Non-Technical Skill Assessment and Mental Load Evaluation in Robot-Assisted Minimally Invasive Surgery
Abstract
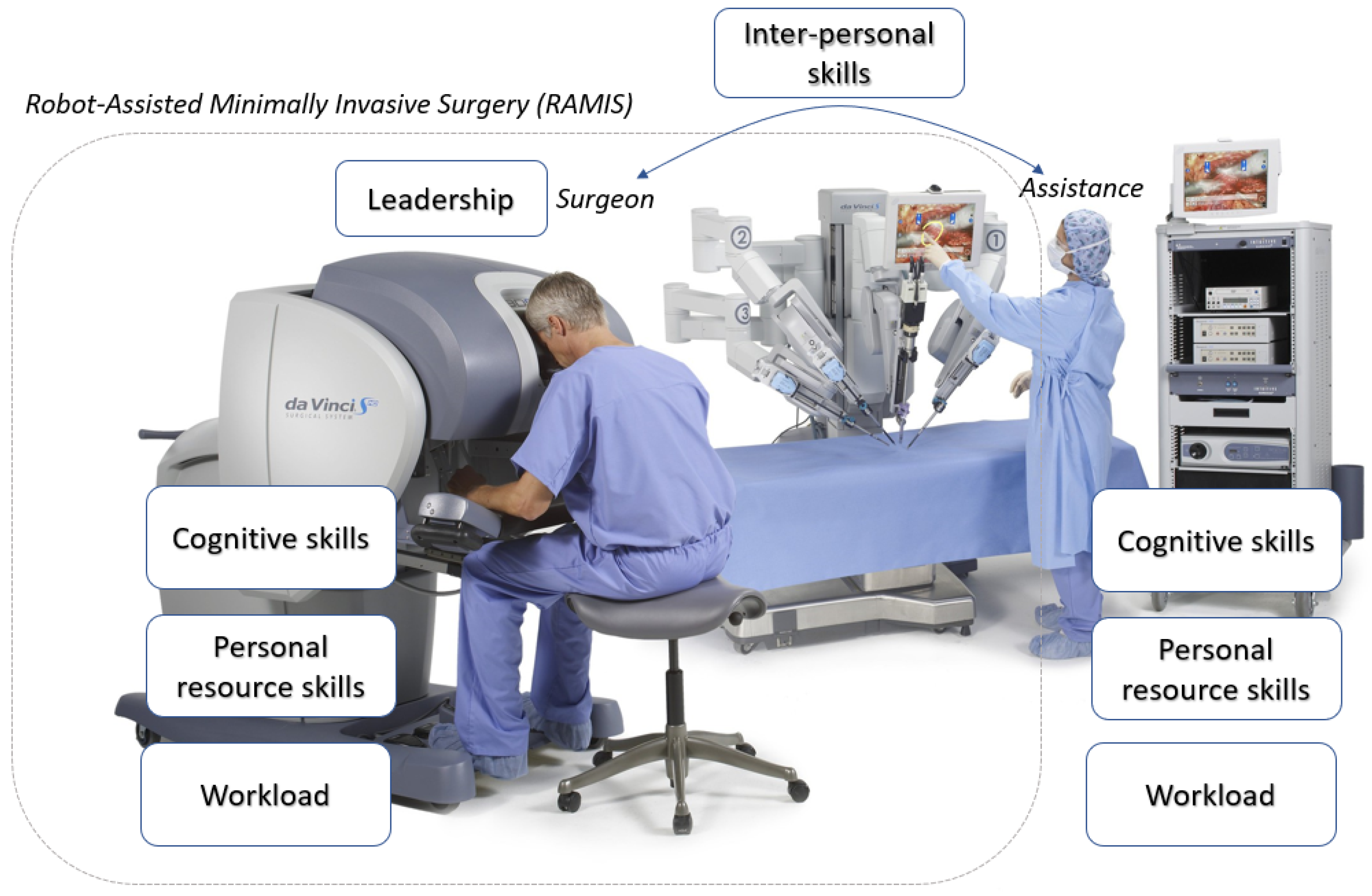
1. Introduction
- self-rating questionnaires,
- expert-based scoring and
- automated (sensor-based) skill assessment.
