Interactive 3D Force/Torque Parameter Acquisition and Correlation Identification during Primary Trocar Insertion in Laparoscopic Abdominal Surgery: 5 Cases
Abstract
:1. Introduction
2. Related Works
3. Materials and Methods
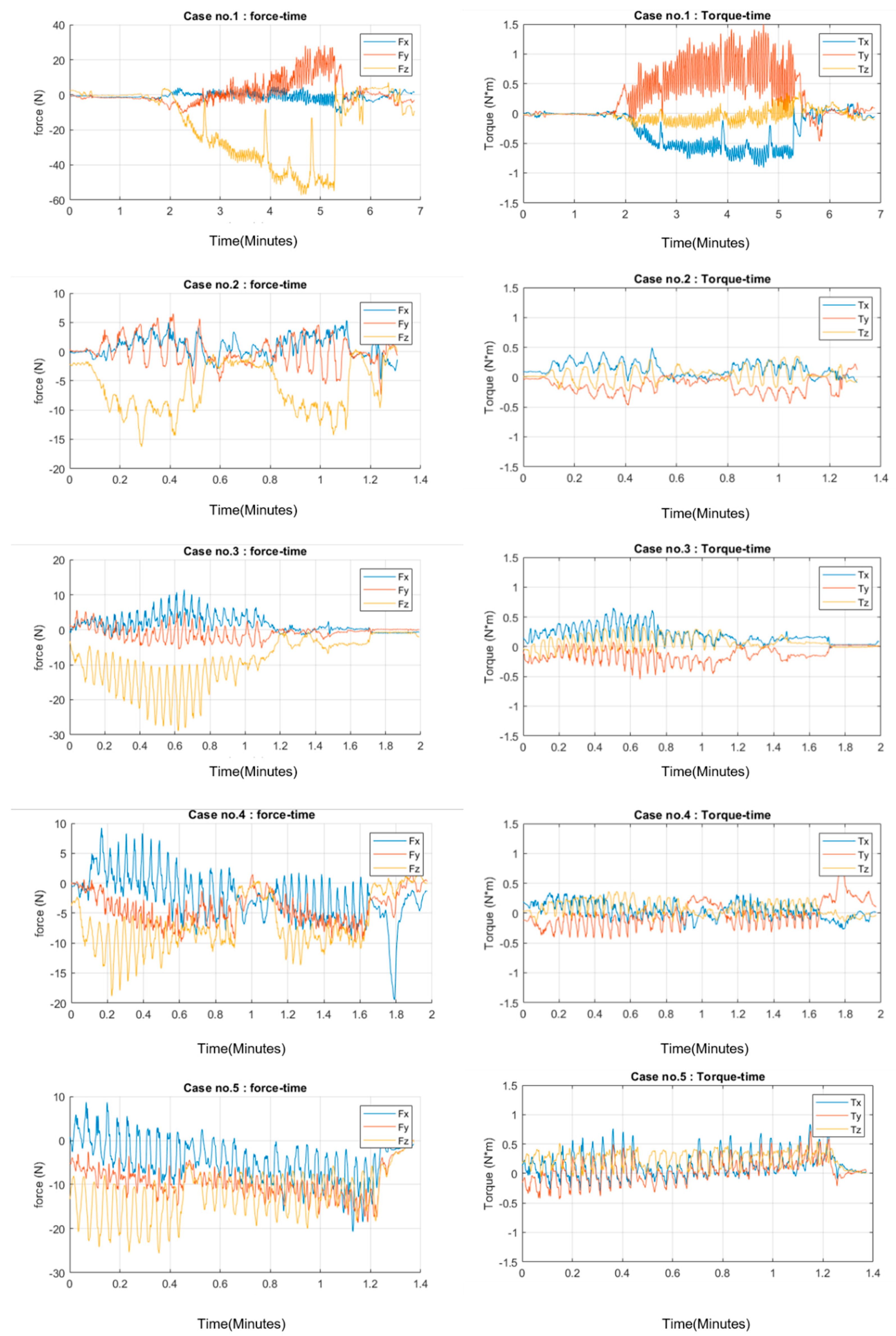
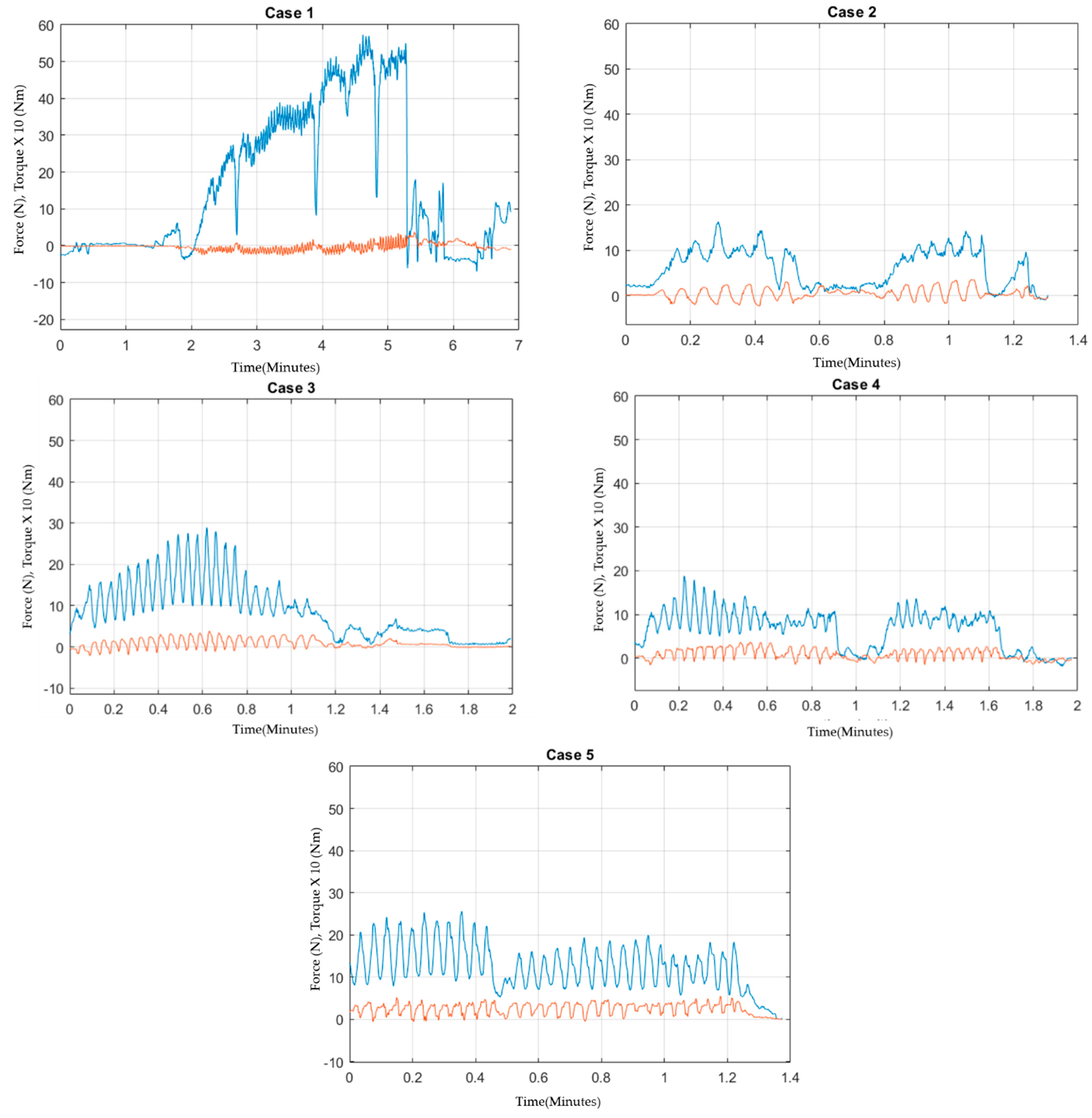
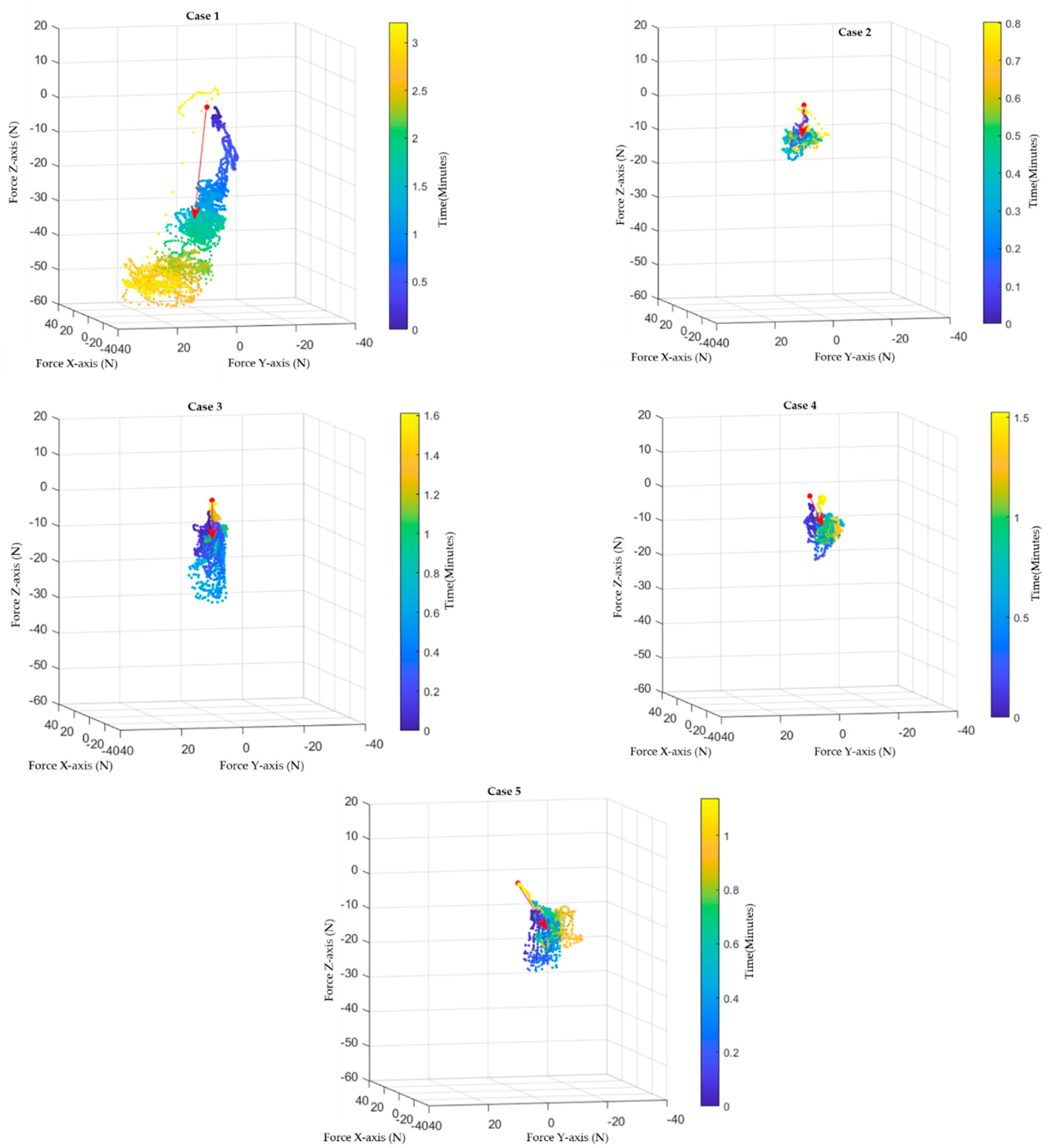
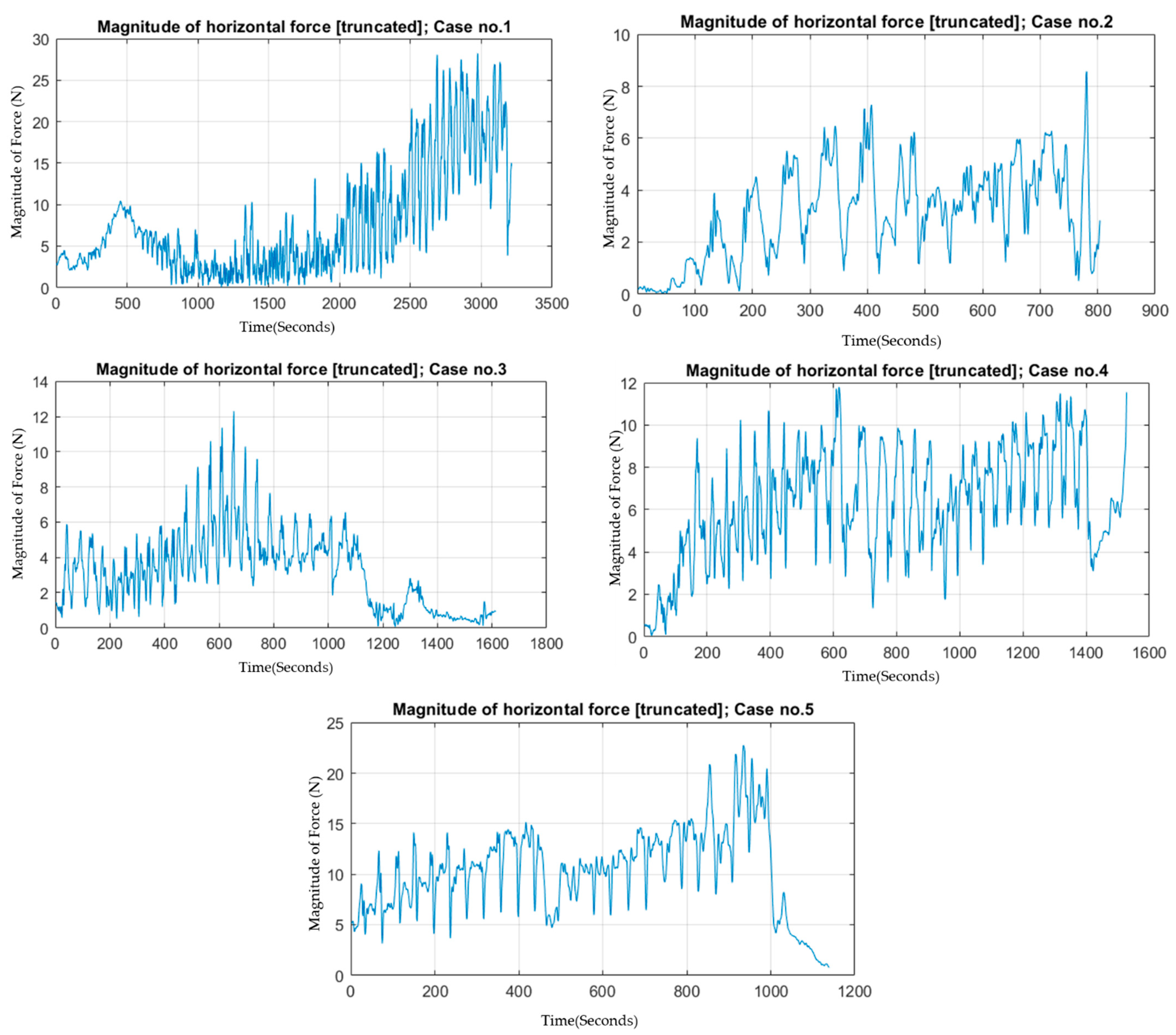
4. Results
Cases Summary
5. Discussion
5.1. Dynamics of Primary Trocar Insertion
5.2. Relationship to Depth of Penetration
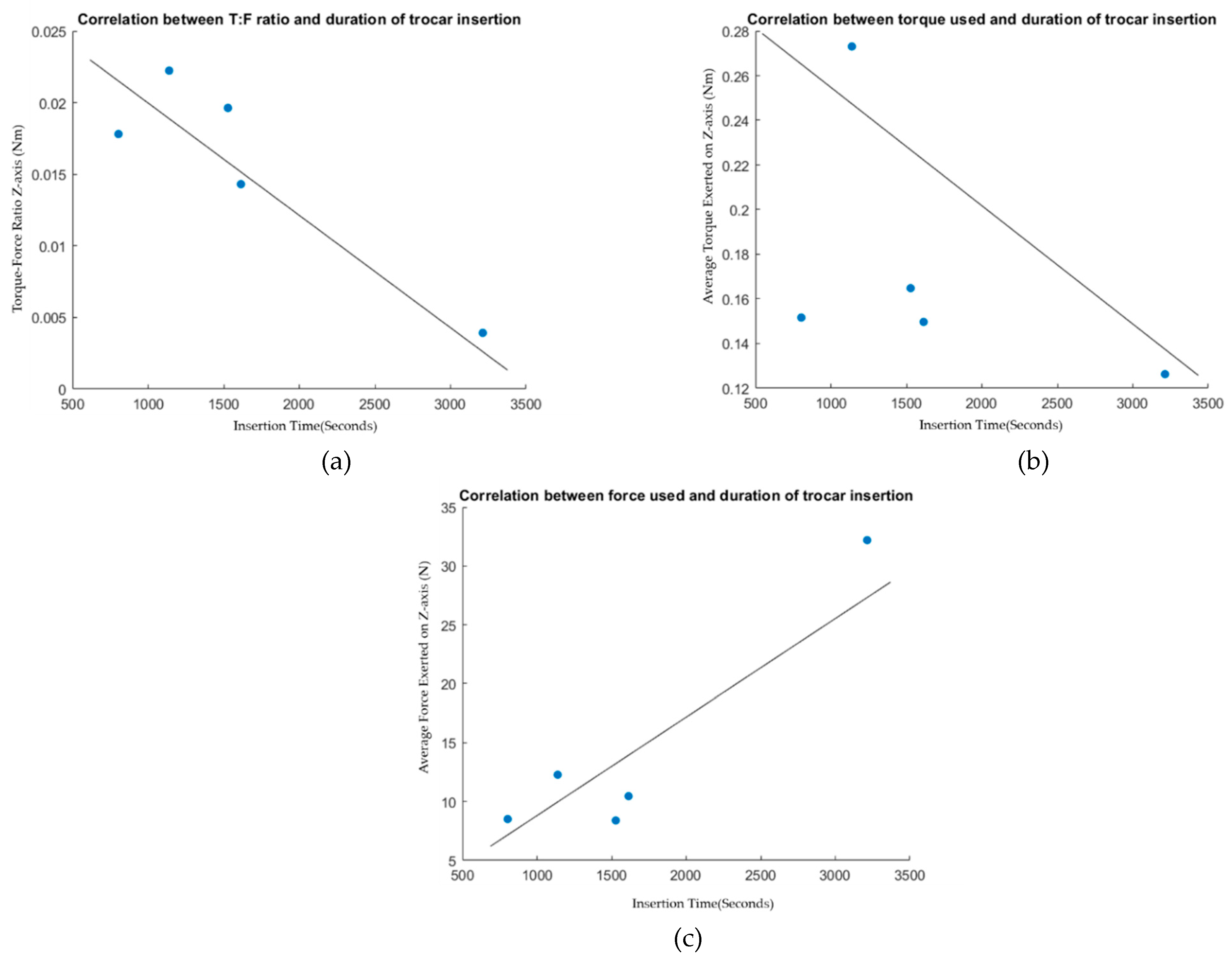
5.3. Correlation Analysis
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Mallat, A.F.; Mancini, M.L.; Daley, B.J.; Enderson, B.L. The role of laparoscopy in trauma: A ten-year review of diagnosis and therapeutics. Am. Surg. 2008, 74, 1166–1170. [Google Scholar] [CrossRef] [PubMed]
- Chavarriaga, A.; Wyrzykowski, A.; Feliciano, D.V. Minimally invasive surgery. Trauma Surg. Acute Care Open 2018, 3, e000290. [Google Scholar] [CrossRef]
- Tsui, C.; Klein, R.; Garabrant, M. Minimally invasive surgery: National trends in adoption and future directions for hospital strategy. Surg. Endosc. 2013, 27, 2253–2257. [Google Scholar] [CrossRef] [PubMed]
- Lajkó, G.; Nagyné Elek, R.; Haidegger, T. Endoscopic Image-Based Skill Assessment in Robot-Assisted Minimally Invasive Surgery. Sensors 2021, 21, 5412. [Google Scholar] [CrossRef] [PubMed]
- Bhoyrul, S.; Vierra, M.A.; Nezhat, C.R.; Krummel, T.M.; Way, L.W. Trocar injuries in laparoscopic surgery. J. Am. Coll. Surg. 2001, 192, 677–683. [Google Scholar] [CrossRef]
