Core Synergies Measured with Ultrasound in Subjects with Chronic Non-Specific Low Back Pain and Healthy Subjects: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Eligibility Criteria
2.3. Sources of Information
2.4. Search Strategy
2.5. Data Selection and Extraction Process
2.6. Outcomes
2.7. Risk of Bias Assessment
3. Results
3.1. Selection of Studies
3.2. Characteristics of the Studies Included
3.3. Outcomes
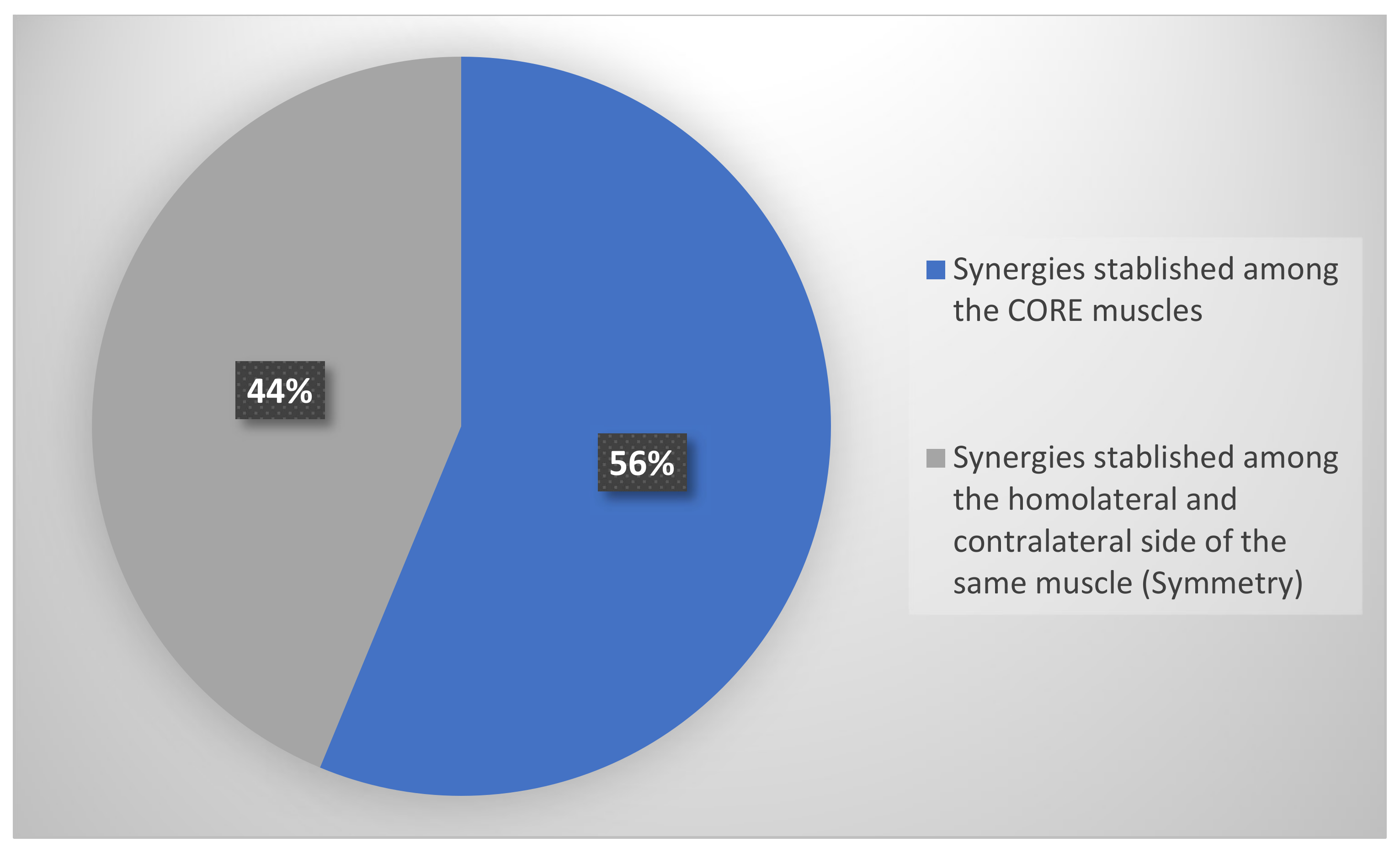
3.3.1. Outcomes: Synergies Established among the Core Muscles Measured with Ultrasound
3.3.2. Synergies Established among the Homolateral and Contralateral Side of the Same Muscle with Ultrasound (Symmetry)
3.4. Results on the Population Studied
3.5. The Quality of the Included Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Miossenet, F.; Rose-Dulcina, K.; Armand, S.; Genevay, S. A systematic review of movement and muscular activity biomarkers to discriminate non-specific chronic low back pain patients from an asymptomatic population. Sci. Rep. 2021, 11, 5850. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.-W.C.; Chenot, J.-F.; van Tulder, M.; Koes, B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef] [PubMed]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Ehsani, F.; Arab, A.M.; Salavati, M.; Jaberzadeh, S.; Hajihasani, A. Ultrasound measurement of abdominal muscle thickness with and without transducer fixation during standing postural tasks in participants with and without chronic low back pain: Intrasession and intersession reliability. PM&R 2016, 8, 1159–1167. [Google Scholar]
- Ramond, A.; Bouton, C.; Richard, I.; Roquelaure, Y.; Baufreton, C.; Legrand, E.; Huez, J.-F. Psychosocial risk factors for chronic low back pain in primary care—A systematic review. Fam. Pract. 2011, 28, 12–21. [Google Scholar] [CrossRef]
- Macedo, L.G.; Saragiotto, B.T.; Yamato, T.P.; Costa, L.O.; Costa, L.C.M.; Ostelo, R.W.; Maher, C.G. Motor control exercise for acute non-specific low back pain. Cochrane Database Syst. Rev. 2016, 2016, CD012085. [Google Scholar] [CrossRef]
- Huxel-Bliven, K.C.; Anderson, B.E. Core Stability Training for Injury Prevention. Sports Health 2013, 5, 514–522. [Google Scholar] [CrossRef]
- Sekendiz, B.; Cuğ, M.; Korkusuz, F. Effects of Swiss-ball core strength training on strength, endurance, flexibility, and balance in sedentary women. J. Strength Cond. Res. 2010, 24, 3032–3040. [Google Scholar] [CrossRef]
- Sapsford, R.R.; Hodges, P.W.; Richardson, C.A.; Cooper, D.H.; Markwell, S.J.; Jull, G.A. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol. Urodyn. 2001, 20, 31–42. [Google Scholar] [CrossRef]
