Development and Analytical Evaluation of a Point-of-Care Electrochemical Biosensor for Rapid and Accurate SARS-CoV-2 Detection
Abstract
:1. Introduction
| Platforms | Analyte | Sensitivity and LoD | Response Time | Advantages | Refs. | |
|---|---|---|---|---|---|---|
| Laboratory based | ||||||
| PCR | Nucleic Acid | 98–100% and 10–100 copies/mL | 3–4 h |
| [48,49,50,51] | |
| ELISA | Antigen, Antibodies | 85–90% and 0.01–0.1 ng | 1–5 h |
| [52,53,54] | |
| Point of Care (POCs) | ||||||
| RATs | Antigen | 60–70% and 10–100 PFU/mL | 13–15 min |
| [55,56,57] | |
| Biosensors | Electrical | Nucleic Acid Antigen | High and 0.1–1 fg/mL | 5–10 min |
| [19] |
| Optical | Antibody | 86.7% and <2 ng/spot | <30 min |
| [58] | |
| Optical | Nucleic Acid | 97.5% and 10 ng/mL | 30 min |
| [37] | |
| Optical | Antigen | High and 100 copies/mL | <15 min |
| [59] | |
| Opto-magnetic | Nucleic Acid | 10 copies/µL and 0.4 fM | 100 min |
| [60] | |
| Electrochemical | N-gene | 231 copies/µL and <10 copies/µL | <5 min |
| [61] | |
| Electrochemical | Reactive oxygen species | 97% and <500 µL | <30 s |
| [62] | |
| Electrochemical | Spike Protein | 77.8% and 20–30 copies/mL | <1 min |
| [20] | |
| Electrochemical | Spike Protein | High and 18.2 ng/mL | 15 min |
| [35]. | |
| Electrochemical | Antigen | 95% and 40 TCID50/mL | 1 min |
| This Work | |
2. Materials and Methods
2.1. Reagents
2.2. Viruses and Clinical Specimens
2.3. Development of the Biosensors
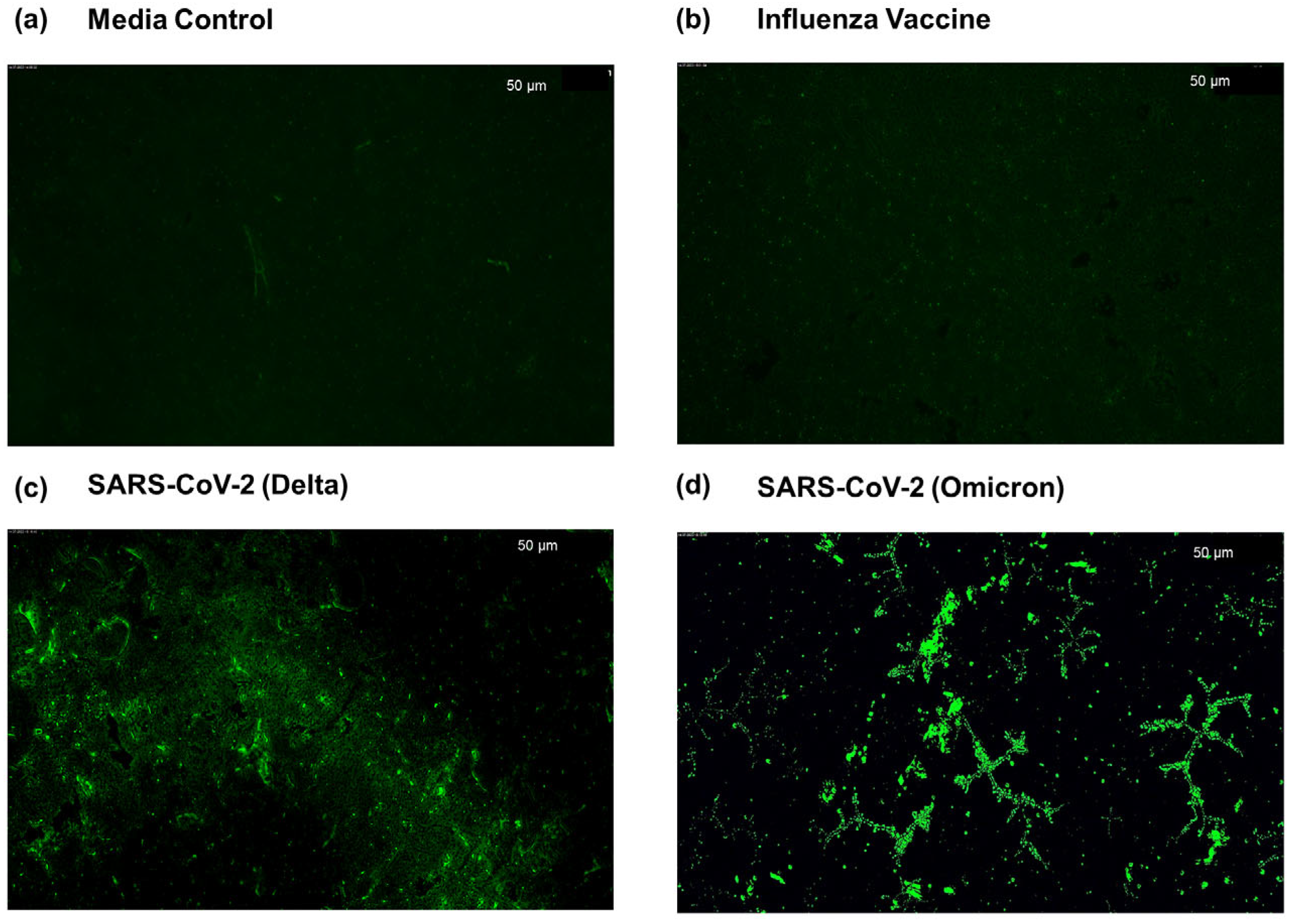
2.4. Assessment of Selective hACE-2 Peptide Binding to SARS-CoV-2
2.5. Electrochemical Impedance Measurement
3. Results and Discussion
3.1. Characterization of Biosensor and Detection of SARS-CoV-2 Using Electrochemical Impedance Spectroscopy

3.2. Determination of Virus Detection Based on Relative Impedance Threshold
3.3. Limit of Detection, Sensitivity, and Specificity of the Biosensor

4. Conclusions
5. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dhama, K.; Khan, S.; Tiwari, R.; Sircar, S.; Bhat, S.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Coronavirus Disease 2019–COVID-19. Clin. Microbiol. Rev. 2020, 33, e00028-20. [Google Scholar] [CrossRef] [PubMed]
- Pascarella, G.; Strumia, A.; Piliego, C.; Bruno, F.; Del Buono, R.; Costa, F.; Scarlata, S.; Agrò, F.E. COVID-19 Diagnosis and Management: A Comprehensive Review. J. Intern. Med. 2020, 288, 192–206. [Google Scholar] [CrossRef]
- More, N.; Ranglani, D.; Kharche, S.; Choppadandi, M.; Ghosh, S.; Vaidya, S.; Kapusetti, G. Current Challenges in Identification of Clinical Characteristics and Detection of COVID-19: A Comprehensive Review. Meas. Sens. 2021, 16, 100052. [Google Scholar] [CrossRef] [PubMed]
