Energy Drinks Decrease Left Ventricular Efficiency in Healthy Children and Teenagers: A Randomized Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Study Population
2.3. Study Design
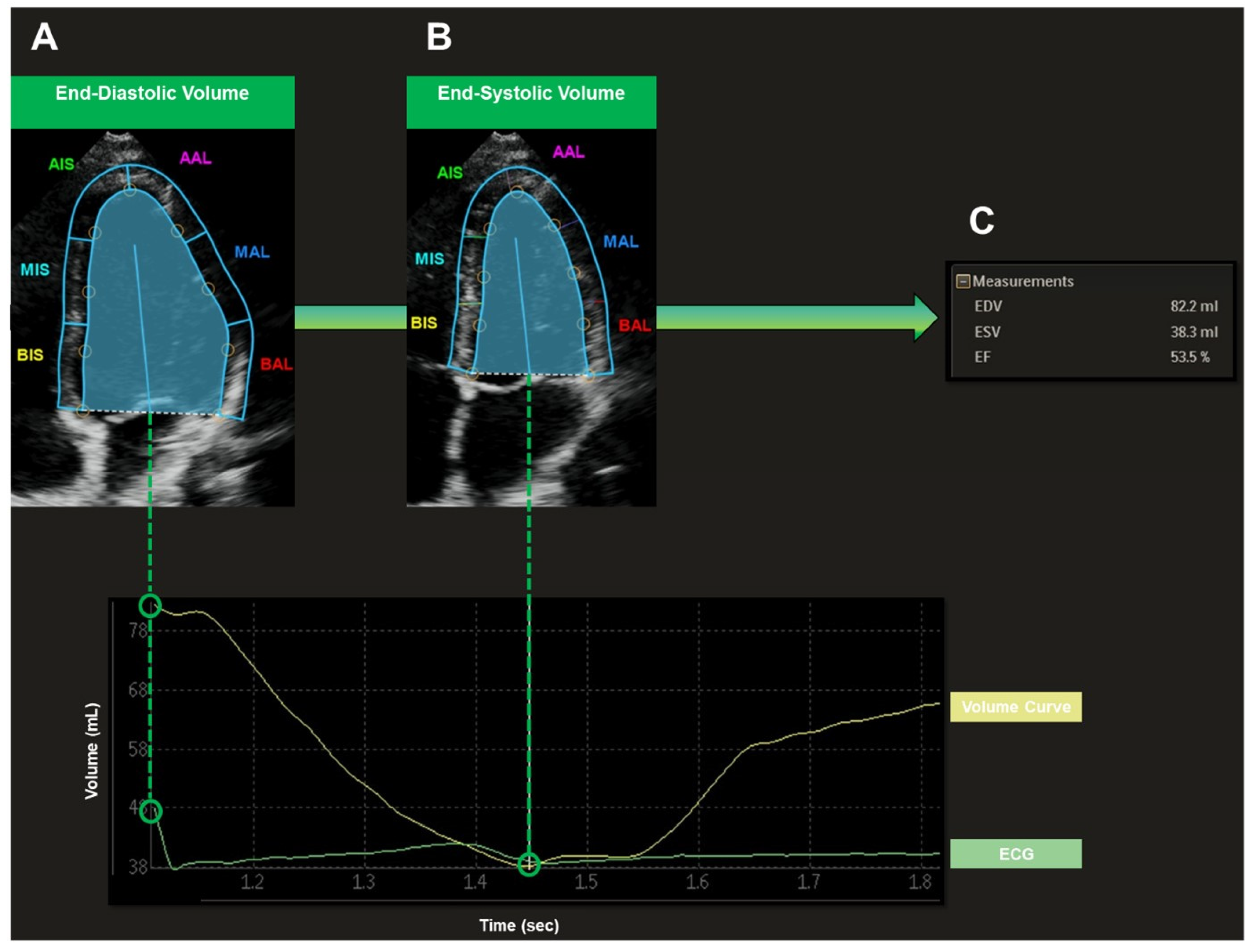
2.4. Echocardiographic Examination
2.5. Blood Pressure Measurement
2.6. Non-Invasive Left Ventricular Pressure-Volume Loops
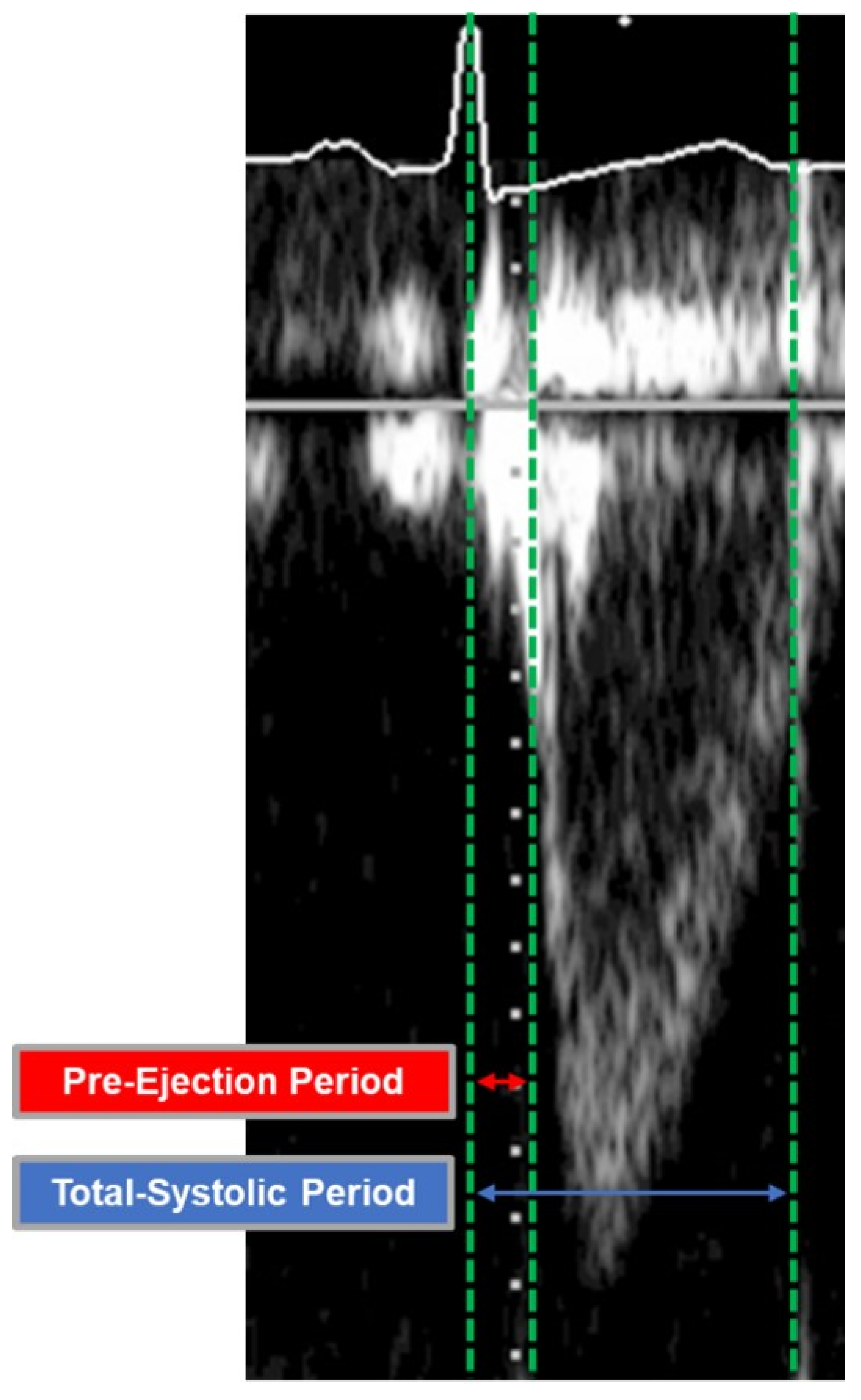
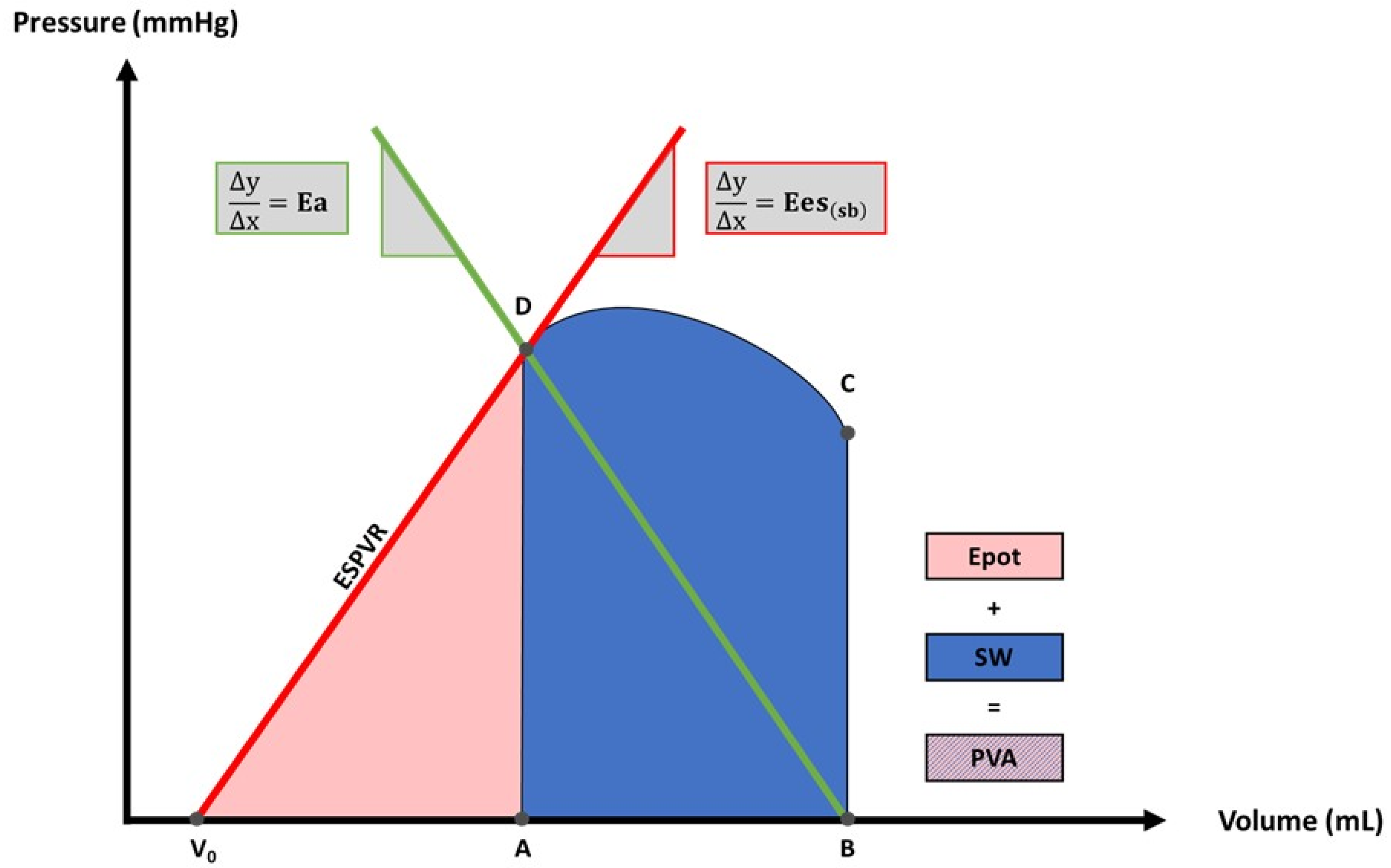
2.6.1. Arterial Elastance and End-Systolic Elastance
2.6.2. Potential Energy, Stroke Work and Pressure–Volume Area
2.6.3. Left Ventricular Efficiency Parameters
2.7. End-Point Measurement
2.8. Statistical Analysis
3. Results
3.1. Acute Effects of Energy Drinks on Left Ventricular Hemodynamics
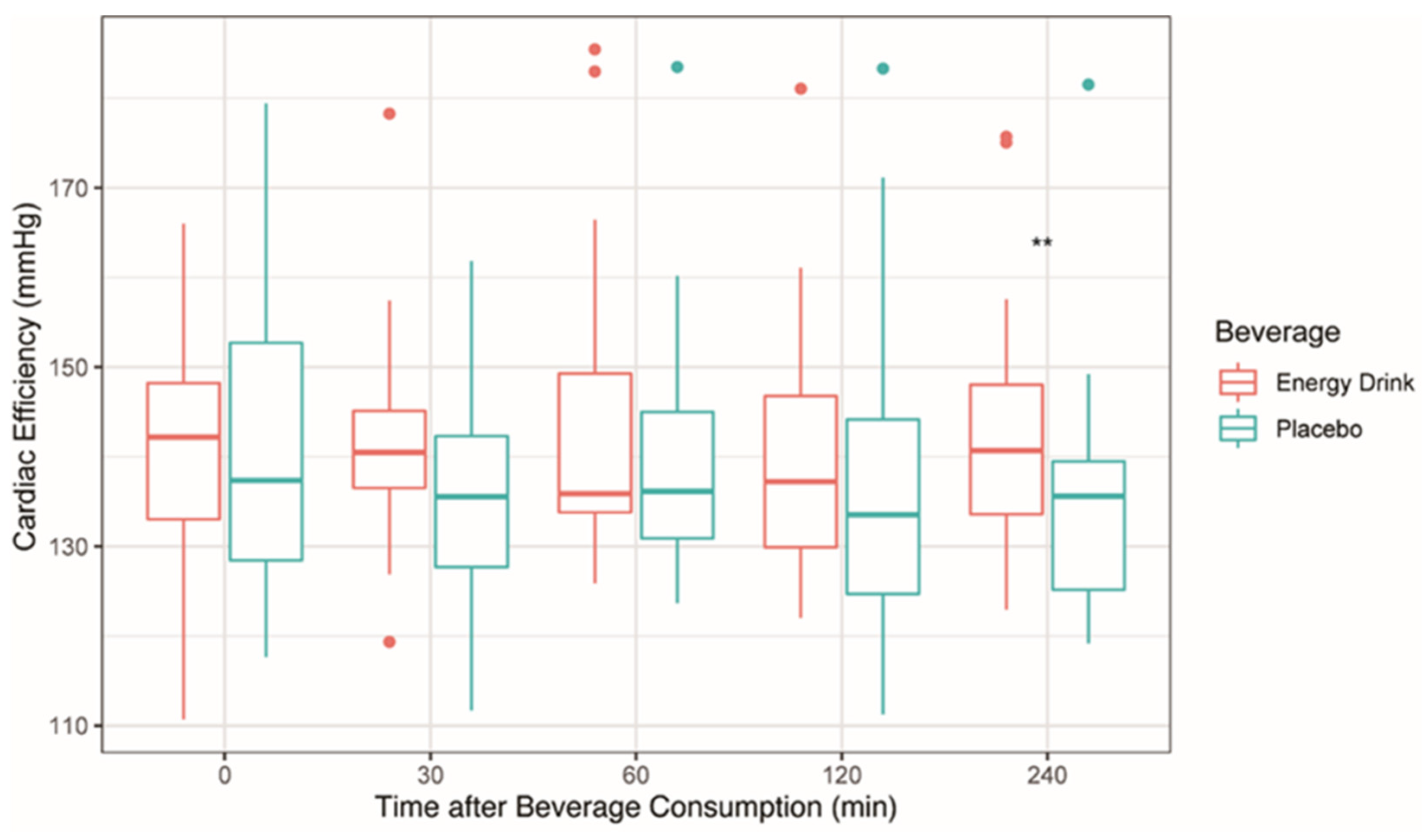
3.2. Acute Effects of Energy Drinks on Left Ventricular Efficiency
4. Discussion
4.1. Pathophysiological Considerations
4.2. Energy Drinks: A Potential Threat for Pediatric Heart Function?
4.3. Limitations
4.3.1. Study Design
4.3.2. Methodology
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zucconi, S.; Volpato, C.; Adinolfi, F.; Gandini, E.; Gentile, E.; Loi, A.; Fioriti, L. Gathering consumption data on specific consumer groups of energy drinks. EFS3 2013, 10, 115. [Google Scholar] [CrossRef]
- Cao, D.X.; Maiton, K.; Nasir, J.M.; Estes, N.A.M.; Shah, S.A. Energy Drink-Associated Electrophysiological and Ischemic Abnormalities: A Narrative Review. Front. Cardiovasc. Med. 2021, 8, 679105. [Google Scholar] [CrossRef] [PubMed]
