Digital Biomarker Representing Frailty Phenotypes: The Use of Machine Learning and Sensor-Based Sit-to-Stand Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Experimental Protocols
2.2. Sensor Data Processing and Feature Extraction
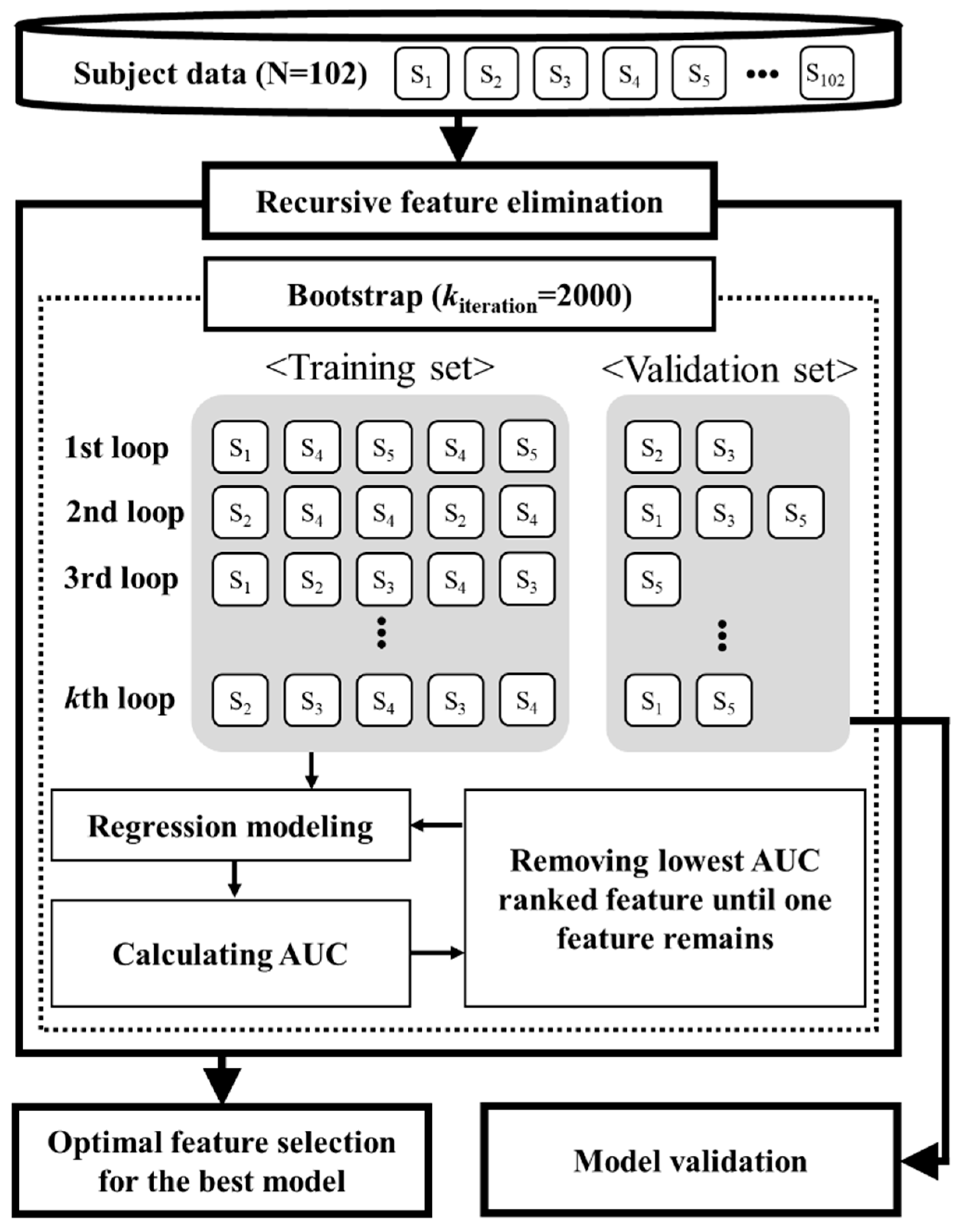
2.3. Optimal Feature Selection and Evaluation of Frailty Modeling
3. Results
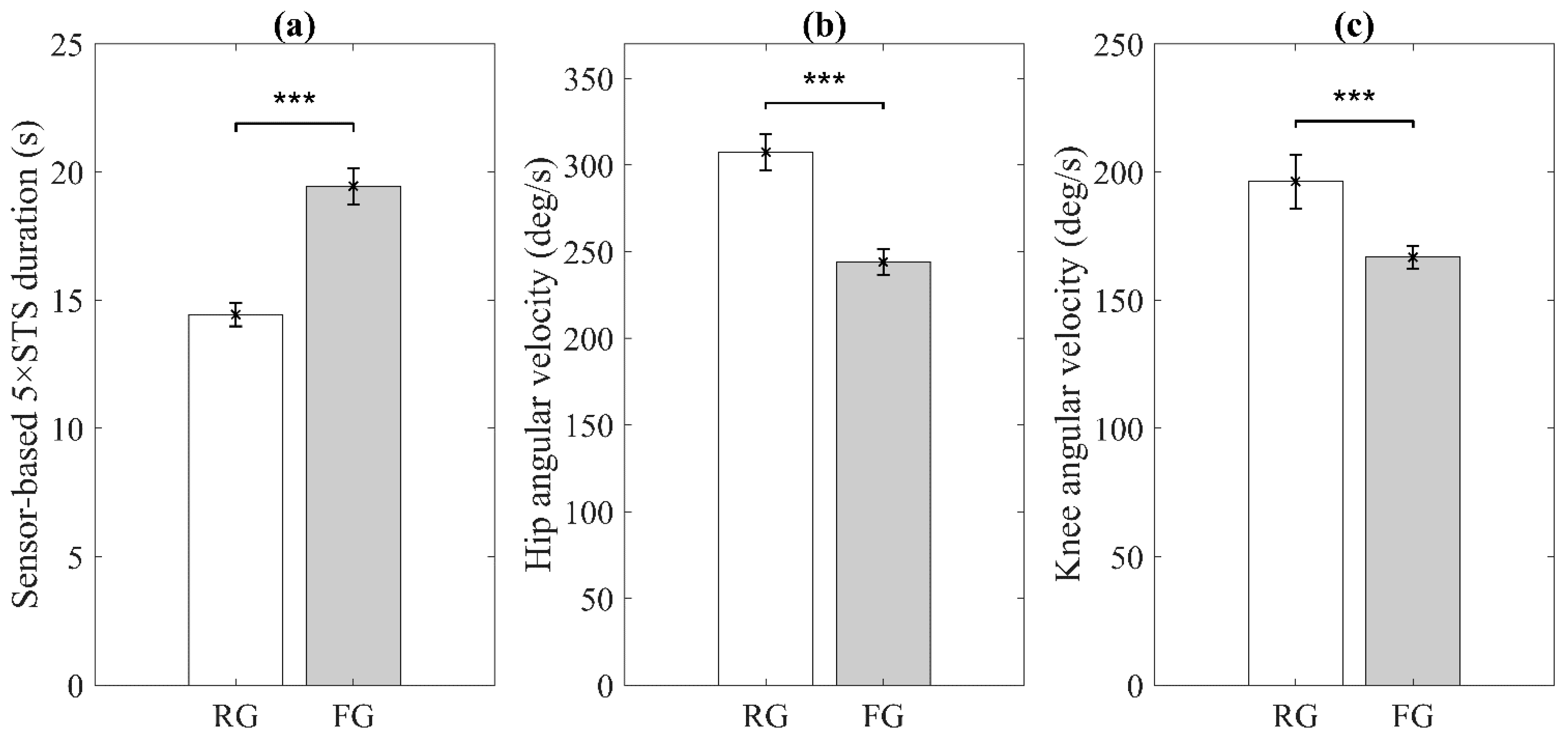
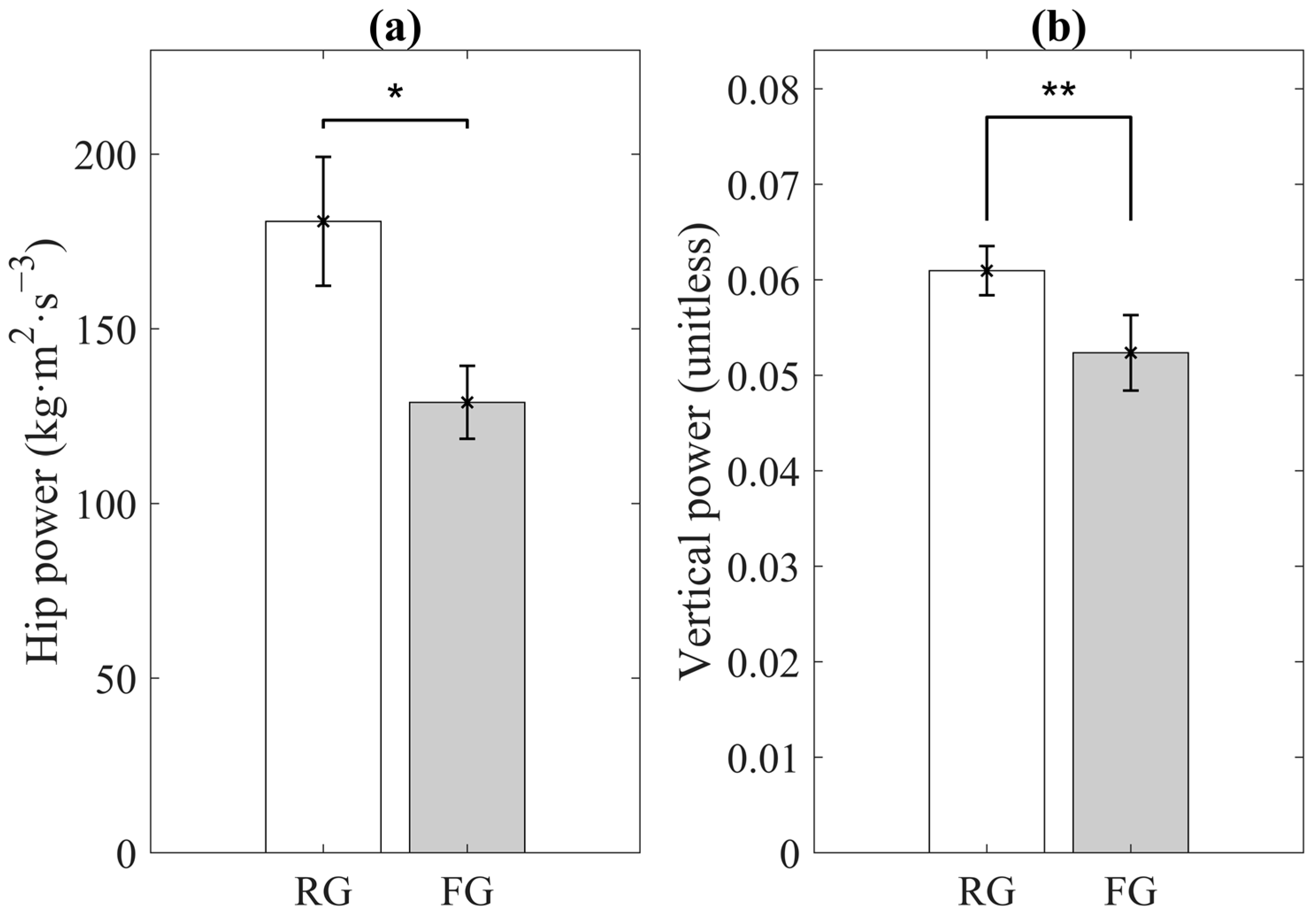
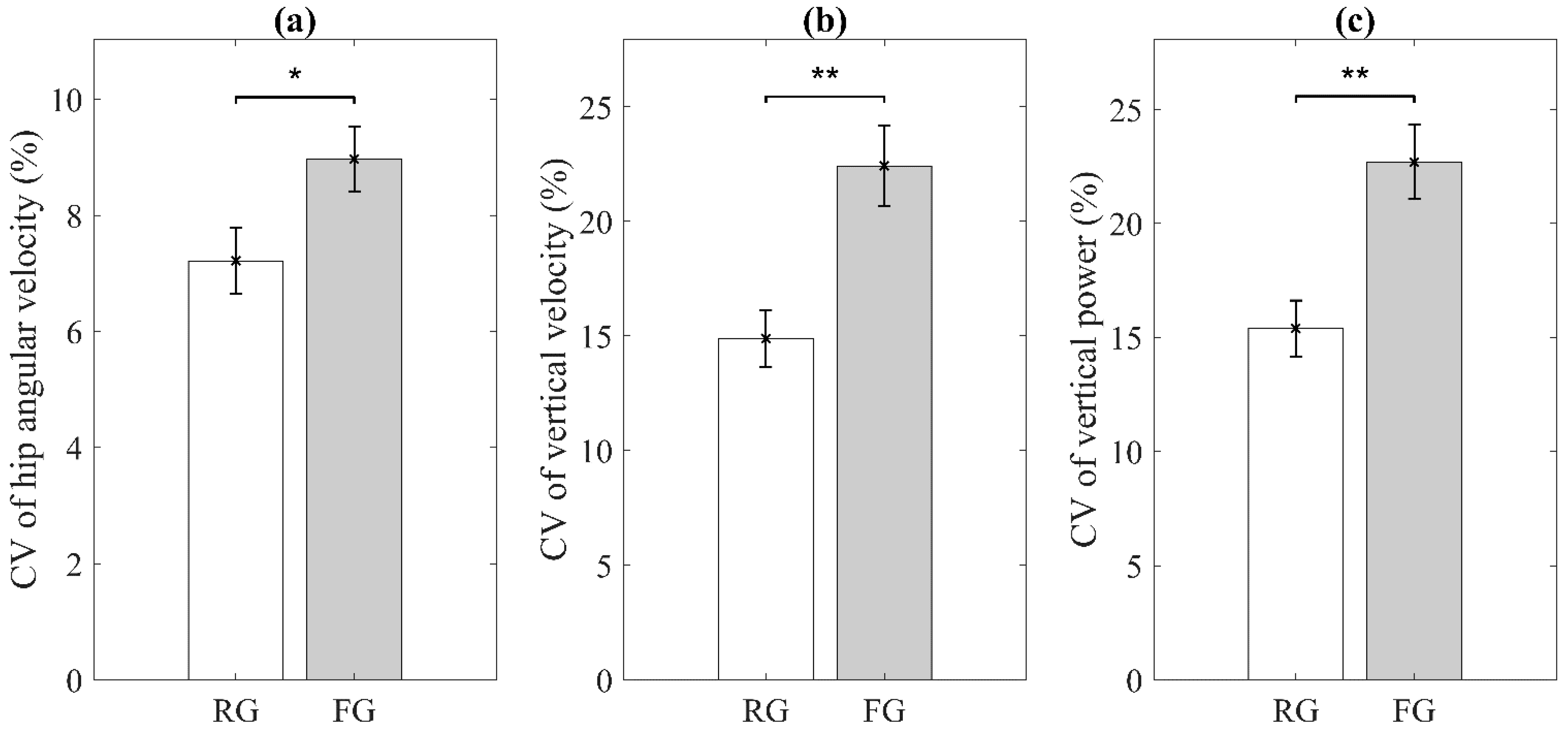
3.1. Significant Sensor-Derived Features
3.2. Optimal Feature Selection and Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 28 March 2021).
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Ofori-Asenso, R.; Chin, K.L.; Mazidi, M.; Zomer, E.; Ilomaki, J.; Zullo, A.R.; Gasevic, D.; Ademi, Z.; Korhonen, M.J.; LoGiudice, D.; et al. Global incidence of frailty and prefrailty among community-dwelling older adults: A systematic review and meta-analysis. JAMA Netw. Open 2019, 2, e198398. [Google Scholar] [CrossRef]
- Harrison, J.K.; Clegg, A.; Conroy, S.P.; Young, J. Managing frailty as a long-term condition. Age Ageing 2015, 44, 732–735. [Google Scholar] [CrossRef]
- Koller, K.; Rockwood, K. Frailty in older adults: Implications for end-of-life care. Clevel. Clin. J. Med. 2013, 80, 168–174. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef]