- Mohite, V.; Vyas, K.; Phadke, G.; Rawtani, D. Challenges and Future Aspects of COVID-19 Monitoring and Detection. In COVID-19 in the Environment; Elsevier: Amsterdam, The Netherlands, 2022; pp. 131–150. ISBN 978-0-323-90272-4. [Google Scholar]
- Rahman, M.M.; Masum, M.H.U.; Wajed, S.; Talukder, A. A Comprehensive Review on COVID-19 Vaccines: Development, Effectiveness, Adverse Effects, Distribution and Challenges. VirusDisease 2022, 33, 1–22. [Google Scholar] [CrossRef]
- Ndwandwe, D.; Wiysonge, C.S. COVID-19 Vaccines. Curr. Opin. Immunol. 2021, 71, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Pokhrel, P.; Hu, C.; Mao, H. Detecting the Coronavirus (COVID-19). ACS Sens. 2020, 5, 2283–2296. [Google Scholar] [CrossRef]
- Ji, T.; Liu, Z.; Wang, G.; Guo, X.; Akbar Khan, S.; Lai, C.; Chen, H.; Huang, S.; Xia, S.; Chen, B.; et al. Detection of COVID-19: A Review of the Current Literature and Future Perspectives. Biosens. Bioelectron. 2020, 166, 112455. [Google Scholar] [CrossRef] [PubMed]
- Filchakova, O.; Dossym, D.; Ilyas, A.; Kuanysheva, T.; Abdizhamil, A.; Bukasov, R. Review of COVID-19 Testing and Diagnostic Methods. Talanta 2022, 244, 123409. [Google Scholar] [CrossRef]
- Teymouri, M.; Mollazadeh, S.; Mortazavi, H.; Naderi Ghale-noie, Z.; Keyvani, V.; Aghababaei, F.; Hamblin, M.R.; Abbaszadeh-Goudarzi, G.; Pourghadamyari, H.; Hashemian, S.M.R.; et al. Recent Advances and Challenges of RT-PCR Tests for the Diagnosis of COVID-19. Pathol. Res. Pract. 2021, 221, 153443. [Google Scholar] [CrossRef]
- Feng, W.; Newbigging, A.M.; Le, C.; Pang, B.; Peng, H.; Cao, Y.; Wu, J.; Abbas, G.; Song, J.; Wang, D.-B.; et al. Molecular Diagnosis of COVID-19: Challenges and Research Needs. Anal. Chem. 2020, 92, 10196–10209. [Google Scholar] [CrossRef]
- Routsias, J.G.; Mavrouli, M.; Tsoplou, P.; Dioikitopoulou, K.; Tsakris, A. Diagnostic Performance of Rapid Antigen Tests (RATs) for SARS-CoV-2 and Their Efficacy in Monitoring the Infectiousness of COVID-19 Patients. Sci. Rep. 2021, 11, 22863. [Google Scholar] [CrossRef] [PubMed]
- Idili, A.; Arroyo-Currás, N.; Ploense, K.L.; Csordas, A.T.; Kuwahara, M.; Kippin, T.E.; Plaxco, K.W. Seconds-Resolved Pharmacokinetic Measurements of the Chemotherapeutic Irinotecan in Situ in the Living Body. Chem. Sci. 2019, 10, 8164–8170. [Google Scholar] [CrossRef] [PubMed]
- Ligler, F.S.; Gooding, J.J. Lighting Up Biosensors: Now and the Decade To Come. Anal. Chem. 2019, 91, 8732–8738. [Google Scholar] [CrossRef] [PubMed]
- Mahshid, S.S.; Flynn, S.E.; Mahshid, S. The Potential Application of Electrochemical Biosensors in the COVID-19 Pandemic: A Perspective on the Rapid Diagnostics of SARS-CoV-2. Biosens. Bioelectron. 2021, 176, 112905. [Google Scholar] [CrossRef]
- Kaya, S.I.; Ozcelikay, G.; Mollarasouli, F.; Bakirhan, N.K.; Ozkan, S.A. Recent Achievements and Challenges on Nanomaterial Based Electrochemical Biosensors for the Detection of Colon and Lung Cancer Biomarkers. Sens. Actuators B Chem. 2022, 351, 130856. [Google Scholar] [CrossRef]
