Quantitative Gait Analysis of Patients with Severe Symptomatic Spinal Stenosis Utilizing the Gait Profile Score: An Observational Clinical Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Aims and Hypothesis
2.2. Patient and Control Selection Criteria
2.3. 3D Quantitative Motion Analysis
2.4. Spatiotemporal and Kinematic Gait Parameters
2.5. Statistical Methods
3. Results
3.1. General Information and Demographics
3.2. Spatiotemporal Gait Parameters
3.3. Kinematic Gait Parameters
4. Discussion
4.1. Gait Analysis Technique and Patient Selection
4.2. Interpretation of Kinematic Gait Parameters
4.3. Interpretation of Spatiotemporal Gait Parameters
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Forsth, P.; Olafsson, G.; Carlsson, T.; Frost, A.; Borgstrom, F.; Fritzell, P.; Ohagen, P.; Michaelsson, K.; Sanden, B. A Randomized, Controlled Trial of Fusion Surgery for Lumbar Spinal Stenosis. N. Engl. J. Med. 2016, 374, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Ammendolia, C.; Stuber, K.; Tomkins-Lane, C.; Schneider, M.; Rampersaud, Y.R.; Furlan, A.D.; Kennedy, C.A. What interventions improve walking ability in neurogenic claudication with lumbar spinal stenosis? A systematic review. Eur. Spine J. 2014, 23, 1282–1301. [Google Scholar] [CrossRef]
- Wang, J.; Ullah, S.; Solano, M.A.; Overley, S.C.; Bumpass, D.B.; Mannen, E.M. Changes in kinematics, kinetics, and muscle activity in patients with lumbar spinal stenosis during gait: Systematic review. Spine J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kuwahara, W.; Kurumadani, H.; Tanaka, N.; Nakanishi, K.; Nakamura, H.; Ishii, Y.; Ueda, A.; Deie, M.; Adachi, N.; Sunagawa, T. Correlation between spinal and pelvic movements during gait