Research and Development of a COVID-19 Tracking System in Order to Implement Analytical Tools to Reduce the Infection Risk
Abstract
:1. Introduction
2. Symptoms, Transmission, and Monitoring of COVID-19 Physiological Manifestations
2.1. Ways of Spreading Diseases
2.2. Temperature as an Indicator of Human Health Condition
3. State of the Art of Monitoring Devices
4. Design of the Tracking System
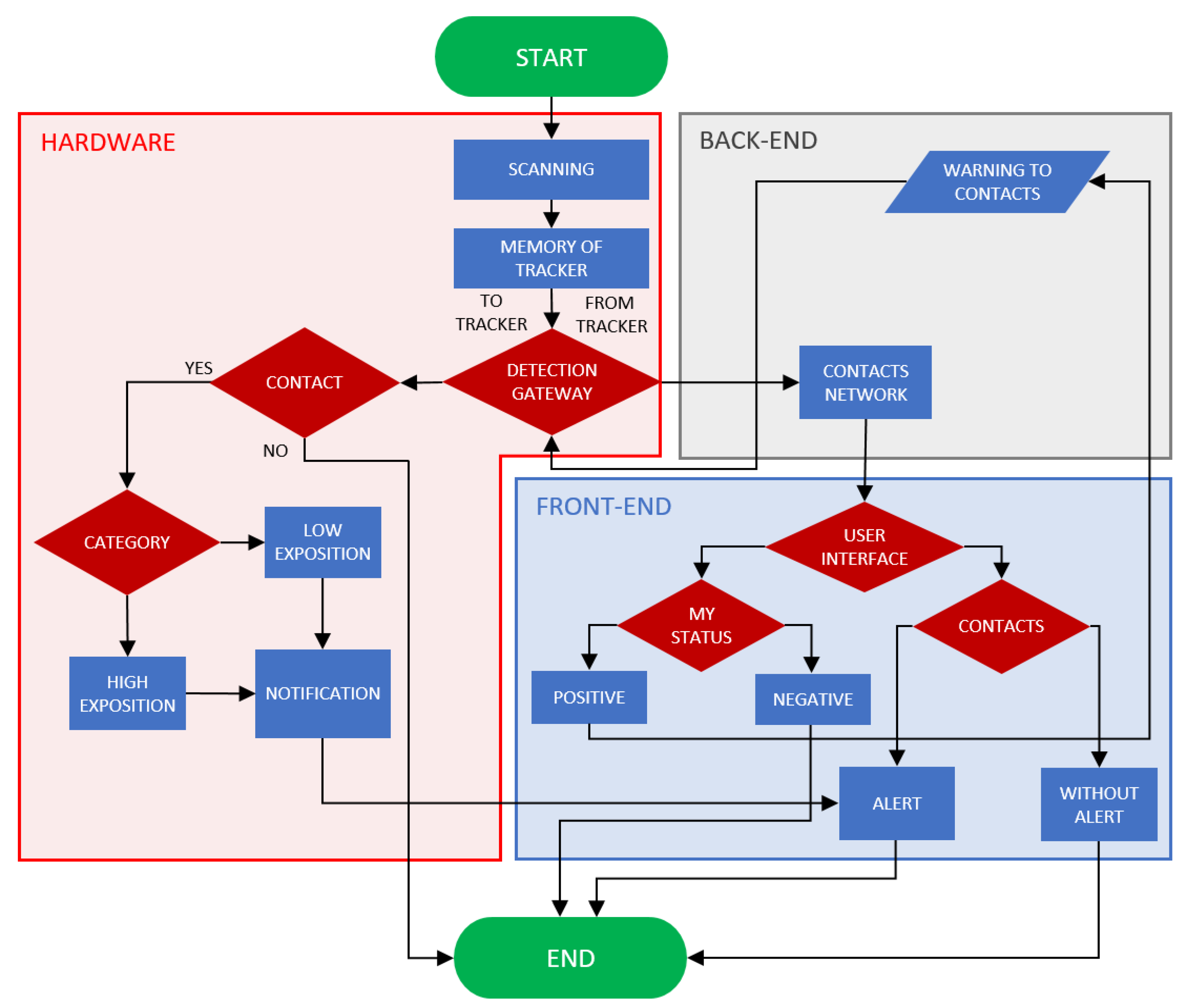
4.1. Principle
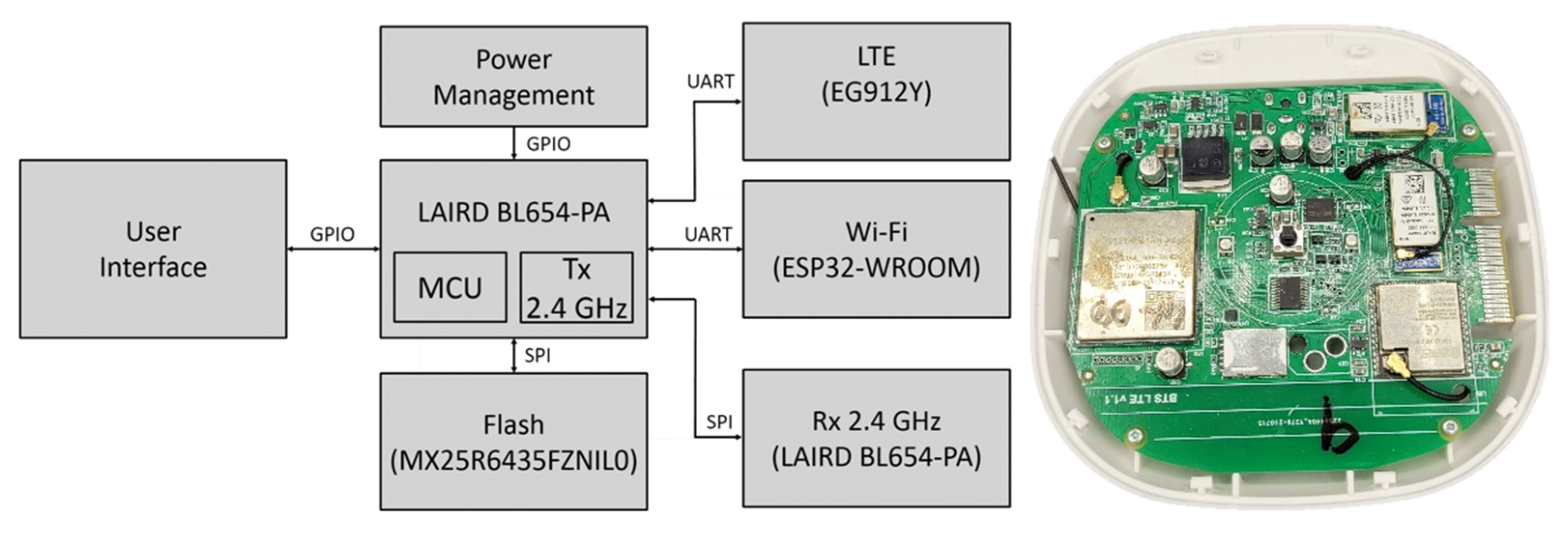
4.2. Hardware Design and Technical Specification
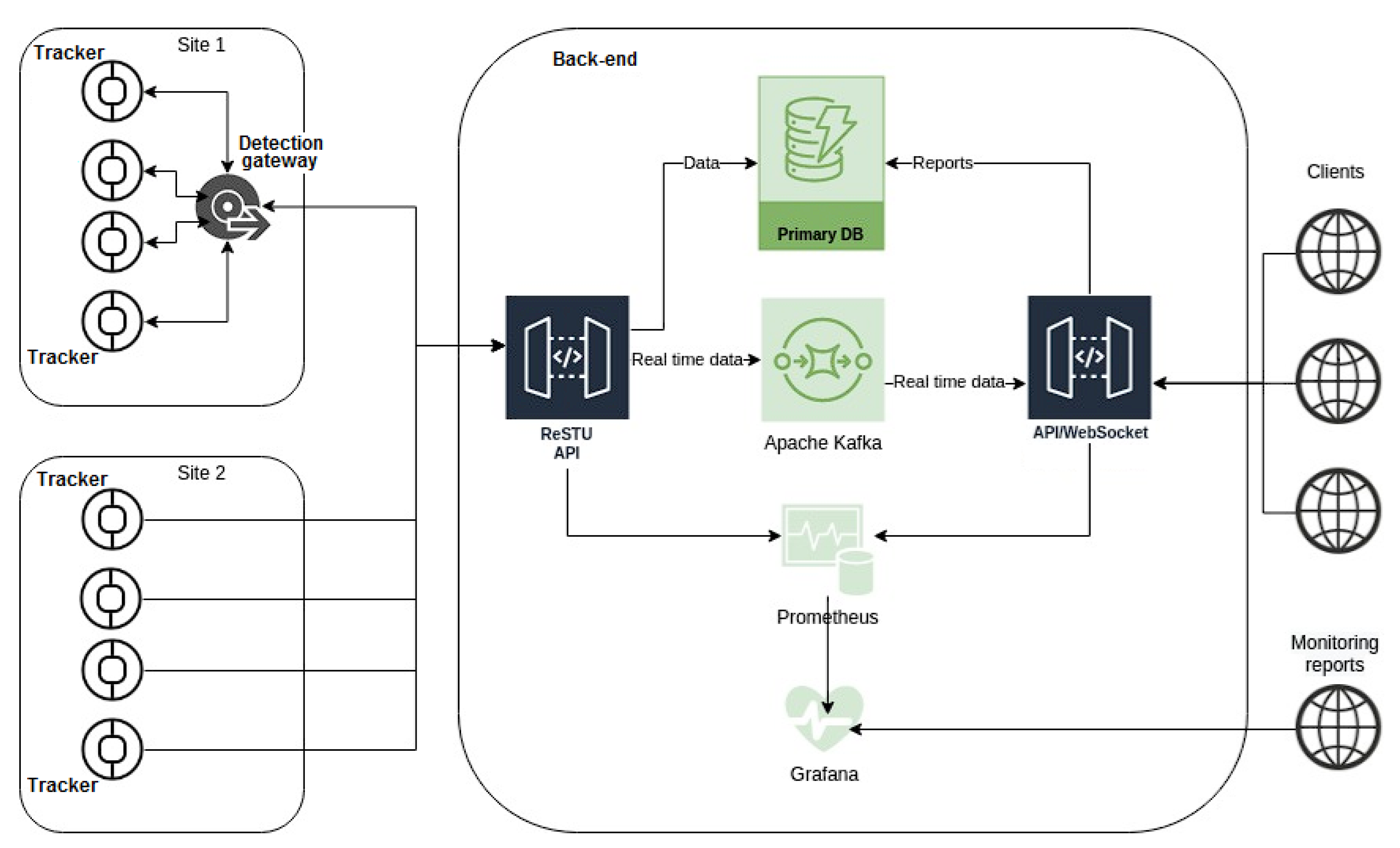
4.3. Back-End and Software
4.4. Functional Testing
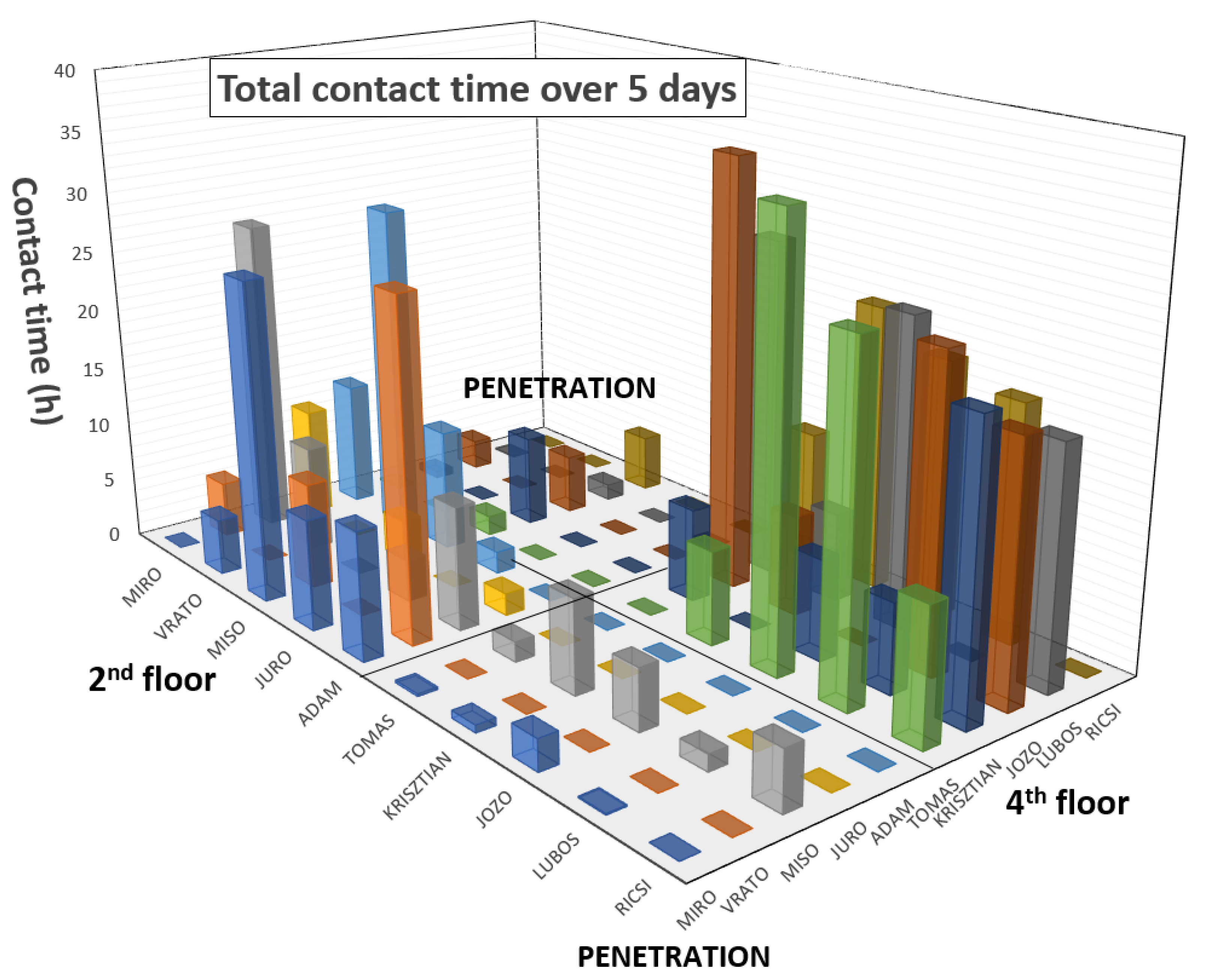
5. Results of Functional Testing
6. Discussion
7. Conclusions
8. Patents
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef]
- Coronavirus Worldometers. Available online: https://www.worldometers.info/coronavirus/ (accessed on 11 October 2021).