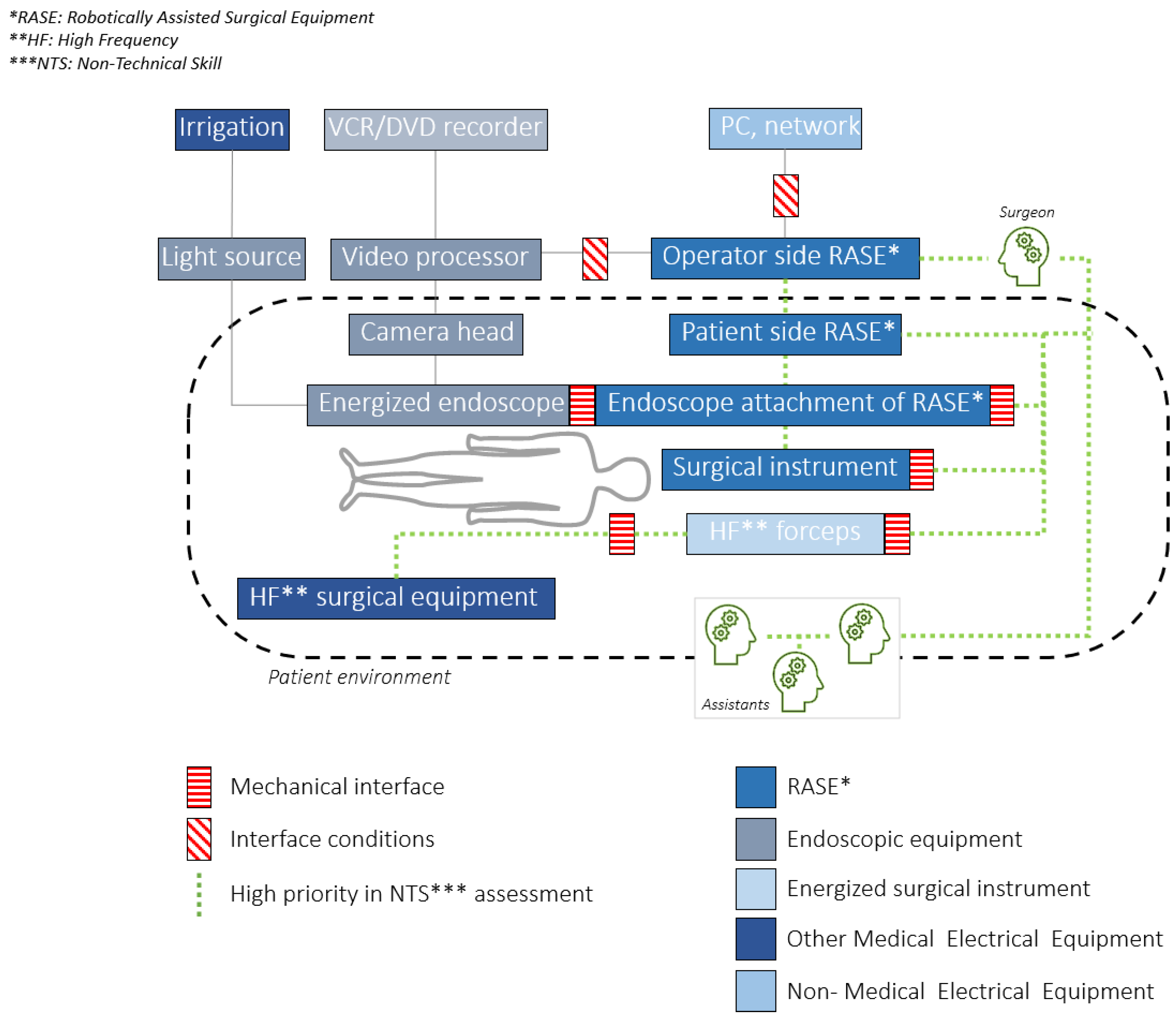
- Robotically Assisted Surgical Equipment—RASE: ‘Medical electrical equipment that incorporates programmable electrical medical system actuated mechanism intended to facilitate the placement or manipulation of a robotic surgical instrument’ (the ISO 8373 standard strictly defines the term "robot" in the ISO domain, therefore the working group decided to use the more inclusive "Robotically Assisted" expression within RAMIS, while it is less commonly used in the domain).
- Robotic surgical instrument: ‘Invasive device with applied part, intended to be manipulated by RASE to perform tasks in surgery’.
- High frequency (HF): ‘less than 5 MHz and generally greater than 200 kHz’.
- HF surgical equipment: ‘medical electrical equipment which generates HF currents intended for the performance of surgical tasks, such as the cutting or coagulation of biological tissue by means of these HF currents’.
- Interface conditions: conditions that shall be fulfilled to achieve basic safety for any functional connection between RAMIS and other medical electrical equipment or non-medical electrical equipment in the robotic surgery configuration.