- Usman, A.; Jawaid, A. Hypertension in a young boy: An energy drink effect. BMC Res. Notes 2012, 5, 591. [Google Scholar] [CrossRef] [PubMed]
- Polat, N.; Ardıç, I.; Akkoyun, M.; Vuruşkan, E. Spontaneous coronary artery dissection in a healthy adolescent following consumption of caffeinated “energy drinks”. Turk Kardiyol. Dern. Ars. 2013, 41, 738–742. [Google Scholar] [CrossRef] [PubMed]
- Fisk, G.; Hammond-Haley, M.; D’Silva, A. Energy drink-induced cardiomyopathy. BMJ Case Rep. 2021, 14, e239370. [Google Scholar] [CrossRef]
- Belzile, D.; Cinq-Mars, A.; Bernier, M.; Leblanc, M.-H.; Bourgault, C.; Morin, J.; Laflamme, M.; Charbonneau, É.; Sénéchal, M. Do Energy Drinks Really Give You Wings? Left Ventricular Assist Device Therapy as a Bridge to Recovery for an Energy Drink-Induced Cardiomyopathy. Can. J. Cardiol. 2020, 36, 317.e1–317.e3. [Google Scholar] [CrossRef]
- Kaoukis, A.; Panagopoulou, V.; Mojibian, H.R.; Jacoby, D. Reverse Takotsubo cardiomyopathy associated with the consumption of an energy drink. Circulation 2012, 125, 1584–1585. [Google Scholar] [CrossRef]
- Oberhoffer, F.S.; Li, P.; Jakob, A.; Dalla-Pozza, R.; Haas, N.A.; Mandilaras, G. Energy Drinks: Effects on Blood Pressure and Heart Rate in Children and Teenagers. A Randomized Trial. Front. Cardiovasc. Med. 2022, 9, 394E. [Google Scholar] [CrossRef]
