New Internet of Medical Things for Home-Based Treatment of Anorectal Disorders
Abstract
:1. Introduction
- (1)
- Rising medical costs: The high cost of equipment and technical staff required to deliver BF makes it difficult to establish clinics in regional and community hospitals.
- (2)
- Time consuming: Average BF therapy involves the 6 weekly sessions and follow-up sessions after 6 and 12 months. Despite demand, clinics are limited by the number of patients they can treatment at one time.
- (3)
- Adherence: Difficulties accessing BF and the relatively invasive nature of the procedure means fewer than 30% of patients are able to adhere and complete their prescribed treatment.
- Designing a new IoMT for home-based treatment of anorectal disorders using a user-centric approach.
- Development and implementation of hardware and software components of the proposed IoMT including a new sensor in a modular architecture.
- Evaluation of the proposed IoMT in terms of accuracy and consistency in a real working condition.
2. Related Work
- (1)
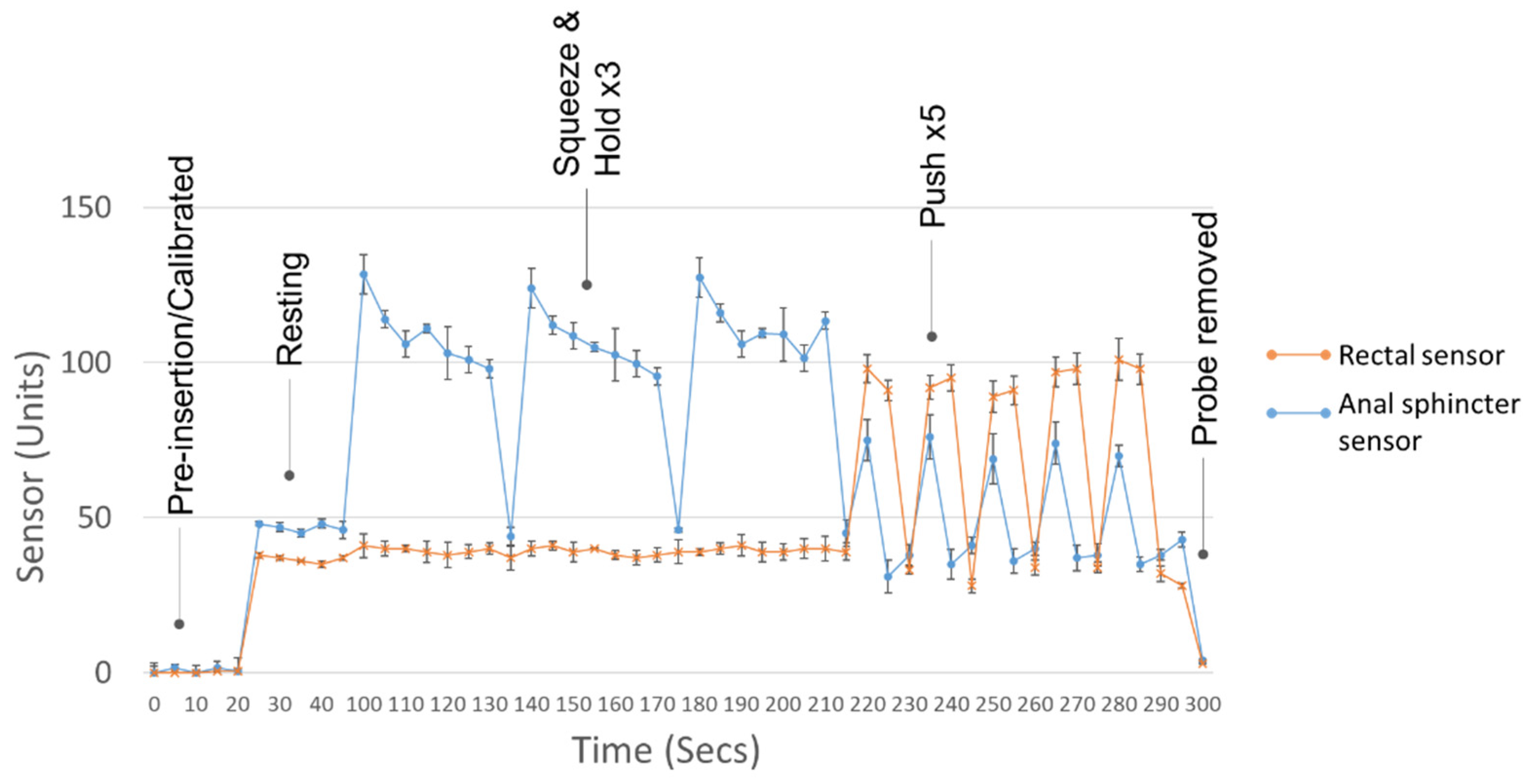
- Rest: After probe placement, a period of time is given for the patient to relax, so that the anal sphincter tone returns to basal levels. Anal resting pressure is measured using the averaged resting pressure over the length of the anal canal over a period of 20 s. This pressure is a composition of the internal and external anal sphincter and, to a lesser extent, the hemorrhoidal plexus.
- (2)
- Squeeze and hold: The patient is asked to squeeze the anus for as long as possible, for a maximum of 30 s. By convention, this manoeuvre is performed three times. Both the maximal contractile pressure and endurance times are measured. Ideally, rectal pressure should not increase, because that would imply the patient has contracted the abdominal wall.
- (3)
- Simulated defecation (push): The patient bear down as if to defecate and attempt to expel the catheter. This manoeuvre should produce sufficient rectal propulsion pressures with simultaneous anal sphincter relaxation (>20% relaxation).