and aggravation of low back pain by gait loading in lumbar spinal stenosis patients. J. Orthop. Sci. 2019, 24, 207–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashi, H.; Toribatake, Y.; Murakami, H.; Yoneyama, T.; Watanabe, T.; Tsuchiya, H. Gait Analysis Using a Support Vector Machine for Lumbar Spinal Stenosis. Orthopedics 2015, 38, e959–e964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schizas, C.; Theumann, N.; Burn, A.; Tansey, R.; Wardlaw, D.; Smith, F.W.; Kulik, G. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine 2010, 35, 1919–1924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jan, S.v.S. Color Atlas of Skeletal Landmark Definitions: Guidelines for Reproducible Manual and Virtual Palpations; Churchill Livingstone: Edinburgh, UK, 2007. [Google Scholar]
- Cappozzo, A.; Catani, F.; Croce, U.D.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Baker, R.; McGinley, J.L.; Schwartz, M.H.; Beynon, S.; Rozumalski, A.; Graham, H.K.; Tirosh, O. The gait profile score and movement analysis profile. Gait Posture 2009, 30, 265–269. [Google Scholar] [CrossRef]
- Deyo, R.A. Treatment of lumbar spinal stenosis: A balancing act. Spine J. 2010, 10, 625–627. [Google Scholar] [CrossRef]
- Akhtaruzzaman, A.A.S.; Khan, R. Gait Analysis: Systems, technologies and importance. J. Mech. Med. Biol. 2016, 16, 45. [Google Scholar] [CrossRef]
- Chung, P.Y.; Ng, G.Y. Comparison between an accelerometer and a three-dimensional motion analysis system for the detection of movement. Physiotherapy 2012, 98, 256–259. [Google Scholar] [CrossRef] [PubMed]
- White, S.C.; Yack, H.J.; Tucker, C.A.; Lin, H.Y. Comparison of vertical ground reaction forces during overground and treadmill walking. Med. Sci. Sports Exerc. 1998, 30, 1537–1542. [Google Scholar] [CrossRef] [PubMed]