- Doerner, J.M.; Kuetting, D.L.; Luetkens, J.A.; Naehle, C.P.; Dabir, D.; Homsi, R.; Nadal, J.; Schild, H.H.; Thomas, D.K. Caffeine and taurine containing energy drink increases left ventricular contractility in healthy volunteers. Int. J. Cardiovasc. Imaging 2015, 31, 595–601. [Google Scholar] [CrossRef]
- Menci, D.; Righini, F.M.; Cameli, M.; Lisi, M.; Benincasa, S.; Focardi, M.; Mondillo, S. Acute effects of an energy drink on myocardial function assessed by conventional echo-Doppler analysis and by speckle tracking echocardiography on young healthy subjects. J. Amino Acids 2013, 2013, 646703. [Google Scholar] [CrossRef]
- El Mahdiui, M.; van der Bijl, P.; Abou, R.; Ajmone Marsan, N.; Delgado, V.; Bax, J.J. Global Left Ventricular Myocardial Work Efficiency in Healthy Individuals and Patients with Cardiovascular Disease. J. Am. Soc. Echocardiogr. 2019, 32, 1120–1127. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-H.; Fetics, B.; Nevo, E.; Rochitte, C.E.; Chiou, K.-R.; Ding, P.-A.; Kawaguchi, M.; Kass, D.A. Noninvasive single-beat determination of left ventricular end-systolic elastance in humans. J. Am. Coll. Cardiol. 2001, 38, 2028–2034. [Google Scholar] [CrossRef]
- Oberhoffer, F.S.; Abdul-Khaliq, H.; Jung, A.-M.; Rohrer, T.R.; Abd El Rahman, M. Left ventricular remodelling among Turner syndrome patients: Insights from non-invasive 3D echocardiography-derived pressure-volume loop analysis. Clin. Res. Cardiol. 2020, 109, 892–903. [Google Scholar] [CrossRef]
