Participatory Action Design and Engineering of Powered Personal Transfer System for Wheelchair Users: Initial Design and Assessment
Abstract
1. Introduction
2. Materials and Methods
2.1. The Description of the PPTS
2.1.1. Overview
- Inhibit EPW driving mode during transfer;
- The EPW backrest must be displaced to clear the path between EPW and the bed;
- The EPW seat pan must move along with the bed’s leg segment to safely transfer the person (i.e., maintain the user’s posture/comfort);
- The PPTS will follow a finite-state machine model with checkpoints to ensure a safe transfer process (sensor feedback).
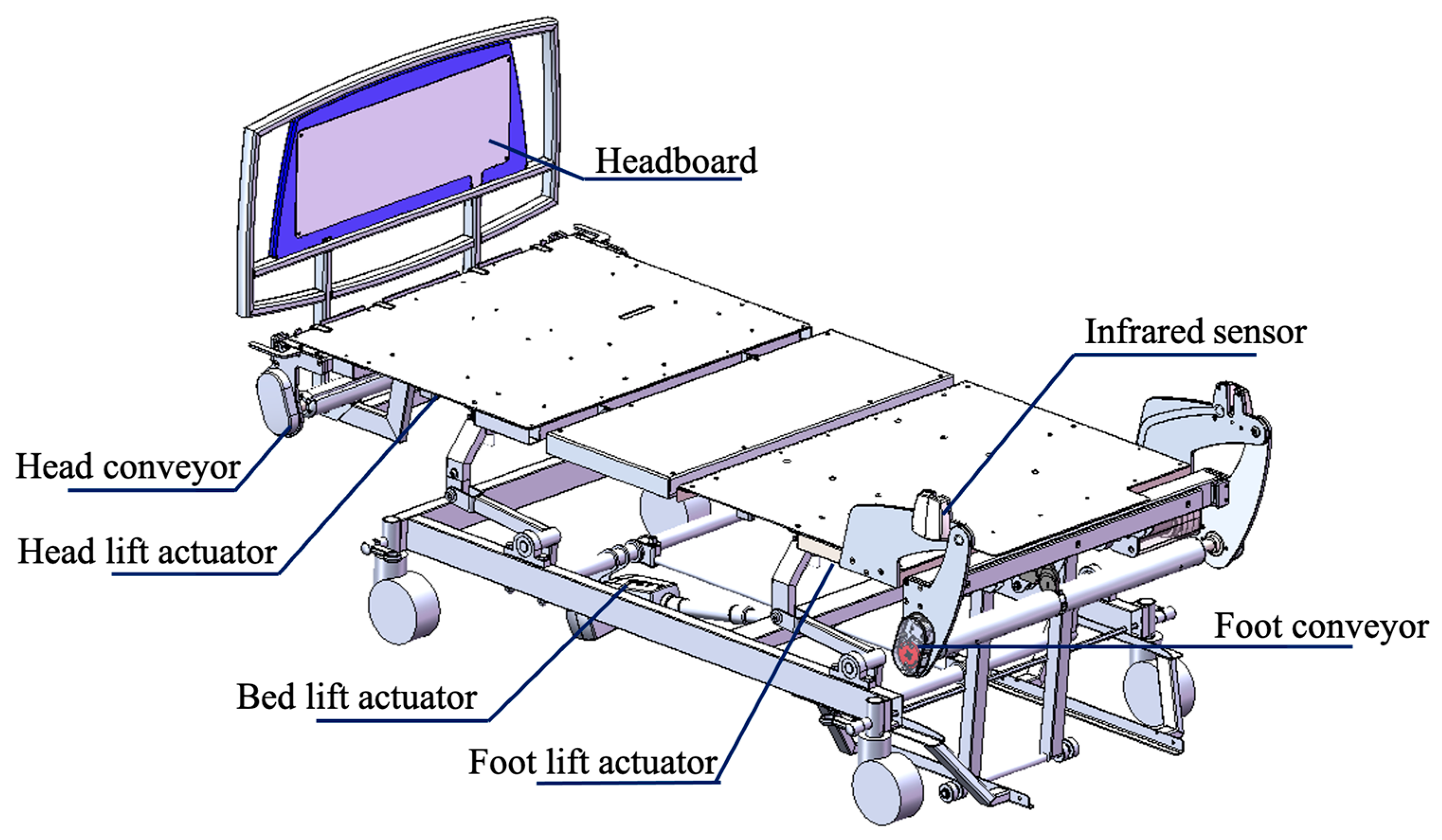
2.1.2. The Robotic Bed
2.1.3. The Chair
2.1.4. Cyberphysical System and Control
2.2. Transfer Process
2.3. PPTS Kinematic Analysis
2.4. Focus Groups
2.4.1. Participants
2.4.2. Focus Group Data Analysis
3. Results
3.1. PPTS System Verification
3.2. Focus Group Participants and Demographics
3.3. Focus Group Results
3.3.1. Overall Impressions
3.3.2. Best Features
3.3.3. People That Can Be Served by PPTS
3.3.4. Usability and Automation
3.3.5. Limitations of PPTS
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- U.S. Census Bureau. Americans with Disabilities: 2014. 2018. Available online: https://www.census.gov/content/dam/Census/library/publications/2018/demo/p70-152.pdf (accessed on 29 November 2019).
- Dicianno, B.E.; Joseph, J.; Eckstein, S.; Zigler, C.K.; Quinby, E.; Schmeler, M.R.; Schein, R.M.; Pearlman, J.; Cooper, R.A. The voice of the consumer: A survey of veterans and other users of assistive technology. Mil. Med. 2018, 183, e518–e525. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days away from Work, 2015; Technical Report; U.S. Department of Labor: Washington, DC, USA, 2015.