- Mechanical interface: mounting surface on RAMIS that allows for attachment of detachable accessories, components or parts that are mechanically manipulated by the RAMIS.
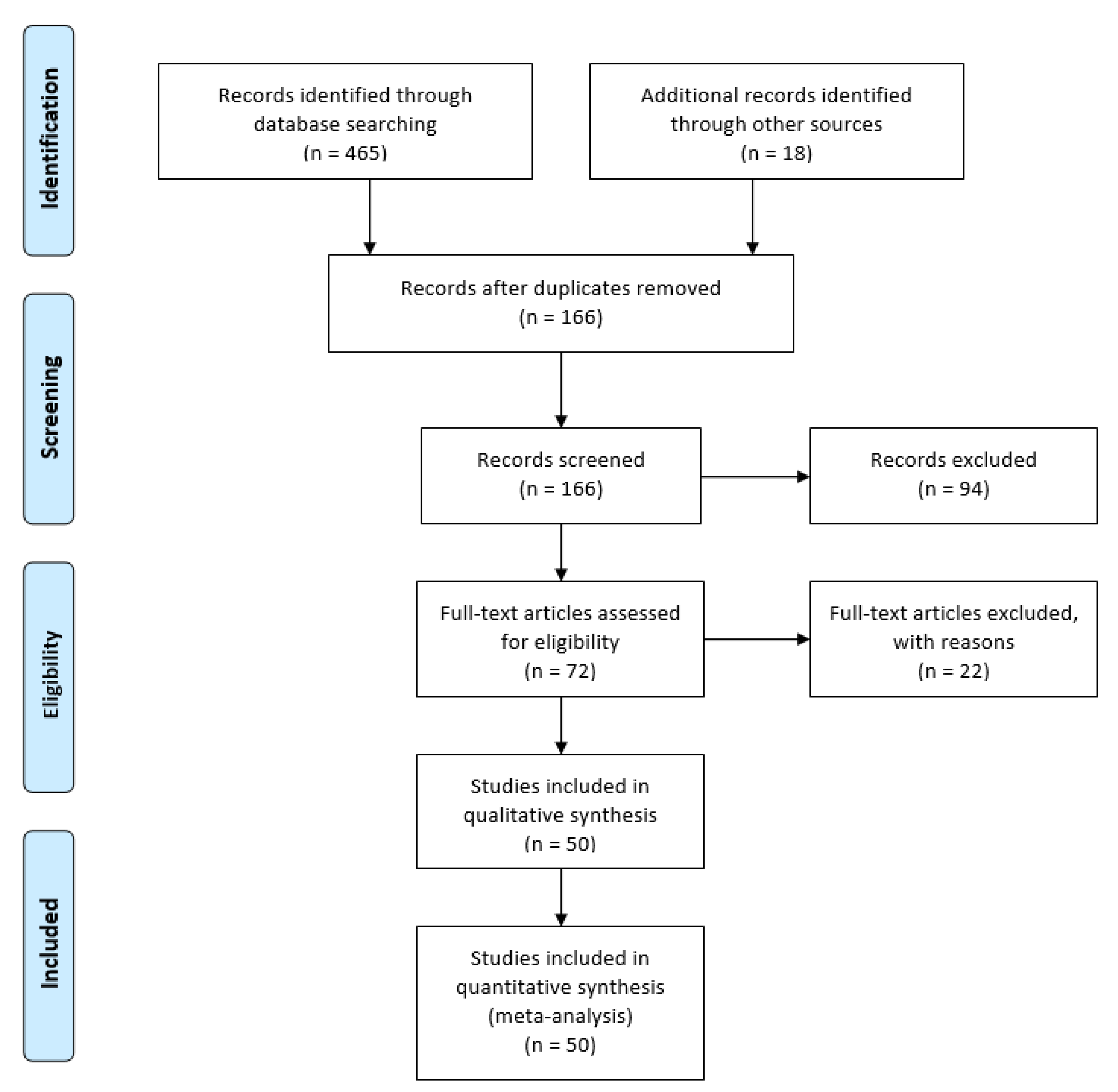
2. Materials and Methods
- High: high-level of confidence in the effects;
- Moderate: confidence in the effects may change with future research findings;
- Low: confidence in the effects is very likely to change with future research findings;
- Very low: uncertainty about the effects.
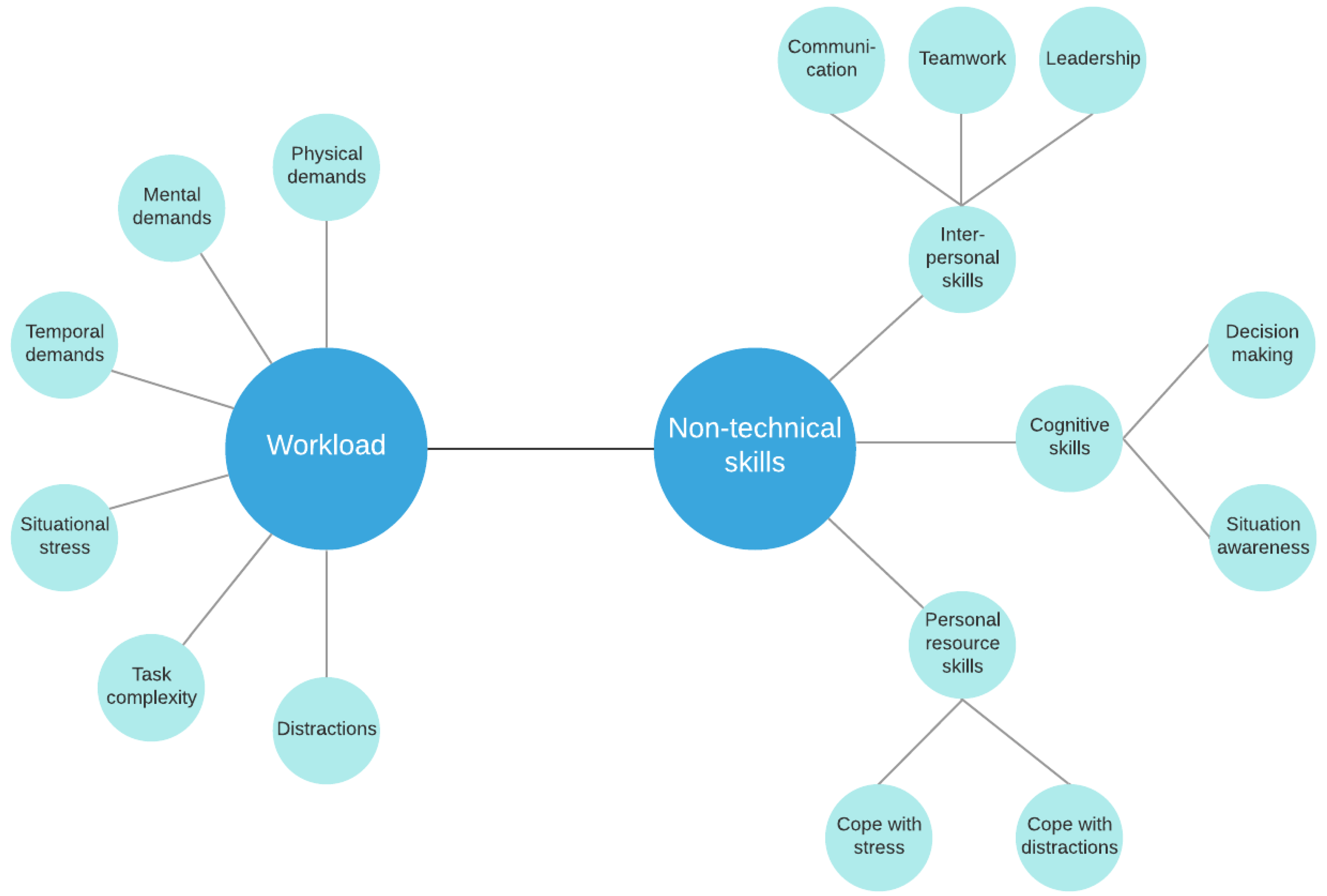
3. Technical Approaches for Non-Technical Skill and Mental Workload Assessment in RAMIS
3.1. Mental Workload Assessment—Self-Rating Techniques
3.2. Non-Technical Skill Assessment—Expert Rating
3.3. Automated Non-Technical Skill and Mental Workload Assessment in RAMIS
- simple HR;
- Heart Rate Variability (HRV);
- mean square of successive differences between consecutive heartbeats (MSSD);
- average heart rate (HRA).