- Broyles, J.M.; Schuenke, M.D.; Patel, S.R.; Vail, C.M.; Broyles, H.V.; Dellon, A.L. Defining the Anatomy of the Tendinous Intersections of the Rectus Abdominis Muscle and Their Clinical Implications in Functional Muscle Neurotization. Ann. Plast. Surg. 2018, 80, 50–53. [Google Scholar] [CrossRef]
- Bordoni, B.; Marelli, F.; Bordoni, G. A review of analgesic and emotive breathing: A multidisciplinary approach. J. Multidiscip. Healthc. 2016, 9, 97–102. [Google Scholar] [CrossRef]
- Fan, C.; Fede, C.; Gaudreault, N.; Porzionato, A.; Macchi, V.; De Caro, R.; Stecco, C. Anatomical and functional relationships between external abdominal oblique muscle and posterior layer of thoracolumbar fascia. Clin. Anat. 2018, 31, 1092–1098. [Google Scholar] [CrossRef]
- Taghipour, M.; Mohseni-Bandpei, M.A.; Behtash, H.; Abdollahi, I.; Rajabzadeh, F.; Pourahmadi, M.R.; Emami, M. Reliability of Real-time Ultrasound Imaging for the Assessment of Trunk Stabilizer Muscles: A Systematic Review of the Literature. J. Ultrasound Med. 2019, 38, 15–26. [Google Scholar] [CrossRef]
- Salvioli, S.; Pozzi, A.; Testa, M. Movement Control Impairment and Low Back Pain: State of the Art of Diagnostic Framing. Medicina 2019, 55, 548. [Google Scholar] [CrossRef]
- Miura, T.; Yamanaka, M.; Ukishiro, K.; Tohyama, H.; Saito, H.; Samukawa, M.; Kobayashi, T.; Ino, T.; Takeda, N. Individuals with chronic low back pain do not modulate the level of transversus abdominis muscle contraction across different postures. Man. Ther. 2014, 19, 534–540. [Google Scholar] [CrossRef]
- Keshwani, N.; McLean, L. Ultrasound Imaging in postpartum women with diastasis recti: Intrarater between-session reliability. J. Orthop. Sports Phys. Ther. 2015, 45, 713–718. [Google Scholar] [CrossRef]
- Kiesel, K.B.; Uhl, T.L.; Underwood, F.B.; Rodd, D.W.; Nitz, A.J. Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man. Ther. 2007, 12, 161–166. [Google Scholar] [CrossRef]
- Hides, J.; Stanton, W.; Mendis, M.D.; Sexton, M. The relationship of transversus abdominis and lumbar multifidus clinical muscle tests in patients with chronic low back pain. Man. Ther. 2011, 16, 573–577. [Google Scholar] [CrossRef]
- Blanchard, T.W.; Smith, C.; Grenier, S.G. In a dynamic lifting task, the relationship between cross-sectional abdominal muscle thickness and the corresponding muscle activity is affected by the combined use of a weightlifting belt and the Valsalva maneuver. J. Electromyogr. Kinesiol. 2016, 28, 99–103. [Google Scholar] [CrossRef]
- Calvo-Lobo, C.; Almazán-Polo, J.; Becerro-De-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Palomo-López, P.; Rodríguez-Sanz, D.; López-López, D. Ultrasonography comparison of diaphragm thickness and excursion between athletes with and without lumbopelvic pain. Phys. Ther. Sport 2019, 37, 128–137. [Google Scholar] [CrossRef]