- Yang, G.; Xiao, Z.; Tang, C.; Deng, Y.; Huang, H.; He, Z. Recent Advances in Biosensor for Detection of Lung Cancer Biomarkers. Biosens. Bioelectron. 2019, 141, 111416. [Google Scholar] [CrossRef]
- Torrente-Rodríguez, R.M.; Martín, C.M.-S.; Gamella, M.; Pedrero, M.; Martínez-Bosch, N.; Navarro, P.; García De Frutos, P.; Pingarrón, J.M.; Campuzano, S. Electrochemical Immunosensing of ST2: A Checkpoint Target in Cancer Diseases. Biosensors 2021, 11, 202. [Google Scholar] [CrossRef]
- Ke, G.; Su, D.; Li, Y.; Zhao, Y.; Wang, H.; Liu, W.; Li, M.; Yang, Z.; Xiao, F.; Yuan, Y.; et al. An Accurate, High-Speed, Portable Bifunctional Electrical Detector for COVID-19. Sci. China Mater. 2021, 64, 739–747. [Google Scholar] [CrossRef]
- Ghumra, D.P.; Shetty, N.; McBrearty, K.R.; Puthussery, J.V.; Sumlin, B.J.; Gardiner, W.D.; Doherty, B.M.; Magrecki, J.P.; Brody, D.L.; Esparza, T.J.; et al. Rapid Direct Detection of SARS-CoV-2 Aerosols in Exhaled Breath at the Point of Care. ACS Sens. 2023, 8, 3023–3031. [Google Scholar] [CrossRef]
- Patel, S.K.; Surve, J.; Parmar, J.; Ahmed, K.; Bui, F.M.; Al-Zahrani, F.A. Recent Advances in Biosensors for Detection of COVID-19 and Other Viruses. IEEE Rev. Biomed. Eng. 2023, 16, 22–37. [Google Scholar] [CrossRef]
- Samson, R.; Navale, G.R.; Dharne, M.S. Biosensors: Frontiers in Rapid Detection of COVID-19. 3 Biotech 2020, 10, 385. [Google Scholar] [CrossRef] [PubMed]
- Ferrag, C.; Kerman, K. Grand Challenges in Nanomaterial-Based Electrochemical Sensors. Front. Sens. 2020, 1, 583822. [Google Scholar] [CrossRef]
- Gupta, P.; Tsai, K.; Ruhunage, C.K.; Gupta, V.K.; Rahm, C.E.; Jiang, D.; Alvarez, N.T. True Picomolar Neurotransmitter Sensor Based on Open-Ended Carbon Nanotubes. Anal. Chem. 2020, 92, 8536–8545. [Google Scholar] [CrossRef] [PubMed]
- Suherman, A.L.; Ngamchuea, K.; Tanner, E.E.L.; Sokolov, S.V.; Holter, J.; Young, N.P.; Compton, R.G. Electrochemical Detection of Ultratrace (Picomolar) Levels of Hg 2+ Using a Silver Nanoparticle-Modified Glassy Carbon Electrode. Anal. Chem. 2017, 89, 7166–7173. [Google Scholar] [CrossRef]
- Wu, Y.; Tilley, R.D.; Gooding, J.J. Challenges and Solutions in Developing Ultrasensitive Biosensors. J. Am. Chem. Soc. 2019, 141, 1162–1170. [Google Scholar] [CrossRef]
- Aydemir, N.; Malmström, J.; Travas-Sejdic, J. Conducting Polymer Based Electrochemical Biosensors. Phys. Chem. Chem. Phys. 2016, 18, 8264–8277. [Google Scholar] [CrossRef]
- Ahmadi, M.; Ahour, F. An Electrochemical Biosensor Based on a Graphene Oxide Modified Pencil Graphite Electrode for Direct Detection and Discrimination of Double-Stranded DNA Sequences. Anal. Methods 2020, 12, 4541–4550. [Google Scholar] [CrossRef]