- magnetic pose trackers;
- EEG;
- ECG;
- fNIRS;
- skin conductance sensor;
- electromyograph (EMG);
- eye-gaze tracker;
- nose temperature and dryness sensor;
- heart rate monitor.
- position sensors (encoders);
- gyroscopes;
- 2D/3D endoscopic camera.
- force sensors (strain gauges, capacitive sensors, piezoelectric sensors, optical sensors);
- tool position sensing (optical, electromagnetic);
- master/surgeon arm position sensing (external);
- wearable eyeglasses (Oculus Rift, Google Glass);
- tool thermal sensor;
- pressure sensors;
- camera (RGBD, external);
- communication (RF sensors);
- speech (microspeaker);
- sound (microphones).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Haidegger, T.; Sándor, J.; Benyó, Z. Surgery in Space: The Future of Robotic Telesurgery. Surg. Endosc. 2011, 25, 681–690. [Google Scholar] [CrossRef] [PubMed]
- Ochsner, J.L. Minimally Invasive Surgical Procedures. Ochsner J. 2000, 2, 135–136. [Google Scholar]
- Haidegger, T. Autonomy for Surgical Robots: Concepts and Paradigms. IEEE Trans. Med. Robot. Bionics 2019, 1, 65–76. [Google Scholar] [CrossRef]
- Haidegger, T. Probabilistic Method to Improve the Accuracy of Computer-Integrated Surgical Systems. Acta Polytech. Hung. 2019, 16, 119–140. [Google Scholar] [CrossRef]
- Hernandez, J.D.; Bann, S.D.; Munz, Y.; Moorthy, K.; Datta, V.; Martin, S.; Dosis, A.; Bello, F.; Darzi, A.; Rockall, T. Qualitative and Quantitative Analysis of the Learning Curve of a Simulated Surgical Task on the Da Vinci System. Surg. Endosc. Other Interv. Tech. 2004, 18, 372–378. [Google Scholar] [CrossRef]
- Gomes, P. Surgical Robotics: Reviewing the Past, Analysing the Present, Imagining the Future. Robot. Comput. Integr. Manuf. 2011, 27, 261–266. [Google Scholar] [CrossRef]
- Heemskerk, J.; Zandbergen, H.R.; Keet, S.W.M.; Martijnse, I.; van Montfort, G.; Peters, R.J.A.; Svircevic, V.; Bouwman, R.A.; Baeten, C.G.M.I.; Bouvy, N.D. Relax, It’s Just Laparoscopy! A Prospective Randomized Trial on Heart Rate Variability of the Surgeon in Robot-Assisted versus Conventional Laparoscopic Cholecystectomy. Dig. Surg. 2014, 31, 225–232. [Google Scholar] [CrossRef]
- Stefanidis, D.; Wang, F.; Korndorffer, J.R.; Dunne, J.B.; Scott, D.J. Robotic Assistance Improves Intracorporeal Suturing Performance and Safety in the Operating Room While Decreasing Operator Workload. Surg. Endosc. 2010, 24, 377–382. [Google Scholar] [CrossRef]
- Cleary, K.; Nguyen, C. State of the Art in Surgical Robotics: Clinical Applications and Technology Challenges. Comput. Aided Surg. 2001, 6, 312–328. [Google Scholar] [CrossRef]
- Intuitive|Robotic-Assisted Surgery|Da Vinci Surgical System. Available online: https://www.intuitive.com/en-us (accessed on 22 January 2021).
