4.1. Evaluating Light Sensors with Commercially Available Masks
The aim of this experiment was to measure the variation of light intensity with the strap at different lengths and compare the observation between three distinct masks. There are a variety of environmental factors through which the quality of the fit of the mask can be determined, including humidity, temperature, light, and amount of O2 or CO2. These factors indicate a physical property; e.g., for light, if no light gets inside the mask, then it can be assumed that a reasonable fit is achieved. For this reason, the intensity of light sensed by light sensors plays a prominent role in deciding the fit of the mask.
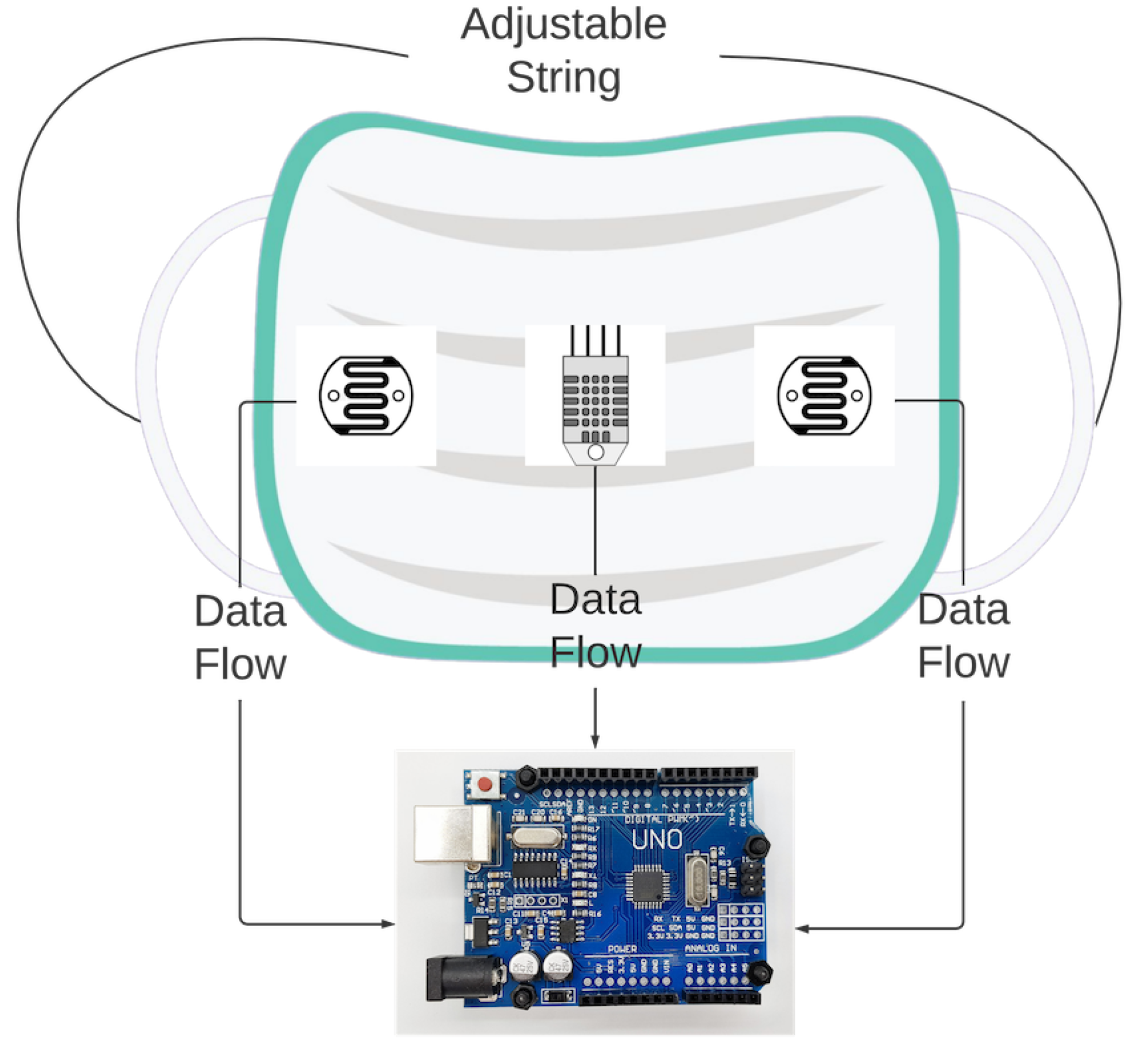
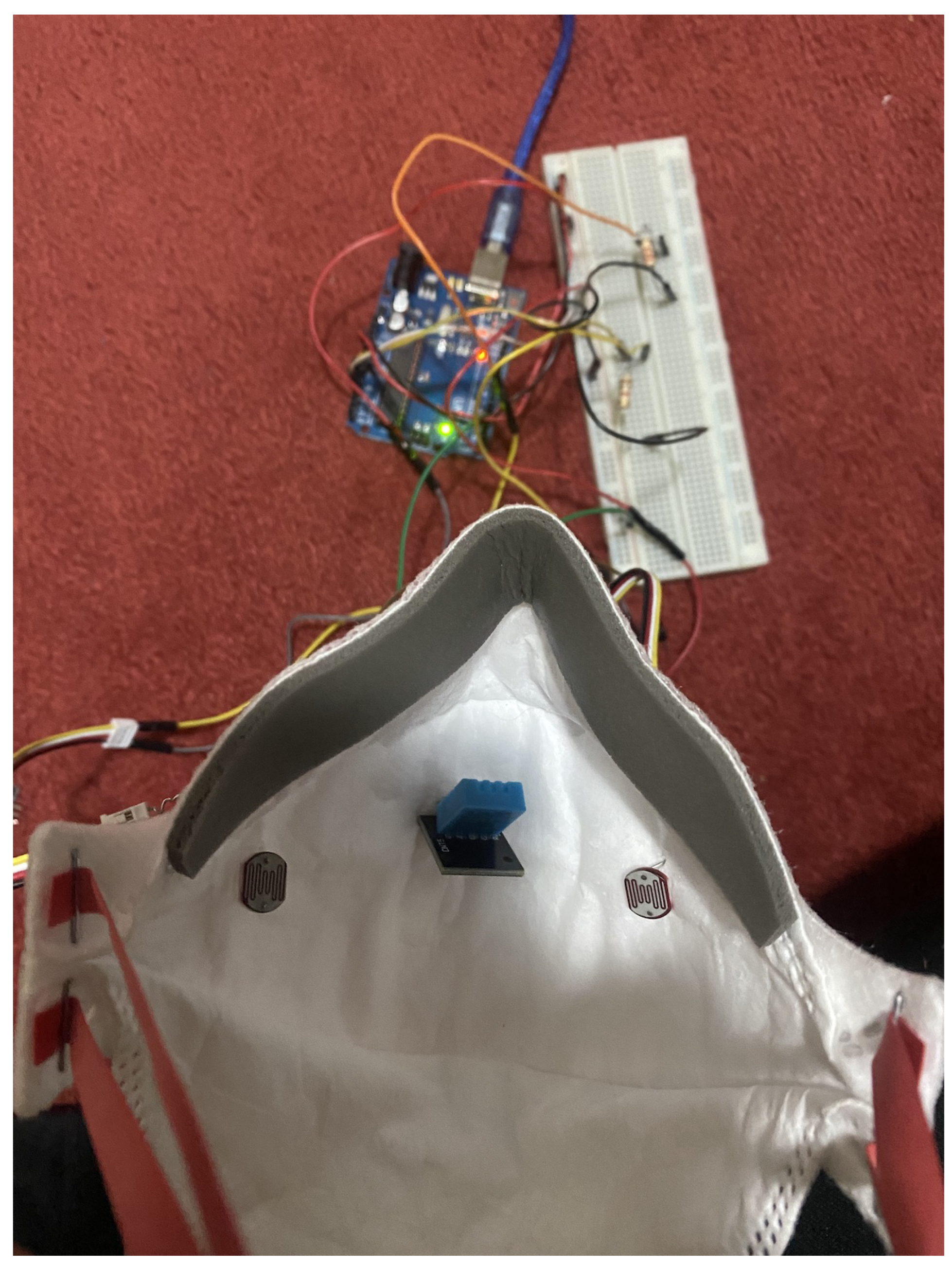
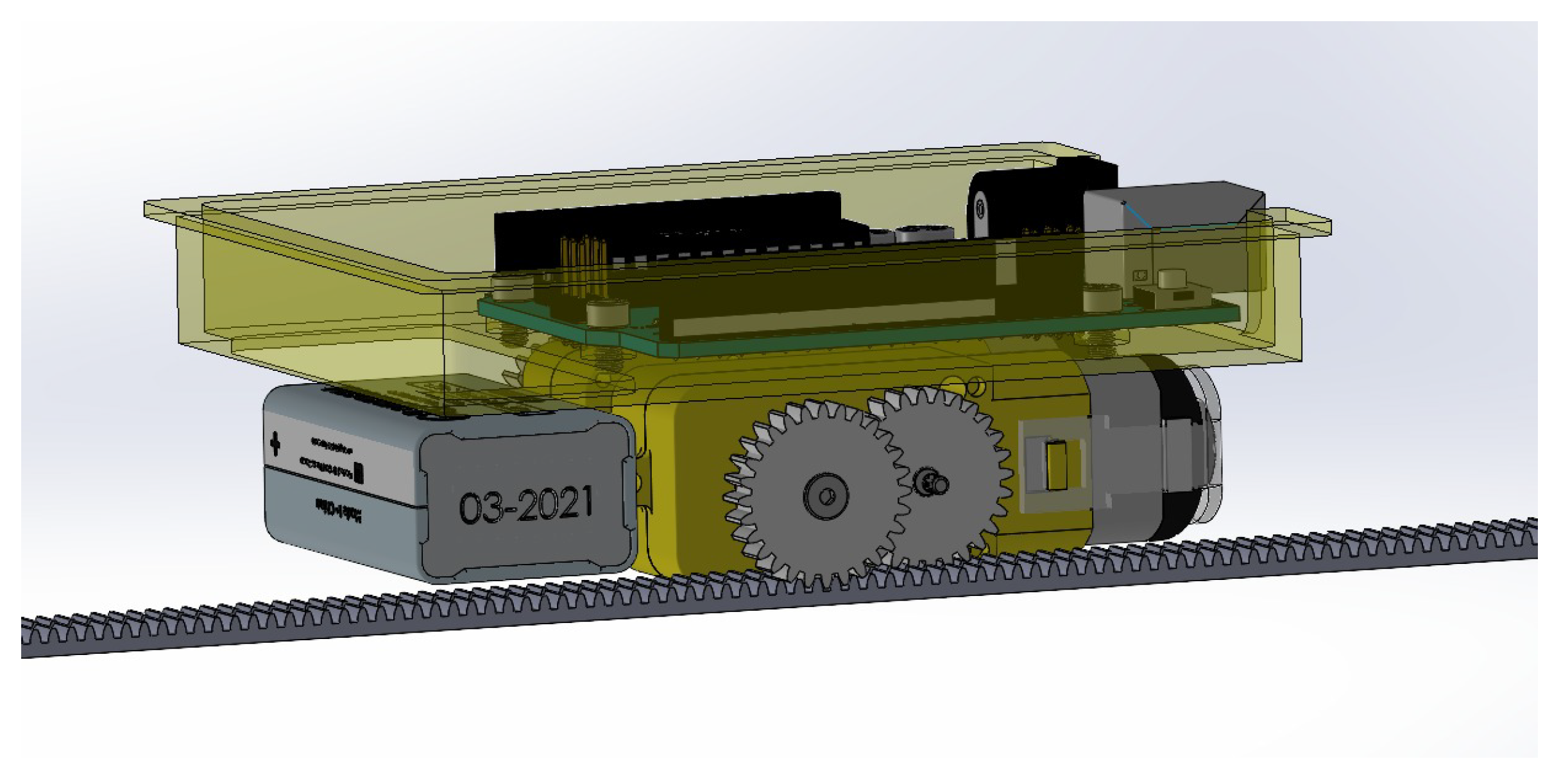
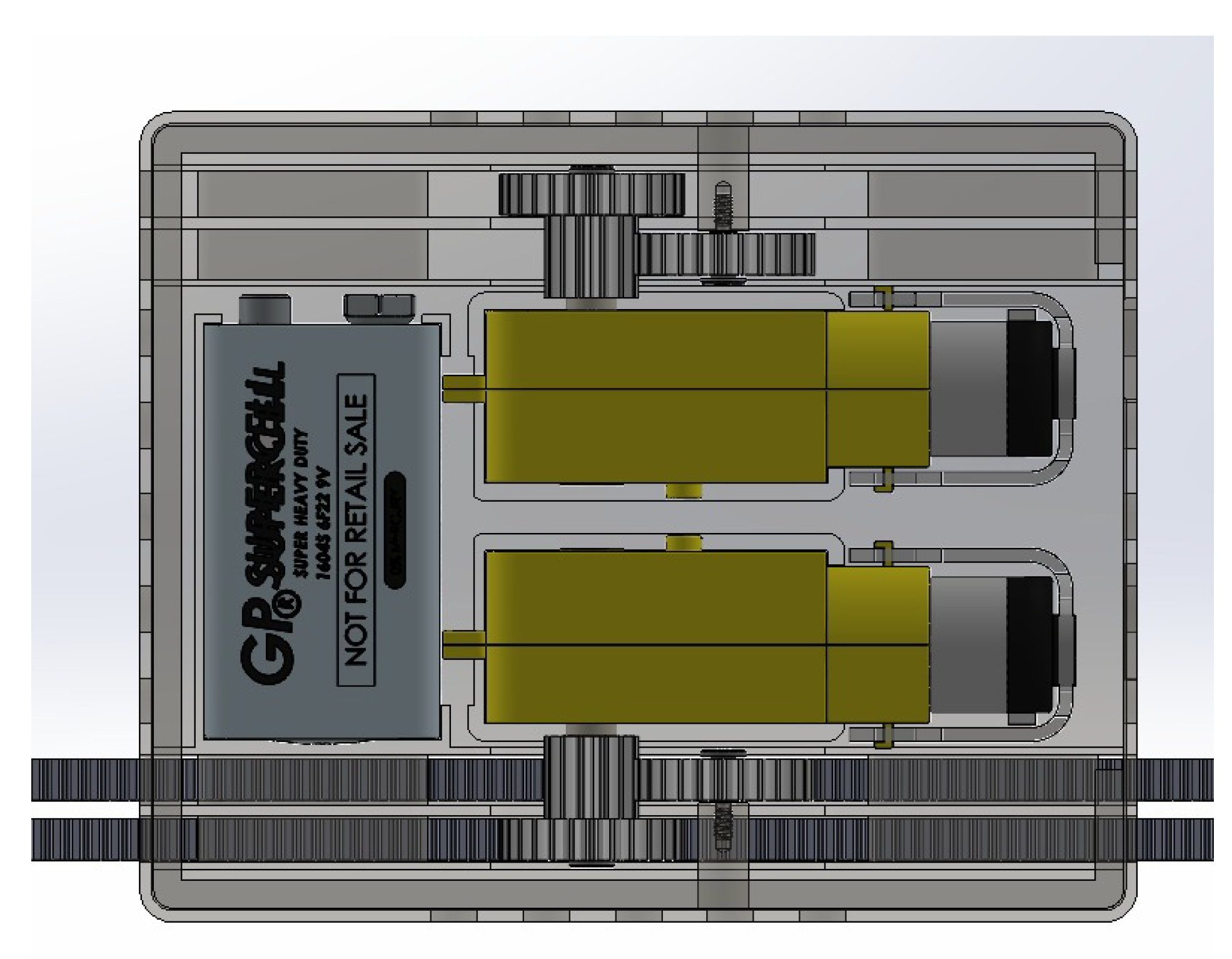
This experiment sought to investigate the feasibility of utilizing light-intensity sensors to determine mask fit quality with commercially available masks. To measure the sensor values at various fit levels, a setup was constructed which allowed for the testing of different masks, as depicted in
Figure 9. The experiments were conducted by collecting the intensity of light captured by the light intensity sensors as the adjustable strap length was varied. The setup worn by the participant consisted of a 19.25 cm adjustable strap attached to the mask. The sensors were connected to the Arduino UNO microcontroller through jumper wires. The light intensity sensors were positioned on each side of the mask facing the user’s face, allowing for the detection of light and air/moisture breaches.
The results of each of the following experiments were documented by repeating them ten times, varying the strap length from 19.25 cm to 0 cm, and averaging the results. The design of the experiment is illustrated in
Figure 10. It states the length of the strap which varied, and which sensors being retrofitted with the mask were connected to the Arduino. Then, sense, think, act paradigm graphs were created from the recorded data. At each point of decrement in the length of the strap the user perception of tightness was also recorded to understand the correlation between strap length, user perception of tightness, and light intensity.