2.1. Pressure Sensors
2.2. Electromyography
3. System Analysis and Design
4. System Architecture and Implementation
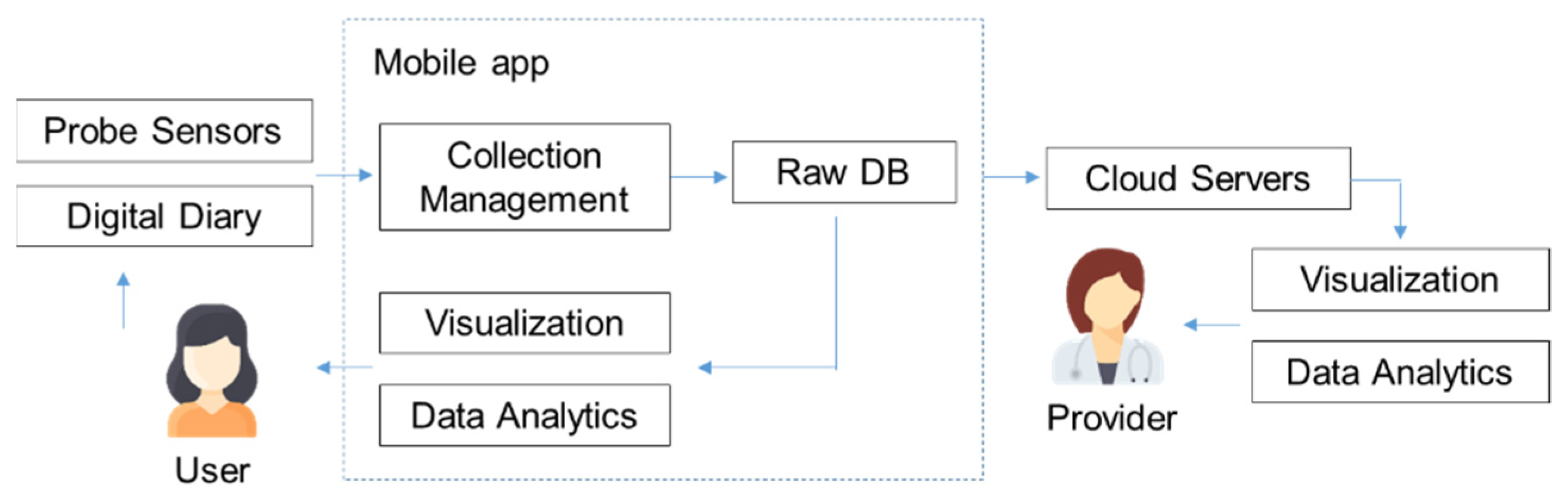
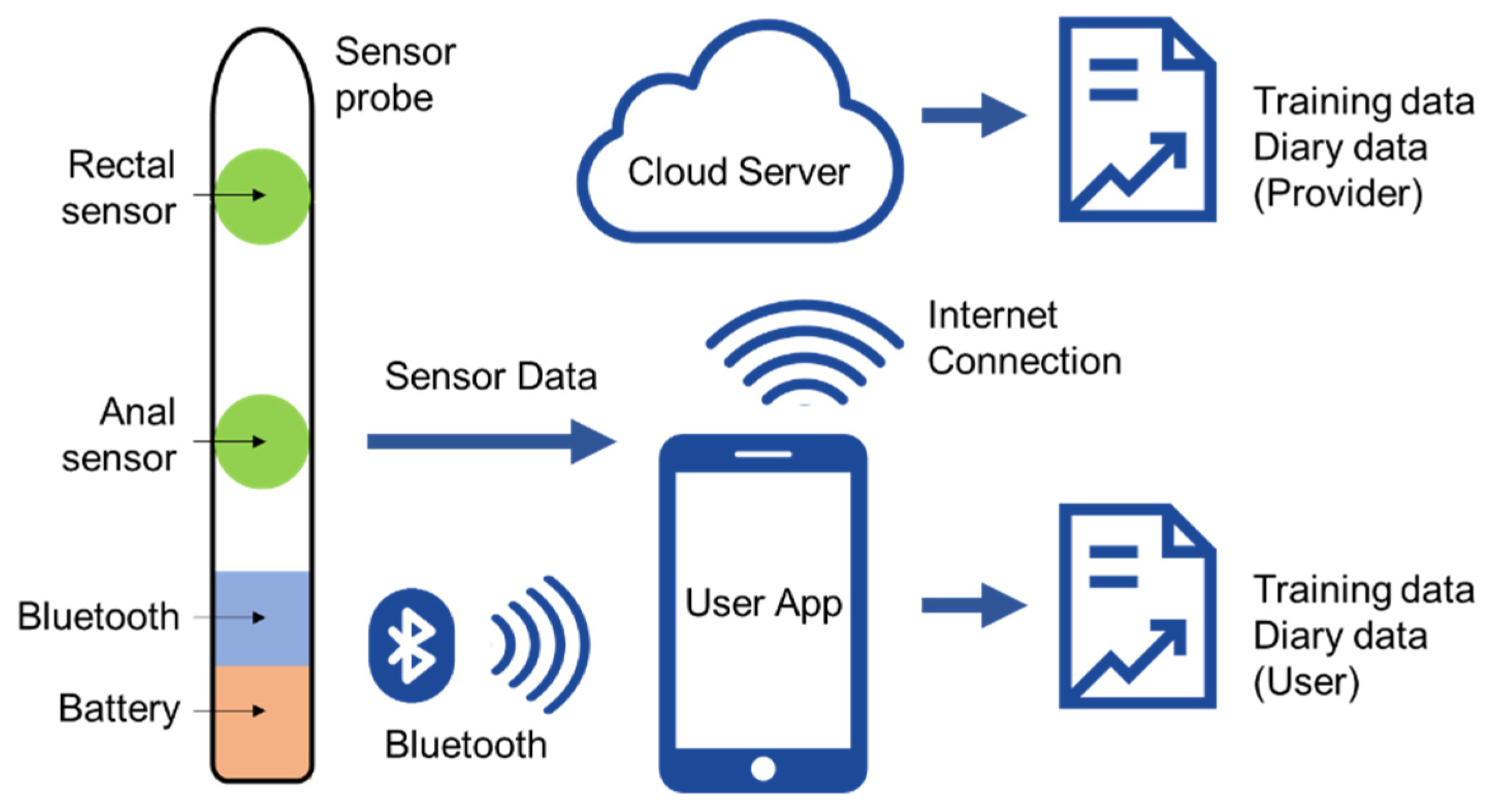
4.1. System Architecture
- (1)
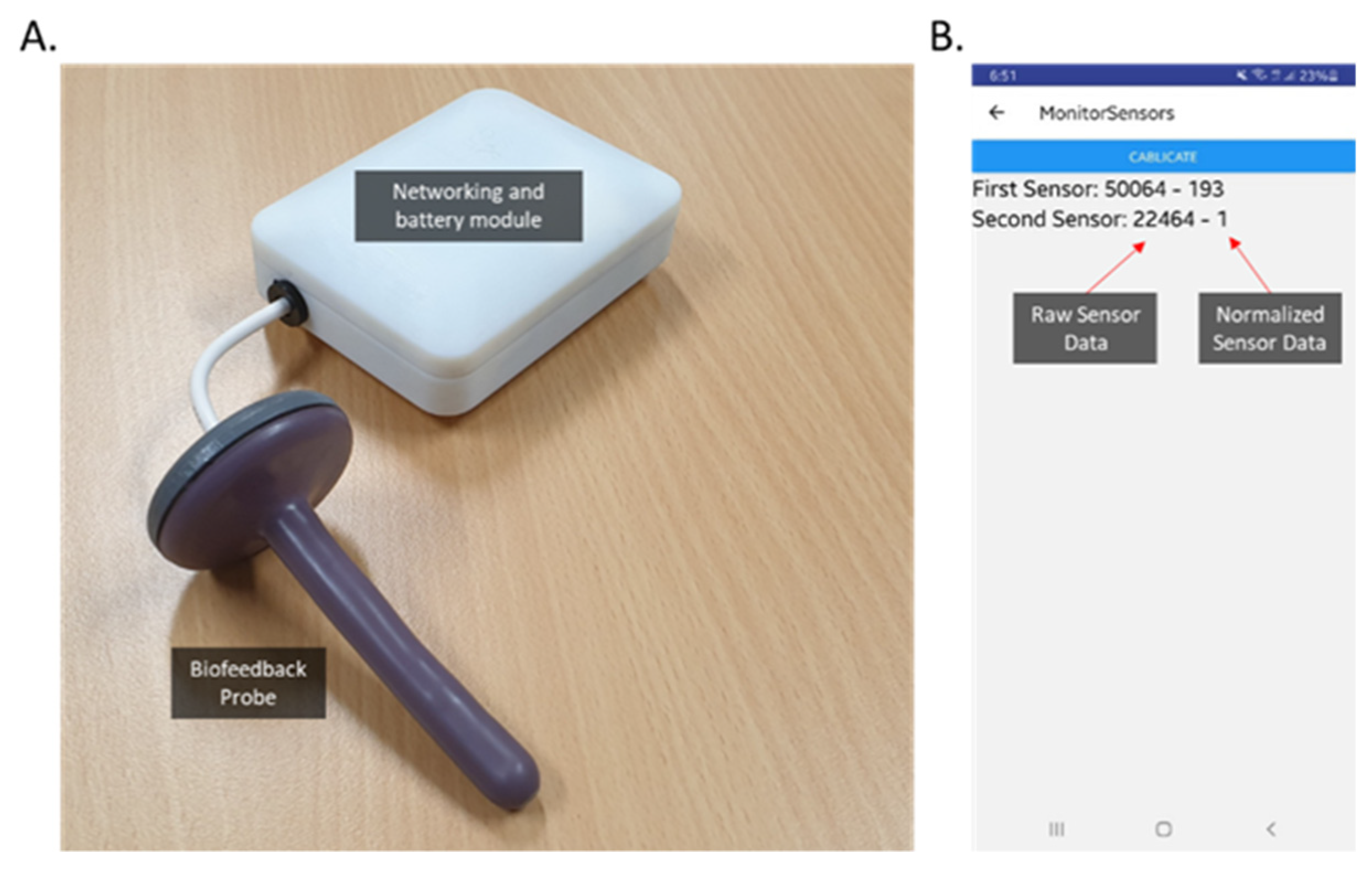
- Sensing layer: Integrates a new sensor array, inserted intra-anally into the patient to collect data from the anorectal muscle activity. The sensors should be small enough to fit within a probe and allow for the measurement of changes in intra-luminal pressures in the rectum and the force applied by the anal sphincter muscles.
- (2)
- Networking layer: Offers networking support and data transfer in the wireless network. We utilized short-range wireless technology (Bluetooth) to transmit our sensor data to a patient’s smart phone app.