- Papadakis, N.C.; Christakis, D.G.; Tzagarakis, G.N.; Chlouverakis, G.I.; Kampanis, N.A.; Stergiopoulos, K.N.; Katonis, P.G. Gait variability measurements in lumbar spinal stenosis patients: Part A. Comparison with healthy subjects. Physiol. Meas. 2009, 30, 1171–1186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schutte, L.M.; Narayanan, U.; Stout, J.L.; Selber, P.; Gage, J.R.; Schwartz, M.H. An index for quantifying deviations from normal gait. Gait Posture 2000, 11, 25–31. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, M.H.; Rozumalski, A. The Gait Deviation Index: A new comprehensive index of gait pathology. Gait Posture 2008, 28, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Morel, E.; Allali, G.; Laidet, M.; Assal, F.; Lalive, P.H.; Armand, S. Gait Profile Score in multiple sclerosis patients with low disability. Gait Posture 2017, 51, 169–173. [Google Scholar] [CrossRef]
- Speciali, D.S.; Oliveira, E.M.; Cardoso, J.R.; Correa, J.C.; Baker, R.; Lucareli, P.R. Gait profile score and movement analysis profile in patients with Parkinson’s disease during concurrent cognitive load. Braz. J. Phys. Ther. 2014, 18, 315–322. [Google Scholar] [CrossRef] [Green Version]
- Bigoni, M.; Cimolin, V.; Vismara, L.; Tarantino, A.G.; Clerici, D.; Baudo, S.; Galli, M.; Mauro, A. Relationship between gait profile score and clinical assessments of gait in post-stroke patients. J. Rehabil. Med. 2021, 53, jrm00192. [Google Scholar] [CrossRef]
- Bumann, H.; Nuesch, C.; Loske, S.; Byrnes, S.K.; Kovacs, B.; Janssen, R.; Scharen, S.; Mundermann, A.; Netzer, C. Severity of degenerative lumbar spinal stenosis affects pelvic rigidity during walking. Spine J. 2020, 20, 112–120. [Google Scholar] [CrossRef] [Green Version]