The experiment was carried out on three masks made of different materials. The following masks are used:
For the first experiment, a surgical mask was used, and the length of the strap was set to its most loose setting. Over time, this was tightened by 2.25 cm each step until it reached its tightest setting.
Table 2 contains the results of the experiment with the light intensity for the left and right sensors recorded at each tightness step. The range of the light sensor varied from 0 to 1024, where 0 indicates no light and 1024 indicates the maximum light sensed by the sensor. At the loosest setting of 19.25 cm, the light intensities were measured at 9 for the left side and 8 for the right side of the mask. The data show, as the experiment progressed and the mask was tightened, that the light intensity decreased over time until it reached the lowest value possible by the sensor. This demonstrates that light sensors can be used to determine the tightness of a mask.
The data indicate that the intensity of light detected by LDR sensors with a surgical mask is directly proportional to the length of the strap, implying that as the length reduces, so does the distance between the mask and the user’s face. When the length of the strap approaches 0 cm, the intensity of both sensors drops to 1, indicating that the mask is closest to the face without any gaps. According to the user, the face mask is now too tight. The variation for both sensors left and right is similar in the beginning but changes in the middle when the strap length is changed to 6.75 cm. It is suspected that in the initial phase, the mask was too loose and the effect of tightness on the intensity of the sensors was the same. However, as the mask started fitting on the face, the effect of tightness on the intensity of the sensor changed because of the face structure and the mask composition, which resulted in the different readings of sensors at the same length and position inside the mask.