- Jang, J.Y.; Han, H.S.; Yoon, Y.S.; Cho, J.Y.; Choi, Y.R. Retrospective comparison of outcomes of laparoscopic and open surgery for T2 gallbladder cancer–Thirteen-year experience. Surg. Oncol. 2019, 29, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Passerotti, C.C.; Begg, N.; Penna, F.J.; Passerotti, A.M.; Leite, K.R.; Antunes, A.A.; Srougi, M.; Retik, A.B.; Nguyen, H.T. Safety profile of trocar and insufflation needle access systems in laparoscopic surgery. J. Am. Coll. Surg. 2009, 209, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Krishnakumar, S.; Tambe, P. Entry complications in laparoscopic surgery. J. Gynecol. Endosc. Surg. 2009, 1, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Lane, T. A Short History of Robotic Surgery. Ann. R. Coll. Surg. Engl. 2018, 100, 5–7. [Google Scholar] [CrossRef]
- Nagyné Elek, R.; Haidegger, T. Non-Technical Skill Assessment and Mental Load Evaluation in Robot-Assisted Minimally Invasive Surgery. Sensors 2021, 21, 2666. [Google Scholar] [CrossRef]
- Hannaford, B.; Rosen, J.; Friedman, D.W.; King, H.; Roan, P.; Cheng, L.; Glozman, D.; Ma, J.; Kosari, S.N.; White, L. Raven-II: An open platform for surgical robotics research. IEEE Trans. Biomed. Eng. 2012, 60, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Hanly, E.J.; Talamini, M.A. Robotic abdominal surgery. Am. J. Surg. 2004, 188, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Ohnmeiss, D.D.; Lieberman, I.H. Robotic-assisted pedicle screw placement: Lessons learned from the first 102 patients. Eur. Spine J. 2013, 22, 661–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.M.; Huang, Y.J.; Wei, P.L. Outcomes of robotic versus laparoscopic surgery for mid and low rectal cancer after neoadjuvant chemoradiation therapy and the effect of learning curve. Medicine 2017, 96, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Brizuela, G.; Santos-Criado, F.-J.; Sanz-Gobernado, D.; de la Fuente-López, E.; Fraile, J.-C.; Pérez-Turiel, J.; Cisnal, A. Gauze Detection and Segmentation in Minimally Invasive Surgery Video Using Convolutional Neural Networks. Sensors 2022, 22, 5180. [Google Scholar] [CrossRef]