- Puts, M.T.E.; Toubasi, S.; Andrew, M.K.; Ashe, M.C.; Ploeg, J.; Atkinson, E.; Ayala, A.P.; Roy, A.; Rodríguez Monforte, M.; Bergman, H.; et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: A scoping review of the literature and international policies. Age Ageing 2017, 46, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Walston, J.; Buta, B.; Xue, Q.L. Frailty screening and interventions: Considerations for clinical practice. Clin. Geriatr. Med. 2018, 34, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Santos-Eggimann, B.; Sirven, N. Screening for frailty: Older populations and older individuals. Public Health Rev. 2016, 37, 7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Dent, E.; Kowal, P.; Hoogendijk, E.O. Frailty measurement in research and clinical practice: A review. Eur. J. Intern. Med. 2016, 31, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Faller, J.W.; Pereira, D.D.N.; de Souza, S.; Nampo, F.K.; Orlandi, F.S.; Matumoto, S. Instruments for the detection of frailty syndrome in older adults: A systematic review. PLoS ONE 2019, 14, e0216166. [Google Scholar] [CrossRef]
- De Lepeleire, J.; Degryse, J.; Illiffe, S.; Mann, E.; Buntinx, F. Family physicians need easy instruments for frailty. Age Ageing 2008, 37, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Bian, C.; Ye, B.; Chu, C.; McGilton, K.; Mihailidis, A. Technology for home-based frailty assessment and prediction: A systematic review. Gerontechnology 2020, 19, 1–13. [Google Scholar] [CrossRef]
- Park, C.; Sharafkhaneh, A.; Bryant, M.S.; Nguyen, C.; Torres, I.; Najafi, B. Toward remote assessment of physical frailty using sensor-based sit-to-stand test. J. Surg. Res. 2021, 263. in press. [Google Scholar] [CrossRef]