For the second experiment, a fabric mask was used with the strap length set to the loosest setting in a similar way to the surgical mask.
Table 3 contains the results of the experiment with the light intensity for the left and right sensors recorded at each tightness step. The first reading was measured when the length of the strap was at the loosest setting at 19.25 cm, which provides the reading of intensities of 8 for the right and left sides of the mask, respectively. By progressing the experiment, the intensity of light started decreasing, and the tightness of the mask was achieved at the light intensity of 0 for the fabric mask. Based on the outcome, it can be stated that a fabric mask is better at providing protection against contamination than a surgical mask.
The intensity of light recorded by light intensity sensors within the mask is also directly proportional to the length of the strap, providing a comparable result to that of a surgical mask. When the length of the strap approaches 0 cm, the reading of both sensors drops to 0, indicating that the mask is tight according to the user. The key difference between surgical and fabric masks is the type of material used which resulted in the difference in intensity variations when compared to each at the same strap length.
For the third experiment, a KN95 mask was used, and the experiment process was repeated in a similar procedure as with surgical and fabric masks. The results of the experiment are displayed in
Table 4 with the intensity of the light recorded at each tightness step for the left and right sensors. The different structure of the mask makes it unique and more effective than the other masks. A similar setup of tightness was made for the KN95 mask, but because of its uniqueness, some modifications were made in the strap length in order to perform the experiment; the length of the strap has its loosest setting at 25 cm and was tightened by 1 cm each step over time until it reached its tightest setting, which is 18 cm. At the loosest setting of 25 cm, the light intensities were measured at 7 for the left and right sides of the mask. The rate of variation of sensor light intensity strictly decreases compared to other masks when the strap is tightened.
These results indicate that the intensity of light recorded by light intensity sensors within the KN95 mask is exactly proportional to the length of the strap, implying that as the length reduces, so does the distance between the mask and the user’s face. It should be noted that the length of the strap on the KN95 mask varies from 18 cm to 25 cm, but the length on surgical and fabric masks varies from 0 cm to 19.25 cm. Because of the unique construction of N95 masks, when the length of the strap reaches 19 cm, the reading of both sensors drops to zero, indicating that the mask is tight and closest to the user’s face. Furthermore, when the length of the mask’s strap is reduced further by 1 cm, the intensity remains 0 but the mask feels tighter to the user.
To visualize the difference between the three different masks,
Figure 11 provides a graph of these results, showing the correlation between the length of the strap, perceived user mask tightness, and light intensity from the left and right LDR sensors. After analyzing the findings of all three masks, it was determined that the intensity of light decreases with the length of the strap in all cases. It was also discovered that KN95 masks were superior to the other two masks since the minimal value of intensity was observed when the length was lowered to 0 in the surgical and fabric masks, but not in the KN95 mask. The intensity 0 in N95 masks was estimated when the length was 18 cm, indicating that these masks do not need to be tightened as much to provide better performance.
4.2. Variation of Temperature and Humidity with a Length of Strap of Surgical, Fabric, and KN95 Mask
The objective of this experiment was to determine the temperature and humidity inside the mask by varying the adjustable strap length using the same configuration as in the experiments with light-intensity sensors. Temperature and humidity indicate the inhalation and exhalation of the user and how it affects the fitness of the mask [
27]. For this experiment, a DHT11 combined humidity and temperature sensor was added to the setup illustrated in
Figure 9 directly facing the user’s mouth. As observed from the behavior of light intensity, a hypothesis was that when the strap length is tightened, the humidity and temperature value should increase proportionally. For these experiments, the process was the same as in
Section 4.1. For each type of mask, the length of the strap was set to its loosest setting. Over time, this was tightened by 2.25 cm at each step until it reached its tightest setting. The experiments were repeated 10 times, each varying the strap length from 19.25 cm to 0 cm, and the results averaged.
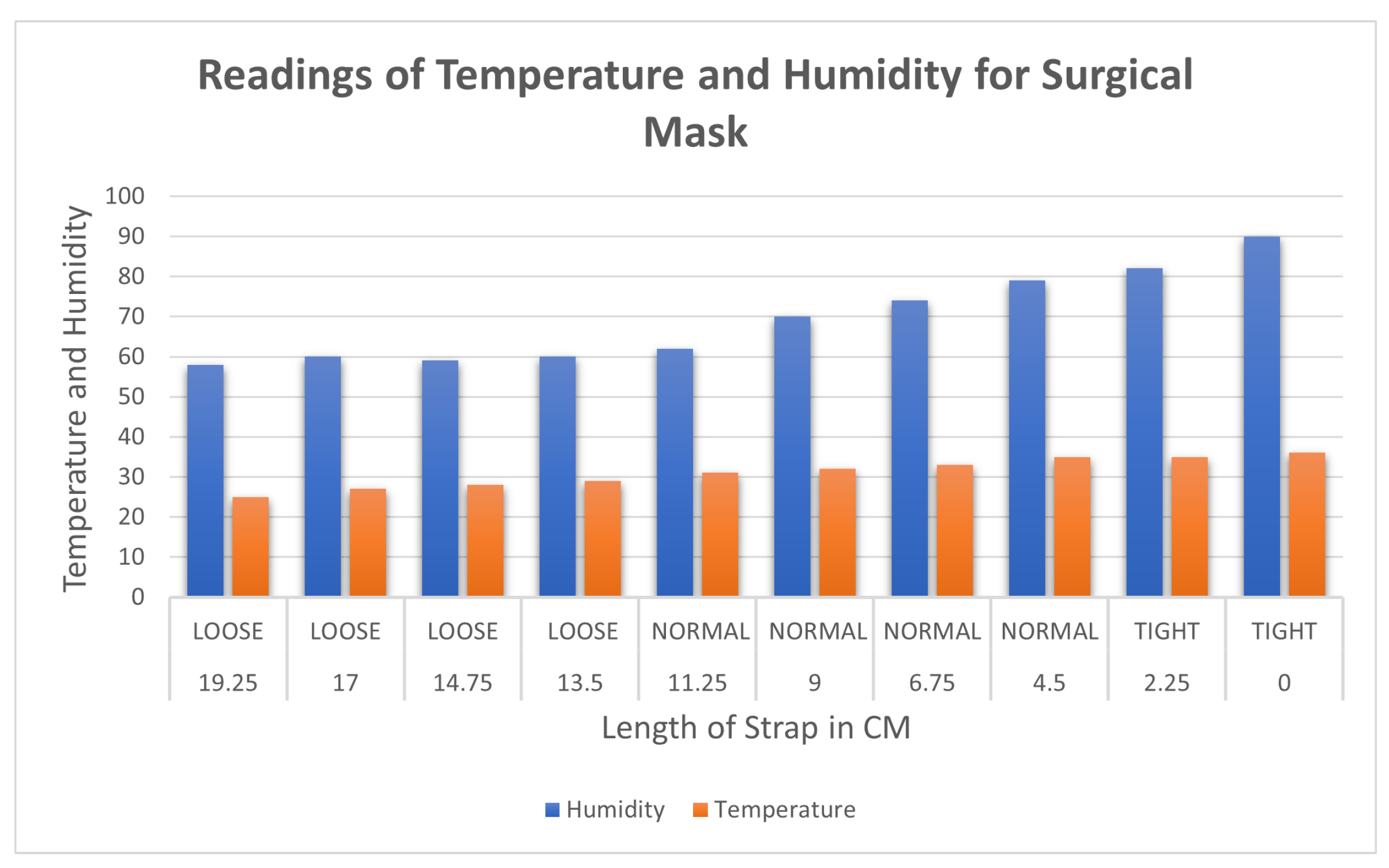
Table 5 contains the measured temperature and humidity with a surgical mask. The first reading was measured when the length of the strap was kept at 19.25, which provides the reading of humidity and temperature of 58 and 25, respectively. The range of the sensor data varied from 0 to 50 degrees Celsius in temperature and 0–100% for humidity. As the mask was tightened, the values for temperature and humidity increased relatively proportionally. When the length of the strap was set to 0 cm, the values of the sensor reading were 90 and 36 for humidity and temperature, respectively.
Figure 12 shows that the hypothesis was proven, as temperature and humidity follow a similar trend of increasing with the decrease in length of the strap. The rate of increase in values is inversely proportional to the length of the strap but directly proportional to the tightness. As the length of the strap decreases the tightness increases. The trend of the plot is increasing temperature and humidity as the mask is tightened.
