Using an Instrumented Hammer to Predict the Rupture of Bone Samples Subject to an Osteotomy
Abstract
1. Introduction
2. Materials and Methods
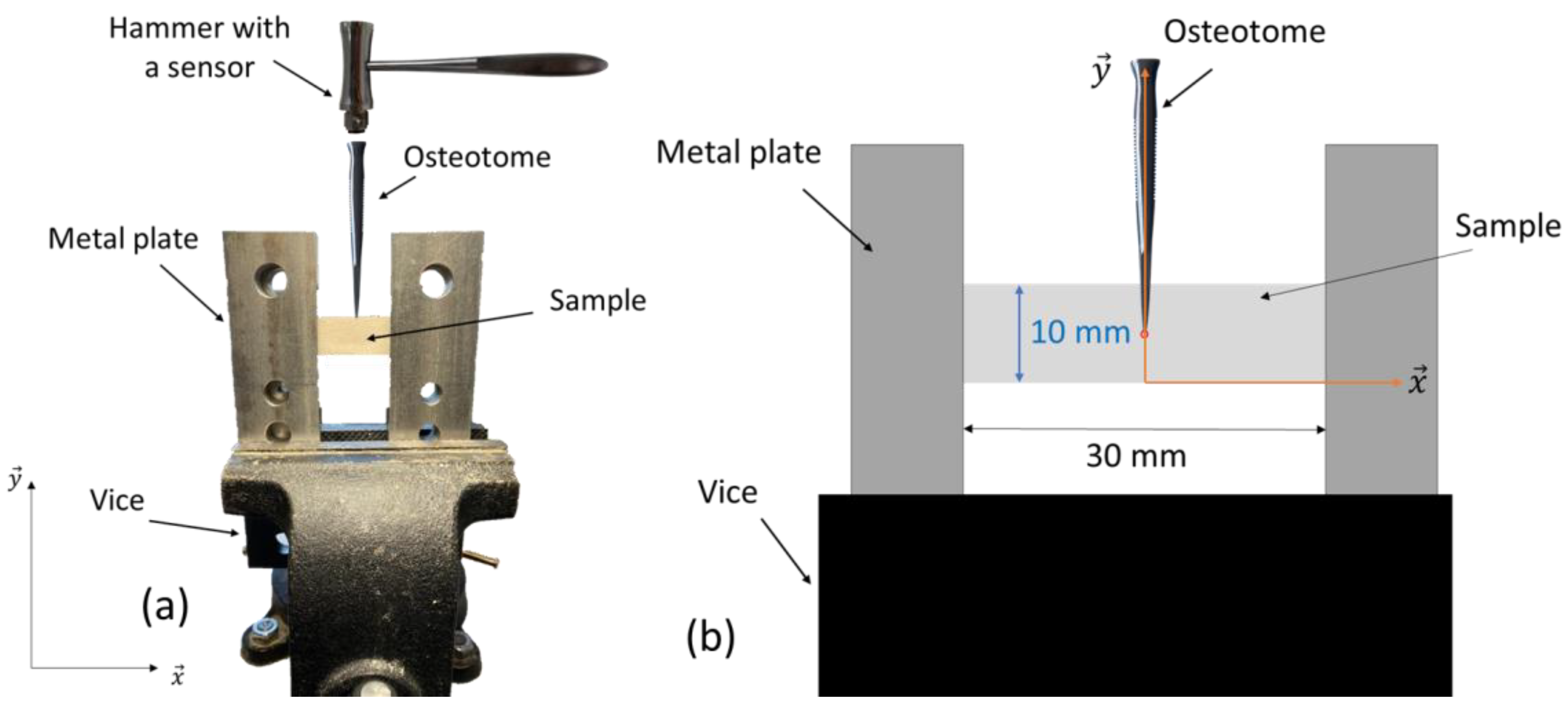
2.1. Experimental Measurements
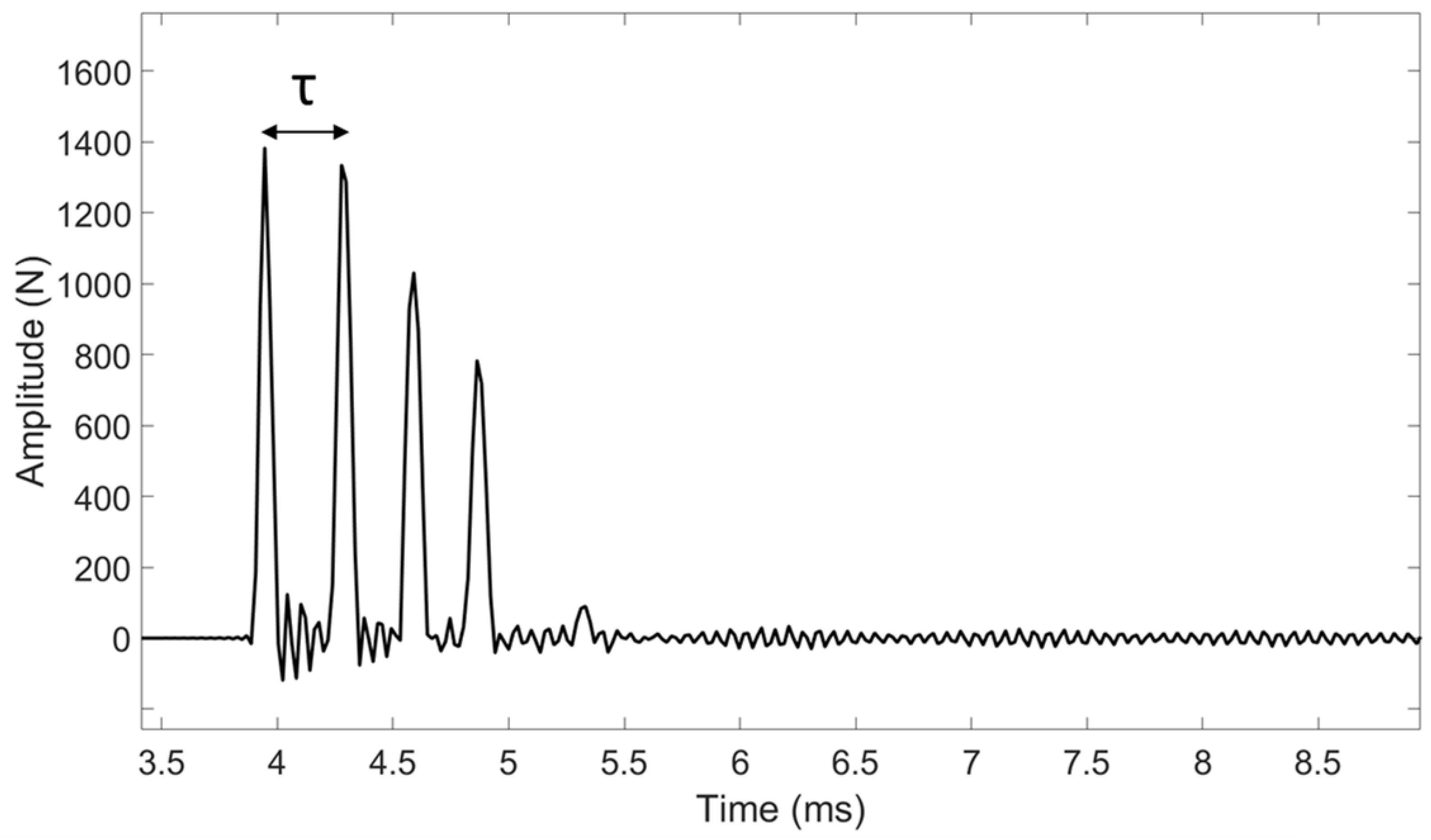
2.2. Signal Processing
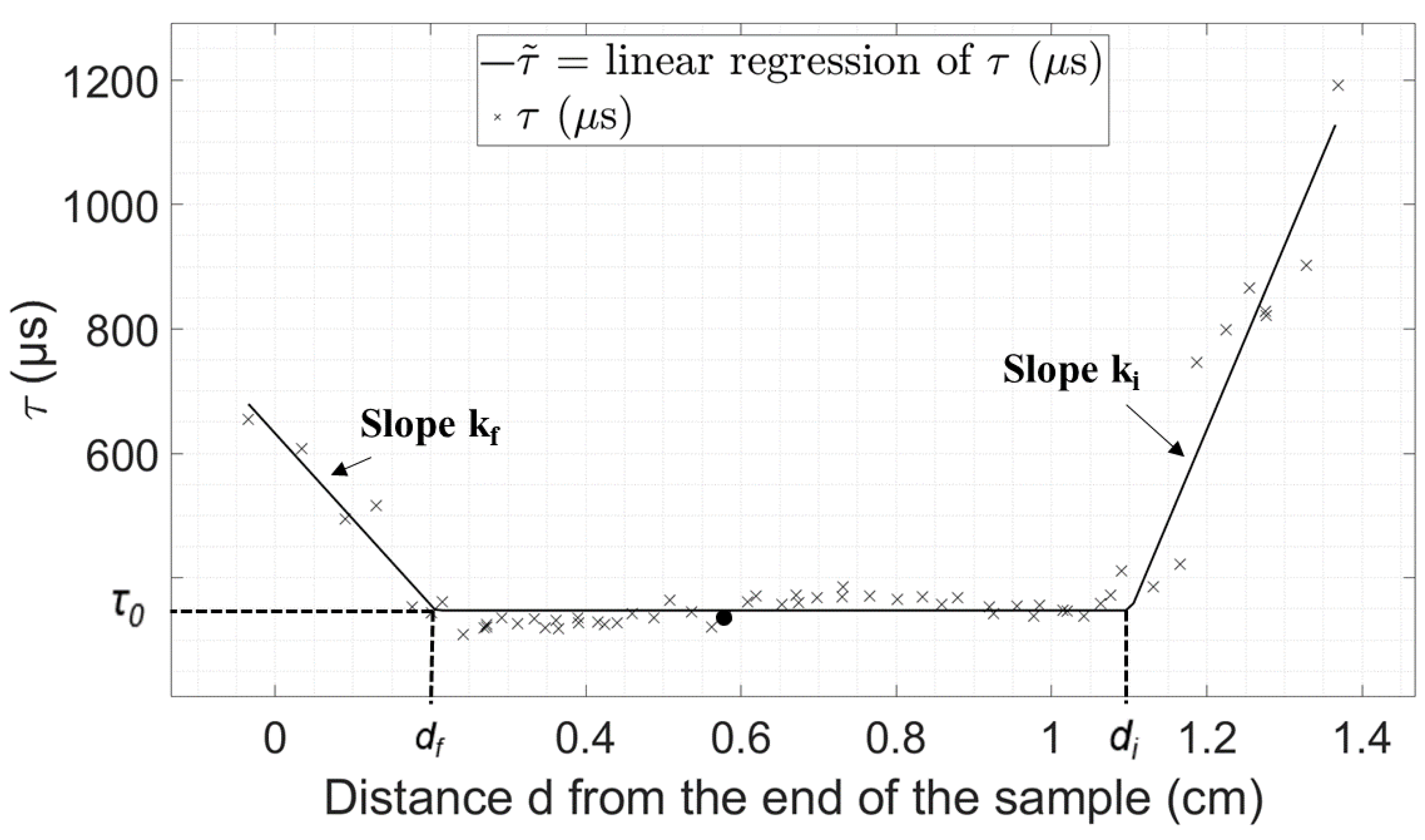
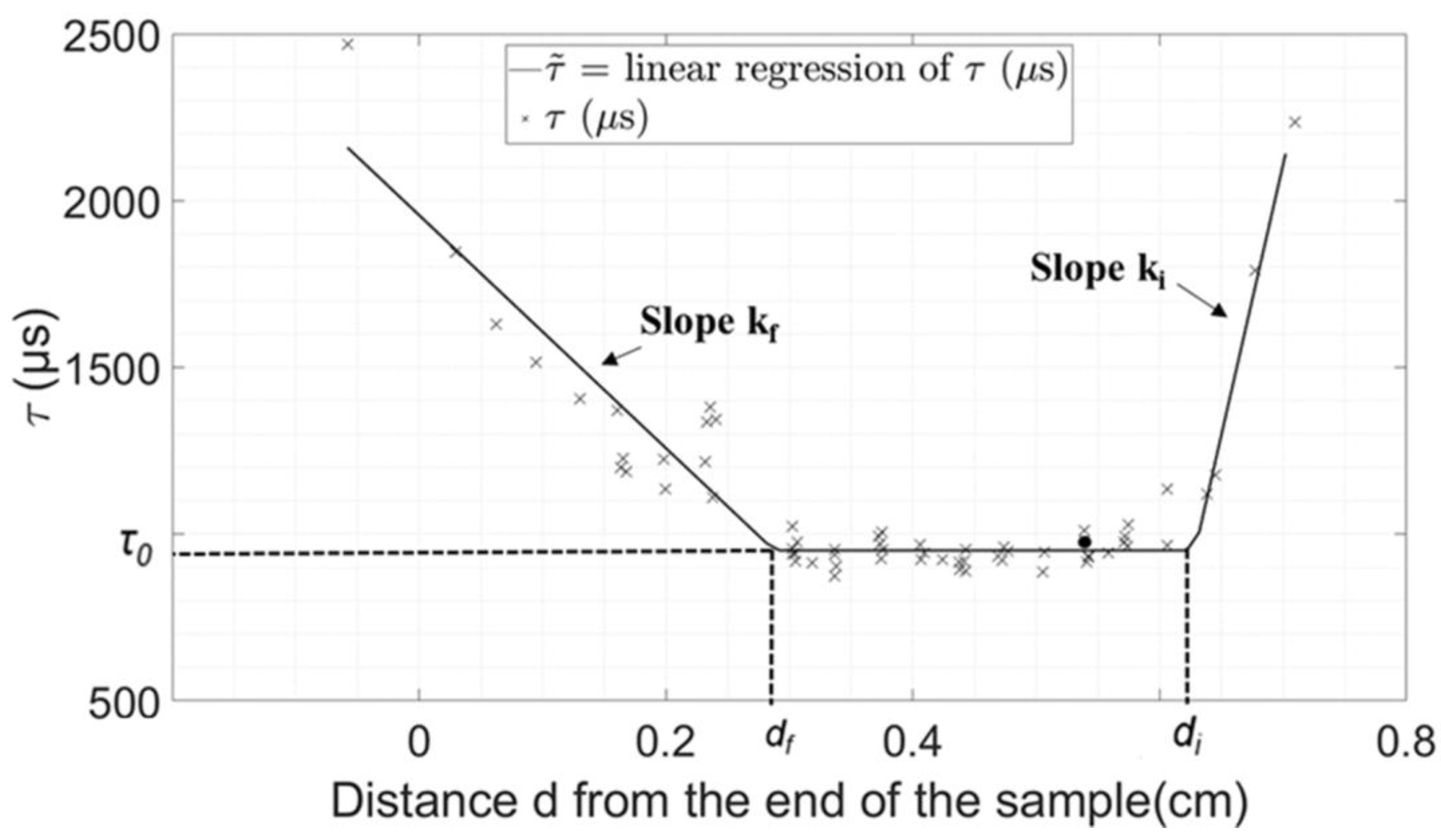
2.3. Data Analysis
3. Results
Experimental Results
4. Discussion
4.1. Repeatability of the Measurements
4.2. Physical Interpretation of the Indicators
4.3. Parameters Derived from Data Analysis
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Becker, D.; Guyuron, B. Nasal Reconstruction and Aesthetic Rhinoplasty. In Plastic and Reconstructive Surgery; Siemionow, M.Z., Eisenmann-Klein, M., Eds.; Springer: London, UK, 2012. [Google Scholar]
- Daniel, R.K. Mastering Rhinoplasty: A Comprehensive Atlas of Surgical Techniques With Integrated Video Clips; Springer Science & Business Media: Berlin, Germany, 2010. [Google Scholar]
- Summers, R.B. A New Concept in Maxillary Implant Surgery: The Osteotome Technique. Compend. Newtown Pa 1994, 15, 152–154. [Google Scholar]
- Ferrigno, N.; Laureti, M.; Fanali, S. Dental Implants Placement in Conjunction with Osteotome Sinus Floor Elevation: A 12-Year Life-Table Analysis from a Prospective Study on 588 ITI Implants. Clin. Oral Implants Res. 2006, 17, 194–205. [Google Scholar] [CrossRef]