- (3)
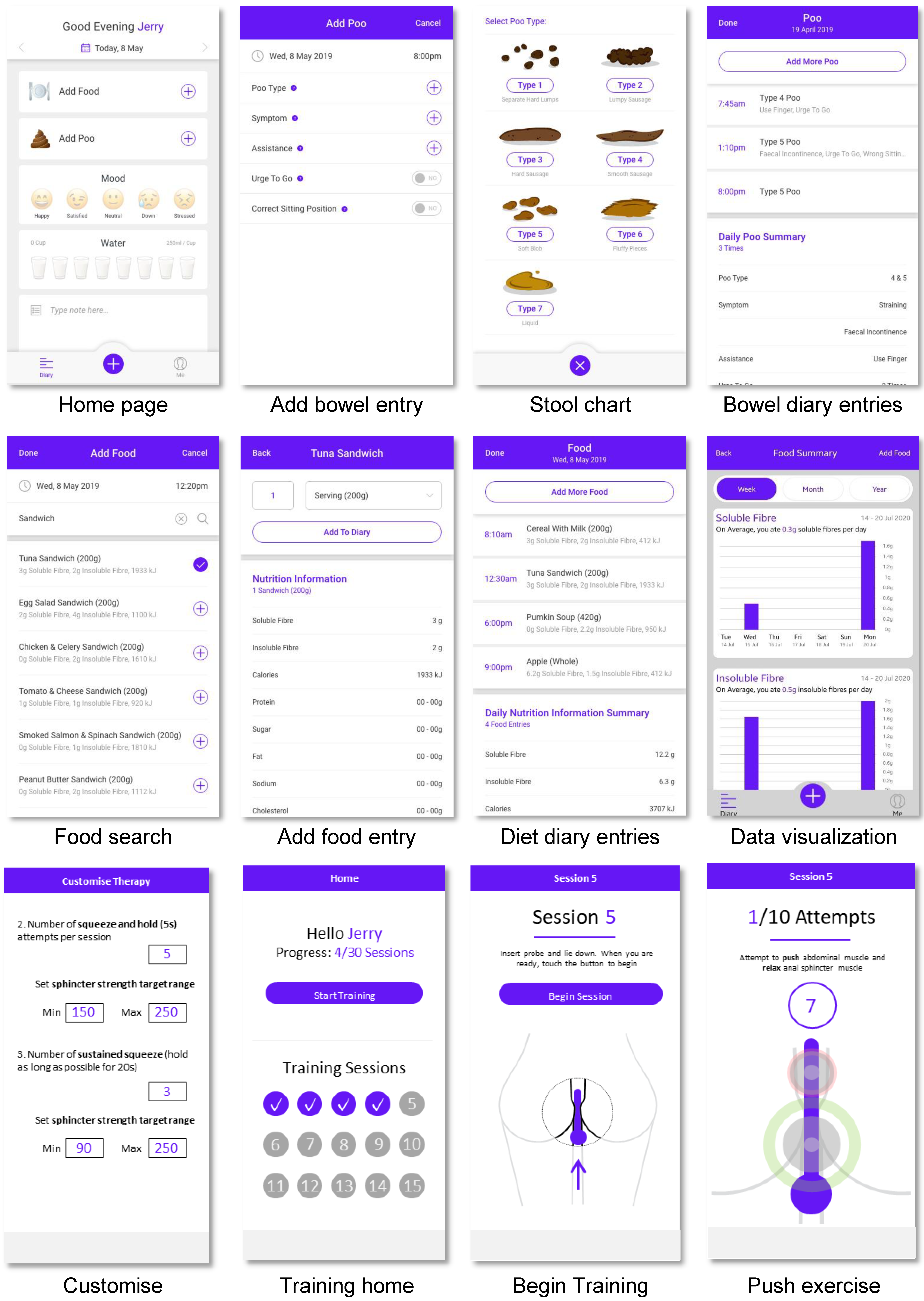
- Service layer: Creates and manages all types of services, aiming to satisfy user requirements. The data collection and processing are tailored to the requirement of the patient’s therapy, such as ensuring correct exercises are performed, adjusting training intensity to be consistent with ability, and comparing current performance with baseline data. Processed data are also synced to the cloud server, allowing data analytics to discover new knowledge to improve the patient care.
- (4)
- Application layer: Provides an easy interface that allows users to retrieve the outputs and to understand the meaning of the outputs. Simple training is provided for understanding graphics and patients can quickly check their progress. Output can also be accessed remotely by their health provider through the cloud-based web application to monitor progress and to aid in decision making.
4.2. Hardware Implementation
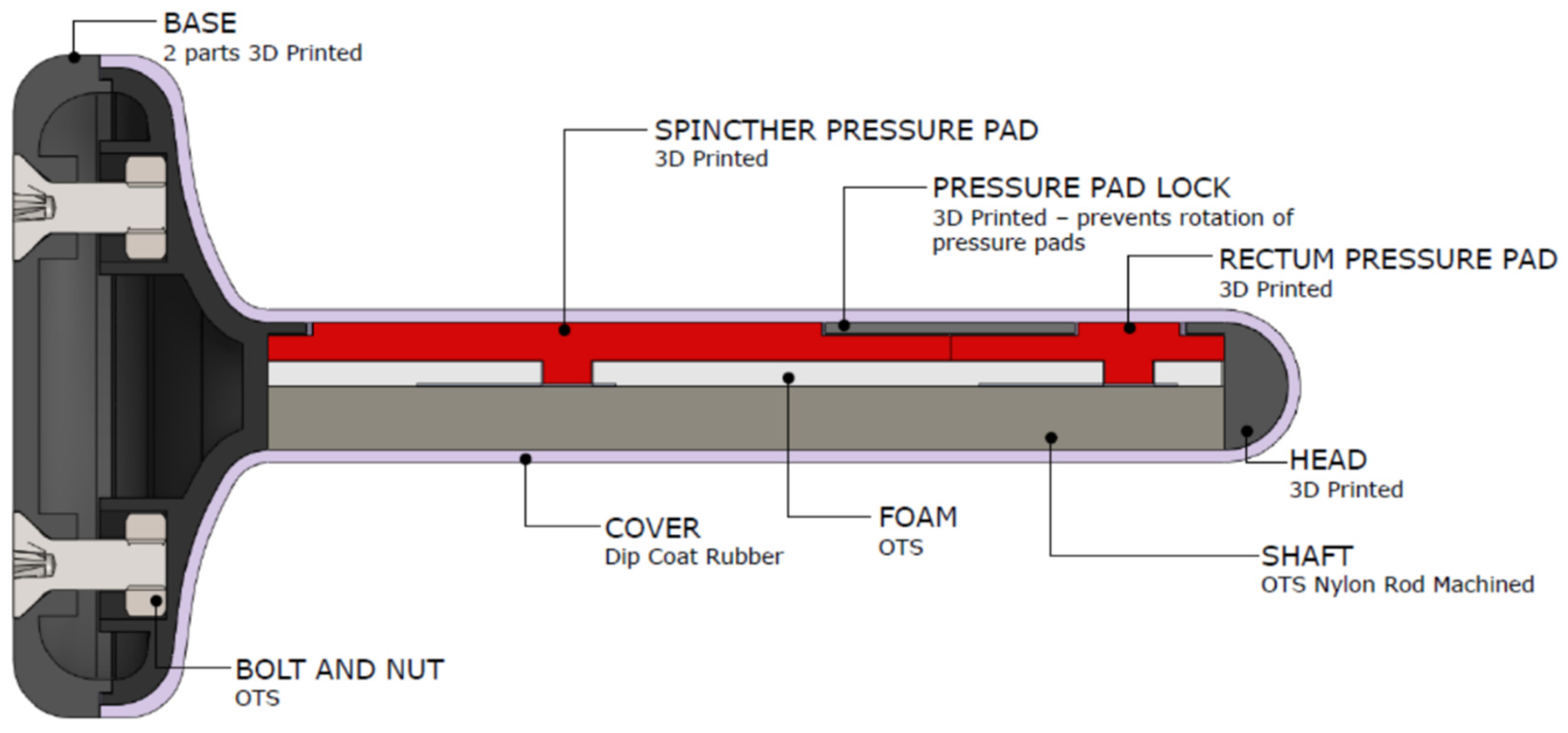
4.3. Sensing Probe
- (1)
- Pressure pads: Made from 3D printable, high-resolution castable wax resin to ensure uniform measurement of force over the surface of the sensors. They captured force over a large surface area and concentrated that force to the sensor, such that we can miniaturize the sensor and obtain a higher measurement for a given applied force or pressure.