- Pan, D.; Gu, Y.; Lan, H.; Sun, Y.; Gao, H. Functional Graphene-Gold Nano-Composite Fabricated Electrochemical Biosensor for Direct and Rapid Detection of Bisphenol A. Anal. Chim. Acta 2015, 853, 297–302. [Google Scholar] [CrossRef]
- Hwang, H.S.; Jeong, J.W.; Kim, Y.A.; Chang, M. Carbon Nanomaterials as Versatile Platforms for Biosensing Applications. Micromachines 2020, 11, 814. [Google Scholar] [CrossRef]
- Heeger, A.J. Semiconducting and Metallic Polymers: The Fourth Generation of Polymeric Materials. J. Phys. Chem. B 2001, 105, 8475–8491. [Google Scholar] [CrossRef]
- Naseri, M.; Fotouhi, L.; Ehsani, A. Recent Progress in the Development of Conducting Polymer-Based Nanocomposites for Electrochemical Biosensors Applications: A Mini-Review. Chem. Rec. 2018, 18, 599–618. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.R.; Caseli, L.; Crespilho, F.N.; Zucolotto, V.; Oliveira, O.N. Immobilization of Biomolecules on Nanostructured Films for Biosensing. Biosens. Bioelectron. 2010, 25, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Tereshchenko, A.; Bechelany, M.; Viter, R.; Khranovskyy, V.; Smyntyna, V.; Starodub, N.; Yakimova, R. Optical Biosensors Based on ZnO Nanostructures: Advantages and Perspectives. A Review. Sens. Actuators B Chem. 2016, 229, 664–677. [Google Scholar] [CrossRef]
- Soto, D.; Orozco, J. Peptide-Based Simple Detection of SARS-CoV-2 with Electrochemical Readout. Anal. Chim. Acta 2022, 1205, 339739. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Wang, J.; Boyd, B.J. Peptide-Based Biosensors. Talanta 2015, 136, 114–127. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.W.; Jeon, W.-Y.; Yoon, B.K.; Jackman, J.A. Mechanistic Evaluation of Antimicrobial Lipid Interactions with Tethered Lipid Bilayers by Electrochemical Impedance Spectroscopy. Sensors 2022, 22, 3712. [Google Scholar] [CrossRef]
- Chen, C.; Jiang, Y.; Kan, J. A Noninterference Polypyrrole Glucose Biosensor. Biosens. Bioelectron. 2006, 22, 639–643. [Google Scholar] [CrossRef]
- Magar, H.S.; Hassan, R.Y.A.; Mulchandani, A. Electrochemical Impedance Spectroscopy (EIS): Principles, Construction, and Biosensing Applications. Sensors 2021, 21, 6578. [Google Scholar] [CrossRef]
- Huerta-Nuñez, L.F.E.; Gutierrez-Iglesias, G.; Martinez-Cuazitl, A.; Mata-Miranda, M.M.; Alvarez-Jiménez, V.D.; Sánchez-Monroy, V.; Golberg, A.; González-Díaz, C.A. A Biosensor Capable of Identifying Low Quantities of Breast Cancer Cells by Electrical Impedance Spectroscopy. Sci. Rep. 2019, 9, 6419. [Google Scholar] [CrossRef]
- Letko, M.; Marzi, A.; Munster, V. Functional Assessment of Cell Entry and Receptor Usage for SARS-CoV-2 and Other Lineage B Betacoronaviruses. Nat. Microbiol. 2020, 5, 562–569. [Google Scholar] [CrossRef]