- Mandilaras, G.; Li, P.; Dalla-Pozza, R.; Haas, N.A.; Oberhoffer, F.S. Energy Drinks and Their Acute Effects on Heart Rhythm and Electrocardiographic Time Intervals in Healthy Children and Teenagers: A Randomized Trial. Cells 2022, 11, 498. [Google Scholar] [CrossRef]
- Li, P.; Mandilaras, G.; Jakob, A.; Dalla-Pozza, R.; Haas, N.A.; Oberhoffer, F.S. Energy Drinks and Their Acute Effects on Arterial Stiffness in Healthy Children and Teenagers: A Randomized Trial. JCM 2022, 11, 2087. [Google Scholar] [CrossRef]
- Scientific Opinion on the safety of caffeine. EFS2 2015, 13, 425. [CrossRef]
- Shah, S.A.; Szeto, A.H.; Farewell, R.; Shek, A.; Fan, D.; Quach, K.N.; Bhattacharyya, M.; Elmiari, J.; Chan, W.; O’Dell, K.; et al. Impact of High Volume Energy Drink Consumption on Electrocardiographic and Blood Pressure Parameters: A Randomized Trial. J. Am. Heart Assoc. 2019, 8, e011318. [Google Scholar] [CrossRef]
- Lavall, D.; Reil, J.-C.; Segura Schmitz, L.; Mehrer, M.; Schirmer, S.H.; Böhm, M.; Laufs, U. Early Hemodynamic Improvement after Percutaneous Mitral Valve Repair Evaluated by Noninvasive Pressure-Volume Analysis. J. Am. Soc. Echocardiogr. 2016, 29, 888–898. [Google Scholar] [CrossRef]