- Buia, A.; Stockhausen, F.; Hanisch, E. Laparoscopic surgery: A qualified systematic review. World J. Methodol. 2015, 5, 238–254. [Google Scholar] [CrossRef] [PubMed]
- Direkwatana, C.; Suthakorn, J.; Wilasrussamee, C. MU-LapaRobot: A Corporative Surgical Robot for Laparoscopic Surgery. Open Biomed. Eng. J. 2020, 14, 43–54. [Google Scholar] [CrossRef]
- Pillai, B.M.; Wilasrusmee, C.; Suthakorn, J. Observer based dynamic control model for bilaterally controlled MU-lapa robot: Surgical tool force limiting. Int. J. Electr. Comput. Eng. 2020, 10, 828–839. [Google Scholar] [CrossRef] [Green Version]
- Nagy, T.D.; Haidegger, T. Performance and Capability Assessment in Surgical Subtask Automation. Sensors 2022, 22, 2501. [Google Scholar] [CrossRef]
- Zhou, X.Y.; Guo, Y.; Shen, M.; Yang, G.Z. Application of artificial intelligence in surgery. Front. Med. 2020, 14, 417–430. [Google Scholar] [CrossRef]
- Wu, J.Y.; Yilmaz, N.; Kazanzides, P.; Tumerdem, U. Estimation of Trocar and Tool Interaction Forces on the da Vinci Research Kit with Two-Step Deep Learning. arXiv 2020, arXiv:2012.01479. [Google Scholar]
- Naerum, E.; Elle, O.J.; Hannaford, B. The effect of interaction force estimation on performance in bilateral teleoperation. IEEE Trans. Haptics 2011, 5, 160–171. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Tadano, K. Force Characteristics of Trocar Insertion Abdomen in Laparoscopic Surgery. In Proceedings of the 3rd World Congress on Electrical Engineering and Computer Systems and Science (EECSS’17), Rome, Italy, 4–6 June 2017; pp. 3–8. [Google Scholar]
- Tarnay, C.M.; Glass, K.B.; Munro, M.G. Entry force and intra-abdominal pressure associated with six laparoscopic trocar-cannula systems: A randomized comparison. Obstet. Gynecol. 1999, 94, 83–88. [Google Scholar] [PubMed]