- Peña, A. The Dreyfus Model of Clinical Problem-Solving Skills Acquisition: A Critical Perspective. Med. Educ. Online 2010, 15. [Google Scholar] [CrossRef]
- Azari, D.; Greenberg, C.; Pugh, C.; Wiegmann, D.; Radwin, R. In Search of Characterizing Surgical Skill. J. Surg. Educ. 2019, 76, 1348–1363. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.; Truong, M.; Perez, M. Comparative Analysis of the Functionality of Simulators of the Da Vinci Surgical Robot. Surg. Endosc. 2015, 29, 972–983. [Google Scholar] [CrossRef] [PubMed]
- Meier, M.; Horton, K.; John, H. Da Vinci© Skills Simulator™: Is an Early Selection of Talented Console Surgeons Possible? J. Robot. Surg. 2016, 10, 289–296. [Google Scholar] [CrossRef]
- Matsuda, T.; Yoshida, K.; Habuchi, T.; Kinoshita, H.; Kanayama, H.O.; Terachi, T. Scientific Skill Assessment of Basic Surgical Dissection and Overall Laparoscopic Performance. J. Endourol. 2017, 31, S25–S29. [Google Scholar] [CrossRef]
- Fard, M.J.; Ameri, S.; Ellis, R.D. Toward Personalized Training and Skill Assessment in Robotic Minimally Invasive Surgery. arXiv 2016, arXiv:1610.07245. [Google Scholar]
- Nagyné Elek, R.; Haidegger, T. Robot-Assisted Minimally Invasive Surgical Skill Assessment—Manual and Automated Platforms. Acta Polytech. Hung. 2019, 16, 141–169. [Google Scholar]
- Hart, S.G. Nasa-Task Load Index (NASA-TLX); 20 Years Later. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2006, 50, 904–908. [Google Scholar] [CrossRef]
- Gibaud, B.; Forestier, G.; Feldmann, C.; Ferrigno, G.; Gonçalves, P.; Haidegger, T.; Julliard, C.; Katić, D.; Kenngott, H.; Maier-Hein, L.; et al. Toward a Standard Ontology of Surgical Process Models. Int. J. Comput. Assist. Radiol. Surg. 2018, 13, 1397–1408. [Google Scholar] [CrossRef] [PubMed]
- Gharagozloo, F.; Patel, V.R.; Giulianotti, P.C.; Poston, R.S.; Gruessner, R.; Meyer, M. Robotic Surgery, Defining and Validating Non-technical Skills Training in Robotics. Springer Nature Switzerland AG 2021, 75–81. [Google Scholar] [CrossRef]
- Sharma, B.; Mishra, A.; Aggarwal, R.; Grantcharov, T.P. Non-Technical Skills Assessment in Surgery. Surg. Oncol. 2011, 20, 169–177. [Google Scholar] [CrossRef]
- Raison, N.; Wood, T.; Brunckhorst, O.; Abe, T.; Ross, T.; Challacombe, B.; Khan, M.S.; Novara, G.; Buffi, N.; Van Der Poel, H.; et al. Development and Validation of a Tool for Non-Technical Skills Evaluation in Robotic Surgery-the ICARS System. Surg. Endosc. 2017, 31, 5403–5410. [Google Scholar] [CrossRef]
- Drexler, D.A.; Takács, A.; Nagy, T.D.; Haidegger, T. Handover Process of Autonomous Vehicles-technology and application challenges. Acta Polytech. Hung. 2019, 16.9, 235–255. [Google Scholar] [CrossRef]
- Yule, S.; Paterson-Brown, S. Surgeons’ Non-Technical Skills. Surg. Clin. 2012, 92, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Hull, L.; Arora, S.; Aggarwal, R.; Darzi, A.; Vincent, C.; Sevdalis, N. The Impact of Nontechnical Skills on Technical Performance in Surgery: A Systematic Review. J. Am. Coll. Surg. 2012, 214, 214–230. [Google Scholar] [CrossRef]
- Collins, J.W.; Dell’Oglio, P.; Hung, A.J.; Brook, N.R. The Importance of Technical and Non-Technical Skills in Robotic Surgery Training. Eur. Urol. Focus 2018, 4, 674–676. [Google Scholar] [CrossRef] [PubMed]
- Urban, C.; Galambos, P.; Györök, G.; Haidegger, T. Simulated Medical Ultrasound Trainers A Review of Solutions and Applications. Acta Polytech. Hung. 2018, 15, 111–131. [Google Scholar]
- Collins, J.; Wisz, P. Training in Robotic Surgery, Replicating the Airline Industry. How Far Have We Come? World J. Urol. 2020, 38, 1645–1651. [Google Scholar] [CrossRef]
- Sánchez, R.; Rodríguez, O.; Rosciano, J.; Vegas, L.; Bond, V.; Rojas, A.; Sanchez-Ismayel, A. Robotic Surgery Training: Construct Validity of Global Evaluative Assessment of Robotic Skills (GEARS). J. Robot. Surg. 2016, 10, 227–231. [Google Scholar] [CrossRef]
- Berguer, R.; Smith, W. An Ergonomic Comparison of Robotic and Laparoscopic Technique: The Influence of Surgeon Experience and Task Complexity. J. Surg. Res. 2006, 134, 87–92. [Google Scholar] [CrossRef]
- Klein, M.I.; Warm, J.S.; Riley, M.A.; Matthews, G.; Gaitonde, K.; Donovan, J.F.; Doarn, C.R. Performance, Stress, Workload, and Coping Profiles in 1st Year Medical Students’ Interaction with the Endoscopic/Laparoscopic and Robot-Assisted Surgical Techniques. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2008, 52, 885–889. [Google Scholar] [CrossRef]
- Ahmed, Y.; Lone, Z.; Hussein, A.A.; Feng, Y.; Khan, H.; Broad, S.; Kannappan, R.; Skowronski, A.; Cole, A.; Wang, D.; et al. Do Surgeon Non-Technical Skills Correlate with Teamwork-Related Outcomes during Robot-Assisted Surgery? BMJ Lead. 2019, 3, 69–74. [Google Scholar] [CrossRef]
- Raison, N.; Ahmed, K.; Abe, T.; Brunckhorst, O.; Novara, G.; Buffi, N.; McIlhenny, C.; van der Poel, H.; van Hemelrijck, M.; Gavazzi, A.; et al. Cognitive Training for Technical and Non-Technical Skills in Robotic Surgery: A Randomised Controlled Trial. BJU Int. 2018, 122, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Shafiei, S.B.; Hussein, A.A.; Guru, K.A. Dynamic Changes of Brain Functional States during Surgical Skill Acquisition. PLoS ONE 2018, 13, e0204836. [Google Scholar] [CrossRef] [PubMed]
- The Da Vinci Research Kit (dVRK)—Intuitive Foundation. Available online: http://www.intuitive-foundation.org/dvrk/ (accessed on 22 January 2020).