- Kelly, R.P.; Ting, C.T.; Yang, T.M.; Liu, C.P.; Maughan, W.L.; Chang, M.S.; Kass, D.A. Effective arterial elastance as index of arterial vascular load in humans. Circulation 1992, 86, 513–521. [Google Scholar] [CrossRef]
- Antonini-Canterin, F.; Poli, S.; Vriz, O.; Pavan, D.; Di Bello, V.; Nicolosi, G.L. The Ventricular-Arterial Coupling: From Basic Pathophysiology to Clinical Application in the Echocardiography Laboratory. J. Cardiovasc. Echogr. 2013, 23, 91–95. [Google Scholar] [CrossRef]
- Ky, B.; French, B.; May Khan, A.; Plappert, T.; Wang, A.; Chirinos, J.A.; Fang, J.C.; Sweitzer, N.K.; Borlaug, B.A.; Kass, D.A.; et al. Ventricular-arterial coupling, remodeling, and prognosis in chronic heart failure. J. Am. Coll. Cardiol. 2013, 62, 1165–1172. [Google Scholar] [CrossRef] [PubMed]
- Kameyama, T.; Asanoi, H.; Ishizaka, S.; Yamanishi, K.; Fujita, M.; Sasayama, S. Energy conversion efficiency in human left ventricle. Circulation 1992, 85, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Seemann, F.; Arvidsson, P.; Nordlund, D.; Kopic, S.; Carlsson, M.; Arheden, H.; Heiberg, E. Noninvasive Quantification of Pressure-Volume Loops From Brachial Pressure and Cardiovascular Magnetic Resonance. Circ. Cardiovasc. Imaging 2019, 12, e008493. [Google Scholar] [CrossRef]
- Obokata, M.; Kurosawa, K.; Ishida, H.; Ito, K.; Ogawa, T.; Ando, Y.; Kurabayashi, M.; Negishi, K. Echocardiography-based pressure-volume loop assessment in the evaluation for the effects of indoxyl sulfate on cardiovascular function. J. Echocardiogr. 