- Zhou, J.; Ning, X.; Fathallah, F. Differences in lumbopelvic rhythm between trunk flexion and extension. Clin. Biomech. 2016, 32, 274–279. [Google Scholar] [CrossRef]
- Inufusa, A.; An, H.S.; Lim, T.H.; Hasegawa, T.; Haughton, V.M.; Nowicki, B.H. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine 1996, 21, 2412–2420. [Google Scholar] [CrossRef] [PubMed]
- Yokogawa, N.; Toribatake, Y.; Murakami, H.; Hayashi, H.; Yoneyama, T.; Watanabe, T.; Tsuchiya, H. Differences in Gait Characteristics of Patients with Lumbar Spinal Canal Stenosis (L4 Radiculopathy) and Those with Osteoarthritis of the Hip. PLoS ONE 2015, 10, e0124745. [Google Scholar] [CrossRef] [PubMed]
- Neumann, D.A. Kinesiology of the Musculoskeletal System, 3rd ed.; Mosby: Maryland Heights, MO, USA, 2017; p. 784. [Google Scholar]
- Kreiner, D.S.; Shaffer, W.O.; Baisden, J.L.; Gilbert, T.J.; Summers, J.T.; Toton, J.F.; Hwang, S.W.; Mendel, R.C.; Reitman, C.A.; North American Spine, S. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013, 13, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; Cho, H.; Park, Y.; Jang, J.; Kim, J.W.; Ryu, J.S. Biomechanical influences of gait patterns on knee joint: Kinematic & EMG analysis. PLoS ONE 2020, 15, e0233593. [Google Scholar] [CrossRef]
- Lodin, J.; Jelinek, M.; Prochazka, J.; Sames, M.; Vachata, P. Quantitative gait analysis of patients with severe sacroiliac joint dysfunction: A prospective clinical study. J. Neurosurg. Sci. 2021. [Google Scholar] [CrossRef]
- Loske, S.; Nuesch, C.; Byrnes, K.S.; Fiebig, O.; Scharen, S.; Mundermann, A.; Netzer, C. Decompression surgery improves gait quality in patients with symptomatic lumbar spinal stenosis. Spine J. 2018, 18, 2195–2204. [Google Scholar] [CrossRef]