- Chinzei, K. Safety of Surgical Robots and IEC 80601-2-77: The First International Standard for Surgical Robots. Acta Polytech. Hung. 2019, 16, 171–184. [Google Scholar]
- IEC 80601-2-77:2019. Available online: https://www.iso.org/cms/render/live/en/sites/isoorg/contents/data/standard/06/84/68473.html (accessed on 22 January 2021).
- Riem, N.; Boet, S.; Bould, M.D.; Tavares, W.; Naik, V.N. Do Technical Skills Correlate with Non-Technical Skills in Crisis Resource Management: A Simulation Study. Br. J. Anaesth. 2012, 109, 723–728. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Vist, G.E.; Falck-Ytter, Y.; Schünemann, H.J. What Is “Quality of Evidence” and Why Is It Important to Clinicians? BMJ Br. Med J. 2008, 336, 995–998. [Google Scholar] [CrossRef]
- Tiferes, J.; Hussein, A.A.; Bisantz, A.; Kozlowski, J.D.; Sharif, M.A.; Winder, N.M.; Ahmad, N.; Allers, J.; Cavuoto, L.; Guru, K.A. The Loud Surgeon Behind the Console: Understanding Team Activities During Robot-Assisted Surgery. J. Surg. Educ. 2016, 73, 504–512. [Google Scholar] [CrossRef]
- Wu, C.; Cha, J.; Sulek, J.; Zhou, T.; Sundaram, C.P.; Wachs, J.; Yu, D. Eye-Tracking Metrics Predict Perceived Workload in Robotic Surgical Skills Training. Hum. Factors 2019, 18720819874544. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.J.; Wilson, M.R.; McGrath, J.S.; Waine, E.; Masters, R.S.W.; Vine, S.J. Surgeons’ Display Reduced Mental Effort and Workload While Performing Robotically Assisted Surgical Tasks, When Compared to Conventional Laparoscopy. Surg. Endosc. 2015, 29, 2553–2560. [Google Scholar] [CrossRef]
- Hussein, A.A.; Shafiei, S.B.; Sharif, M.; Esfahani, E.; Ahmad, B.; Kozlowski, J.D.; Hashmi, Z.; Guru, K.A. Technical Mentorship during Robot-Assisted Surgery: A Cognitive Analysis. BJU Int. 2016, 118, 429–436. [Google Scholar] [CrossRef]
- Singh, H.; Modi, H.N.; Ranjan, S.; Dilley, J.W.R.; Airantzis, D.; Yang, G.Z.; Darzi, A.; Leff, D.R. Robotic Surgery Improves Technical Performance and Enhances Prefrontal Activation During High Temporal Demand. Ann. Biomed. Eng. 2018, 46, 1621–1636. [Google Scholar] [CrossRef] [PubMed]
- Guru, K.A.; Shafiei, S.B.; Khan, A.; Hussein, A.A.; Sharif, M.; Esfahani, E.T. Understanding Cognitive Performance during Robot-Assisted Surgery. Urology 2015, 86, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.; Chen, J.; Marshall, S.; Ghodoussipour, S.; Chen, A.; Gill, I.; Hung, A. Using Objective Robotic Automated Performance Metrics and Task-Evoked Pupillary Response to Distinguish Surgeon Expertise. World J. Urol. 2020, 38, 1599–1605. [Google Scholar] [CrossRef]
- Hart, S.G.; Staveland, L.E. Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research. In Human Mental Workload; Advances in Psychology, 52; North-Holland: Oxford, UK, 1988; pp. 139–183. [Google Scholar] [CrossRef]
- Carswell, C.M.; Clarke, D.; Seales, W.B. Assessing Mental Workload during Laparoscopic Surgery. Surg. Innov. 2005, 12, 80–90. [Google Scholar] [CrossRef]
- Wadhera, R.K.; Parker, S.H.; Burkhart, H.M.; Greason, K.L.; Neal, J.R.; Levenick, K.M.; Wiegmann, D.A.; Sundt, T.M. Is the “Sterile Cockpit” Concept Applicable to Cardiovascular Surgery Critical Intervals or Critical Events? The Impact of Protocol-Driven Communication during Cardiopulmonary Bypass. J. Thorac. Cardiovasc. Surg. 2010, 139, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.I.; Riley, M.A.; Warm, J.S.; Matthews, G. Perceived Mental Workload in an Endocopic Surgery Simulator. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2005, 49, 1014–1018. [Google Scholar] [CrossRef]
- Ruiz-Rabelo, J.F.; Navarro-Rodriguez, E.; Di-Stasi, L.L.; Diaz-Jimenez, N.; Cabrera-Bermon, J.; Diaz-Iglesias, C.; Gomez-Alvarez, M.; Briceño-Delgado, J. Validation of the NASA-TLX Score in Ongoing Assessment of Mental Workload During a Laparoscopic Learning Curve in Bariatric Surgery. Obes. Surg. 2015, 25, 2451–2456. [Google Scholar] [CrossRef]
- Zheng, B.; Jiang, X.; Tien, G.; Meneghetti, A.; Panton, O.N.M.; Atkins, M.S. Workload Assessment of Surgeons: Correlation between NASA TLX and Blinks. Surg. Endosc. 2012, 26, 2746–2750. [Google Scholar] [CrossRef]