- Sullivan, S.M. Le Fort I Osteotomy. Atlas Oral Maxillofac. Surg. Clin. North Am. 2016, 24, 1–13. [Google Scholar] [CrossRef]
- Frodel, J.L.; Marentette, L.J.; Quatela, V.C.; Weinstein, G.S. Calvarial Bone Graft Harvest: Techniques, Considerations, and Morbidity. Arch. Otolaryngol.Head Neck Surg. 1993, 119, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Frodel, J.L. Calvarial Bone Graft Harvest in Children. Otolaryngol. Neck Surg. 1999, 121, 78–81. [Google Scholar] [CrossRef]
- Strong, E.B.; Moulthrop, T. Calvarial Bone Graft Harvest: A New Technique. Otolaryngol. Neck Surg. 2000, 123, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Alesi, D.; Rinaldi, V.G.; Meena, A.; Muccioli, G.M.M.; Zaffagnini, S. Understanding Osteotomy: A Narrative Review. J. Clin. Orthop. 2021, 5, 21–30. [Google Scholar]
- Charles, Y.P.; Schuller, S.; Walter, A.; Steib, J.P. Anterior Osteotomy and Percutaneous in Situ Contouring for Correction of Rigid Posttraumatic T12–L1 Malunion. Eur. Spine J. 2011, 20, 2288–2290. [Google Scholar] [CrossRef]
- Chiffolot, X.; Lemaire, J.P.; Bogorin, I.; Steib, J.P. Ostéotomie de Soustraction Pédiculaire Dans Le Traitement Des Déséquilibres Antérieurs Du Rachis. Rev. Chir. Orthopédique Réparatrice Appar. Mot. 2006, 92, 257–265. [Google Scholar] [CrossRef]
- Nijmeh, A.D.; Goodger, N.M.; Hawkes, D.; Edwards, P.J.; McGurk, M. Image-Guided Navigation in Oral and Maxillofacial Surgery. Br. J. Oral Maxillofac. Surg. 2005, 43, 294–302. [Google Scholar] [CrossRef]