- WHO. Coronavirus Disease (COVID 19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 13 October 2021).
- Lai, C.C.; Liu, Y.H.; Wang, C.Y.; Wang, Y.H.; Hsueh, S.C.; Yen, M.Y.; Ko, W.C.; Hsueh, P.R. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J. Microbiol. Immunol. Infect. 2020, 53, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Hassantabar, S.; Stefano, N.; Ghanakota, V.; Ferrari, A.; Nicola, G.N.; Bruno, R.; Marino, I.R.; Hamidouche, K.; Jha, N.K. Coviddeep: SARS-CoV-2/COVID-19 Test Based on Wearable Medical Sensors and Efficient Neural Networks. IEEE Trans. Consum. Electron. 2020, 67, 244–256. [Google Scholar] [CrossRef]
- Ramanathan, K.; Antognini, D.; Combes, A.; Paden, M.; Zakhary, B.; Ogino, M.; Maclaren, G.; Brodie, D. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA-J. Am. Med. Assoc. 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Bai, L.; Yang, D.; Wang, X.; Tong, L.; Zhu, X.; Zhong, N.; Bai, C.; Powell, C.A.; Chen, R.; Zhou, J.; et al. Chinese experts’ consensus on the Internet of Things-aided diagnosis and treatment of coronavirus disease 2019 (COVID-19). Clin. eHealth 2020, 3, 7–15. [Google Scholar] [CrossRef]
- Otoom, M.; Otoum, N.; Alzubaidi, M.A.; Etoom, Y.; Banihani, R. An IoT-based framework for early identification and monitoring of COVID-19 cases. Biomed. Signal Process. Control 2020, 62, 102149. [Google Scholar] [CrossRef] [PubMed]
- Venkataramanaiah, B.; Kamala, J. ECG signal processing and KNN classifier-based abnormality detection by VH-doctor for remote cardiac healthcare monitoring. Soft Comput. 2020, 24, 17457–17466. [Google Scholar] [CrossRef]
- Karthickraja, R.; Kumar, R.; Kirubakaran, S.; Marcilin, L.J.A.; Manikandan, R. COVID-19 prediction and symptom analysis using wearable sensors and IoT. Int. J. Pervasive Comput. Commun. 2020. ahead-of-printing. [Google Scholar] [CrossRef]
- Nitsure, M.; Sarangi, B.; Shankar, G.H.; Reddy, V.S.; Walimbe, A.; Sharma, V.; Prayag, S. Mechanisms of hypoxia in COVID-19 patients: A pathophysiologic reflection. Indian J. Crit. Care Med. 2020, 24, 967–970. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Panigrahy, A.K. COVID-19 ARDS: Can systemic oxygenation utilization guide oxygen therapy? Indian J. Crit. Care Med. 2021, 25, 115–116. [Google Scholar] [CrossRef]
- Ullah, F.; Haq, H.U.; Khan, J.; Safeer, A.A.; Asif, U.; Lee, S. Wearable iots and geo-fencing based framework for COVID-19 remote patient health monitoring and quarantine management to control the pandemic. Electronics 2021, 10, 2035. [Google Scholar] [CrossRef]
- Coronavirus (COVID-19) in the Slovak Republic in Numbers. Available online: https://korona.gov.sk/koronavirus-na-slovensku-v-cislach/ (accessed on 19 October 2021).