- Chowriappa, A.; Raza, S.J.; Fazili, A.; Field, E.; Malito, C.; Samarasekera, D.; Shi, Y.; Ahmed, K.; Wilding, G.; Kaouk, J.; et al. Augmented-Reality-Based Skills Training for Robot-Assisted Urethrovesical Anastomosis: A Multi-Institutional Randomised Controlled Trial. BJU Int. 2015, 115, 336–345. [Google Scholar] [CrossRef]
- Lee, G.I.; Lee, M.R.; Clanton, T.; Clanton, T.; Sutton, E.; Park, A.E.; Marohn, M.R. Comparative Assessment of Physical and Cognitive Ergonomics Associated with Robotic and Traditional Laparoscopic Surgeries. Surg. Endosc. 2014, 28, 456–465. [Google Scholar] [CrossRef]
- Panait, L.; Shetty, S.; Shewokis, P.A.; Sanchez, J.A. Do Laparoscopic Skills Transfer to Robotic Surgery? J. Surg. Res. 2014, 187, 53–58. [Google Scholar] [CrossRef]
- Mouraviev, V.; Klein, M.; Schommer, E.; Thiel, D.D.; Samavedi, S.; Kumar, A.; Leveillee, R.J.; Thomas, R.; Pow-Sang, J.M.; Su, L.M.; et al. Urology Residents Experience Comparable Workload Profiles When Performing Live Porcine Nephrectomies and Robotic Surgery Virtual Reality Training Modules. J. Robot. Surg. 2016, 10, 49–56. [Google Scholar] [CrossRef]
- Lau, E.; Alkhamesi, N.A.; Schlachta, C.M. Impact of Robotic Assistance on Mental Workload and Cognitive Performance of Surgical Trainees Performing a Complex Minimally Invasive Suturing Task. Surg. Endosc. 2019. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, K.; Kobayashi, Y.; Fujie, M.G. Development of Real-Time Simulation for Workload Quantization in Robotic Tele-Surgery. In Proceedings of the 2006 IEEE International Conference on Robotics and Biomimetics, Kunming, China, 17–20 December 2006; pp. 1420–1425. [Google Scholar] [CrossRef]
- Cavuoto, L.A.; Hussein, A.A.; Vasan, V.; Ahmed, Y.; Durrani, A.; Khan, S.; Cole, A.; Wang, D.; Kozlowski, J.; Ahmad, B.; et al. Improving Teamwork: Evaluating Workload of Surgical Team During Robot-Assisted Surgery. Urology 2017, 107, 120–125. [Google Scholar] [CrossRef]
- Klein, M.I.; Lio, C.H.; Grant, R.; Carswell, C.M.; Strup, S. A Mental Workload Study on the 2d and 3d Viewing Conditions of the Da Vinci Surgical Robot. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2009, 53, 1186–1190. [Google Scholar] [CrossRef]
- Sexton, K.; Johnson, A.; Gotsch, A.; Hussein, A.A.; Cavuoto, L.; Guru, K.A. Anticipation, Teamwork and Cognitive Load: Chasing Efficiency during Robot-Assisted Surgery. BMJ Qual. Saf. 2018, 27, 148–154. [Google Scholar] [CrossRef]
- Lee, G.I.; Lee, M.R. Can a Virtual Reality Surgical Simulation Training Provide a Self-Driven and Mentor-Free Skills Learning? Investigation of the Practical Influence of the Performance Metrics from the Virtual Reality Robotic Surgery Simulator on the Skill Learning and Associated Cognitive Workloads. Surg. Endosc. 2018, 32, 62–72. [Google Scholar] [CrossRef]
- Xu, S.; Perez, M.; Perrenot, C.; Hubert, N.; Hubert, J. Face, Content, Construct, and Concurrent Validity of a Novel Robotic Surgery Patient-Side Simulator: The Xperience™ Team Trainer. Surg. Endosc. 2016, 30, 3334–3344. [Google Scholar] [CrossRef]
- Hughes-Hallett, A.; Mayer, E.K.; Marcus, H.J.; Pratt, P.; Mason, S.; Darzi, A.W.; Vale, J.A. Inattention Blindness in Surgery. Surg. Endosc. 2015, 29, 3184–3189. [Google Scholar] [CrossRef]
- Sethi, A.S.; Peine, W.J.; Mohammadi, Y.; Sundaram, C.P. Validation of a Novel Virtual Reality Robotic Simulator. J. Endourol. 2009, 23, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Teoh, A.Y.B.; Chan, S.M.; Yip, H.C.; Wong, V.W.Y.; Chiu, P.W.Y.; Ng, E.K.W. Randomized Controlled Trial of EndoWrist-Enabled Robotic versus Human Laparoendoscopic Single-Site Access Surgery (LESS) in the Porcine Model. Surg. Endosc. 2018, 32, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, K.; Kobayashi, Y.; Fujie, M.G. Operability Evaluation Using an Simulation System for Gripping Motion in Robotic Tele-Surgery. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; Volume 2009, pp. 5106–5109. [Google Scholar] [CrossRef]