- Bohannon, R.W. Test-retest reliability of the five-repetition sit-to-stand test: A systematic review of the literature involving adults. J. Strength Cond. Res. 2011, 25, 3205–3207. [Google Scholar] [CrossRef]
- Teo, T.W.L.; Mong, Y.; Ng, S.S.M. The repetitive five-times-sit-to-stand test: Its reliability in older adults. Int. J. Ther. Rehabil. 2014, 20, 122–130. [Google Scholar] [CrossRef]
- Wallmann, H.W.; Evans, N.S.; Day, C.; Neellym, K.R. Interrater reliability of the five-times-sit-to-stand test. Home Health Care Manag. Pract. 2013, 25, 13–17. [Google Scholar] [CrossRef]
- Thiede, R.; Toosizadeh, N.; Mills, J.L.; Zaky, M.; Mohler, J.; Najafi, B. Gait and balance assessments as early indicators of frailty in patients with known peripheral artery disease. Clin. Biomech. 2016, 32, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower extremity function and subsequent disability: Consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M221–M231. [Google Scholar] [CrossRef]
- de Leva, P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. J. Biomech. 1996, 29, 1223–1230. [Google Scholar] [CrossRef]
- Lee, H.; Joseph, B.; Enriquez, A.; Najafi, B. Toward using a smartwatch to monitor frailty in a hospital setting: Using a single wrist-wearable sensor to assess frailty in bedbound inpatients. Gerontology 2018, 64, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W. Making bootstrap statistical inferences: A tutorial. Res. Q. Exerc. Sport 1997, 68, 44–55. [Google Scholar] [CrossRef]