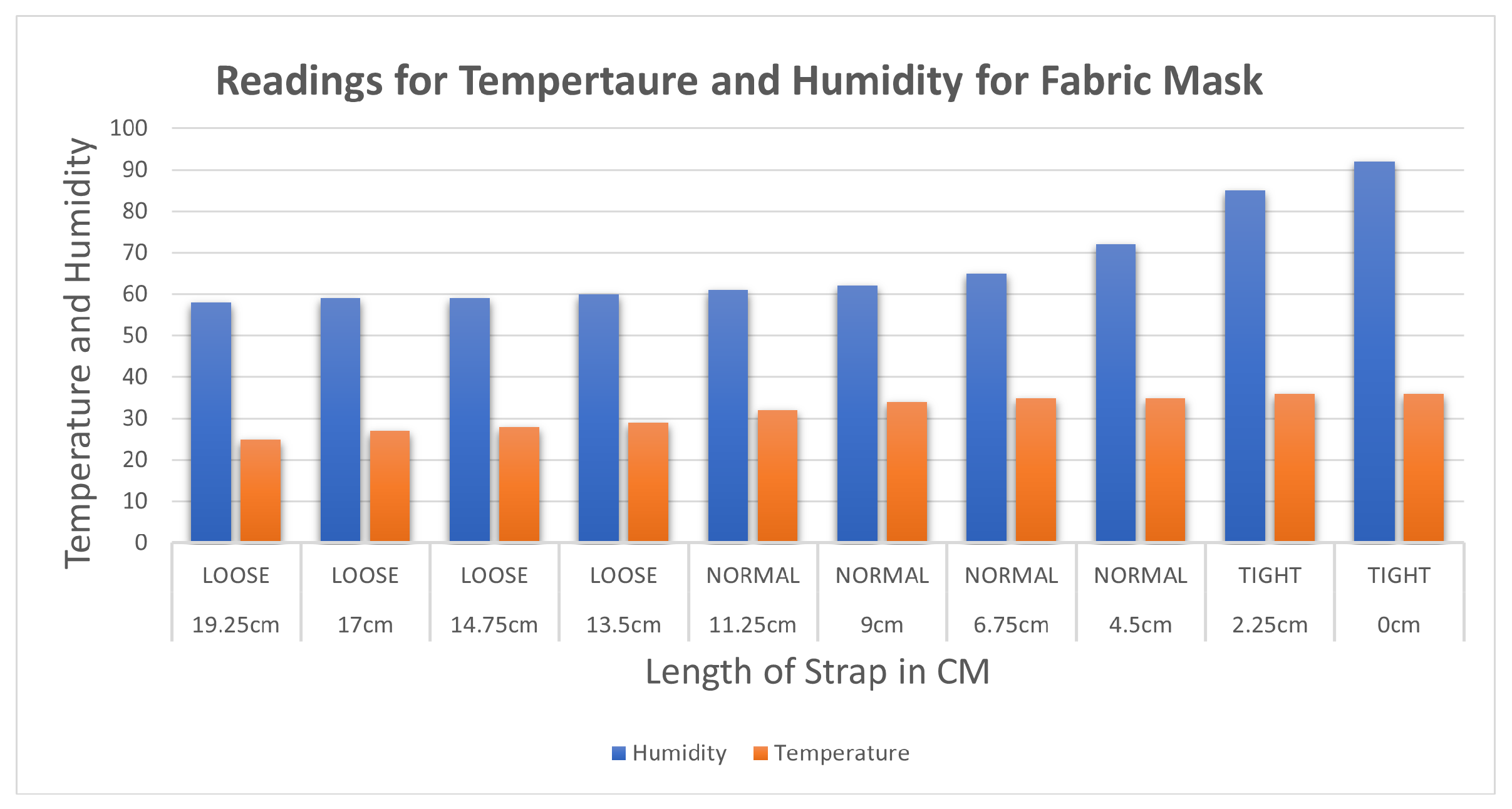
The data for temperature and humidity for the fabric mask using the dht11 sensor are recorded in
Table 6. The first reading was measured when the strap was kept at the loosest end, which is 58 and 25 for humidity and temperature, respectively. As the experiment progressed by decreasing the strap length, humidity and temperature increased. When the strap length was reduced to 0 cm, the maximum values for humidity and temperature recorded were 92 and 36, respectively.
Figure 13 shows the similar trend of the increase in humidity and temperature with the decrease in the length of the strap. The rate of increase in values is inversely proportional to the length of the strap but directly proportional to the tightness. As the length of the strap decreases the tightness increases. The trend of the plot shows increasing temperature and humidity as the mask is tightened.
The results for the temperature and humidity sensor with the N95 are displayed in
Table 7. At the loosest setting, the N95 mask reads a temperature of 28 and a humidity of 78. As the mask is tightened the trend is observed with the KN95 mask when the length of the strap is decreased with respect to the temperature and humidity.
Figure 14 shows that humidity, like temperature, increases as the length is decreased. After carefully evaluating the findings of both experiments, it was determined that the temperature and humidity in a mask rise as the strap length decreases. It was discovered that because of the restricted airflow in KN95 masks, temperature and humidity increased fast when the strap was tightened, making it better for protection than the surgical mask. Furthermore, it should be noted that the temperature and humidity detected are affected by other parameters, such as the mask’s quality/material and construction (in KN95).
Based on the outcome of the above experiments, it is possible to determine that the correlation between three types of masks and sensors impacts the mask’s fitness. The intensity of the light is inversely related to the tightness and fit of the mask, although temperature and humidity are directly proportional. This part focuses on tightening and fitting the mask utilizing the blueprint built using DC motors and gears to automate tightening and fitting.
4.3. Evaluating Mask Automatic Adjustment
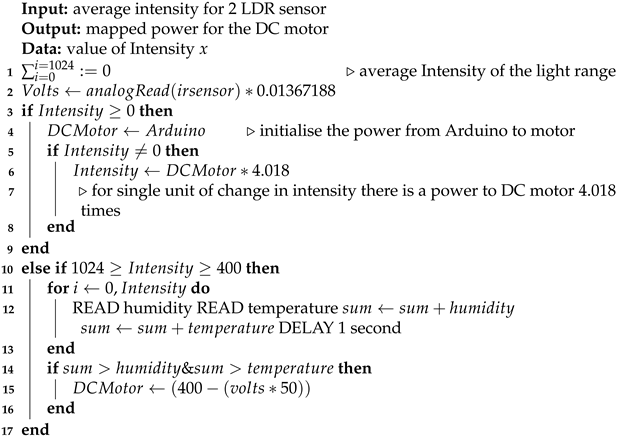
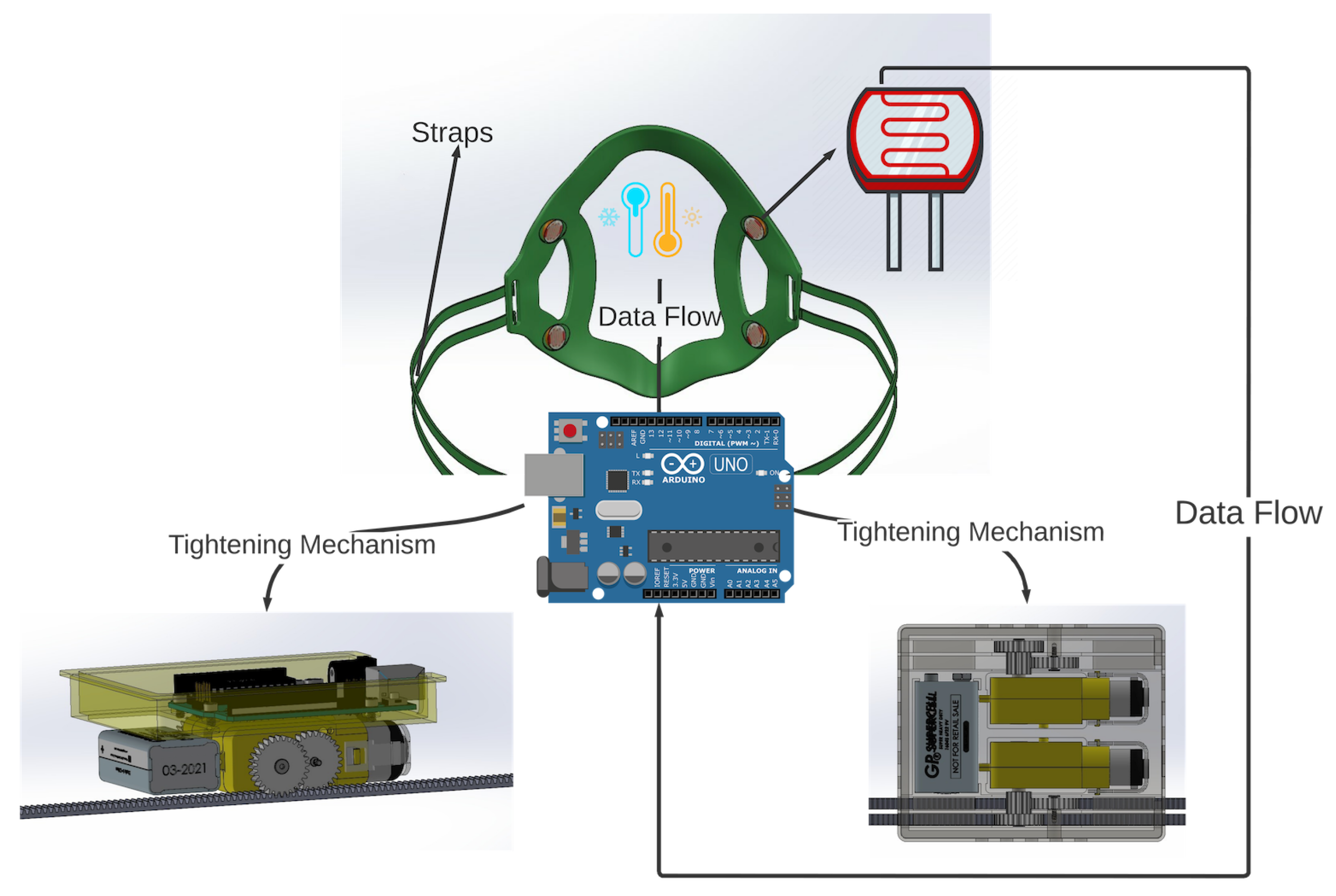
The objectives of these experiments were to assess the efficacy of the automatic mask adjustment mechanism. This mechanism utilizes four straps connected to a brace, with sensor information provided by four light intensity sensors. The data collected from these sensors were utilized to calculate the rotation of the DC motors attached to the mask straps. In this manner, the rotation value is dependent on the current light intensity value. The equipment employed to tighten the straps is a DC motor that operates on a PWM (pulse with modulation) pin on the microcontroller with a power range of 0–1024, where 0 represents no power and 1024 represents high power. Additionally, the LDR sensors are connected to an analog pin with a value range of 0–1024.