- Sun, J.; Liu, Y.C.; Yan, S.H.; Wang, S.S.; Lester, D.K.; Zeng, J.Z.; Miao, J.; Zhang, K. Clinical Gait Evaluation of Patients with Lumbar Spine Stenosis. Orthop. Surg. 2018, 10, 32–39. [Google Scholar] [CrossRef]
- Fujita, N.; Sakurai, A.; Miyamoto, A.; Michikawa, T.; Otaka, Y.; Suzuki, S.; Tsuji, O.; Nagoshi, N.; Okada, E.; Yagi, M.; et al. Stride length of elderly patients with lumbar spinal stenosis: Multi-center study using the Two-Step test. J. Orthop. Sci. 2019, 24, 787–792. [Google Scholar] [CrossRef]
- Suda, Y.; Saitou, M.; Shibasaki, K.; Yamazaki, N.; Chiba, K.; Toyama, Y. Gait analysis of patients with neurogenic intermittent claudication. Spine 2002, 27, 2509–2513. [Google Scholar] [CrossRef]
- Perring, J.; Mobbs, R.; Betteridge, C. Analysis of Patterns of Gait Deterioration in Patients with Lumbar Spinal Stenosis. World Neurosurg. 2020, 141, e55–e59. [Google Scholar] [CrossRef]
- Conrad, B.P.; Shokat, M.S.; Abbasi, A.Z.; Vincent, H.K.; Seay, A.; Kennedy, D.J. Associations of self-report measures with gait, range of motion and proprioception in patients with lumbar spinal stenosis. Gait Posture 2013, 38, 987–992. [Google Scholar] [CrossRef] [PubMed]



| Anatomical Position | Marker Count | Bilateral Marker | Marker Discarded for Gait | Anatomical Position | Marker Count | Bilateral Marker | Marker Discarded for Gait |
|---|---|---|---|---|---|---|---|
| Trunk | Lower limb | ||||||
| C7 spinous process | 1 | No | No | Anterior + posterior superior iliac spine | 2 | Yes | No |
| T10 spinous process | 1 | No | No | Midportion of the lateral thigh | 4 (thigh cluster) | Yes | No |