- Kelty, C.J.; Super, P.A.; Stoddard, C.J. The driving force in trocar insertion: A comparison between disposable and reusable trocars. Surg. Endosc. 2000, 14, 1045–1046. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Guo, Q.; Wang, C.X.; Zhang, S.; Wen, C.B.; Sun, T.; Peng, W.; Chen, J.; Li, W.H. Network differentiation: A computational method of pathogenesis diagnosis in traditional Chinese medicine based on systems science. Artif. Intell. Med. 2021, 118, 102134. [Google Scholar] [CrossRef] [PubMed]
- Van Gerwen, D.J.; Dankelman, J.; van den Dobbelsteen, J.J. Needle–tissue interaction forces–A survey of experimental data. Med. Eng. Phys. 2012, 34, 665–680. [Google Scholar] [CrossRef] [PubMed]
- Won, S.; Choi, S.H.; Lee, N.; Shim, S.H.; Kim, M.K.; Kim, M.-L.; Jung, Y.W.; Yun, B.S.; Seong, S.J. Robotic Single-Site Plus Two-Port Myomectomy versus Conventional Robotic Multi-Port Myomectomy: A Propensity Score Matching Analysis. J. Pers. Med. 2022, 12, 928. [Google Scholar] [CrossRef]
- Noh, J.J.; Kim, M.-S.; Kang, J.-H.; Jung, J.-H.; Chang, C.-S.; Jeon, J.; Kim, T.-J. Comparison of Surgical Outcomes of Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) versus Single-Port Access (SPA) Surgery. J. Pers. Med. 2022, 12, 875. [Google Scholar] [CrossRef]
- Fader, A.N.; Rojas-Espaillat, L.; Ibeanu, O.; Grumbine, F.C.; Escobar, P.F. Laparoendoscopic single-site surgery (LESS) in gynecology: A multi-institutional evaluation. Am. J. Obstet. Gynecol. 2010, 203, 501.e1–501.e6. [Google Scholar] [CrossRef]
- Advincula, A.P.; Song, A.; Burke, W.; Reynolds, R.K. Preliminary experience with robot-assisted laparoscopic myomectomy. J. Am. Assoc. Gynecol. Laparosc. 2004, 11, 511–518. [Google Scholar] [CrossRef]