2019, 17, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Suga, H.; Goto, Y.; Futaki, S.; Kawaguchi, O.; Yaku, H.; Hata, K.; Takasago, T. Systolic pressure-volume area (PVA) as the energy of contraction in Starling’s law of the heart. Heart Vessels 1991, 6, 65–70. [Google Scholar] [CrossRef]
- Wilson, A.J.; Wang, V.Y.; Sands, G.B.; Young, A.A.; Nash, M.P.; LeGrice, I.J. Increased cardiac work provides a link between systemic hypertension and heart failure. Physiol. Rep. 2017, 5, e13104. [Google Scholar] [CrossRef]
- Higgins, J.P.; Tuttle, T.D.; Higgins, C.L. Energy beverages: Content and safety. Mayo Clin. Proc. 2010, 85, 1033–1041. [Google Scholar] [CrossRef]
- Schaefer, S.; Taylor, A.L.; Lee, H.R.; Niggemann, E.H.; Levine, B.D.; Popma, J.J.; Mitchell, J.H.; Hillis, L.D. Effect of increasing heart rate on left ventricular performance in patients with normal cardiac function. Am. J. Cardiol. 1988, 61, 617–620. [Google Scholar] [CrossRef]
- Takaoka, H.; Takeuchi, M.; Odake, M.; Hayashi, Y.; Hata, K.; Mori, M.; Yokoyama, M. Comparison of hemodynamic determinants for myocardial oxygen consumption under different contractile states in human ventricle. Circulation 1993, 87, 59–69. [Google Scholar] [CrossRef]
- Available online: https://www.lrt.lt/en/news-in-english/19/43504/lithuania-bans-sale-of-energy-drinks-to-minors (accessed on 16 September 2022).