| Upper limb | Medial + lateral femoral epicondyle | 2 | Yes | Yes | |||
| Inferior angle of the scapula | 1 | Yes | No | Proximal portion of the lateral shank | 4 (shank cluster) | Yes | No |
| Acromial edge of the scapula | 1 | Yes | No | Prominence of the medial + lateral malleolus | 2 | Yes | Yes |
| Middle of the humerus body | 1 | Yes | No | Achilles’ tendon insertion | 1 | Yes | No |
| Lateral humeral epicondyle | 1 | Yes | No | Dorsal margin of 1st and 5th metatarsal head | 2 | Yes | No |
| Ulnar + radial styloid process | 2 | Yes | No | Dorsal aspect of 2nd metatarsal head | 1 | Yes | No |
| Parameters | Definition | Controls Mean (SD) | Patients Mean (SD | t-Test/Welch’s Test (p) |
|---|---|---|---|---|
| Stride Length (m) | Distance of the full gait cycle from the heel strike of the reference foot to its successive heel strike | 1.35 (0.08) | 1.00 (0.22) | <0.001 |
| Stride width (m) | Lateral distance between heel centers of two consecutive foot contacts | 0.10 (0.02) | 0.14 (0.04) | 0.004 |
| Step Length side-adjusted (m) | Distance between two successive heel strikes of different feet | 0.68 (0.04) | 0.50 (0.11) | <0.001 |
| Cadence (steps/min) | The number of steps performed per unit of time | 111.2 (3.86) | 98.2 (12.51) | 0.003 |
| Step time (s) | Time of two successive heel strikes of different feet | 0.54 (0.02) | 0.62 (0.09) | 0.004 |
| Stance time side-adjusted (s) | Time during which the reference foot is in contact with the ground (from heel strike to toe-off) | 0.66 (0.03) | 0.85 (0.17) | <0.001 |
| Swing time side-adjusted (s) | Time in which the reference foot is not contact with the ground (from toe-off to heel strike) | 0.42 (0.02) | 0.40 (0.04) | 0.04 |