- Schulz, C.; Waldeck, S.; Mauer, U.M. Intraoperative Image Guidance in Neurosurgery: Development, Current Indications, and Future Trends. Radiol. Res. Pract. 2012. [Google Scholar] [CrossRef] [PubMed]
- Eggers, G.; Klein, J.; Blank, J.; Hassfeld, S. Piezosurgery: An Ultrasound Device for Cutting Bone and Its Use and Limitations in Maxillofacial Surgery. Br. J. Oral Maxillofac. Surg. 2004, 42, 451–453. [Google Scholar] [CrossRef] [PubMed]
- Schlee, M.; Steigmann, M.; Bratu, E.; Garg, A.K. Piezosurgery: Basics and Possibilities. Implant Dent. 2006, 15, 334–340. [Google Scholar] [CrossRef]
- Beziat, J.L.; Bera, J.C.; Lavandier, B.; Gleizal, A. Ultrasonic Osteotomy as a New Technique in Craniomaxillofacial Surgery. Int. J. Oral Maxillofac. Surg. 2007, 36, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, V.; Michel, A.; Lachaniette, C.-H.F.; Poignard, A.; Hernigou, P.; Allain, J.; Haïat, G. Variation of the Impact Duration during the in Vitro Insertion of Acetabular Cup Implants. Med. Eng. Phys. 2013, 35, 1558–1563. [Google Scholar] [CrossRef]
- Michel, A.; Bosc, R.; Meningaud, J.-P.; Hernigou, P.; Haiat, G. Assessing the Acetabular Cup Implant Primary Stability by Impact Analyses: A Cadaveric Study. PLoS ONE 2016, 11, e0166778. [Google Scholar] [CrossRef]
- Michel, A.; Bosc, R.; Sailhan, F.; Vayron, R.; Haiat, G. Ex Vivo Estimation of Cementless Acetabular Cup Stability Using an Impact Hammer. Med. Eng. Phys. 2016, 38, 80–86. [Google Scholar] [CrossRef]