- Golahmadi, A.K.; Khan, D.Z.; Mylonas, G.P.; Marcus, H.J. Tool-tissue forces in surgery: A systematic review. Ann. Med. Surg. 2021, 65, 102268. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, C.; Chen, Z. The advance of surgical blades in cutting soft biological tissue: A review. Int. J. Adv. Manuf. Technol. 2021, 113, 1817–1832. [Google Scholar] [CrossRef]
- Barrie, J.; Russell, L.; Hood, A.J.; Jayne, D.G.; Neville, A.; Culmer, P.R. An in vivo analysis of safe laparoscopic grasping thresholds for colorectal surgery. Surg. Endosc. 2018, 32, 4244–4250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardon, S.F.; van Kasteren, R.J.; Dankelman, J.; Bonjer, H.J.; Tuynman, J.B.; Horeman, T. The value of force and torque measurements in transanal total mesorectal excision (TaTME). Tech. Coloproctology 2019, 23, 843–852. [Google Scholar] [CrossRef] [Green Version]
- Zemiti, N.; Morel, G.; Ortmaier, T.; Bonnet, N. Mechatronic design of a new robot for force control in minimally invasive surgery. IEEE/ASME Trans. Mechatron. 2007, 12, 143–153. [Google Scholar] [CrossRef]
- Sang, H.; Yun, J.; Monfaredi, R.; Wilson, E.; Fooladi, H.; Cleary, K. External force estimation and implementation in robotically assisted minimally invasive surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2017, 13, e1824. [Google Scholar] [CrossRef]
- Puangmali, P.; Althoefer, K.; Seneviratne, L.D.; Murphy, D.; Dasgupta, P. State-of-the-art in force and tactile sensing for minimally invasive surgery. IEEE Sens. J. 2008, 8, 371–381. [Google Scholar] [CrossRef]
- Abeywardena, S.; Yuan, Q.; Tzemanaki, A.; Psomopoulou, E.; Droukas, L.; Melhuish, C.; Dogramadzi, S. Estimation of tool-tissue forces in robot-assisted minimally invasive surgery using neural networks. Front. Robot. AI 2019, 6, 56. [Google Scholar] [CrossRef] [Green Version]