- Available online: https://eng.lsm.lv/article/society/society/latvia-bans-energy-drink-sales-to-minors.a165212/ (accessed on 16 September 2022).
- Renda, G.; Zimarino, M.; Antonucci, I.; Tatasciore, A.; Ruggieri, B.; Bucciarelli, T.; Prontera, T.; Stuppia, L.; de Caterina, R. Genetic determinants of blood pressure responses to caffeine drinking. Am. J. Clin. Nutr. 2012, 95, 241–248. [Google Scholar] [CrossRef]
- Nehlig, A. Interindividual Differences in Caffeine Metabolism and Factors Driving Caffeine Consumption. Pharmacol. Rev. 2018, 70, 384–411. [Google Scholar] [CrossRef] [PubMed]
- Grothues, F.; Smith, G.C.; Moon, J.C.C.; Bellenger, N.G.; Collins, P.; Klein, H.U.; Pennell, D.J. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am. J. Cardiol. 2002, 90, 29–34. [Google Scholar] [CrossRef]
- Nishikage, T.; Nakai, H.; Mor-Avi, V.; Lang, R.M.; Salgo, I.S.; Settlemier, S.H.; Husson, S.; Takeuchi, M. Quantitative assessment of left ventricular volume and ejection fraction using two-dimensional speckle tracking echocardiography. Eur. J. Echocardiogr. 2009, 10, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.M.; Butts, R.J.; Taylor, C.L.; Bandisode, V.M.; Chessa, K.S.; Hlavacek, A.M.; Shirali, G.S.; Baker, G.H. Validation of Noninvasive Measures of Left Ventricular Mechanics in Children: A Simultaneous Echocardiographic and Conductance Catheterization Study. J. Am. Soc. Echocardiogr. 2016, 29, 640–647. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total |
|---|---|
| Age, years (mean ± standard deviation) | 14.90 ± 2.27 |
| Sex, n (%) | |
| Male | 13 (54.17) |
| Female | 11 (45.83) |
| Weight Classification, n (%) | |
| Normal weight | 21 (87.50) |
| Overweight | 3 (12.50) |
| Obese | 0 (0) |
| Caffeine Consumption Behavior, n (%) a | |
| Rarely | 15 (62.5) |
| Occasionally | 3 (12.5) |
| Frequently | 4 (16.67) |
| Daily | 2 (8.33) |
| Energy Drink Consumption Behavior, n (%) b | |
| Never | 10 (41.67) |
| Rarely | 11 (45.83) |
| Occasionally | 1 (4.17) |
| Frequently | 2 (8.33) |
| Daily | 0 (0) |
| Parameters | Energy Drink | Placebo | p-Value |
|---|---|---|---|
| EDV (mL) | 88.66 ± 20.47 | 86.83 ± 18.81 | 0.42 |
| ESV (mL) | 46.56 ± 11.82 | 45.70 ± 11.27 | 0.67 |
| SV (mL) | 42.10 ± 11.41 | 41.13 ± 10.81 | 0.61 |
| EF (%) | 47.51 ± 6.47 | 47.21 ± 6.29 | 0.87 |
| Ea (mmHg/mL) | 2.43 (2.09–3.25) | 2.58 (2.12–2.98) | 0.56 |
| Ees(sb) (mmHg/mL) | 3.50 ± 0.93 | 3.63 ± 1.14 | 0.49 |
| Epot (mmHg × mL) | 1545 (1319–1820) | 1442 (1167–1976) | 0.66 |
| SW (mmHg × mL) | 4301 ± 1266 | 4222 ± 1188 | 0.80 |
| PVA (mmHg × mL) | 5892 ± 1680 | 5855 ± 1751 | 0.32 |
| Ea/Ees(sb) | 0.75 (0.67–0.82) | 0.69 (0.64–0.82) | 0.56 |
| CW (mmHg × mL × HR) | 290434 ± 82889 | 288475 ± 75661 | 0.75 |
| WE (%) | 72.77 (70.84–75.04) | 74.27 (70.95–75.82) | 0.71 |