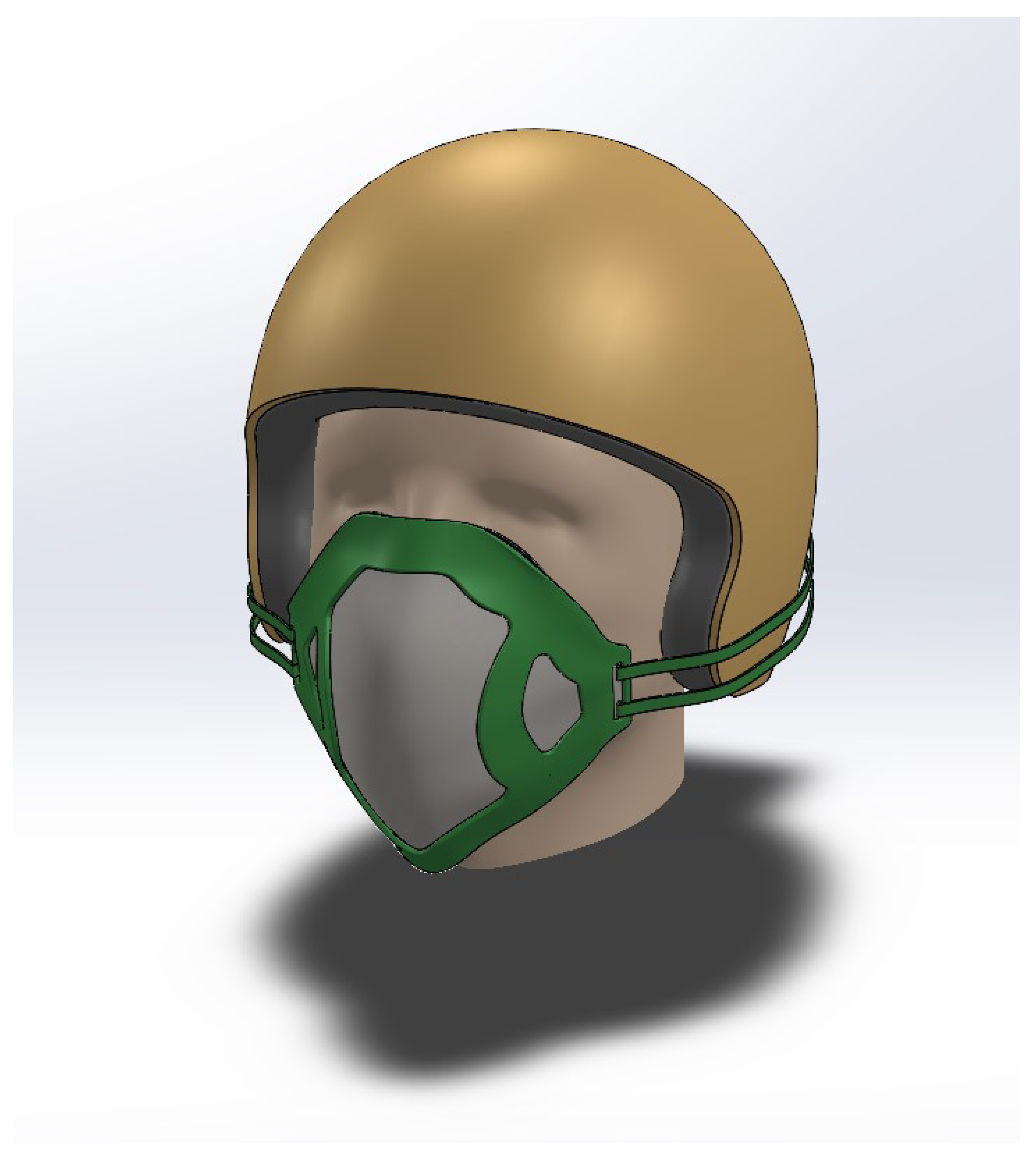
Figure 15 illustrates the experimental setup, which comprises a 3D-printed mask brace placed over an N95 mask. The participant is instructed to sit in an idle position after donning the setup.
For each step, the value of the intensity of light was mapped with the intensity attribute. The power delivered to the motor at that intensity was computed with the tightness attribute as specified by the user. Both motors operate in a similar manner, utilizing the power series calculated in the table.
The DC motors are connected with the Arduino and work as per Algorithm 1. When the mask brace is worn, the sensors start collecting the intensity of the light from the LDR sensors. When the motor is switched on it starts rotating depending on the initial average value coming from two LDR sensors per strap. With a delay of 500 milliseconds, the second value is based on which power is given to the DC motor. Temperature and humidity also affect the power. It reads the value of temperature and humidity at an interval of one second and checks if the value is increasing or decreasing based on the variation of power supply. In the algorithm designed, the light intensity energy is converted to power supply for the DC motor; the higher the intensity of light, the higher the power supply and the rotation of the motor. If the intensity of light is less, sensors will be able to detect the intensity, but not much power will be generated, which implies, as per the algorithm, that enough torque is required for rotating the motors. In short, more intensity of light is required. This also states that the mask is in a fit state. The flowchart of the algorithm design can be seen in
Figure 16.
| Algorithm 1: An algorithm for detecting the mask fitness. |
![Sensors 23 01711 i001]() |
For these experiments, a user wears the mask brace using an N95 mask filter which is tied to the edges of the brace. The mask is set to its most loose setting and the automatic adjustment mechanism is activated. The adjustment mechanism algorithm takes control of the DC motors and tightens the mask straps until it reaches a state that it considers ideal.
4.3.1. Motor Response to Light Intensity
To first investigate the response of the motor algorithm to the automatic tightening process, the light intensity, motor power, and light intensity were recorded.
Table 8 lists the results of the experiment.
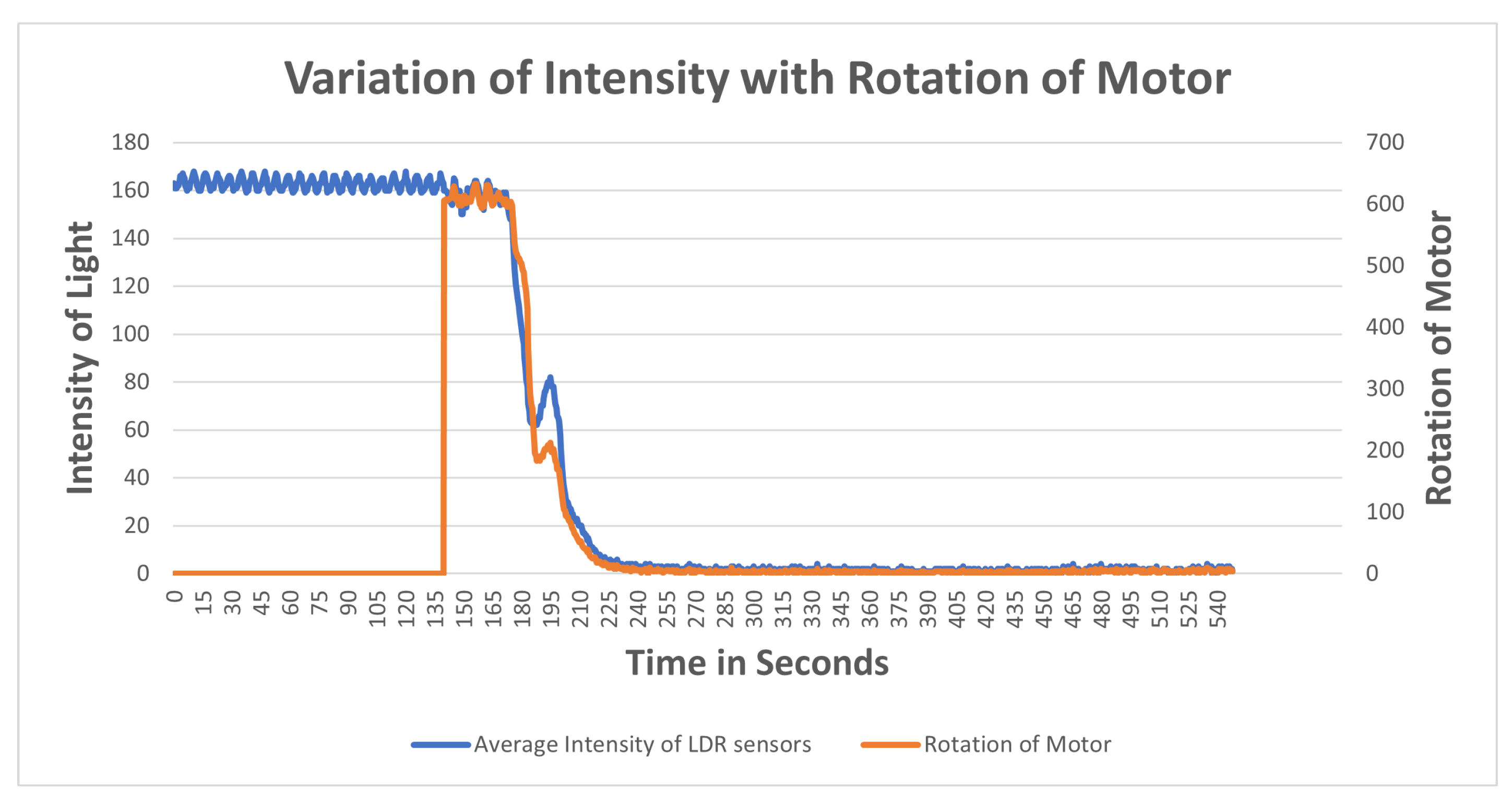
4.3.2. Variation of Intensity of Light
The aim of this experiment was to investigate how light intensity varies with respect to the rotation of the motor which adjusts the mask straps attached to the mask brace. Understanding this behavior allows the creation of an optimal automatic mask adjustment algorithm. When the microprocessor is powered up, LDR sensors begin capturing the intensity of the light, and after some time, when the motor is turned on, an immediate spin in the motor is noticed, which begins tightening the strap of the brace. As a result, the mask brace is pulled closer to the user’s face, and the light intensity of the sensor gradually decreases, slowing the rotation. When the light intensity hits zero, the spinning of motor gears stops. The algorithm was developed to rotate the motor depending on the intensity of light such that for a single intensity of light there is rotation in the motor based on the amount of power which means if the intensity of light from the average of LDR sensors is 1 then there is a power from the DC motor but there is not enough torque to rotate the gears.