- Ribeiro, T.; Serranheira, F.; Loureiro, H. Work-related musculoskeletal disorders in primary health care nurses. Appl. Nurs. Res. 2017, 33, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Oranye, N.O.; Bennett, J. Prevalence of work-related musculoskeletal and non-musculoskeletal injuries in health care workers: The implications for work disability management. Ergonomics 2018, 61, 355–366. [Google Scholar] [CrossRef]
- Vieira, E.R.; Schneider, P.; Guidera, C.; Gadotti, I.C.; Brunt, D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J. Back Musculoskelet. Rehabil. 2016, 29, 417–428. [Google Scholar] [CrossRef]
- Darragh, A.R.; Sommerich, C.M.; Lavender, S.A.; Tanner, K.J.; Vogel, K.; Campo, M. Musculoskeletal discomfort, physical demand, and caregiving activities in informal caregivers. J. Appl. Gerontol. 2015, 34, 734–760. [Google Scholar] [CrossRef] [PubMed]
- Skotte, J.H.; Essendrop, M.; Hansen, A.F.; Schibye, B. A dynamic 3D biomechanical evaluation of the load on the low back during different patient-handling tasks. J. Biomech. 2002, 35, 1357–1366. [Google Scholar] [CrossRef]
- Marras, W.S.; Davis, K.G.; Kirking, B.C.; Bertsche, P.K. A comprehensive analysis of low-back disorder risk and spinal loading during the transferring and repositioning of patients using different techniques. Ergonomics 1999, 42, 904–926. [Google Scholar] [CrossRef]
- Andersen, L.L.; Burdorf, A.; Fallentin, N.; Persson, R.; Jakobsen, M.D.; Mortensen, O.S.; Clausen, T.; Holtermann, A. Patient transfers and assistive devices: Prospective cohort study on the risk for occupational back injury among healthcare workers. Scand. J. Work. Environ. Health 2014, 40, 74–81. [Google Scholar] [CrossRef]
- Pompeii, L.A.; Lipscomb, H.J.; Schoenfisch, A.L.; Dement, J.M. Musculoskeletal injuries resulting from patient handling tasks among hospital workers. Am. J. Ind. Med. 2009, 52, 571–578. [Google Scholar] [CrossRef]
- The National Caregiving Alliance; AARP Public Policy Institute. Caregiving in the U.S. 2015. Available online: https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf (accessed on 4 June 2023).