- Michel, A.; Bosc, R.; Vayron, R.; Haiat, G. In Vitro Evaluation of the Acetabular Cup Primary Stability by Impact Analysis. J. Biomech. Eng. 2015, 137, 031011. [Google Scholar] [CrossRef]
- Tijou, A.; Rosi, G.; Hernigou, P.; Flouzat-Lachaniette, C.-H.; Haïat, G. Ex Vivo Evaluation of Cementless Acetabular Cup Stability Using Impact Analyses with a Hammer Instrumented with Strain Sensors. Sensors 2017, 18, 62. [Google Scholar] [CrossRef] [PubMed]
- Dubory, A.; Rosi, G.; Tijou, A.; Lomami, H.A.; Flouzat-Lachaniette, C.-H.; Haïat, G. A Cadaveric Validation of a Method Based on Impact Analysis to Monitor the Femoral Stem Insertion. J. Mech. Behav. Biomed. Mater. 2020, 103, 103535. [Google Scholar] [CrossRef]
- Lomami, H.A.; Damour, C.; Rosi, G.; Poudrel, A.-S.; Dubory, A.; Flouzat-Lachaniette, C.-H.; Haiat, G. Ex Vivo Estimation of Cementless Femoral Stem Stability Using an Instrumented Hammer. Clin. Biomech. 2020, 76, 105006. [Google Scholar] [CrossRef] [PubMed]
- Poudrel, A.-S.; Albine Lomami, H.; Rosi, G.; Dubory, A.; Flouzat-Lachaniette, C.-H.; Haiat, G. Estimation of Cementless Femoral Stem Stability Using an Impact Hammer. In Proceedings of the Forum Acusticum, Lyon, France, 07–11 December 2020. [Google Scholar] [CrossRef]