The observation of variation of intensity is divided into three steps. The procedure for the experiment is that the mask brace is put on; it does not fit and is a bit loose in the beginning. The average intensity of the upper two LDR sensors is computed with the rotation of power in the first stage, then the bottom two, and finally all of the sensors at their positions are turned on and the rotation of the motor is determined. Each graph is plotted on the axis of time and rotation of the motor, where x is time and the secondary y-axis is a rotation of the motor. The primary x-axis is a variable entity that varies with time and rotation. The variable entity in each graph is plotted with a logarithmic function below to show the skewness of the larger data of intensity temperature and humidity with the rotation of the motor in order to determine the percent change or factors that affect the motor rotation.
Observation for upper two sensors
Figure 17 illustrates the results of an experiment when the mask was mounted, no power was supplied to the motors, as witnessed from time 0–42.4, the sensors measuring the intensity with no rotation. Motors were switched on from 42.4 to 47.4 and a light source was directed at sensors at the same time. When the intensity of light reaches 400, the rotation of the motor detected is 402, indicating that at higher intensities, there is maximum rotation. The intensity of light gradually decreases as the rotation slows down between 56 and 115 seconds. A progressive shift is noted at the time period of 115 s after which both intensity and rotation have a steady decline in values. At the interval of 121 seconds the intensity starts varying in the range of 0–1; at this interval, rotation becomes variable in the range of 0–10. Algorithm 1 is being satisfied here. From the plot it is observed that as the length of the strap decreases the average intensity of LDR sensors decreases which also meets the hypothesis in
Section 4.1 that tightness is inversely proportional to the length of the strap and it increases with the decrease in intensity. It can also be concluded that the rotation of the motor is directly proportional to the intensity of light.
Observation for bottom two sensors
The aim of this experiment was to investigate the impact on the bottom LDR sensors during the mask adjustment process. The experiment is performed in the same way as for the upper two sensors. The bottom sensor starts sensing the intensity while the motor was off. From
Figure 18 it can be observed that the variation of average intensity of the bottom two LDR sensors is different to that of the average of the upper sensors and to the rotation of the motor. When the motor is turned on it takes some time to process the intensity and then starts decreasing gradually. It is observed that the rotation of the motor is directly proportional to the average intensity sensed by the bottom LDR sensors. The rate of variation as compared to the upper two sensors is significantly distinct because of the position of the sensors and the face structure. The bottom two sensors cover the area of the face near to the chin and jaw line. The position of the source of light is always directed towards the face from the ceiling, which in this case results in low/less light reaching the bottom two sensors. This results in less intensity captured and lowers the speed of rotation as compared to the upper two sensors.
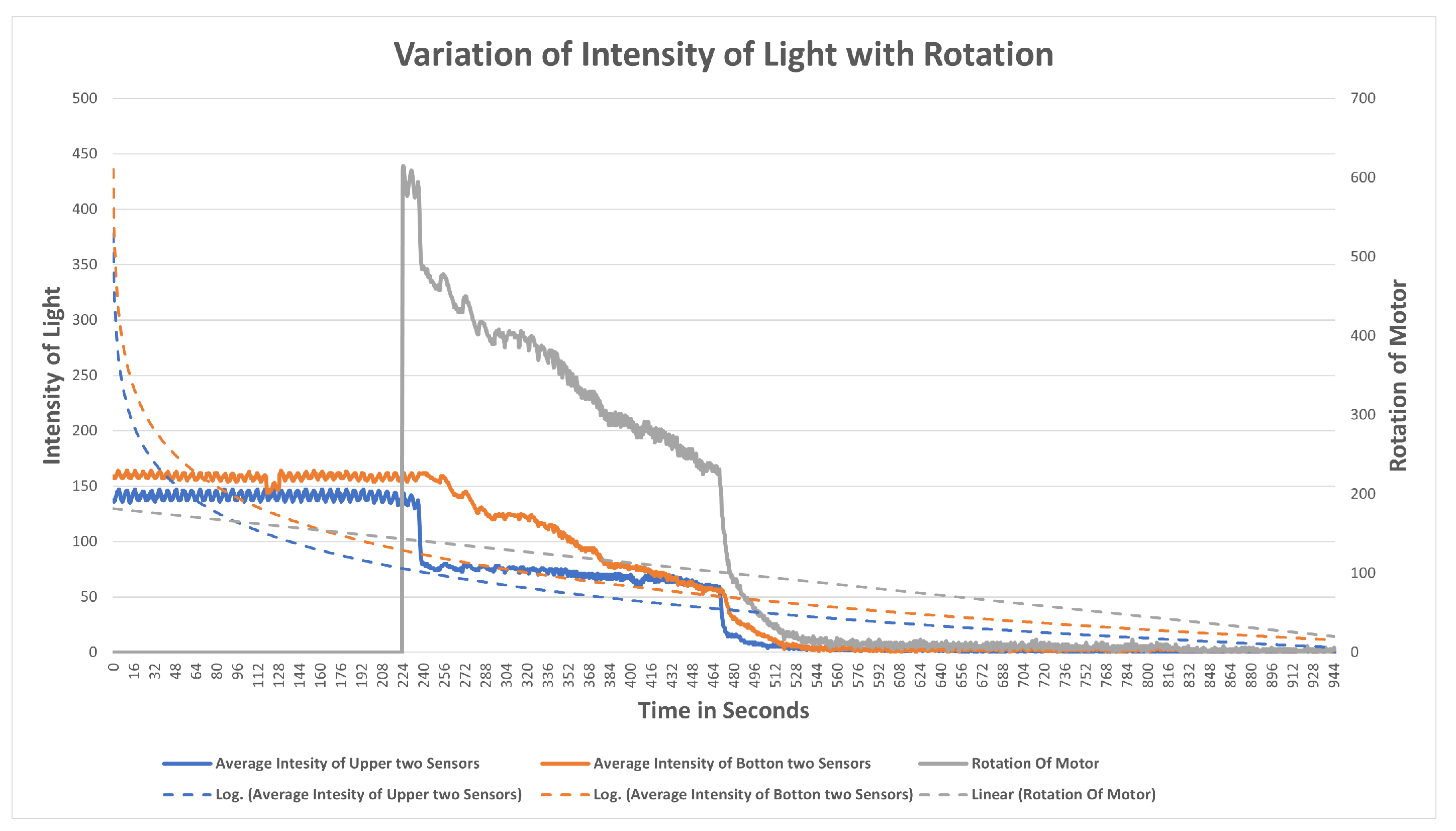
Observation of All Sensors
When all the sensors are put to working in a similar scenario,
Figure 19 is obtained, in which the grey line indicates the rotation of the motor, the blue line indicates the average intensity of the upper two sensors, and the orange line indicates the average intensity of the bottom two sensors. The behavior of the graph is mocking the same variation as that of the above scenarios, which is that average intensity is directly proportional to the rotation of the motor with a multiple of 4.081. The graph depicts a clear picture of variation when the motor is turned on; in a few seconds there is a gradual decrease in the intensity of the LDR sensor and it is strictly decreasing with a decrease in the intensity. The resulting plot satisfies the behavior of all the upper and the bottom sensor processes with the rotation of gears and the DC motor.