| Initial double-limb support (s) | Time during which both feet are in contact with the ground in the initial phase of the gait cycle | 0.12 (0.01) | 0.22 (0.08) | <0.001 |
| Parameter | Definition | Controls Mean (SD) | Patients Mean (SD) | t-Test/Welch’s Test (p) |
|---|---|---|---|---|
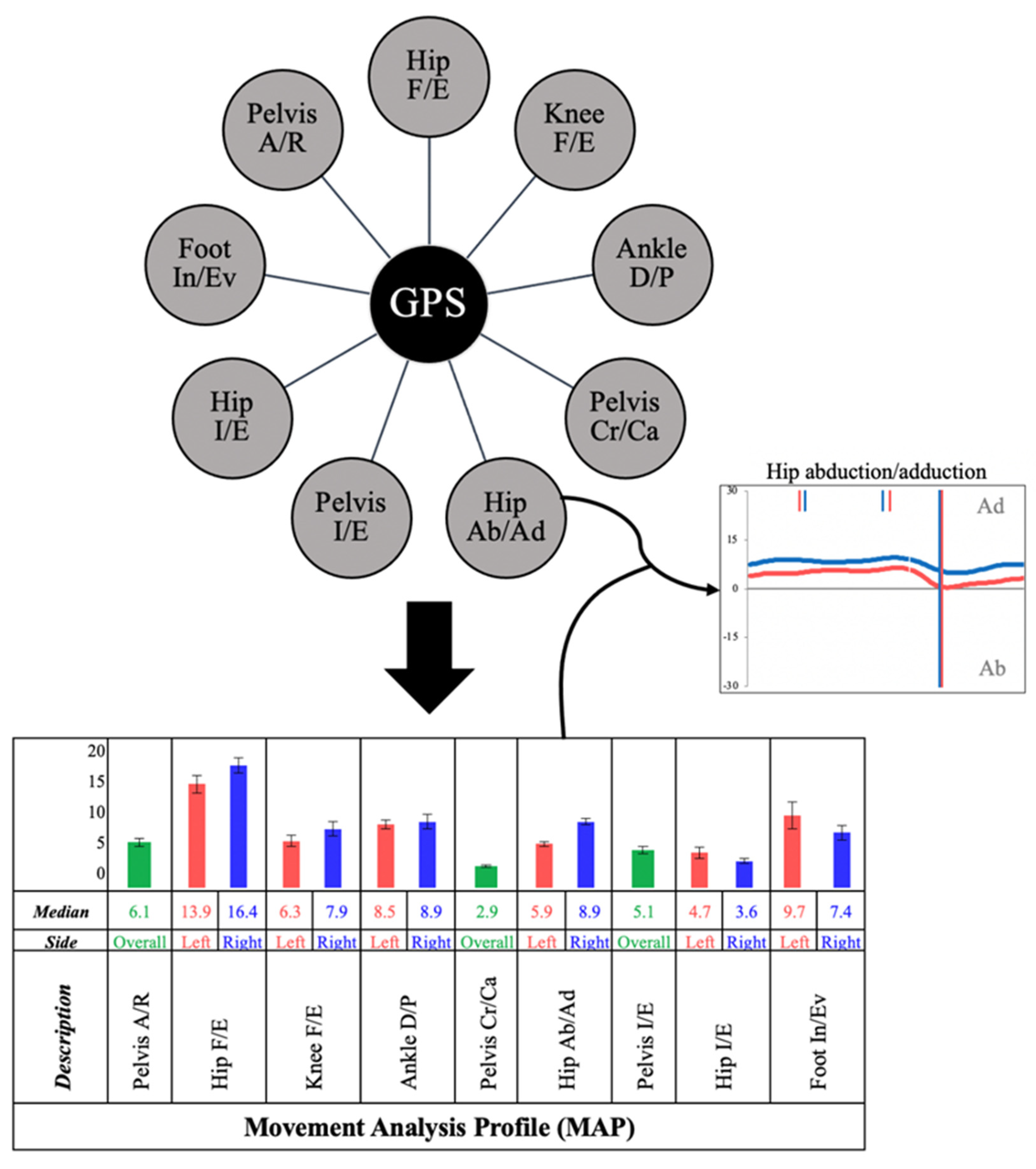
| Gait Profile Score (GPS) | A summarized validated index used to compare a patient’s gait pattern with normative data | 6.44 (1.00) | 8.65 (2.44) | 0.004 |
| Pelvic anteversion/retroversion | Describes pelvic tilting around the femur heads in the sagittal plane | 4.24 (2.55) | 5.41 (3.16) | 0.273 |
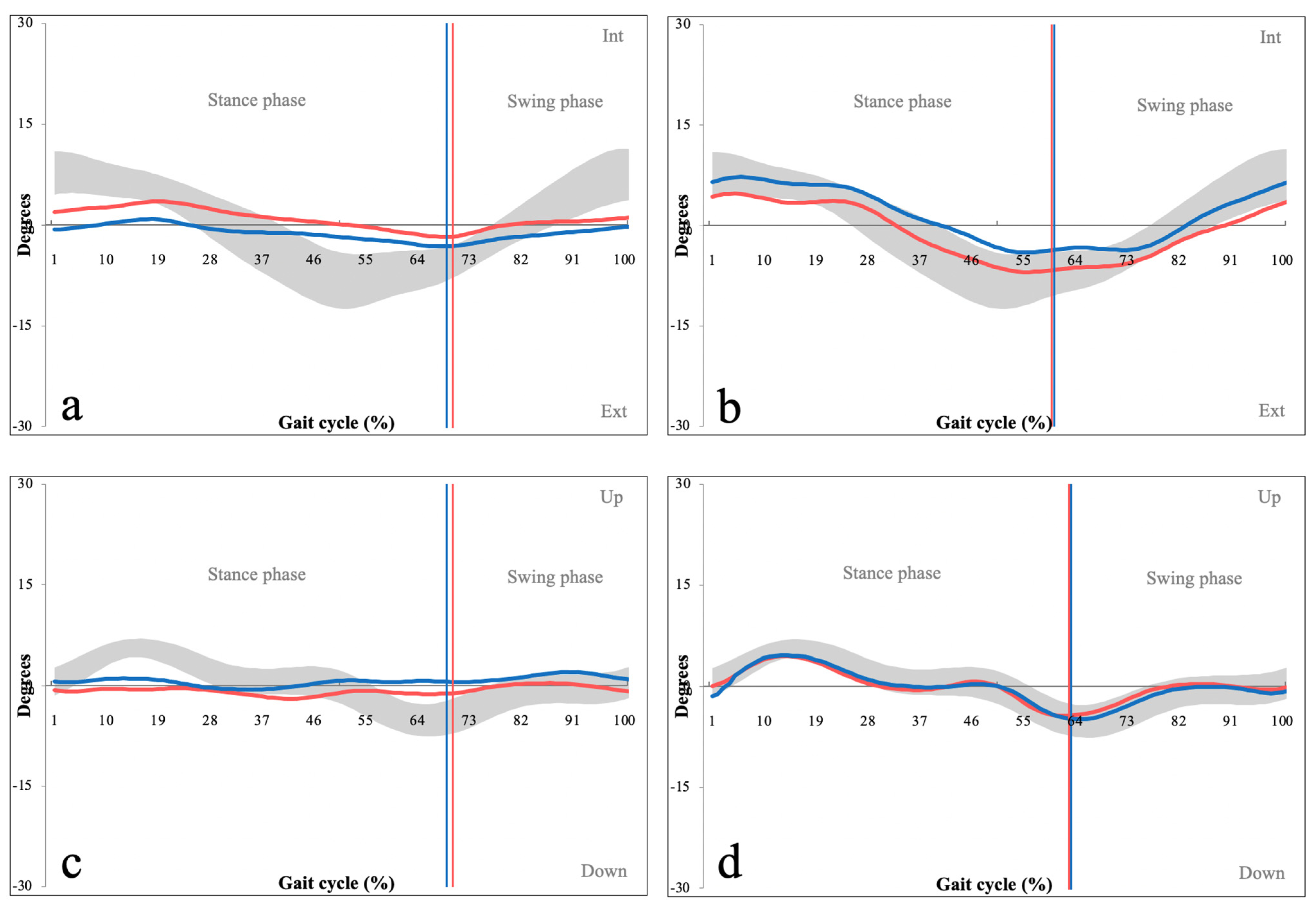
| Pelvic cranial/caudal tilt | Describes cranial/caudal pelvic tilt, measured against a horizonal plotline the frontal plane | 1.82 (0.54) | 3.20 (2.24) | 0.034 |
| Pelvic internal/external rotation | Describes rotational pelvic motion around the lumbar column axis in the axial plane | 3.44 (0.87) | 5.31 (1.41) | <0.001 |
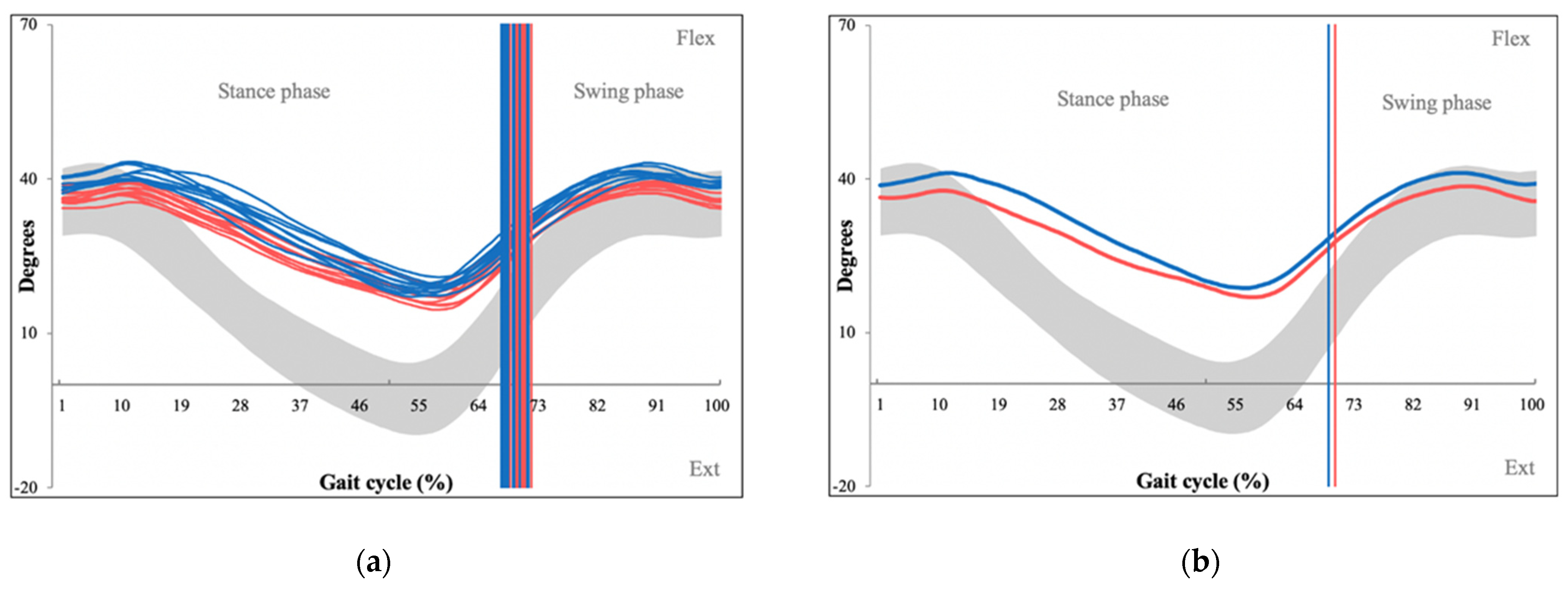
| Hip flexion/extension | Describes flexion/extension of the hip joint in the sagittal plane | 6.22 (2.79) | 11.31 (6.50) | 0.012 |
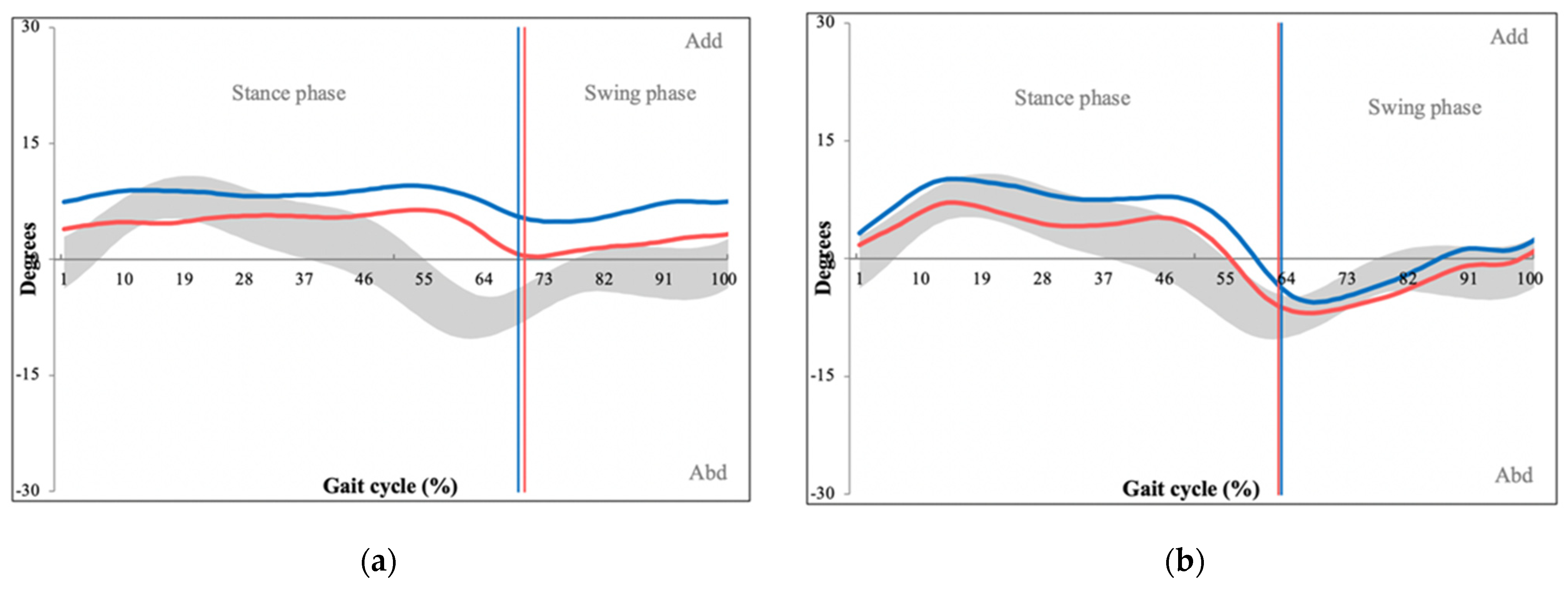
| Hip abduction/adduction | Describes medial/lateral hip movement in the frontal plane | 3.73 (1.19) | 5.73 (2.57) | 0.012 |
| Hip internal/external rotation | Describes rotational hip movement around the femur head in the axial plane | 7.58 (4.17) | 9.49 (4.95) | 0.264 |
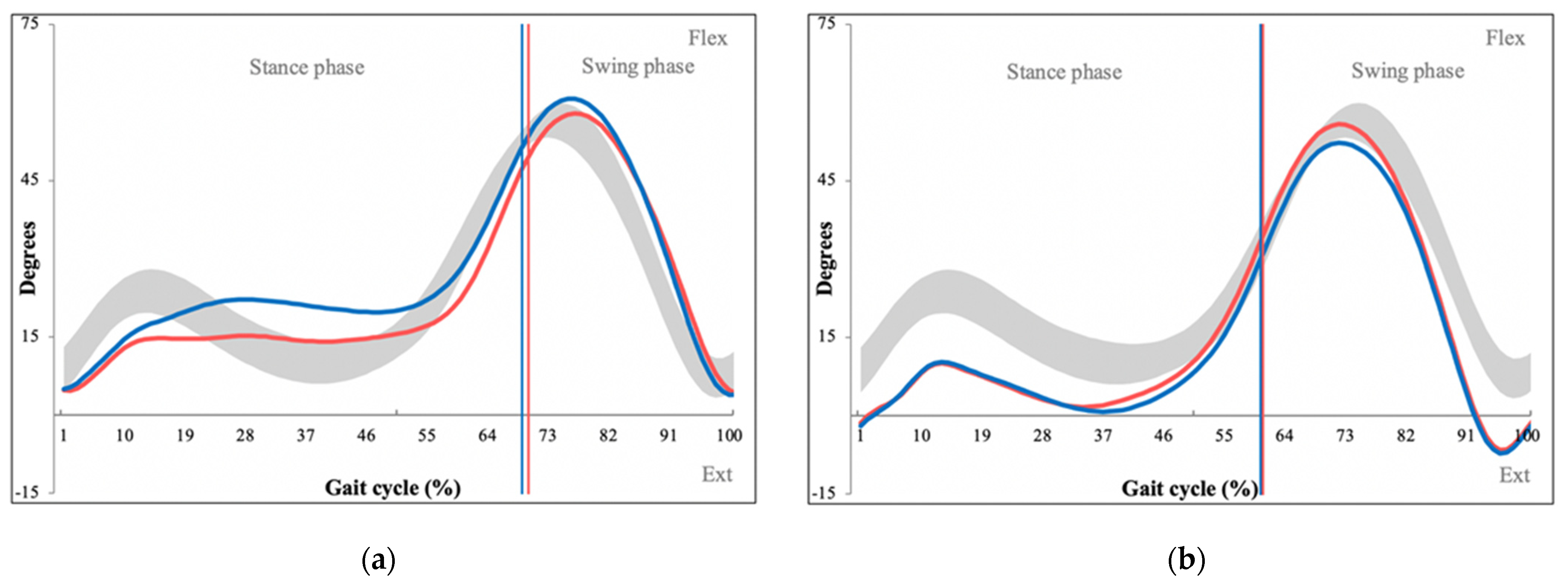
| Knee flexion/extension | Describes flexion/extension of the knee joint in the sagittal plane | 9.74 (2.66) | 8.46 (2.58) | 0.192 |
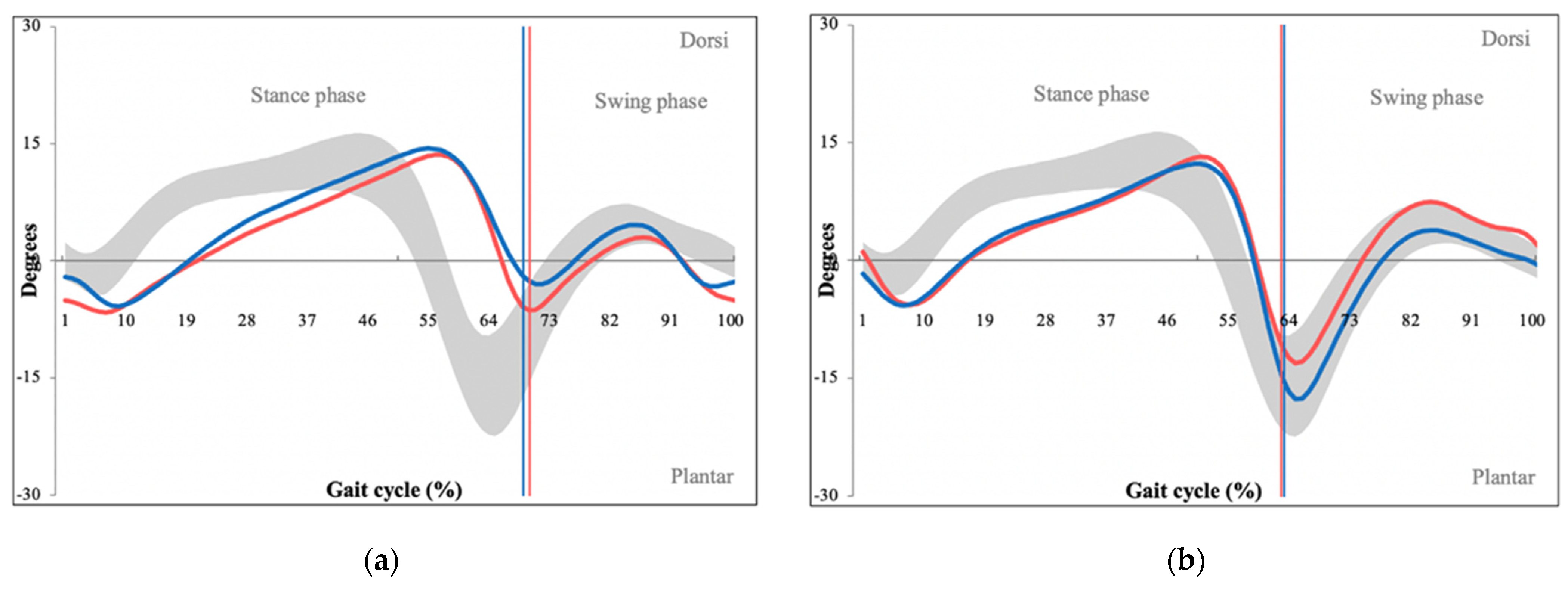