- Thompson, J.A.; O’Sullivan, P.B.; Briffa, N.K.; Neumann, P. Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional maneouvres in continent and incontinent women. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2007, 18, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 10, 1–11. [Google Scholar]
- Santos, W.M.D.; Secoli, S.R.; Püschel, V.A.D.A. The Joanna Briggs Institute approach for systematic reviews. Rev. Lat. Am. Enferm. 2018, 26, e3074. [Google Scholar] [CrossRef] [PubMed]
- Institute of Health Economics (IHE). Quality Appraisal of Case Series Studies Checklist; Institute of Health Economics: Edmonton, AB, Canada, 2014; Available online: http://www.ihe.ca/research-programs/rmd/cssqac/cssqac-about (accessed on 20 September 2022).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Puentedura, E.J.; Buckingham, S.J.; Morton, D.; Montoya, C.; Fernandez-de-las-Penas, C. Immediate changes in resting and contracted thickness of transversus abdominis after dry needling of lumbar multifidus in healthy participants: A randomized controlled crossover trial. J. Manip. Physiol. Ther. 2017, 40, 615–623. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Miltenberger, C.E.; Deiters, H.M.; Del Toro, Y.M.; Pulliam, J.N.; Childs, J.D.; Boyles, R.E.; Flynn, T.W. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J. Orthop. Sports Phys. Ther. 2005, 35, 346–355. [Google Scholar] [CrossRef]
- Dafkou, K.; Kellis, E.; Ellinoudis, A.; Sahinis, C. The effect of additional external resistance on inter-set changes in abdominal muscle thickness during bridging exercise. J. Sports Sci. Med. 2020, 19, 102–111. [Google Scholar]
- Lee, D.Y.; Seo, D.K. A comparison of abdominal muscle thicknesses measured by ultrasonography between the abdominal drawing-in and straight leg raise maneuvers. J. Phys. Ther. Sci. 2012, 24, 929–931. [Google Scholar] [CrossRef][Green Version]
- Mannion, A.F.; Pulkovski, N.; Toma, V.; Sprott, H. Abdominal muscle size and symmetry at rest and during abdominal hollowing exercises in healthy control subjects. J. Anat. 2008, 213, 173–182. [Google Scholar] [CrossRef]
- Rankin, G.; Stokes, M.; Newham, D.J. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve 2006, 34, 320–326. [Google Scholar] [CrossRef]
- Seo, D.K.; Kim, J.S.; Lee, D.Y.; Kwon, O.S.; Lee, S.S.; Kim, J.H. The relationship of abdominal muscles balance and body balance. J. Phys. Ther. Sci. 2013, 25, 765–767. [Google Scholar] [CrossRef][Green Version]
- Tahan, N.; Khademi-Kalantari, K.; Mohseni-Bandpei, M.A.; Mikaili, S.; Baghban, A.A.; Jaberzadeh, S. Measurement of superficial and deep abdominal muscle thickness: An ultrasonography study. J. Physiol. Anthropol. 2016, 35, 1–5. [Google Scholar] [CrossRef]