- Shang, J.; Wan, Y.; Luo, C.; Ye, G.; Geng, Q.; Auerbach, A.; Li, F. Cell Entry Mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA 2020, 117, 11727–11734. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Penninger, J.M.; Li, Y.; Zhong, N.; Slutsky, A.S. Angiotensin-Converting Enzyme 2 (ACE2) as a SARS-CoV-2 Receptor: Molecular Mechanisms and Potential Therapeutic Target. Intensive Care Med. 2020, 46, 586–590. [Google Scholar] [CrossRef]
- Lupala, C.S.; Li, X.; Lei, J.; Chen, H.; Qi, J.; Liu, H.; Su, X. Computational Simulations Reveal the Binding Dynamics between Human ACE2 and the Receptor Binding Domain of SARS-CoV-2 Spike Protein. Quant. Biol. 2020, 9, 61–72. [Google Scholar] [CrossRef]
- Lupala, C.S.; Kumar, V.; Li, X.; Su, X.; Liu, H. Computational Analysis on the ACE2-Derived Peptides for Neutralizing the ACE2 Binding to the Spike Protein of SARS-CoV-2. bioRxiv 2020. [Google Scholar] [CrossRef]
- Maas, M.N.; Hintzen, J.C.J.; Löffler, P.M.G.; Mecinović, J. Targeting SARS-CoV-2 Spike Protein by Stapled hACE2 Peptides. Chem. Commun. 2021, 57, 3283–3286. [Google Scholar] [CrossRef] [PubMed]
- Nevola, L.; Giralt, E. Modulating Protein–Protein Interactions: The Potential of Peptides. Chem. Commun. 2015, 51, 3302–3315. [Google Scholar] [CrossRef]
- Arnaout, R.; Lee, R.A.; Lee, G.R.; Callahan, C.; Cheng, A.; Yen, C.F.; Smith, K.P.; Arora, R.; Kirby, J.E. The Limit of Detection Matters: The Case for Benchmarking Severe Acute Respiratory Syndrome Coronavirus 2 Testing. Clin. Infect. Dis. 2021, 73, e3042–e3046. [Google Scholar] [CrossRef]
- Skittrall, J.P.; Wilson, M.; Smielewska, A.A.; Parmar, S.; Fortune, M.D.; Sparkes, D.; Curran, M.D.; Zhang, H.; Jalal, H. Specificity and Positive Predictive Value of SARS-CoV-2 Nucleic Acid Amplification Testing in a Low-Prevalence Setting. Clin. Microbiol. Infect. 2021, 27, 469.e9–469.e15. [Google Scholar] [CrossRef]
- He, R.; Liu, H.; Niu, Y.; Zhang, H.; Genin, G.M.; Xu, F. Flexible Miniaturized Sensor Technologies for Long-Term Physiological Monitoring. Npj Flex. Electron. 2022, 6, 20. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhang, S.; Qin, H.; Meng, S.; Deng, X.; Lin, H.; Xin, X.; Liang, Y.; Chen, B.; Cui, Y.; et al. Establishment of a Quantitative RT-PCR Detection of SARS-CoV-2 Virus. Eur. J. Med. Res. 2021, 26, 147. [Google Scholar] [CrossRef]
- Younes, N.; Al-Sadeq, D.W.; AL-Jighefee, H.; Younes, S.; Al-Jamal, O.; Daas, H.I.; Yassine, H.M.; Nasrallah, G.K. Challenges in Laboratory Diagnosis of the Novel Coronavirus SARS-CoV-2. Viruses 2020, 12, 582. [Google Scholar] [CrossRef] [PubMed]
- Carter, L.J.; Garner, L.V.; Smoot, J.W.; Li, Y.; Zhou, Q.; Saveson, C.J.; Sasso, J.M.; Gregg, A.C.; Soares, D.J.; Beskid, T.R.; et al. Assay Techniques and Test Development for COVID-19 Diagnosis. ACS Cent. Sci. 2020, 6, 591–605. [Google Scholar] [CrossRef] [PubMed]