- (2)
- Foam: Made from neoprene, to provide a spring force against the pad to ensure the pressure is released from the sensor when the contraction of the muscles and cavity is released.
- (3)
- Pressure pad locks: These ensure uniform measurement of pressure over the surface of the pressure pad by maintaining alignment of pressure pad to the sensor.
- (4)
- Cover and core: Dip coat rubber was used for the cover to allow for a soft surface, and the probe shaft was a nylon rod, machined to specification.
4.4. Networking
4.5. Software Implementation
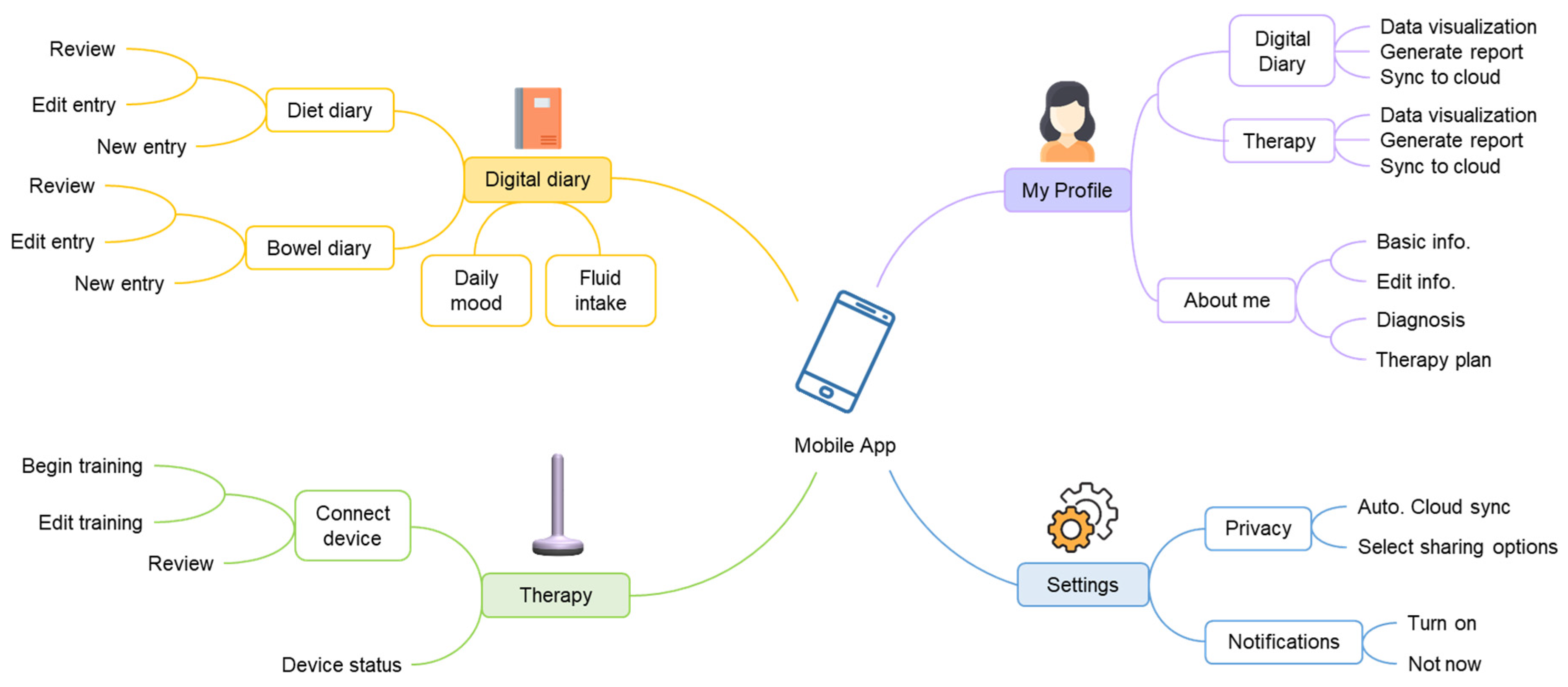
4.5.1. Mobile App
4.5.2. Cloud-Based Web Application
5. Performance Evaluation
5.1. IoMT Clinical Feasibility Study
5.2. Results and Discussion
5.3. User Evaluation of the Mobile App and Web Application
5.4. Security and Privacy Considerations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bayer, K.; Laura, M.; Gardner, S.; Pine, R. Engaging Stakeholders in the Home Medical Device Market. British Standards Institution. 2014. Available online: http://www.bsigroup.com/meddev/LocalFiles/en-US/Whitepapers/bsi-medical-device-home-devices-whitepaper.pdf (accessed on 29 July 2021).