- Westad, C.; Mork, P.J.; Vasseljen, O. Location and sequence of muscle onset in deep abdominal muscles measured by different modes of ultrasound imaging. J. Electromyogr. Kinesiol. 2010, 20, 994–999. [Google Scholar] [CrossRef]
- Yoon, B.; Pyeon, H.; Kim, Y.; Hong, Y.; Lee, S. The relation between abdominal muscle asymmetry and trunk postural stability: An ultrasound imaging study. J. Back Musculoskelet. Rehabil. 2018, 31, 1151–1157. [Google Scholar] [CrossRef]
- Bialy, M.; Adamczyk, W.M.; Marczykowski, P.; Majchrzak, R.; Gnat, R. Deformations of abdominal muscles under experimentally induced low back pain. Eur. Spine J. 2019, 28, 2444–2451. [Google Scholar] [CrossRef]
- Hides, J.A.; Belavy, D.L.; Cassar, L.; Williams, M.; Wilson, S.J.; Richardson, C.A. Altered response of the anterolateral abdominal muscles to simulated weight-bearing in subjects with low back pain. Eur. Spine J. 2009, 18, 410–418. [Google Scholar] [CrossRef]
- Hoseinpoor, T.S.; Kahrizi, S.; Mobini, B.; Naji, M.A. Comparison of abdominal muscle thickness changes after a lifting task in subjects with and without chronic low-back pain. Hum. Factors 2015, 57, 208–217. [Google Scholar] [CrossRef]
- ShahAli, S.; Shanbehzadeh, S.; ShahAli, S.; Ebrahimi-Takamjani, I. Application of ultrasonography in the assessment of abdominal and lumbar trunk muscle activity in participants with and without low back pain: A systematic review. J. Manip. Physiol. Ther. 2019, 42, 541–550. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Williamson, J.N.; Carlson, N.H.; Suttles, S.T.; O’Laughlin, S.J.; Whittaker, J.; Goffar, S.L.; Childs, J.D. Ultrasound characteristics of the deep abdominal muscles during the active straight leg raise test. Arch. Phys. Med. Rehabil. 2009, 90, 761–767. [Google Scholar] [CrossRef]
- McGill, S.; Juker, D.; Kropf, P. Appropriately placed surface EMG electrodes reflect deep muscle activity (psoas, quadratus lumborum, abdominal wall) in the lumbar spine. J. Biomech. 1996, 29, 1503–1507. [Google Scholar] [CrossRef]
- Hodges, P.W.; Richardson, C.A. Transversus abdominis and the superficial abdominal muscles are controlled independently in a postural task. Neurosci. Lett. 1999, 265, 91–94. [Google Scholar] [CrossRef]
- Hides, J.; Wilson, S.; Stanton, W.; McMahon, S.; Keto, H.; McMahon, K.; Bryant, M.; Richardson, C. An MRI investigation into the function of the transversus abdominis muscle during “drawing-in” of the abdominal wall. Spine 2006, 31, 175–178. [Google Scholar] [CrossRef] [PubMed]


| Author/Year | Population | Outcome | Core Muscles Synergies |
|---|---|---|---|
| Bialy M, | (n = 42) | Onset | TrA, IO, EO |
| 2019 [36] | Healthy and NSLBP | ||
| Dafkou K, 2020 [28] | (n = 20) | % change thickness | TrA, RA |
| Healthy | |||
| Hoseinpoor TS, | (n = 28) | % change thickness | TrA, IO, EO, LM |
| 2015 [38] | Chronic NSLBP and healthy | ||