| CE (mmHg) | 139.83 ± 12.59 | 141.91 ± 15.99 | 0.49 |
| Parameters | Energy Drink | Placebo | p-Value |
|---|---|---|---|
| EDV (mL) | 87.93 ± 19.12 | 88.95 ± 19.78 | 0.44 |
| ESV (mL) | 44.94 ± 11.54 | 45.51 ± 11.89 | 0.52 |
| SV (mL) | 42.99 ± 10.51 | 43.43 ± 10.74 | 0.68 |
| EF (%) | 48.98 ± 6.36 | 48.84 ± 6.31 | 0.86 |
| Ea (mmHg/mL) | 2.56 ± 0.62 | 2.47 ± 0.67 | 0.19 |
| Ees(sb) (mmHg/mL) | 3.66 ± 1.00 | 3.47 ± 0.98 | 0.05 |
| Epot (mmHg × mL) | 1624 ± 633 | 1630 ± 671 | 0.88 |
| SW (mmHg × mL) | 4501 ± 1266 | 4413 ± 1262 | 0.40 |
| PVA (mmHg × mL) | 6124 ± 1796 | 6043 ± 1821 | 0.53 |
| Parameters | Energy Drink | Placebo | p-Value |
|---|---|---|---|
| Ea/Ees(sb) | |||
| Time 0 | 0.75 (0.67–0.82) | 0.69 (0.64–0.82) | 0.56 |
| Time 30 | 0.66 (0.64–0.70) | 0.66 (0.61–0.75) | 1.00 |
| Time 60 | 0.66 (0.62–0.76) | 0.69 (0.61–0.79) | 0.87 |
| Time 120 | 0.65 (0.61–0.74) | 0.67 (0.63–0.80) | 0.13 |
| Time 240 | 0.67 (0.62–0.79) | 0.71 (0.62–0.75) | 0.56 |
| CW (mmHg × mL × HR) | 307,145 ± 98,350 | 304,361 ± 97,313 | 0.69 |
| WE (%) | |||
| Time 0 | 72.77 (70.84–75.04) | 74.27 (70.95–75.82) | 0.71 |
| Time 30 | 75.12 (74.07–75.84) | 75.19 (72.70–76.52) | 0.66 |
| Time 60 | 75.08 (72.58–76.33) | 74.28 (71.59–76.50) | 0.79 |
| Time 120 | 75.49 (73.07–76.54) | 74.97 (71.38–76.14) | 0.15 |
| Time 240 | 75.05 (71.68–76.22) | 73.85 (72.80–76.49) | 0.63 |
| CE (mmHg) | |||
| Time 0 | 139.83 ± 12.59 | 141.91 ± 15.99 | 0.49 |
| Time 30 | 141.86 ± 11.98 | 137.72 ± 12.38 | 0.13 |
| Time 60 | 135.89 (133.12–154.15) | 136.15 (129.31–146.06) | 0.14 |
| Time 120 | 137.23 (129.91–146.89) | 133.56 (122.90–145.29) | 0.21 |
| Time 240 | 140.72 (133.21–149.73) | 135.60 (124.78–140.33) | <0.01 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oberhoffer, F.S.; Li, P.; Jakob, A.; Dalla-Pozza, R.; Haas, N.A.; Mandilaras, G. Energy Drinks Decrease Left Ventricular Efficiency in Healthy Children and Teenagers: A Randomized Trial. Sensors 2022, 22, 7209. https://doi.org/10.3390/s22197209
Oberhoffer FS, Li P, Jakob A, Dalla-Pozza R, Haas NA, Mandilaras G. Energy Drinks Decrease Left Ventricular Efficiency in Healthy Children and Teenagers: A Randomized Trial. Sensors. 2022; 22(19):7209. https://doi.org/10.3390/s22197209
Chicago/Turabian StyleOberhoffer, Felix Sebastian, Pengzhu Li, André Jakob, Robert Dalla-Pozza, Nikolaus Alexander Haas, and Guido Mandilaras. 2022. "Energy Drinks Decrease Left Ventricular Efficiency in Healthy Children and Teenagers: A Randomized Trial" Sensors 22, no. 19: 7209. https://doi.org/10.3390/s22197209
APA StyleOberhoffer, F. S., Li, P., Jakob, A., Dalla-Pozza, R., Haas, N. A., & Mandilaras, G. (2022). Energy Drinks Decrease Left Ventricular Efficiency in Healthy Children and Teenagers: A Randomized Trial. Sensors, 22(19), 7209. https://doi.org/10.3390/s22197209