- Efron, B.; Tibshirani, R.J. An Introduction to the Bootstrap; Chapman & Hall: New York, NY, USA; London, UK, 1993. [Google Scholar]
- Bradley, A.P. The use of the area under the ROC curve in the evaluation of machine learning algorithms. Pattern Recognit. 1997, 30, 1145–1159. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2010, 5, 1315–1316. [Google Scholar] [CrossRef]
- Millor, N.; Lecumberri, P.; Gomez, M.; Martinez-Ramirez, A.; Izquierdo, M. An evaluation of the 30-s chair stand test in older adults: Frailty detection based on kinematic parameters from a single inertial unit. J. Neuroeng. Rehabil. 2013, 10, 86. [Google Scholar] [CrossRef]
- van Lummel, R.C.; Walgaard, S.; Maier, A.B.; Ainsworth, E.; Beek, P.J.; van Dieën, J.H. The instrumented sit-to-stand test (iSTS) has greater clinical relevance than the manually recorded sit-to-stand test in older adults. PLoS ONE 2016, 11, e0157968. [Google Scholar] [CrossRef]
- Millor, N.; Lecumberri, P.; Gomez, M.; Martinez, A.; Martinikorena, J.; Rodriguez-Manas, L.; Garcia-Garcia, F.J.; Izquierdo, M. Gait Velocity and Chair Sit-Stand-Sit Performance Improves Current Frailty-Status Identification. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 2018–2025. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Ramírez-Vélez, R.; López Sáez de Asteasu, M.; Morley, J.E.; Cano-Gutierrez, C.A.; Izquierdo, M. Performance of the Short Physical Performance Battery in identifying the frailty phenotype and predicting geriatric syndromes in community-dwelling elderly. J. Nutr. Health Aging 2021, 25, 209–217. [Google Scholar] [CrossRef]