| Puentedura EJ, | (n = 47) | % change thickness | TrA, LM |
| 2017 [26] | Healthy | ||
| Rankin G, | (n = 123) | Muscle Pattern | TrA, IO, EO, RA |
| 2006 [31] * | Healthy | ||
| ShahAli S, 2019 [39] | (n = 20) | % change thickness | TrA, IO, EO |
| Chronic NSLBP and healthy (Women) | |||
| Tahan N, 2016 [33] * | (n = 156) | Muscle Pattern | TrA, IO, EO, RA |
| Healthy | |||
| Teyhen DS, 2005 [27] | (n = 30) | Muscle Pattern | TrA, (IO + EO] ** |
| Chronic NSLBP | |||
| Westad C, 2010 [34] | (n = 24) | Onset | TrA, IO, EO |
| Chronic NSLBP |
| Author/ | Population | Outcome | Core Muscles Synergies |
|---|---|---|---|
| Year | |||
| Hides JA, 2009 [37] | (n = 39) | % change thickness | TrA, IO |
| Chronic NSLBP and healthy | |||
| Mannion AF, | (n = 57) | % change thickness | TrA, IO, EO |
| 2008 [30] | Healthy | ||
| Rankin G, | (n = 123) | % change thickness | TrA, IO, EO, RA |
| 2006 [31] ** | Healthy | ||
| Seo D-K, | (n = 41) | % change thickness | TrA, IO, EO |
| 2013 [32] | Healthy | ||
| Tahan N, 2016 [33] ** | (n = 156) | % change thickness | TrA, IO, EO, RA |
| Healthy | |||
| Teyhen DS, 2009 [40] | (n = 30) | % change thickness | TrA, IO |
| Chronic NSLBP and healthy | |||
| Yoon B, 2018 [35] | (n = 18) | % change thickness | TrA, IO, EO |
| Healthy (Men) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cervera-Cano, M.; López-González, L.; Valcárcel-Linares, D.; Fernández-Carnero, S.; Achalandabaso-Ochoa, A.; Andrés-Sanz, V.; Pecos-Martín, D. Core Synergies Measured with Ultrasound in Subjects with Chronic Non-Specific Low Back Pain and Healthy Subjects: A Systematic Review. Sensors 2022, 22, 8684. https://doi.org/10.3390/s22228684
Cervera-Cano M, López-González L, Valcárcel-Linares D, Fernández-Carnero S, Achalandabaso-Ochoa A, Andrés-Sanz V, Pecos-Martín D. Core Synergies Measured with Ultrasound in Subjects with Chronic Non-Specific Low Back Pain and Healthy Subjects: A Systematic Review. Sensors. 2022; 22(22):8684. https://doi.org/10.3390/s22228684
Chicago/Turabian StyleCervera-Cano, Maria, Luis López-González, David Valcárcel-Linares, Samuel Fernández-Carnero, Alexander Achalandabaso-Ochoa, Verónica Andrés-Sanz, and Daniel Pecos-Martín. 2022. "Core Synergies Measured with Ultrasound in Subjects with Chronic Non-Specific Low Back Pain and Healthy Subjects: A Systematic Review" Sensors 22, no. 22: 8684. https://doi.org/10.3390/s22228684
APA StyleCervera-Cano, M., López-González, L., Valcárcel-Linares, D., Fernández-Carnero, S., Achalandabaso-Ochoa, A., Andrés-Sanz, V., & Pecos-Martín, D. (2022). Core Synergies Measured with Ultrasound in Subjects with Chronic Non-Specific Low Back Pain and Healthy Subjects: A Systematic Review. Sensors, 22(22), 8684. https://doi.org/10.3390/s22228684