- Van Elslande, J.; Houben, E.; Depypere, M.; Brackenier, A.; Desmet, S.; André, E.; Van Ranst, M.; Lagrou, K.; Vermeersch, P. Diagnostic Performance of Seven Rapid IgG/IgM Antibody Tests and the Euroimmun IgA/IgG ELISA in COVID-19 Patients. Clin. Microbiol. Infect. 2020, 26, 1082–1087. [Google Scholar] [CrossRef] [PubMed]
- Brihn, A.; Chang, J.; OYong, K.; Balter, S.; Terashita, D.; Rubin, Z.; Yeganeh, N. Diagnostic Performance of an Antigen Test with RT-PCR for the Detection of SARS-CoV-2 in a Hospital Setting—Los Angeles County, California, June–August 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Jeewandara, C.; Guruge, D.; Pushpakumara, P.D.; Madhusanka, D.; Jayadas, T.T.; Chaturanga, I.P.; Aberathna, I.S.; Danasekara, S.; Pathmanathan, T.; Jayathilaka, D.; et al. Sensitivity and Specificity of Two WHO Approved SARS-CoV2 Antigen Assays in Detecting Patients with SARS-CoV2 Infection. BMC Infect. Dis. 2022, 22, 276. [Google Scholar] [CrossRef]
- Bangar, M.A.; Shirale, D.J.; Chen, W.; Myung, N.V.; Mulchandani, A. Single Conducting Polymer Nanowire Chemiresistive Label-Free Immunosensor for Cancer Biomarker. Anal. Chem. 2009, 81, 2168–2175. [Google Scholar] [CrossRef]
- Cady, N.C.; Tokranova, N.; Minor, A.; Nikvand, N.; Strle, K.; Lee, W.T.; Page, W.; Guignon, E.; Pilar, A.; Gibson, G.N. Multiplexed Detection and Quantification of Human Antibody Response to COVID-19 Infection Using a Plasmon Enhanced Biosensor Platform. Biosens. Bioelectron. 2021, 171, 112679. [Google Scholar] [CrossRef]
- Sitjar, J.; Liao, J.-D.; Lee, H.; Tsai, H.-P.; Wang, J.-R.; Liu, P.-Y. Challenges of SERS Technology as a Non-Nucleic Acid or -Antigen Detection Method for SARS-CoV-2 Virus and Its Variants. Biosens. Bioelectron. 2021, 181, 113153. [Google Scholar] [CrossRef]
- Tian, B.; Gao, F.; Fock, J.; Dufva, M.; Hansen, M.F. Homogeneous Circle-to-Circle Amplification for Real-Time Optomagnetic Detection of SARS-CoV-2 RdRp Coding Sequence. Biosens. Bioelectron. 2020, 165, 112356. [Google Scholar] [CrossRef]
- Alafeef, M.; Dighe, K.; Moitra, P.; Pan, D. Rapid, Ultrasensitive, and Quantitative Detection of SARS-CoV-2 Using Antisense Oligonucleotides Directed Electrochemical Biosensor Chip. ACS Nano 2020, 14, 17028–17045. [Google Scholar] [CrossRef]
- Miripour, Z.S.; Sarrami-Forooshani, R.; Sanati, H.; Makarem, J.; Taheri, M.S.; Shojaeian, F.; Eskafi, A.H.; Abbasvandi, F.; Namdar, N.; Ghafari, H.; et al. Real-Time Diagnosis of Reactive Oxygen Species (ROS) in Fresh Sputum by Electrochemical Tracing; Correlation between COVID-19 and Viral-Induced ROS in Lung/Respiratory Epithelium during This Pandemic. Biosens. Bioelectron. 2020, 165, 112435. [Google Scholar] [CrossRef] [PubMed]