- Thachil, J.; Tang, N.; Gando, S.; Falanga, A.; Cattaneo, M.; Levi, M.; Clark, C.; Iba, T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J. Thromb. Haemost. 2020, 18, 1023–1026. [Google Scholar] [CrossRef]
- Bourouiba, L. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential Implications for Reducing Transmission of COVID-19. JAMA-J. Am. Med. Assoc. 2020, 323, 1837–1838. [Google Scholar] [CrossRef]
- Lewis, D. Is the coronavirus airborne? Experts can’t agree. Nature 2020, 580, 175. [Google Scholar] [CrossRef] [Green Version]
- Kremer, C.; Ganyani, T.; Chen, D.; Torneri, A.; Faes, C.; Wallinga, J.; Hens, N. Authors’ response: Estimating the generation interval for COVID-19 based on symptom onset data. Eurosurveillance 2020, 25, 18–19. [Google Scholar] [CrossRef]
- Chia, P.Y.; Coleman, K.K.; Tan, Y.K.; Ong, S.W.X.; Gum, M.; Lau, S.K.; Lim, X.F.; Lim, A.S.; Sutjipto, S.; Lee, P.H.; et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020, 11, 2800. [Google Scholar] [CrossRef] [PubMed]
- Santarpia, J.L.; Rivera, D.N.; Herrera, V.L.; Morwitzer, M.J.; Creager, H.M.; Santarpia, G.W.; Crown, K.K.; Brett-Major, D.M.; Schnaubelt, E.R.; Broadhurst, M.J.; et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020, 10, 12732. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; El-harakeh, A.; Bognanni, A.; Lotfi, T.; Loeb, M.; et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Sun, C.; Zhai, Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020, 62, 102390. [Google Scholar] [CrossRef]
- Tysiąc-Miśta, M.; Dubiel, A.; Brzoza, K.; Burek, M.; Pałkiewicz, K. Air disinfection procedures in the dental office during the COVID-19 pandemic. Med. Pr. 2021, 72, 39–48. [Google Scholar] [CrossRef] [PubMed]
- O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials 2020, 13, 3363. [Google Scholar] [CrossRef] [PubMed]
- Mouchtouri, V.A.; Koureas, M.; Kyritsi, M.; Vontas, A.; Kourentis, L.; Sapounas, S.; Rigakos, G.; Petinaki, E.; Tsiodras, S.; Hadjichristodoulou, C. Environmental contamination of SARS-CoV-2 on surfaces, air-conditioner and ventilation systems. Int. J. Hyg. Environ. Health 2020, 230, 113599. [Google Scholar] [CrossRef] [PubMed]
- Bueckert, M.; Gupta, R.; Gupta, A.; Garg, M.; Mazumder, A. Correction: Bueckert et al. Infectivity of SARS-CoV-2 and Other Coronaviruses on Dry Surfaces: Potential for Indirect Transmission. Materials 2020, 13, 5211. Materials 2021, 14, 2816. [Google Scholar] [CrossRef]
- Chirico, F.; Sacco, A.; Bragazzi, N.L.; Magnavita, N. Can air-conditioning systems contribute to the spread of SARS/MERS/COVID-19 infection? Insights from a rapid review of the literature. Int. J. Environ. Res. Public Health 2020, 17, 6052. [Google Scholar] [CrossRef]
- Sagripanti, J.L.; Lytle, C.D. Estimated Inactivation of Coronaviruses by Solar Radiation With Special Reference to COVID-19. Photochem. Photobiol. 2020, 96, 731–737. [Google Scholar] [CrossRef]
- Suwanwongse, K.; Shabarek, N. Hyperpyrexia in patients with COVID-19. J. Med. Virol. 2020, 92, 2857–2862. [Google Scholar] [CrossRef]
- Schneider, A.; Kirsten, H.; Lordick, F.; Lordick, F.; Lubbert, C.; Braun, A. Von COVID-19 in outpatients-Is fever a useful indicator for SARS-CoV-2 infection? PLoS ONE 2021, 16, e0246312. [Google Scholar] [CrossRef]