- Su, H.; Mariani, A.; Ovur, S.E.; Menciassi, A.; Ferrigno, G.; De Momi, E. Toward teaching by demonstration for robot-assisted minimally invasive surgery. IEEE Trans. Autom. Sci. Eng. 2021, 18, 484–494. [Google Scholar] [CrossRef]
- Haidegger, T.; Speidel, S.; Stoyanov, D.; Satava, R.M. Robot-assisted minimally invasive surgery—Surgical robotics in the data age. Proc. IEEE 2022, 110, 835–846. [Google Scholar] [CrossRef]
- Attanasio, A.; Scaglioni, B.; Leonetti, M.; Frangi, A.F.; Cross, W.; Biyani, C.S.; Valdastri, P. Autonomous tissue retraction in robotic assisted minimally invasive surgery–a feasibility study. IEEE Robot. Autom. Lett. 2020, 5, 6528–6535. [Google Scholar] [CrossRef]
- Cheng, Z.; Schwaner, K.L.; Dall’Alba, D.; Fiorini, P.; Savarimuthu, T.R. An electrical bioimpedance scanning system for subsurface tissue detection in robot assisted minimally invasive surgery. IEEE Trans. Biomed. Eng. 2021, 69, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Caccianiga, G.; Mariani, A.; De Momi, E.; Cantarero, G.; Brown, J.D. An evaluation of inanimate and virtual reality training for psychomotor skill development in robot-assisted minimally invasive surgery. IEEE Trans. Med. Robot. Bionics 2020, 2, 118–129. [Google Scholar] [CrossRef]
- Kastritsi, T.; Doulgeri, Z. A controller to impose a RCM for hands-on robotic-assisted minimally invasive surgery. IEEE Trans. Med. Robot. Bionics 2021, 3, 392–401. [Google Scholar] [CrossRef]
- Chua, Z.; Jarc, A.M.; Okamura, A.M. Toward force estimation in robot-assisted surgery using Deep Learning with vision and Robot State. In Proceedings of the IEEE International Conference on Robotics and Automation (ICRA), Xi’an, China, 30 May–5 June 2021; pp. 12335–12341. [Google Scholar]