- Tijou, A.; Rosi, G.; Vayron, R.; Lomami, H.A.; Hernigou, P.; Flouzat-Lachaniette, C.H.; Haïat, G. Monitoring Cementless Femoral Stem Insertion by Impact Analyses: An in Vitro Study. J. Mech. Behav. Biomed. Mater. 2018, 88, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Hubert, A.; Rosi, G.; Bosc, R.; Haiat, G. Using an Impact Hammer to Estimate Elastic Modulus and Thickness of a Sample During an Osteotomy. J. Biomech. Eng. 2020, 142, 071009. [Google Scholar] [CrossRef] [PubMed]
- Lamassoure, L.; Giunta, J.; Rosi, G.; Poudrel, A.-S.; Bosc, R.; Haiat, G. Using an Impact Hammer to Perform Biomechanical Measurement during Osteotomies: Study of an Animal Model. Proc. Inst. Mech. Eng. H. 2021, 235, 838–845. [Google Scholar] [CrossRef]
- Lamassoure, L.; Giunta, J.; Rosi, G.; Poudrel, A.-S.; Meningaud, J.-P.; Bosc, R.; Haïat, G. Anatomical Subject Validation of an Instrumented Hammer Using Machine Learning for the Classification of Osteotomy Fracture in Rhinoplasty. Med. Eng. Phys. 2021, 95, 111–116. [Google Scholar] [CrossRef]
- Giunta, J.; Lamassoure, L.; Nokovitch, L.; Rosi, G.; Poudrel, A.-S.; Meningaud, J.-P.; Haïat, G.; Bosc, R. Validation of an Instrumented Hammer for Rhinoplasty Osteotomies: A Cadaveric Study. Facial Plast. Surg. Aesthetic Med. 2021, 24, 369–374. [Google Scholar] [CrossRef]
- Poumarat, G.; Squire, P. Comparison of mechanical properties of human, bovine bone and a new processed bone xenograft. Biomaterials 1993, 14, 337–340. [Google Scholar] [CrossRef]