- Reinhard, S.C.; Given, B.; Petlick, N.H.; Bemis, A. Supporting family caregivers in providing care. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- Sivakanthan, S.; Blaauw, E.; Greenhalgh, M.; Koontz, A.M.; Vegter, R.; Cooper, R.A. Person transfer assist systems: A literature review. Disabil. Rehabil. Assist. Technol. 2021, 16, 270–279. [Google Scholar] [CrossRef]
- Sun, C.; Buchholz, B.; Quinn, M.; Punnett, L.; Galligan, C.; Gore, R. Ergonomic evaluation of slide boards used by home care aides to assist client transfers. Ergonomics 2018, 61, 913–922. [Google Scholar] [CrossRef]
- Owen, B.; Garg, A. Assistive devices for use with patient handling tasks. Adv. Ind. Ergon. Saf. 1990, 2, 585–592. [Google Scholar]
- Dutta, T.; Holliday, P.J.; Gorski, S.M.; Baharvandy, M.S.; Fernie, G.R. A biomechanical assessment of floor and overhead lifts using one or two caregivers for patient transfers. Appl. Ergon. 2012, 43, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Owen, B.; Beller, D.; Banaag, J. A biomechanical and ergonomic evaluation of patient transferring tasks: Bed to wheelchair and wheelchair to bed. Ergonomics 1991, 34, 289–312. [Google Scholar] [CrossRef] [PubMed]
- Seecharan, S.; Seecharan, S.; Genese, J.; Arana, C.; Liggett, A.; Kulsum, N.; Ahmad, R. Fall Risk Associated with Mechanical Lifts in Nursing Homes. J. Am. Med. Dir. Assoc. 2019, 20, B28. [Google Scholar] [CrossRef]
- Satpute, S.; Cooper, R.; Dicianno, B.E.; Joseph, J.; Chi, Y.; Cooper, R.A. Mini-review: Rehabilitation engineering: Research priorities and trends. Neurosci. Lett. 2021, 764, 136207. [Google Scholar] [CrossRef] [PubMed]
- Bostelman, R.; Albus, J. Home Lift Position and Rehabilitation (HLPR) Apparatus. U.S. Patent No. 7,827,630, 9 November 2010. [Google Scholar]
- Cooper, R.A.; Grindle, G.G.; McCartney, M. Robotic Strong Arm. U.S. Patent No. 9,254,234, 9 February 2016. [Google Scholar]
- Block, J.E.; Miller, L.E. AgileLife™; NextHealth, Inc.: Norwalk, CT, USA, 2011. [Google Scholar]
- Kulich, H.R.; Wei, L.; Crytzer, T.M.; Cooper, R.A.; Koontz, A.M. Preliminary evaluation of an automated robotic transfer assist device in the home setting. Disabil. Rehabil. Assist. Technol. 2021, 1–8. [Google Scholar] [CrossRef]
- Ding, D.; Cooper, R.A.; Pearlman, J. Incorporating participatory action design into research and education. In Proceedings of the International Conference on Electrical Engineering, Coimbra, Portugal, 3–7 September 2007. [Google Scholar]
- Cooper, R.A.; Ohnabe, H.; Hobson, D.A. (Eds.) An Introduction to Rehabilitation Engineering; CRC Press: Boca Raton, FL, USA, 2006. [Google Scholar]
- Cooper, R.A.; Beckstrom, D.; Curatolo, R.A.; Grindle, G.; Kovacsics, R. System and Methods for Powered Wheelchair Personal Transfer. U.S. Patent No. 10,322,048, 18 June 2019. [Google Scholar]
- Vicon Home Page. Available online: https://www.vicon.com (accessed on 11 February 2023).