- Ramot, Y.; Haim-Zada, M.; Domb, A.J.; Nyska, A. Biocompatibility and safety of PLA and its Copolymers. Adv. Drug Deliv. Rev. 2016, 107, 153–162. [Google Scholar] [CrossRef]
- Nillahoot, N.; Patel, S.; Suthakorn, J. A Technique for Mimicking Soft Tissue Manipulation from Experimental Data to a Wave Equation Model for a New Laparoscopic Virtual Reality Training System. Open Biomed. Eng. J. 2021, 15, 16–28. [Google Scholar] [CrossRef]
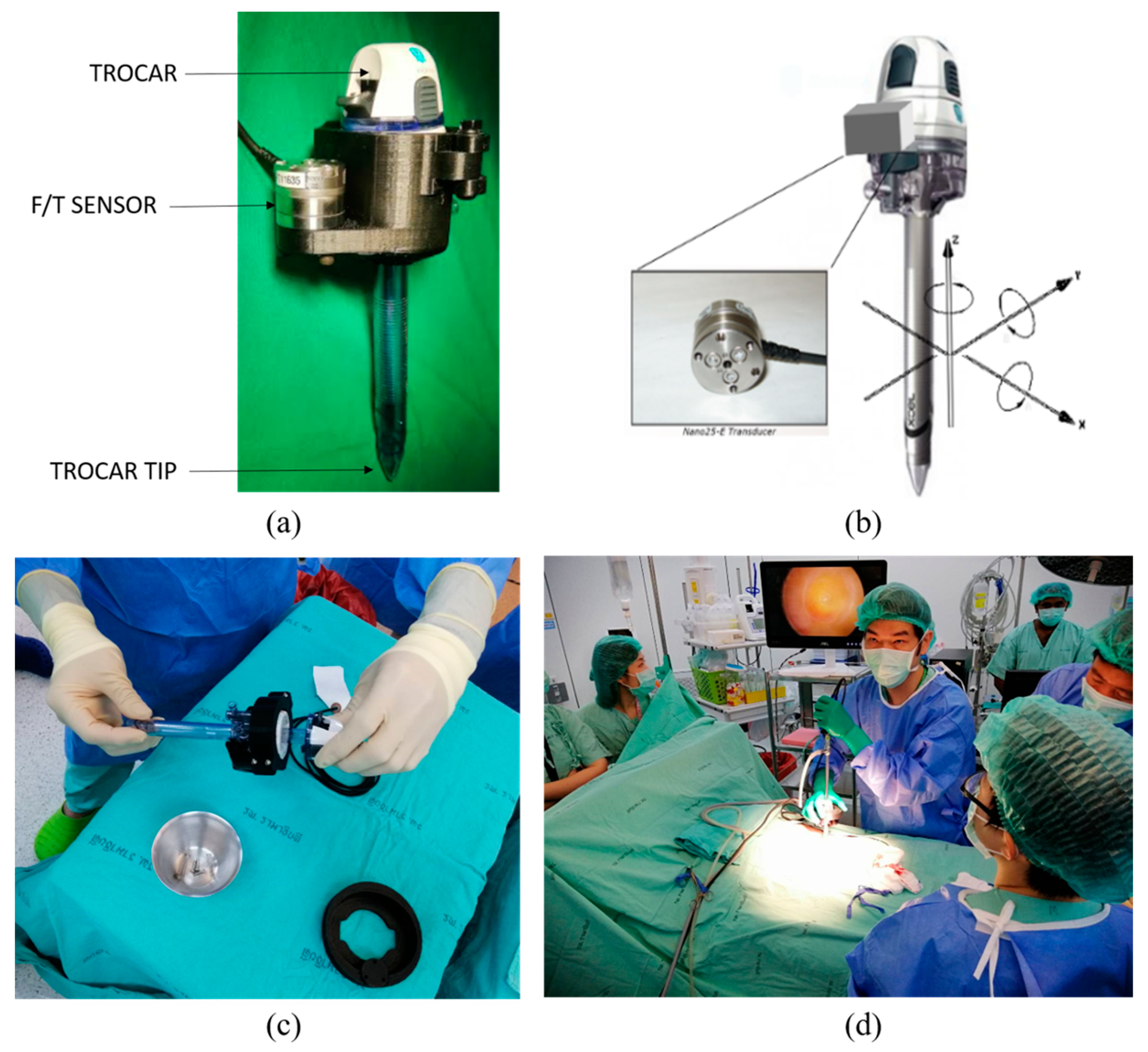

| Surgical Trocar | |
| Model | Ethicon endo surgery system XCEL endopath |
| specification | Size 12 (P92k16) |
| Force/Torque sensor | |
| Model | F/T sensor ATi Nano25 |
| specification | Fx, Fy, Fz, Tx, Ty, Tz; frequency: 1000/s |
| Maximum Fz: 500 N, maximum Tz: 3 NmForce resolution: 1/16 N, torque resolution: 1/2640 Nm | |
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Trocar location | Midline at the base of umbilicus | ||||
| Operation | Abdominal herniation repair | ||||
| Time (unit) With pauses Without pauses Pause time | 4490 3213 1277 | 1273 804 469 | 1714 1614 100 | 1741 1528 213 | 1294 1139 155 |
| Maximum FR (N) | 61.86 | 16.83 | 29.22 | 19.16 | 28.60 |
| Mean FR (N) | 37.22 | 9.78 | 12.75 | 11.27 | 17.47 |
| Maximum TR (Nm) | 1.76 | 0.552 | 0.721 | 0.629 | 1.11 |
| Mean TR (Nm) | 0.923 | 0.348 | 0.359 | 0.284 | 0.410 |
| T/F x-axis (Nm/N) | |||||
| Max (N) | −10.0834 | 5.3399 | 11.4816 | −11.2557 | −18.4729 |
| Mean (N) | −0.3240 | 1.5211 | 2.1746 | −1.7023 | −3.6505 |
| Max (Nm) | −0.9096 | 0.4929 | 0.6544 | 0.3456 | 0.8375 |
| Mean (Nm) | 0.5549 | 0.2158 | 0.2613 | 0.1423 | 0.2375 |
| Ratio (m) | −1.7125 | 0.1419 | 0.1202 | −0.0836 | −0.0651 |
| T/F y-axis (Nm/N) | |||||
| Max (N) | 28.2760 | −7.3552 | 5.6133 | −9.8137 | −18.6518 |
| Mean (N) | 3.8928 | 0.3215 | −0.9310 | −4.9831 | −8.8952 |
