi RH, Habib YS, Alhowimel AS, Bedewi MA. Reliability of Ultrasound Measurements of the Median Nerve in Asymptomatic Subjects Using a Handheld Device. Sensors. 2024; 24(11):3444. https://doi.org/10.3390/s24113444
Chicago/Turabian StyleAlfuraih, Abdulrahman M., Rana Hussain Aldahlawi, Yomna S. Habib, Ahmed S. Alhowimel, and Mohamed Abdelmohsen Bedewi. 2024. "Reliability of Ultrasound Measurements of the Median Nerve in Asymptomatic Subjects Using a Handheld Device" Sensors 24, no. 11: 3444. https://doi.org/10.3390/s24113444
APA StyleAlfuraih, A. M., Aldahlawi, R. H., Habib, Y. S., Alhowimel, A. S., & Bedewi, M. A. (2024). Reliability of Ultrasound Measurements of the Median Nerve in Asymptomatic Subjects Using a Handheld Device. Sensors, 24(11), 3444. https://doi.org/10.3390/s24113444