- Choron, R.L.; Butts, C.A.; Bargoud, C.; Krumrei, N.J.; Teichman, A.L.; Schroeder, M.E.; Bover Manderski, M.T.; Cai, J.; Song, C.; Rodricks, M.B.; et al. Fever in the ICU: A Predictor of Mortality in Mechanically Ventilated COVID-19 Patients. J. Intensive Care Med. 2021, 36, 484–493. [Google Scholar] [CrossRef]
- Chew, N.W.; Ngiam, J.N.; Tham, S.M.; Lim, Z.Y.; Li, T.Y.W.; Cen, S.; Yap, E.S.; Tambyah, P.A.; Santosa, A.; Cross, G.B.; et al. Fever as a predictor of adverse outcomes in COVID-19. QJM An Int. J. Med. 2021, 114, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Ding, F.M.; Feng, Y.; Han, L.; Zhou, Y.; Ji, Y.; Hao, H.J.; Xue, Y.S.; Yin, D.N.; Xu, Z.C.; Luo, S.; et al. Early Fever Is Associated With Clinical Outcomes in Patients with Coronavirus Disease. Front. Public Health 2021, 9, 1249. [Google Scholar] [CrossRef]
- Leung, C. Risk factors for predicting mortality in elderly patients with COVID-19: A review of clinical data in China. Mech. Ageing Dev. 2020, 188, 111255. [Google Scholar] [CrossRef]
- Drewry, A.M.; Hotchkiss, R.; Kulstad, E. Response to “body temperature correlates with mortality in COVID-19 patients”. Crit. Care 2020, 24, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, P.; Joshua Pfefer, T.; Casamento, J.P.; Simpson, R.; Wang, Q. Best practices for standardized performance testing of infrared thermographs intended for fever screening. PLoS ONE 2018, 13, e0203302. [Google Scholar] [CrossRef] [Green Version]
- Bitar, D.; Goubar, A.; Desenclos, J.C. International travels and fever screening during epidemics: A literature review on the effectiveness and potential use of non-contact infrared thermometers. Euro Surveill. 2009, 14, 19115. [Google Scholar] [CrossRef]
- Stave, G.M.; Smith, S.E.; Hymel, P.A.; Heron, R.J.L. Worksite Temperature Screening for COVID-19. J. Occup. Environ. Med. 2021, 63, 638–641. [Google Scholar] [CrossRef] [PubMed]
- Mekjavic, I.B.; Tipton, M.J. Myths and methodologies: Degrees of freedom–limitations of infrared thermographic screening for COVID-19 and other infections. Exp. Physiol. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Fernando, L.; Vargas, A. Limitations of Temporal (Forehead) Temperature Readings. PENSAR EN MOVIMIENTO Rev. Cienc. Ejerc. Salud 2020, 18, 1–11. [Google Scholar]
- Dell’isola, G.B.; Cosentini, E.; Canale, L.; Ficco, G.; Dell’isola, M. Noncontact body temperature measurement: Uncertainty evaluation and screening decision rule to prevent the spread of COVID-19. Sensors 2021, 21, 346. [Google Scholar] [CrossRef]
- Niven, D.J.; Gaudet, J.E.; Laupland, K.B.; Mrklas, K.J.; Roberts, D.J.; Stelfox, H.T. Accuracy of Peripheral Thermometers for Estimating Temperature. Ann. Intern. Med. 2015, 163, 768–777. [Google Scholar] [CrossRef]
- Nuertey, B.D.; Ekremet, K.; Haidallah, A.R.; Mumuni, K.; Addai, J.; Attibu, R.I.E.; Damah, M.C.; Duorinaa, E.; Seidu, A.S.; Adongo, V.C.; et al. Performance of COVID-19 associated symptoms and temperature checking as a screening tool for SARS-CoV-2 infection. PLoS ONE 2021, 16, e0257450. [Google Scholar] [CrossRef]
- Resideo, LifeStream TM Remote Health Monitoring Solution. Available online: https://lifecare.resideo.com/ (accessed on 5 November 2021).
- Boaz, A.; Al, E. Remote Health Monitoring System. 2001. Available online: https://patents.google.com/patent/US6171237/ (accessed on 5 November 2021).