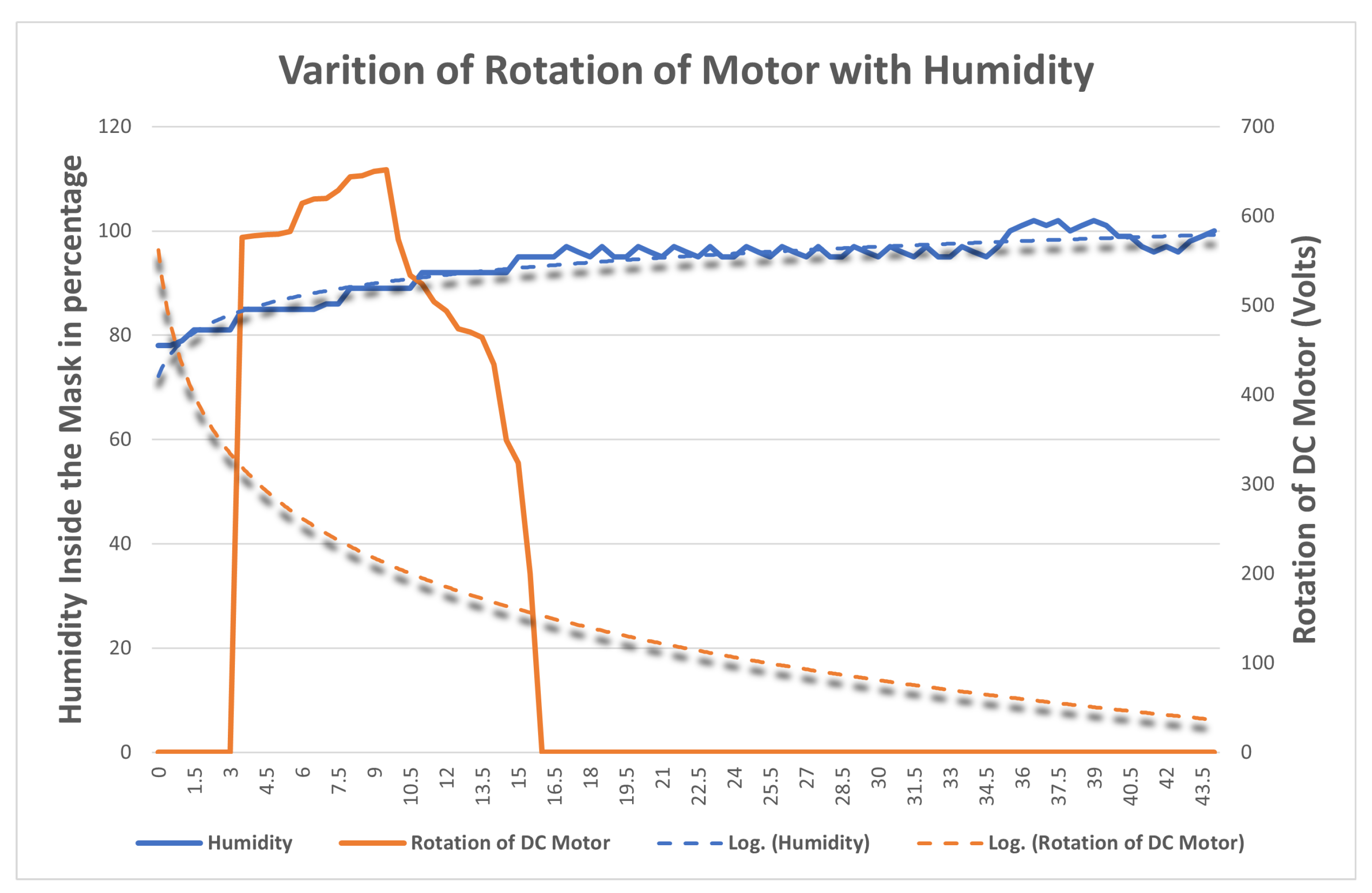
4.3.3. Variation of Temperature and Humidity Inside the Mask
The aim is to find the variation of temperature and humidity of the DHT11 sensors inside by changing the length of the string with the DC Motor. The DHT11 sensor is fitted inside the cavity of the filter attached to the mask brace. The setup is similar to that in
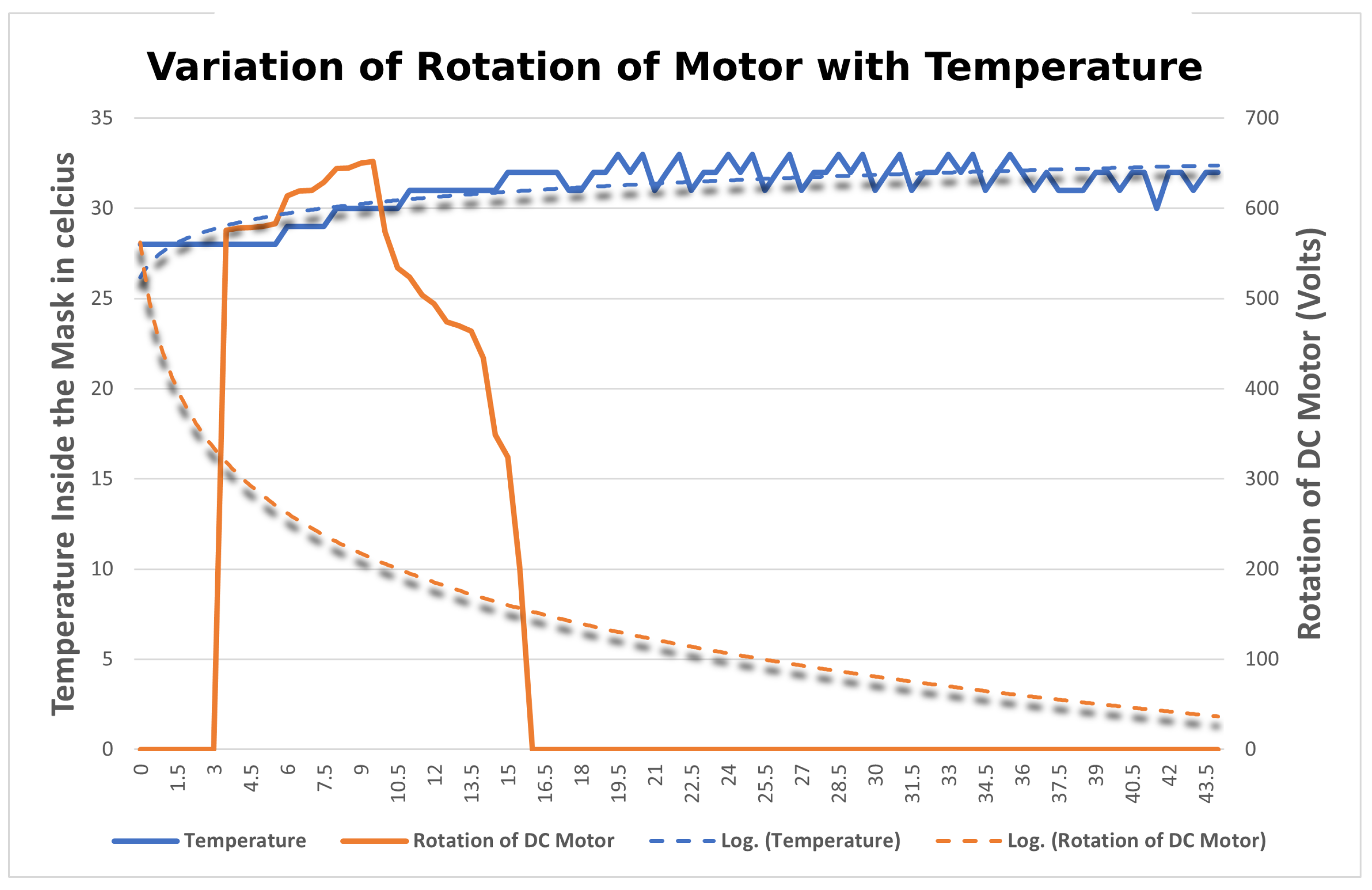
Section 4.3.2. The sensor collects the temperature and humidity readings at different lengths of string and their readings are compared and categorized with the rotation of the motor. The variation of temperature and humidity sensor is plotted onto a graph in
Figure 20 and
Figure 21, respectively. When the motor starts rotating there is a gradual increase in the temperature and humidity observed inside the mask. The blue line in the graph indicates the temperature and humidity and the orange line indicates the rotation of the motor. When the temperature and humidity start varying in the range of 90–100, the rotation of the motor starts decreasing. After analyzing the results, it was observed that the readings of the DHT11 sensor are quite different from that of the LDR sensor. As the length of the strap is tightened, the temperature and humidity recorded by the sensor located on the inner side vary inversely with the rotation of the motor. This is because the length of the string decreases and the mask is fitting to the user’s face as a result of the humidity inside the mask increasing. Thus, it can be concluded that the mask is tight for the user if the temperature and humidity are maximum inside, which also implies that the mask is a perfect fit for the user.