- Swartz, D.-E.; Wittenberg, R.-H.; Shea, M.; White, A.-A.; Hayes, W.-C. Physical and mechanical properties of calf lumbosacral trabecular bone. J. Biomech. 1991, 24, 1059–1068. [Google Scholar] [CrossRef]
- Wang, T.; Wang, Y.; Crocetti, R.; Wålinder, M. In-plane mechanical properties of birch plywood. Constr. Build. Mater. 2022, 340, 127852. [Google Scholar] [CrossRef]
- Morita, A.; Sora, S.; Mitsuishi, M.; Warisawa, S.; Suruman, K.; Asai, D.; Arata, J.; Baba, S.; Takahashi, H.; Mochizuki, R.; et al. Microsurgical robotic system for the deep surgical field: Development of a prototype and feasibility studies in animal and cadaveric models. J. Neurosurg. 2005, 103, 320–327. [Google Scholar] [CrossRef]
- Bosc, R.; Tijou, A.; Rosi, G.; Nguyen, V.-H.; Meningaud, J.-P.; Hernigou, P.; Flouzat-Lachaniette, C.-H.; Haiat, G. Influence of Soft Tissue in the Assessment of the Primary Fixation of Acetabular Cup Implants Using Impact Analyses. Clin. Biomech. 2018, 55, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Songu, M.; Cingi, C.; Palma, P. Osteotomies. In All Around the Nose; Cingi, C., Muluk, N.B., Eds.; Springer: London, UK, 2012. [Google Scholar]

| Parameter | Plywood Sample (Figure 4) | Bone Sample (Figure 5) |
|---|---|---|
| τ0 (μs) | 348 | 951 |
| di (cm) | 1.10 | 0.63 |
| df (cm) | 0.21 | 0.29 |
| ki (μs/cm) | 2956 | 16,220 |
| kf (μs/cm) | −1375 | −3495 |
| Eτ | 5.04 | 10.9 |
| Parameter | Mean (±SD) | Min | Max |
|---|---|---|---|