- Jovanov, E.; Raskovic, D.; Price, J.; Chapman, J.; Moore, A.; Krishnamurthy, A. Patient monitoring using personal area networks of wireless intelligent sensors. Biomed. Sci. Instrum. 2001, 37, 373–378. [Google Scholar] [PubMed]
- Oleshchuk, V.; Fensli, R. Remote Patient Monitoring Within a Future 5G Infrastructure. Wirel. Pers. Commun. 2011, 57, 431–439. [Google Scholar] [CrossRef] [Green Version]
- Malasinghe, L.P.; Ramzan, N.; Dahal, K. Remote patient monitoring: A comprehensive study. J. Ambient Intell. Humaniz. Comput. 2019, 10, 57–76. [Google Scholar] [CrossRef] [Green Version]
- Strempel, P. EIT Digital Pilots COVID-19 Tracing with Physical Tokens in Stadiums, Hospitals, Schools, and Concert Halls. Available online: https://www.eitdigital.eu/newsroom/news/archive/article/eit-digital-pilots-covid-19-tracing-with-physical-tokens-in-stadiums-hospitals-schools-and-concert-halls/ (accessed on 5 November 2021).
- Bentotahewa, V.; Hewage, C.; Williams, J. Security and Privacy Issues Associated with Coronavirus Diagnosis and Prognosis. In Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering; Paiva, S., Lopes, S.I., Zitouni, R., Gupta, N., Lopes, S.F., Yonezawa, T., Eds.; Springer International Publishing: Cham, Switzerland, 2021; Volume 372, pp. 108–116. ISBN 978-3-030-76062-5. [Google Scholar]
- Yousif, M.; Hewage, C.; Nawaf, L. IOT technologies during and beyond COVID-19: A comprehensive review. Future Internet 2021, 13, 105. [Google Scholar] [CrossRef]
- Boss, G.J.; Finn, P.G.; Rick, A.; Hamilton, I.; Kozloski, J.R. Tracking Pathogen Exposure 2018. U.S. Patent 2018052970A1, 22 February 2018. [Google Scholar]
- Akutagava, C.E.; Myslinski, L.J. Method of and Device fore Implementing Contagious Illness Analysis and Tracking 2020. U.S. Patent 2020279339A1, 3 September 2020. [Google Scholar]
- Wong, C.M. System and Method for Creating a Proximity Map of Plurality of Living Beings and Objects 2007. U.S. Patent 2007106775A1, 10 May 2007. [Google Scholar]
- Wairehealth C-Detect: A Wearable Vital Signs Monitor for Everyone. Available online: https://www.c19detect.com/ (accessed on 5 November 2021).
- EIT Digital Crowdband. Available online: https://en.crowdband.life/ (accessed on 5 November 2021).
- Nachverfolgung von Kontakten Innerhalb Einer Gruppe von Personen 2020. DE Patent 202020102994U1, 20 August 2020.
- Free COVID 19 Contact Tracing for Restaurateurs. Available online: https://www.restauranthub.co.nz/for-restaurants/covid-19-contact-tracing/ (accessed on 5 November 2021).
- Digital Check-in Solution for Restaurants. Available online: https://www.resmio.com/en/reservations/guest-check-in-qr-code/ (accessed on 5 November 2021).
- Cypress Semiconductor, Comparison of 2.4-GHz Proprietary RF and Bluetooth 4.0 for HID Applications. In DigiKey Techzone Magazine; Digi-Key Corporation: Thief River Falls, MN, USA, 2010; pp. 52–55.