- Deloitte. 2016 Global Health Care Outlook: Battling Costs while Improving Care. 2016. Available online: http://www2.deloitte.com/content/dam/Deloitte/global/Documents/Life-Sciences-Health-Care/gxlshc-2016-health-care-outlook.pdf (accessed on 4 July 2021).
- Geng, F.; Mansouri, S.; Stevenson, D.G.; Grabowski, D.C. Evolution of the home health care market: The expansion and quality performance of multi-agency chains. Health Serv. Res. 2020, 55, 1073–1084. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, J.M.; Swift, E.K.; Hurtado, M.P. (Eds.) Envisioning the National Health Care Quality Report; The National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- Gubbi, J.; Buyya, R.; Marusic, S.; Palaniswami, M. Internet of Things (IoT): A vision, architectural elements, and future directions. Future Gener. Comput. Syst. 2013, 29, 1645–1660. [Google Scholar] [CrossRef] [Green Version]
- Javadi, B.; Calheiros, R.N.; Matawie, K.M.; Ginige, A.; Cook, A. (Eds.) Smart Nutrition Monitoring System Using Heterogeneous Internet of Things Platform, in Internet and Distributed Computing Systems; Springer: Cham, Switzerland, 2018; pp. 63–74. [Google Scholar]
- Al-Turjman, F.; Nawaz, M.H.; Ulusar, U.D. Intelligence in the Internet of Medical Things era: A systematic review of current and future trends. Comput. Commun. 2020, 150, 644–660. [Google Scholar] [CrossRef]
- Rao, S.S.; Bharucha, A.E.; Chiarioni, G.; Felt-Bersma, R.; Knowles, C.; Malcolm, A.; Wald, A. Anorectal disorders. Gastroenterology 2016, 150, 1430–1442. [Google Scholar] [CrossRef]
- Rao, S.S.C.; Benninga, M.A.; Bharucha, A.E.; Chiarioni, G.; Di Lorenzo, C.; Whitehead, W.E. ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol. Motil. 2015, 27, 594–609. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.S.C.; Tuteja, A.K.; Vellema, T.; Kempf, J.; Stessman, M. Dyssynergic defecation: Demographics, symptoms, stool patterns, and quality of life. J. Clin. Gastroenterol. 2004, 38, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Pehl, C.; Seidl, H.; Scalercio, N.; Gundling, F.; Schmidt, T.; Schepp, W.; Labermeyer, S. Accuracy of Anorectal Manometry in Patients with Fecal Incontinence. Digestion 2012, 86, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.S.; Sivakumaran, Y.; Nassar, N.; Gladman, M.A. Fecal incontinence: Community prevalence and associated factors—A systematic review. Dis. Colon Rectum 2015, 58, 1194–1209. [Google Scholar] [CrossRef]
- Camilleri, M.; Ford, A.C.; Mawe, G.M.; Dinning, P.G.; Rao, S.S.C.; Chey, W.D.; Simrén, M.; Lembo, A.; Young-Fadok, T.M.; Chang, L. Chronic constipation. Nat. Rev. Dis. Primers 2017, 3, 17095. [Google Scholar] [CrossRef]
- Rao, S.S.; Seaton, K.; Miller, M.; Brown, K.; Nygaard, I.; Stumbo, P.; Zimmerman, B.; Schulze, K. Randomized Controlled Trial of Biofeedback, Sham Feedback, and Standard Therapy for Dyssynergic Defecation. Clin. Gastroenterol. Hepatol. 2007, 5, 331–338. [Google Scholar] [CrossRef]
- Heymen, S.; Scarlett, Y.; Jones, K.; Ringel, Y.; Drossman, D.; Whitehead, W.E. Randomized Controlled Trial Shows Biofeedback to be Superior to Pelvic Floor Exercises for Fecal Incontinence. Dis. Colon Rectum 2009, 52, 1730–1737. [Google Scholar] [CrossRef] [PubMed]
- Norton, C.; Kamm, M.A. Anal sphincter biofeedback and pelvic floor exercises for faecal incontinence in adults—A systematic review. Aliment. Pharmacol. Ther. 2001, 15, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.S.; Go, J.T.; Valestin, J.; Schneider, J. Home Biofeedback for the Treatment of Dyssynergic Defecation: Does It Improve Quality of Life and Is It Cost-Effective? Am. J. Gastroenterol. 2019, 114, 938–944. [Google Scholar] [CrossRef]
- Rao, S.S.C.; Valestin, J.A.; Xiang, X.; Hamdy, S.; Bradley, C.S.; Zimmerman, M.B. Home-based versus office-based biofeedback therapy for constipation with dyssynergic defecation: A randomised controlled trial. Lancet Gastroenterol. Hepatol. 2018, 3, 768–777. [Google Scholar] [CrossRef]