- Colyer, S.L.; Evans, M.; Cosker, D.P.; Salo, A.I. A review of the evolution of vision-based motion analysis and the integration of advanced computer vision methods towards developing a markerless system. Sport. Med. Open 2018, 4, 24. [Google Scholar]
- Moro, M.; Marchesi, G.; Hesse, F.; Odone, F.; Casadio, M. Markerless vs. marker-based gait analysis: A proof of concept study. Sensors 2022, 22, 2011. [Google Scholar] [CrossRef]
- Niederberger, M.; Spranger, J. Delphi technique in health sciences: A map. Front. Public Health 2020, 8, 457. [Google Scholar] [CrossRef]
- Musich, S.; Wang, S.S.; Ruiz, J.; Hawkins, K.; Wicker, E. The impact of mobility limitations on health outcomes among older adults. Geriatr. Nurs. 2018, 39, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Beach, S.R.; Schulz, R.; Matthews, J.T.; Courtney, K.; Dabbs, A.D. Preferences for technology versus human assistance and control over technology in the performance of kitchen and personal care tasks in baby boomers and older adults. Disabil. Rehabil. Assist. Technol. 2014, 9, 474–486. [Google Scholar] [PubMed]
- Schulz, R. Quality of Life Technology Handbook; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Wiggermann, N.; Zhou, J.; McGann, N. Effect of repositioning aids and patient weight on biomechanical stresses when repositioning patients in bed. Hum. Factors 2021, 63, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Skotte, J.; Fallentin, N. Low back injury risk during repositioning of patients in bed: The influence of handling technique, patient weight, and disability. Ergonomics 2008, 51, 1042–1052. [Google Scholar] [PubMed]










| Variable | Mobility Device User | Caregivers/Rehabilitation Professionals |
|---|---|---|
| Gender | Female: 3 Male: 15 | Female = 15 Male = 3 |
| Age (years) | 58.33 ± 10.72 (Range = 30–76) | 42.6 ± 16.3 (Range = 25–74) |
| Height (m) | 1.75 ± 0.064 (Range = 1.60–1.84) | 1.67 ± 0.12 (Range = 1.5–1.88) |
| Weight (Kg) | 90.10 ± 26.35 (Range= 49.50–164.70) | 79.57 ± 18.44 (Range = 44.1–112.5) |
| Ethnicity | Caucasian = 13 African American = 3 Mixed = 1 Caribbean = 1 | Caucasian = 11 African American = 2 Asian = 2 Hispanic = 1 Undisclosed = 2 |
| Education Level | Bachelor Degree = 7 Master Degree = 6 High School Diploma or GED = 3 Associate Degree = 1 Vocational/Technical School = 1 | |
| Occupation Level or Type of Caregiver | Retired = 10 Work part-time = 3 Work full-time = 2 Unemployed = 2 Volunteer = 1 | Professional caregivers = 11 Physical therapists = 7 Personal care attendant = 2 Occupational therapist = 1 Nurse = 1 Informal Caregivers = 7 |
| Mobility Device or Experience with mobility devices | Power Wheelchair = 11 Manual Wheelchair = 6 Scooter = 1 | Manual wheelchairs = 17 Powered wheelchairs= 12 Scooter= 6 Recreational (handcycle, racing, quad rugby chairs) = 5 |
| Disability or Disability demographic experience | SCI = 11 Neuromuscular diseases = 5 Cognitive impairment = 2 | Neuromuscular Diseases (e.g., multiple sclerosis; muscular dystrophy, ALS) = 12 Spinal Cord Injury = 9 Cerebrovascular Disease (Stroke) = 8 Cardiovascular Disease = 7 Congenital impairment (e.g., cerebral palsy, spinal bifida) = 7 Cognitive impairment (e.g., traumatic brain injury, Alzheimer’s, and dementia) = 6 Orthopedic impairments = 5 Cardiopulmonary Disease = 4 Osteoarthritis = 3 Rheumatoid arthritis = 3 |