| τ0 (μs) | 384.17 ± 44.07 | 347.7 | 480.1 |
| df (cm) | 0.267 ± 0.104 | 0.19 | 0.5 |
| ki (μs/cm) | 3482 ± 1950 | 1169 | 6805 |
| kf (μs/cm) | −1201.4 ± 795.7 | −2977.6 | −562.9 |
| Eτ | 4.61 ± 3.27 | 1.25 | 12.08 |
| Parameter | Mean (±SD) | Min | Max |
|---|---|---|---|
| τ0 (μs) | 1128.1 ± 359.5 | 560.9 | 1937.6 |
| df (cm) | 0.262 ± 0.127 | 0.060 | 0.543 |
| ki (μs/cm) | 8751 ± 12,726 | 1281 | 58,071 |
| kf (μs/cm) | −8268 ± 4794 | −16,840 | −1067 |
| Eτ | 41.36 ± 36.05 | 8.29 | 140.31 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bas dit Nugues, M.; Rosi, G.; Hériveaux, Y.; Haïat, G. Using an Instrumented Hammer to Predict the Rupture of Bone Samples Subject to an Osteotomy. Sensors 2023, 23, 2304. https://doi.org/10.3390/s23042304
Bas dit Nugues M, Rosi G, Hériveaux Y, Haïat G. Using an Instrumented Hammer to Predict the Rupture of Bone Samples Subject to an Osteotomy. Sensors. 2023; 23(4):2304. https://doi.org/10.3390/s23042304
Chicago/Turabian StyleBas dit Nugues, Manon, Giuseppe Rosi, Yoann Hériveaux, and Guillaume Haïat. 2023. "Using an Instrumented Hammer to Predict the Rupture of Bone Samples Subject to an Osteotomy" Sensors 23, no. 4: 2304. https://doi.org/10.3390/s23042304
APA StyleBas dit Nugues, M., Rosi, G., Hériveaux, Y., & Haïat, G. (2023). Using an Instrumented Hammer to Predict the Rupture of Bone Samples Subject to an Osteotomy. Sensors, 23(4), 2304. https://doi.org/10.3390/s23042304