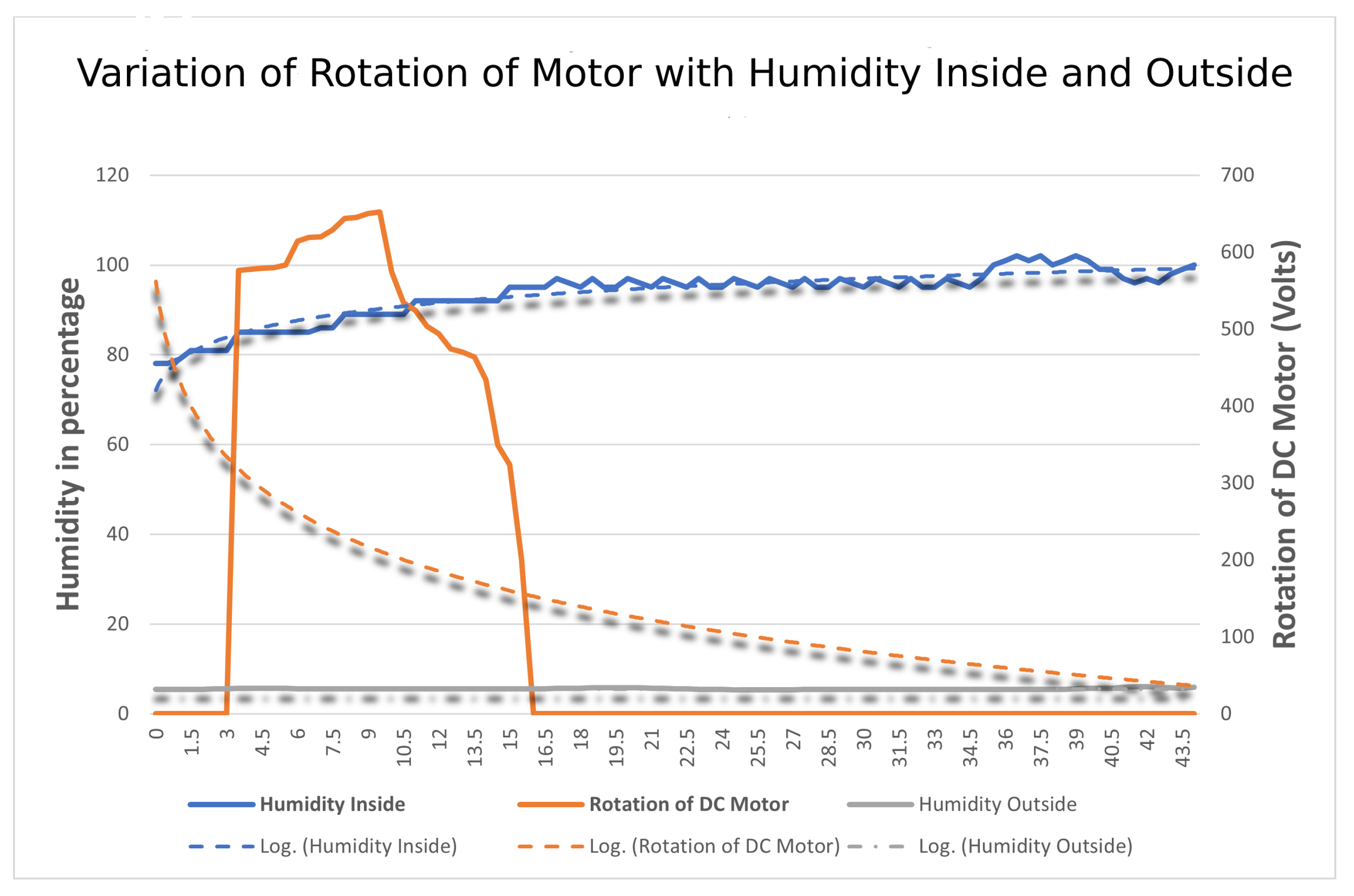
4.3.4. Variation of Humidity Inside and Outside
The aim is to find the comparison of humidity of DHT11 sensors both outside and inside by changing the length of the string with the rotation of the DC Motor. In this, a total of two DHT11 sensors are used, one inside and the other outside, retrofitted in the middle of the mask. The setup is similar to that in
Section 4.3.3. All the sensors collect the humidity reading at different lengths of string and their readings are compared and categorized according to the sensor located in and out of the mask with the power given to the DC Motor in terms of rotation. The variation of humidity of sensors is plotted onto a graph in
Figure 22 w.r.t to time at the X-axis, humidity, and rotation of motor recorded at the Y-axis. After analyzing the results, it was observed that the readings of the DHT11 sensor outside of the masks were quite different from the one present inside. As the length of the strap is tightened, humidity recorded by the sensor located on the inner side varies inversely with the humidity recorded by the sensor located outside.
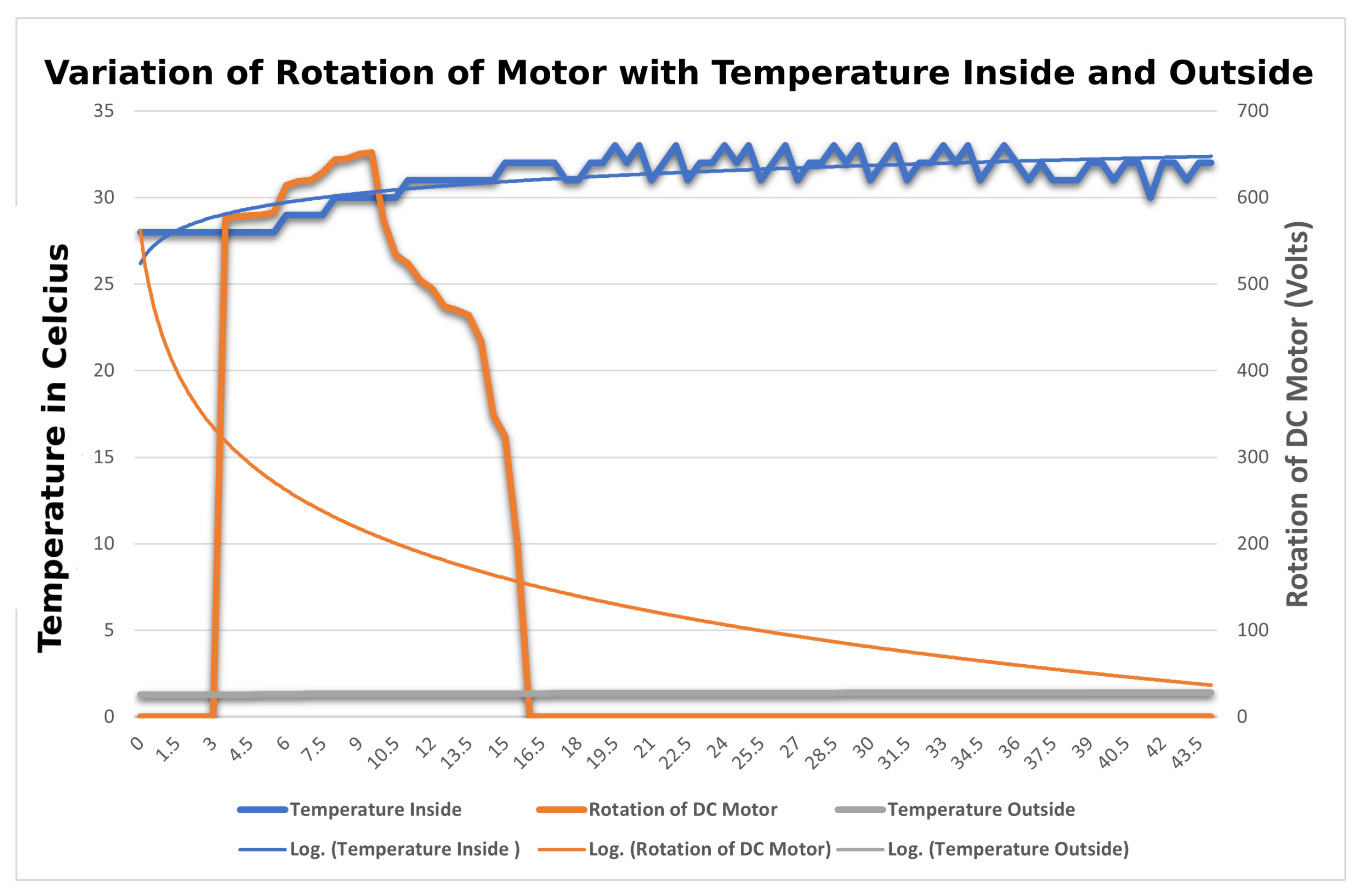
4.3.5. Variation of Temperature Inside and Outside
The aim is to find the comparison of the temperature of DHT11 sensors both outside and inside by changing the length of the string. In this, a total of two DHT11 sensors are used, one inside and the other outside, retrofitted in the middle of the mask. The setup is similar to that in
Section 4.3.4. All the sensors collect the temperature readings at different lengths of string and their readings are compared and categorized according to the sensor located in and out of the mask with the power given to the DC Motor in terms of rotation. The variation of temperatures of sensors is plotted onto a graph in
Figure 23 w.r.t to time at the X-axis, temperature, and rotation of motor recorded at Y-axis. After analyzing the results, it was observed that the readings of the DHT11 sensor outside of the masks were quite different from the ones present inside. As the length of the strap is tightened, the temperature recorded by the sensor located on the inner side varied inversely with the temperature recorded by the sensor located on the outside.