- Damin, D.C.; Hommerding, F.; Schirmer, D.; Sanches, P.R.; Junior, D.P.S.; Müller, A.F.; Thome, P.R. Patient-controlled biofeedback device for the treatment of fecal incontinence: A pilot study. Appl. Psychophysiol. Biofeedback 2017, 42, 133–137. [Google Scholar] [CrossRef]
- Gatouillat, A.; Badr, Y.; Massot, B.; Sejdic, E. Internet of Medical Things: A Review of Recent Contributions Dealing with Cyber-Physical Systems in Medicine. IEEE Internet Things J. 2018, 5, 3810–3822. [Google Scholar] [CrossRef] [Green Version]
- Solomon, M.; Pager, C.K.; Rex, J.; Roberts, R.; Manning, J. Randomized, Controlled Trial of Biofeedback with Anal Manometry, Transanal Ultrasound, or Pelvic Floor Retraining with Digital Guidance Alone in the Treatment of Mild to Moderate Fecal Incontinence. Dis. Colon Rectum 2003, 46, 703–710. [Google Scholar] [CrossRef]
- Rao, S.S.C.; Azpiroz, F.; Diamant, N.; Enck, P.; Tougas, G.; Wald, A. Minimum standards of anorectal manometry. Neurogastroenterol. Motil. 2002, 14, 553–559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azpiroz, F.; Enck, P.; Whitehead, W.E. Anorectal functional testing: Review of collective experience1. Am. J. Gastroenterol. 2002, 97, 232–240. [Google Scholar] [CrossRef]
- Lee, T.H.; Bharucha, A.E. How to Perform and Interpret a High-resolution Anorectal Manometry Test. J. Neurogastroenterol. Motil. 2016, 22, 46–59. [Google Scholar] [CrossRef]
- Heymen, S.; Jones, K.R.; Scarlett, Y.; Whitehead, W.E. Biofeedback treatment of constipation: A critical review. Dis. Colon Rectum 2003, 46, 1208–1217. [Google Scholar] [CrossRef]
- Gilliland, R.; Heymen, S.; Altomare, D.F.; Park, U.C.; Vickers, D.; Wexner, S.D. Outcome and predictors of success of biofeedback for constipation. Br. J. Surg. 1997, 84, 1123–1126. [Google Scholar]
- Lubowski, D.Z.; King, D.W. Obstructed Defecation: Current Status of Pathophysiology and Management. Aust. N. Z. J. Surg. 1995, 65, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Xiang, X.; Yan, Y.; Patcharatrakul, T.; Parr, R.; Rao, S.S. Home Biofeedback Therapy Improves Fecal Incontinence Severity and Quality of Life in a Non-Inferiority Randomized Controlled Study. Am. J. Gastroenterol. 2018, 113, S246. [Google Scholar] [CrossRef]
- Hay-Smith, E.J.; Bø Berghmans, L.C.; Hendriks, H.J.; De Bie, R.A.; Van Waalwijk Van Doorn, E.S. Pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst. Rev. 2001, CD001407. [Google Scholar] [CrossRef]
- Jundt, K.; Peschers, U.M.; Dimpfl, T. Long-term efficacy of pelvic floor re-education with EMG-controlled biofeedback. Eur. J. Obstet. Gynecol. Reprod. Biol. 2002, 105, 181–185. [Google Scholar] [CrossRef]
- Kawimbe, B.M.; Papachrysostomou, M.; Binnie, N.R.; Clare, N.; Smith, A.N. Outlet obstruction constipation (anismus) managed by biofeedback. Gut 1991, 32, 1175–1179. [Google Scholar] [CrossRef] [Green Version]
- Norton, C.; Cody, J.D. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst. Rev. 2012, 2012, CD002111. [Google Scholar] [CrossRef]
- Biosearch Medical Products Inc. Portable Anorectal Biofeedback System. Available online: https://cdn.icsa.es:8080/wp-content/uploads/2015/09/Sistema-portatil-Biofeedback.pdf (accessed on 24 August 2021).
- Kang, M.; Choo, P.; Watters, C.E. Design for experiencing: Participatory design approach with multidisciplinary perspectives. Procedia Soc. Behav. Sci. 2015, 174, 830–833. [Google Scholar] [CrossRef] [Green Version]
- Tekscan. FlexiForce A101 Datasheet. Available online: https://www.tekscan.com/resources/datasheets-guides/flexiforce-a101-datasheet (accessed on 11 September 2021).
- Adafruit. Adafruit Feather nRF52840 Express. Available online: https://www.adafruit.com/product/4062 (accessed on 9 September 2021).