- Kojima, G.; Liljas, A.E.M.; Iliffe, S. Frailty syndrome: Implications and challenges for health care policy. Risk Manag. Healthc. Policy 2019, 12, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Cegri, F.; Orfila, F.; Abellana, R.M.; Pastor-Valero, M. The impact of frailty on admission to home care services and nursing homes: Eight-year follow-up of a community-dwelling, older adult, Spanish cohort. BMC Geriatr. 2020, 20, 281. [Google Scholar] [CrossRef] [PubMed]
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. JAMIA 2020, 27, 1132–1135. [Google Scholar] [CrossRef] [PubMed]

| No./Total No. (%) by Group | p-Value | ||
|---|---|---|---|
| RG (n = 42) | FG (n = 60) | ||
| Age, years | 74.79 ± 6.64 | 76.57 ± 8.00 | 0.085 |
| Female, n (%) | 34/42 (81.0) | 39/60 (65.0) | 0.079 |
| Height, cm | 162.09 ± 7.34 | 164.90 ± 10.77 | 0.230 |
| Weight, kg | 66.77 ± 12.21 | 78.61 ± 19.95 | 0.001 * |
| BMI, kg/m2 | 25.40 ± 4.23 | 28.70 ± 5.79 | <0.0001 * |
| Rank | Sensor-Driven Features | Phenotype | Sensor Configuration |
|---|---|---|---|
| 1 | Mean of hip angular velocity range | Slowness | Trunk/Thigh |
| 2 | Mean of vertical power range | Weakness | Trunk |
| 3 | Coefficient of Variation (CV) of vertical power range | Exhaustion | Trunk |
| 4 | CV of vertical velocity range | Exhaustion | Trunk |
| 5 | Mean of hip power range | Weakness | Trunk/Thigh |
| 6 | Sensor-based 5×STS duration | Slowness | Trunk/Thigh/Shank |
| 7 | Mean of knee angular velocity range | Slowness | Thigh/Shank |