| Max (Nm) | 1.5168 | −0.4707 | −0.5462 | 0.6059 | 0.7249 |
| Mean (Nm) | 0.7274 | 0.2271 | 0.1969 | 0.1832 | 0.1930 |
| Ratio (m) | 0.1868 | 0.7062 | −0.2115 | −0.0368 | −0.0217 |
| T/F z-axis (Nm/N) | |||||
| Max (N) | −57.3079 | −16.2875 | −28.9105 | −18.8188 | −25.5875 |
| Mean (N) | −32.1967 | −8.5141 | −10.4603 | −8.3956 | −12.2807 |
| Max (Nm) | 0.3427 | 0.3534 | 0.3793 | 0.3620 | 0.5395 |
| Mean (Nm) | 0.1263 | 0.1516 | 0.1497 | 0.1648 | 0.2731 |
| Ratio (m) | −0.0039 | −0.0178 | −0.0143 | −0.0196 | −0.0222 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nillahoot, N.; Pillai, B.M.; Sharma, B.; Wilasrusmee, C.; Suthakorn, J. Interactive 3D Force/Torque Parameter Acquisition and Correlation Identification during Primary Trocar Insertion in Laparoscopic Abdominal Surgery: 5 Cases. Sensors 2022, 22, 8970. https://doi.org/10.3390/s22228970
Nillahoot N, Pillai BM, Sharma B, Wilasrusmee C, Suthakorn J. Interactive 3D Force/Torque Parameter Acquisition and Correlation Identification during Primary Trocar Insertion in Laparoscopic Abdominal Surgery: 5 Cases. Sensors. 2022; 22(22):8970. https://doi.org/10.3390/s22228970
Chicago/Turabian StyleNillahoot, Nantida, Branesh M. Pillai, Bibhu Sharma, Chumpon Wilasrusmee, and Jackrit Suthakorn. 2022. "Interactive 3D Force/Torque Parameter Acquisition and Correlation Identification during Primary Trocar Insertion in Laparoscopic Abdominal Surgery: 5 Cases" Sensors 22, no. 22: 8970. https://doi.org/10.3390/s22228970
APA StyleNillahoot, N., Pillai, B. M., Sharma, B., Wilasrusmee, C., & Suthakorn, J. (2022). Interactive 3D Force/Torque Parameter Acquisition and Correlation Identification during Primary Trocar Insertion in Laparoscopic Abdominal Surgery: 5 Cases. Sensors, 22(22), 8970. https://doi.org/10.3390/s22228970