- Kos, A.; Umek, A. Wearable Sensor Devices for Prevention and Rehabilitation in Healthcare: Swimming Exercise with Real-Time Therapist Feedback. IEEE Internet Things J. 2018, 6, 1331–1341. [Google Scholar] [CrossRef]
- Robertson, E.V.; Lee, Y.Y.; Derakhshan, M.H.; Wirz, A.A.; Whiting, J.R.H.; Seenan, J.P.; Connolly, P.; McColl, K.E.L. High-resolution esophageal manometry: Addressing thermal drift of the manoscan system. Neurogastroenterol. Motil. 2011, 24, 61-e11. [Google Scholar] [CrossRef] [PubMed]
- Babaei, A.; Lin, E.C.; Szabo, A.; Massey, B.T. Determinants of pressure drift in Manoscan™esophageal high-resolution manometry system. Neurogastroenterol. Motil. 2014, 27, 277–284. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.P.; Post, J.; Crowell, M.D. High-Resolution Manometry in the Evaluation of Anorectal Disorders: A Simultaneous Comparison with Water-Perfused Manometry. Am. J. Gastroenterol. 2007, 102, 850–855. [Google Scholar] [CrossRef]
- Sauter, M.; Heinrich, H.; Fox, M.; Misselwitz, B.; Halama, M.; Schwizer, W.; Fried, M.; Fruehauf, H. Toward more accurate measurements of anorectal motor and sensory function in routine clinical practice: Validation of High-Resolution Anorectal Manometry and Rapid Barostat Bag measurements of rectal function. Neurogastroenterol. Motil. 2014, 26, 685–695. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.R.; Lee, J.-E.; Lee, J.S.; Lee, T.H.; Hong, S.J.; Kim, J.O.; Jeon, S.R.; Kim, H.G. Comparison of High-resolution Anorectal Manometry with Water-perfused Anorectal Manometry. J. Neurogastroenterol. Motil. 2015, 21, 126–132. [Google Scholar] [CrossRef] [Green Version]
- Sivaraman, V.; Gharakheili, H.H.; Vishwanath, A.; Boreli, R.; Mehani, O. (Eds.) Network-level security and privacy control for smart-home IoT devices. In Proceedings of the 2015 IEEE 11th International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob), Abu Dhabi, United Arab Emirates, 19–21 October 2015. [Google Scholar]
- Garcia Lopez, P.; Montresor, A.; Epema, D.; Datta, A.; Higashino, T.; Iamnitchi, A.; Barcellos, M.; Felber, P.; Riviere, E. Edge-centric computing: Vision and challenges. ACM SIGCOMM Comput. Commun. Rev. 2015, 45, 37–42. [Google Scholar] [CrossRef]
- Yang, Y.; Wu, L.; Yin, G.; Li, L.; Zhao, H. A Survey on Security and Privacy Issues in Internet-of-Things. IEEE Internet Things J. 2017, 4, 1250–1258. [Google Scholar] [CrossRef]
- Ammar, M.; Russello, G.; Crispo, B. Internet of Things: A survey on the security of IoT frameworks. J. Inf. Secur. Appl. 2018, 38, 8–27. [Google Scholar] [CrossRef] [Green Version]



| Device | Sensor Type | Feedback | Data Storage/Sharing | Refs |
|---|---|---|---|---|
| MyoTron 120 (Enting Instruments & Systems, Dorst, The Netherlands) | EMG electrode | Audio feedback | No | [31] |
| Home Biofeedback device (DMI Medical Limited, Shrewsbury, UK) | Light strip illumination | No | [32] | |
| InTone MV (InControl Medical, Brookfield, WI, USA) | Numeric and light strip display | Internal data storage, downloadable to PC | [28] | |
| Biosearch Biofeedback monitor (Biosearch Medical Product Inc., Somerville, NJ, USA) | Single (air-filled) pressure sensor | Light strip illumination | Analogue strip chart recorder | [33] |
| Anatoner (Protech, Bengaluru, India) | Two (air-filled) pressure sensors | Light strip illumination | No | [18] |
| Portable Biofeedback Device (Research Prototype, Porto Alegre, Brazil) | Single pressure transducer | Waveform on LCD display | Internal data storage, downloadable to PC | [19] |
| Proposed IoMT | Two force sensors | Mobile app display | In app storage, cloud platform data sharing |
| Therapy | Pain Points | Needs | Service Opportunity | |
|---|---|---|---|---|
| Patients (user) | Clinic | Treatment is time consuming; requiring multiple clinic visits to selected clinics | Improve accessibility | Home therapy |
| Clinic | Therapy is embarrassing and invasive | Private and comfortable settings | Home therapy | |
| Home | Difficult to setup | Quick setup | Intuitive user experience (UX) | |
| Home | No sure if performing correct exercises | Clear training instructions | Simple training user interface (UI) | |
| Clinical Staff (provider) | Clinic | Resource intensive; limited by number of patients they can treat at once | Time and cost saving | Home therapy |
| Clinical | Poor compliance; <30% complete full therapy | Improve accessibility | Home therapy | |
| Home | Cannot ensure patients are performing training correctly | Remote monitoring | Data sync with cloud server | |
| Home | No standardization between home devices and clinical equipment | Comparable to HD-ARM | Calibrate against HD-ARM |
| Biofeedback Manoeuvres | Proposed IoMT (Units) Mean ± SD | HD-ARM (mmHg) Mean ± SD | Normal HD-ARM Range (mmHg) |
|---|---|---|---|
| Mean resting anal pressure | 48 ± 1.1 | 49 ± 0.8 | 40–70 |
| Mean resting rectal pressure | 36 ± 0.6 | 36 ± 0.2 | 30–90 |
| Maximum anal squeeze pressure | 132 ± 4.8 | 133 ± 4.0 | 100–180 |
| Duration of sustained squeeze (s) | 30 ± 0.2 | 30 ± 1.2 | >15 |
| Recto–anal pressure gradient | −58 ± 3.9 | −59 ± 2.9 | −50–−6 |
| Anal relaxation (%) | 41 ± 1.6 | 41 ± 1.7 | 20–60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, J.; Ho, V.; Javadi, B. New Internet of Medical Things for Home-Based Treatment of Anorectal Disorders. Sensors 2022, 22, 625. https://doi.org/10.3390/s22020625
Zhou J, Ho V, Javadi B. New Internet of Medical Things for Home-Based Treatment of Anorectal Disorders. Sensors. 2022; 22(2):625. https://doi.org/10.3390/s22020625
Chicago/Turabian StyleZhou, Jerry, Vincent Ho, and Bahman Javadi. 2022. "New Internet of Medical Things for Home-Based Treatment of Anorectal Disorders" Sensors 22, no. 2: 625. https://doi.org/10.3390/s22020625
APA StyleZhou, J., Ho, V., & Javadi, B. (2022). New Internet of Medical Things for Home-Based Treatment of Anorectal Disorders. Sensors, 22(2), 625. https://doi.org/10.3390/s22020625