| 8 | CV of hip angular velocity range | Exhaustion | Trunk/Thigh |
| Validation Metric | Mean | 95% Confidence Interval |
|---|---|---|
| AUC (%) | 82.18 | 81.93 to 82.43 |
| Sensitivity (%) | 79.37 | 78.92 to 79.84 |
| Specificity (%) | 67.20 | 66.64 to 67.76 |
| Accuracy (%) | 73.91 | 73.63 to 74.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.; Mishra, R.; Sharafkhaneh, A.; Bryant, M.S.; Nguyen, C.; Torres, I.; Naik, A.D.; Najafi, B. Digital Biomarker Representing Frailty Phenotypes: The Use of Machine Learning and Sensor-Based Sit-to-Stand Test. Sensors 2021, 21, 3258. https://doi.org/10.3390/s21093258
Park C, Mishra R, Sharafkhaneh A, Bryant MS, Nguyen C, Torres I, Naik AD, Najafi B. Digital Biomarker Representing Frailty Phenotypes: The Use of Machine Learning and Sensor-Based Sit-to-Stand Test. Sensors. 2021; 21(9):3258. https://doi.org/10.3390/s21093258
Chicago/Turabian StylePark, Catherine, Ramkinker Mishra, Amir Sharafkhaneh, Mon S. Bryant, Christina Nguyen, Ilse Torres, Aanand D. Naik, and Bijan Najafi. 2021. "Digital Biomarker Representing Frailty Phenotypes: The Use of Machine Learning and Sensor-Based Sit-to-Stand Test" Sensors 21, no. 9: 3258. https://doi.org/10.3390/s21093258
APA StylePark, C., Mishra, R., Sharafkhaneh, A., Bryant, M. S., Nguyen, C., Torres, I., Naik, A. D., & Najafi, B. (2021). Digital Biomarker Representing Frailty Phenotypes: The Use of Machine Learning and Sensor-Based Sit-to-Stand Test. Sensors, 21(9), 3258. https://doi.org/10.3390/s21093258