- Texas Instrument. Wireless Connectivity Technology Selection Guide; Texas Instruments: Dallas, TX, USA, 2021. [Google Scholar]
- Kumar, P.; Reddy, L.; Varma, S. Distance measurement and error estimation scheme for RSSI based localization in Wireless Sensor Networks. In Proceedings of the 2009 Fifth International Conference on Wireless Communication and Sensor Networks (WCSN), Allahabad, India, 15–19 December 2009; IEEE: Piscataway, NJ, USA, 2009; pp. 1–4. [Google Scholar]
- Laird. User Guide: BL654 smartBASIC Extensions; Laird: Akron, OH, USA, 2018. [Google Scholar]
- Vavrinsky, E.; Subjak, J.; Donoval, M.; Wagner, A.; Zavodnik, T.; Svobodova, H. Application of Modern Multi-Sensor Holter in Diagnosis and Treatment. Sensors 2020, 20, 2663. [Google Scholar] [CrossRef] [PubMed]
- Vavrinsky, E.; Stopjakova, V.; Kopani, M.; Kosnacova, H. The Concept of Advanced Multi-Sensor Monitoring of Human Stress. Sensors 2021, 21, 3499. [Google Scholar] [CrossRef]






| Tracking sensor Communication protocol RSSI Receiver sensitivity | Laird BL654 Proprietary 2.4 GHz 1 dB resolution −95 dBm (1 Mbps) |
| Microcontroller | Nordic nRF52840 64 MHz Cortex-M4 with FPU 1 MB Flash, 256 KB RAM 2.4 GHz Transceiver |
| Real-time clock Accuracy | Micro Crystal RV-8263-C7 RTC ±20 ppm @ 25 °C |
| Temperature sensor Range/Accuracy Resolution Body contact | Silicon Labs SI7051-A20-IM 35.8–41 °C/±0.1 °C 20–70 °C/±0.13 °C 14-bit Surgical steel |
| Barometer Range Precision/Absolute accuracy | Infineon Technologies DPS310 300–1200 hPa ±0.002 hPa/±1 hPa |
| Internal memory Format Size Clock | Macronix MX25R1635FZUILO Flash 16 Mb 33 MHz |
| Dimensions (case) | Ø 46 × 13 mm |
| Weight | 30 g (strap included) |
| Power supply Battery life Charging | 3.7 V Li-Pol 300 mAh Approx. 80 days 60 min via a micro-USB connector |
| Next features | RGB LED signalization Switch on/off by unplugging/plugging to the charger Service button |
| Microcontroller | Nordic nRF52840 64 MHz Cortex-M4 with FPU 1 MB Flash, 256 KB RAM 2.4 GHz transceiver |
| Tracker communication Communication protocol Receive sensitivity Signal zone | Laird BL654-PA extended with LNA Proprietary 2.4 GHz −98.5 to −107 dBm Ideal: 1.6 km (outside)/Real: 50 m (inside) |
| LTE Data transmission Data rates | Quectel EG912Y LTE, GSM/GPRS/EDGE 10/5 Mbps (downlink/uplink @ LTE FDD) |
| Wi-Fi Wi-Fi protocol CPU | Espressif ESP32 WROOM 802.11 b/g/n (802.11n up to 150 Mbps), 2.4 GHz ESP32-D0WD-V3 Dual Core 240 MHz |
| Antenna Number × connector Peak gain | Laird 2.4 GHz Dipole RF 2 × SMA +2 dBi |
| Internal memory Format Size Clock | Macronix MX25R6435FZNIL0 Flash 64 Mb 80 MHz |
| Dimensions (without antenna) | 105 × 105 × 27 mm |
| Weight (without antenna) | 100 g |
| Power supply | 5 V/4 A via power jack |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vavrinsky, E.; Zavodnik, T.; Debnar, T.; Cernaj, L.; Kozarik, J.; Micjan, M.; Nevrela, J.; Donoval, M.; Kopani, M.; Kosnacova, H. Research and Development of a COVID-19 Tracking System in Order to Implement Analytical Tools to Reduce the Infection Risk. Sensors 2022, 22, 526. https://doi.org/10.3390/s22020526
Vavrinsky E, Zavodnik T, Debnar T, Cernaj L, Kozarik J, Micjan M, Nevrela J, Donoval M, Kopani M, Kosnacova H. Research and Development of a COVID-19 Tracking System in Order to Implement Analytical Tools to Reduce the Infection Risk. Sensors. 2022; 22(2):526. https://doi.org/10.3390/s22020526
Chicago/Turabian StyleVavrinsky, Erik, Tomas Zavodnik, Tomas Debnar, Lubos Cernaj, Jozef Kozarik, Michal Micjan, Juraj Nevrela, Martin Donoval, Martin Kopani, and Helena Kosnacova. 2022. "Research and Development of a COVID-19 Tracking System in Order to Implement Analytical Tools to Reduce the Infection Risk" Sensors 22, no. 2: 526. https://doi.org/10.3390/s22020526
APA StyleVavrinsky, E., Zavodnik, T., Debnar, T., Cernaj, L., Kozarik, J., Micjan, M., Nevrela, J., Donoval, M., Kopani, M., & Kosnacova, H. (2022). Research and Development of a COVID-19 Tracking System in Order to Implement Analytical Tools to Reduce the Infection Risk. Sensors, 22(2), 526. https://doi.org/10.3390/s22020526