- McMaster, W.C.; Kouzelos, J.; Liddle, S.; Waugh, T.R. Tendon Grafting with Glutaraldehyde Fixed Material. J. Biomed. Mater. Res. 1976, 10, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Habeeb, A.F.S.A.; Hiramoto, R. Reaction of Proteins with Glutaraldehyde. Arch. Biochem. Biophys. 1968, 126, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Bigdeli, I.K.; Yeganeh, M.; Shoushtari, M.T.; Zadeh, M.K. Electrochemical Impedance Spectroscopy (EIS) for Biosensing. In Nanosensors for Smart Manufacturing; Elsevier: Amsterdam, The Netherlands, 2021; pp. 533–554. ISBN 978-0-12-823358-0. [Google Scholar]
- Do, J.-S.; Wang, S.-H. On the Sensitivity of Conductimetric Acetone Gas Sensor Based on Polypyrrole and Polyaniline Conducting Polymers. Sens. Actuators B Chem. 2013, 185, 39–46. [Google Scholar] [CrossRef]
- Zhao, C.; Wang, H.; Zhang, H. Bio-Inspired Artificial Ion Channels: From Physical to Chemical Gating. Mater. Chem. Front. 2021, 5, 4059–4072. [Google Scholar] [CrossRef]
- Rohatgi, V.K.; Saleh, A.K.M.E.; Rohatgi, V.K. An Introduction to Probability and Statistics, 2nd ed.; Wiley Series in Probability and Statistics; Wiley: New York, NY, USA, 2001; ISBN 978-0-471-34846-7. [Google Scholar]
- Sadani, K.; Muthuraj, L.; Nag, P.; Fernandes, M.; Kondabagil, K.; Mukhopadhyay, C.; Mukherji, S. A Point of Use Sensor Assay for Detecting Purely Viral versus Viral-Bacterial Samples. Sens. Actuators B Chem. 2020, 322, 128562. [Google Scholar] [CrossRef]
- Mondal, D.; Paul, D.; Mukherji, S. Impedance Spectroscopy-Based Detection of Cardiac Biomarkers on Polyaniline Coated Filter Paper. IEEE Sens. J. 2017, 17, 5021–5029. [Google Scholar] [CrossRef]
- Kamran, A.; Guozhu, L.; Rafique, A.F.; Zeeshan, Q. ±3-Sigma Based Design Optimization of 3D Finocyl Grain. Aerosp. Sci. Technol. 2013, 26, 29–37. [Google Scholar] [CrossRef]
- Li, J.; Stones, R.J.; Wang, G.; Liu, X.; Li, Z.; Xu, M. Hard Drive Failure Prediction Using Decision Trees. Reliab. Eng. Syst. Saf. 2017, 164, 55–65. [Google Scholar] [CrossRef]
- Hastie, T.; Friedman, J.; Tibshirani, R. Boosting and Additive Trees. In The Elements of Statistical Learning; Springer Series in Statistics; Springer: New York, NY, USA, 2001; pp. 299–345. ISBN 978-1-4899-0519-2. [Google Scholar]
- Czibere, L.; Burggraf, S.; Becker, M.; Durner, J.; Draenert, M.E. Verification of Lateral Flow Antigen Tests for SARS-CoV-2 by qPCR Directly from the Test Device. Dent. Mater. 2022, 38, e155–e159. [Google Scholar] [CrossRef]
- Bekliz, M.; Adea, K.; Puhach, O.; Perez-Rodriguez, F.; Marques Melancia, S.; Baggio, S.; Corvaglia, A.-R.; Jacquerioz, F.; Alvarez, C.; Essaidi-Laziosi, M.; et al. Analytical Sensitivity of Eight Different SARS-CoV-2 Antigen-Detecting Rapid Tests for Omicron-BA.1 Variant. Microbiol. Spectr. 2022, 10, e00853-22. [Google Scholar] [CrossRef] [PubMed]