| Ankle dorsal/plantar flexion | Describes flexion/extension of the crural joint in the sagittal plane | 4.80 (1.32) | 8.28 (2.45) | <0.001 |
| Foot inversion/eversion | Describes medial/lateral movement of the foot in the frontal plane | 6.49 (1.89) | 7.20 (2.52) | 0.394 |
| Mean Patient Age (SD) | 62.3 (10.6) | Stenotic Level | |
| Gender (male:female) | 11:4 | L3/4 | 1 |
| Mean Body Mass Index (SD) | 32.0 (5.3) | L4/5 | 5 |
| Mean Oswestry Disability Index (SD) | 52.4 (12.1) | L3–5 | 7 |
| Radicular hypesthesia | 7 (46.7%) | L4-S1 | 2 |
| Claudication interval | Schizas degree of stenosis | ||
| Less than 50 m | 7 | C | 3 |
| 50–200 m | 6 | D | 12 |
| 200–500 m | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lodin, J.; Jelínek, M.; Sameš, M.; Vachata, P. Quantitative Gait Analysis of Patients with Severe Symptomatic Spinal Stenosis Utilizing the Gait Profile Score: An Observational Clinical Study. Sensors 2022, 22, 1633. https://doi.org/10.3390/s22041633
Lodin J, Jelínek M, Sameš M, Vachata P. Quantitative Gait Analysis of Patients with Severe Symptomatic Spinal Stenosis Utilizing the Gait Profile Score: An Observational Clinical Study. Sensors. 2022; 22(4):1633. https://doi.org/10.3390/s22041633
Chicago/Turabian StyleLodin, Jan, Marek Jelínek, Martin Sameš, and Petr Vachata. 2022. "Quantitative Gait Analysis of Patients with Severe Symptomatic Spinal Stenosis Utilizing the Gait Profile Score: An Observational Clinical Study" Sensors 22, no. 4: 1633. https://doi.org/10.3390/s22041633
APA StyleLodin, J., Jelínek, M., Sameš, M., & Vachata, P. (2022). Quantitative Gait Analysis of Patients with Severe Symptomatic Spinal Stenosis Utilizing the Gait Profile Score: An Observational Clinical Study. Sensors, 22(4), 1633. https://doi.org/10.3390/s22041633