| Number of hours assisting mobility device user (per week) | 1–8 h = 3 8–16 h = 1 16–24 h = 2 24–32 h = 1 32–40 h = 6 40+ h = 5 | |
| Age of people providing care to | Children (<16 years) = 7 Adults (17–65 years) = 15 Seniors (65+ years) = 12 |
| Overall Impressions in Descending Order of Number of Times Reported | # of Participants |
|---|---|
| Great/Impressive/Innovative | 17 |
| Reduces the chance of injury and human error | 8 |
| Easy and Safe | 4 |
| Better than mechanical lifts | 3 |
| Reduces caregiver effort | 3 |
| Helpful in clinical settings | 2 |
| Cumbersome/expensive | 1 |
| Key Features of the PPTS in Descending Order of Number of Times Reported | # of Participants |
|---|---|
| Person repositioning | 12 |
| Transfers and consistency | 6 |
| Secure and easy | 6 |
| Low effort and human-interaction | 2 |
| Easy controls | 2 |
| EPW backrest design | 2 |
| Limitations of the PPTS in Descending Order of Number of Times Reported | # of Participants |
|---|---|
| Chair Limitations | 19 |
| Lack of independent transfers | 10 |
| Leg Orientation to transfer to the chair | 9 |
| Lacks trunk support | 9 |
| Cost/Insurance | 5 |
| Slow speed | 5 |
| Space constraints | 5 |
| Weight limitation | 4 |
| Limitations with user interface | 4 |
| Lacks lateral repositioning | 4 |
| Social stigmas | 3 |
| After-market modifications | 3 |
| Lacks support for prone transfers | 3 |
| Complex/hard maintenance | 3 |
| Needs additional fault detection | 2 |
| Chair looks institutional | 2 |
| Training requirement | 2 |
| Conveyer impediment to comfort | 1 |
| Patient compliance required | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Satpute, S.A.; Candiotti, J.L.; Duvall, J.A.; Kulich, H.; Cooper, R.; Grindle, G.G.; Gebrosky, B.; Brown, J.; Eckstein, I.; Sivakanthan, S.; et al. Participatory Action Design and Engineering of Powered Personal Transfer System for Wheelchair Users: Initial Design and Assessment. Sensors 2023, 23, 5540. https://doi.org/10.3390/s23125540
Satpute SA, Candiotti JL, Duvall JA, Kulich H, Cooper R, Grindle GG, Gebrosky B, Brown J, Eckstein I, Sivakanthan S, et al. Participatory Action Design and Engineering of Powered Personal Transfer System for Wheelchair Users: Initial Design and Assessment. Sensors. 2023; 23(12):5540. https://doi.org/10.3390/s23125540
Chicago/Turabian StyleSatpute, Shantanu A., Jorge Luis Candiotti, Jonathan A. Duvall, Hailee Kulich, Rosemarie Cooper, Garrett G. Grindle, Benjamin Gebrosky, Josh Brown, Ian Eckstein, Sivashankar Sivakanthan, and et al. 2023. "Participatory Action Design and Engineering of Powered Personal Transfer System for Wheelchair Users: Initial Design and Assessment" Sensors 23, no. 12: 5540. https://doi.org/10.3390/s23125540
APA StyleSatpute, S. A., Candiotti, J. L., Duvall, J. A., Kulich, H., Cooper, R., Grindle, G. G., Gebrosky, B., Brown, J., Eckstein, I., Sivakanthan, S., Deepak, N., Kanode, J., & Cooper, R. A. (2023). Participatory Action Design and Engineering of Powered Personal Transfer System for Wheelchair Users: Initial Design and Assessment. Sensors, 23(12), 5540. https://doi.org/10.3390/s23125540