- Deerain, J.; Druce, J.; Tran, T.; Batty, M.; Yoga, Y.; Fennell, M.; Dwyer, D.E.; Kok, J.; Williamson, D.A. Assessment of the Analytical Sensitivity of 10 Lateral Flow Devices against the SARS-CoV-2 Omicron Variant. J. Clin. Microbiol. 2022, 60, e02479-21. [Google Scholar] [CrossRef] [PubMed]
- Walsh, K.A.; Jordan, K.; Clyne, B.; Rohde, D.; Drummond, L.; Byrne, P.; Ahern, S.; Carty, P.G.; O’Brien, K.K.; O’Murchu, E.; et al. SARS-CoV-2 Detection, Viral Load and Infectivity over the Course of an Infection. J. Infect. 2020, 81, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Corman, V.M.; Haage, V.C.; Bleicker, T.; Schmidt, M.L.; Mühlemann, B.; Zuchowski, M.; Jo, W.K.; Tscheak, P.; Möncke-Buchner, E.; Müller, M.A.; et al. Comparison of Seven Commercial SARS-CoV-2 Rapid Point-of-Care Antigen Tests: A Single-Centre Laboratory Evaluation Study. Lancet Microbe 2021, 2, e311–e319. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, B.; Hojaiji, H.; Wang, Z.; Lin, S.; Yeung, C.; Lin, H.; Nguyen, P.; Chiu, K.; Salahi, K.; et al. A Wearable Freestanding Electrochemical Sensing System. Sci. Adv. 2020, 6, eaaz0007. [Google Scholar] [CrossRef]
- Aliofkhazraei, M.; Ali, N. Recent Developments in Miniaturization of Sensor Technologies and Their Applications. In Comprehensive Materials Processing; Elsevier: Amsterdam, The Netherlands, 2014; pp. 245–306. ISBN 978-0-08-096533-8. [Google Scholar]
- Dahlin, A.B. Size Matters: Problems and Advantages Associated with Highly Miniaturized Sensors. Sensors 2012, 12, 3018–3036. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meshesha, M.; Sardar, A.; Supekar, R.; Bhattacharjee, L.; Chatterjee, S.; Halder, N.; Mohanta, K.; Bhattacharyya, T.K.; Pal, B. Development and Analytical Evaluation of a Point-of-Care Electrochemical Biosensor for Rapid and Accurate SARS-CoV-2 Detection. Sensors 2023, 23, 8000. https://doi.org/10.3390/s23188000
Meshesha M, Sardar A, Supekar R, Bhattacharjee L, Chatterjee S, Halder N, Mohanta K, Bhattacharyya TK, Pal B. Development and Analytical Evaluation of a Point-of-Care Electrochemical Biosensor for Rapid and Accurate SARS-CoV-2 Detection. Sensors. 2023; 23(18):8000. https://doi.org/10.3390/s23188000
Chicago/Turabian StyleMeshesha, Mesfin, Anik Sardar, Ruchi Supekar, Lopamudra Bhattacharjee, Soumyo Chatterjee, Nyancy Halder, Kallol Mohanta, Tarun Kanti Bhattacharyya, and Biplab Pal. 2023. "Development and Analytical Evaluation of a Point-of-Care Electrochemical Biosensor for Rapid and Accurate SARS-CoV-2 Detection" Sensors 23, no. 18: 8000. https://doi.org/10.3390/s23188000
APA StyleMeshesha, M., Sardar, A., Supekar, R., Bhattacharjee, L., Chatterjee, S., Halder, N., Mohanta, K., Bhattacharyya, T. K., & Pal, B. (2023). Development and Analytical Evaluation of a Point-of-Care Electrochemical Biosensor for Rapid and Accurate SARS-CoV-2 Detection. Sensors, 23(18), 8000. https://doi.org/10.3390/s23188000