- Gerull, W.; Zihni, A.; Awad, M. Operative Performance Outcomes of a Simulator-Based Robotic Surgical Skills Curriculum. Surg. Endosc. 2019. [Google Scholar] [CrossRef]
- Shafiei, S.B.; Hussein, A.A.; Muldoon, S.F.; Guru, K.A. Functional Brain States Measure Mentor-Trainee Trust during Robot-Assisted Surgery. Sci. Rep. 2018, 8, 3667. [Google Scholar] [CrossRef] [PubMed]
- Borghini, G.; Arico, P.; Di Flumeri, G.; Colosimo, A.; Storti, S.F.; Menegaz, G.; Fiorini, P.; Babiloni, F. Neurophysiological Measures for Users’ Training Objective Assessment during Simulated Robot-Assisted Laparoscopic Surgery. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; Volume 2016, pp. 981–984. [Google Scholar] [CrossRef]
- Marçon, B.; Sime, W.; Guillemin, F.; Hubert, N.; Lagrange, F.; Huselstein, C.; Hubert, J. An Ergonomic Assessment of Four Different Donor Nephrectomy Approaches for the Surgeons and Their Assistants. Res. Rep. Urol. 2019, 11, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Cha, J.; Gonzalez, G.; Wachs, J.; Sundaram, C.; Yu, D. Joint Surgeon Attributes Estimation in Robot-Assisted Surgery. In Proceedings of the ACM/IEEE International Conference on Human-Robot Interaction, Chicago, IL, USA, 5–8 March 2018; pp. 285–286. [Google Scholar] [CrossRef]
- Kawamura, K.; Kobayashi, Y.; Fujie, M.G. Pilot Study on Verification of Effectiveness on Operability of Assistance System for Robotic Tele-Surgery Using Simulation. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; Volume 2010, pp. 2308–2312. [Google Scholar] [CrossRef]
- Dulan, G.; Rege, R.V.; Hogg, D.C.; Gilberg-Fisher, K.M.; Arain, N.A.; Tesfay, S.T.; Scott, D.J. Proficiency-Based Training for Robotic Surgery: Construct Validity, Workload, and Expert Levels for Nine Inanimate Exercises. Surg. Endosc. 2012, 26, 1516–1521. [Google Scholar] [CrossRef]
- Turiani Hourneaux de Moura, D.; Aihara, H.; Jirapinyo, P.; Farias, G.; Hathorn, K.; Bazarbashi, A.; Sachdev, A.; Thompson, C. Robot-Assisted Endoscopic Submucosal Dissection versus Conventional ESD for Colorectal Lesions: Outcomes of a Randomized Pilot Study in Endoscopists without Prior ESD Experience (with Video). Gastrointest. Endosc. 2019, 90, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Law, K.E.; Lowndes, B.R.; Kelley, S.R.; Blocker, R.C.; Larson, D.W.; Hallbeck, M.S.; Nelson, H. NASA-Task Load Index Differentiates Surgical Approach: Opportunities for Improvement in Colon and Rectal Surgery. Ann. Surg. 2020, 271, 906–912. [Google Scholar] [CrossRef]
- Boles, D.B.; Adair, L.P. The Multiple Resources Questionnaire (MRQ). In Proceedings of the Human Factors and Ergonomics Society Annual Meeting; Sage: Los Angeles, CA, USA, 2001; Volume 45, pp. 1790–1794. [Google Scholar] [CrossRef]
- Klein, M.I.; Warm, J.S.; Riley, M.A.; Matthews, G.; Doarn, C.; Donovan, J.F.; Gaitonde, K. Mental Workload and Stress Perceived by Novice Operators in the Laparoscopic and Robotic Minimally Invasive Surgical Interfaces. J. Endourol. 2012, 26, 1089–1094. [Google Scholar] [CrossRef]
- Matthews, G. Multidimensional Profiling of Task Stress States for Human Factors: A Brief Review. Hum. Factors 2016, 58, 801–813. [Google Scholar] [CrossRef]
- Ghanbary Sartang, A.; Ashnagar, M.; Habibi, E.; Sadeghi, S. Evaluation of Rating Scale Mental Effort (RSME) Effectiveness for Mental Workload Assessment in Nurses. J. Occup. Health Epidemiol. 2016, 5, 211–217. [Google Scholar] [CrossRef]
- Schiff, L.; Tsafrir, Z.; Aoun, J.; Taylor, A.; Theoharis, E.; Eisenstein, D. Quality of Communication in Robotic Surgery and Surgical Outcomes. JSLS J. Soc. Laparoendosc. Surg. 2016, 20. [Google Scholar] [CrossRef]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric Properties, Benchmarking Data, and Emerging Research. BMC Health Serv. Res. 2006, 6, 44. [Google Scholar] [CrossRef]
- Kohli, A.; Kaur, M. Wisconsin Card Sorting Test: Normative Data and Experience. Indian J. Psychiatry 2006, 48, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Liu, Q.; Hu, T.; Jin, X. Adapting the Short Form of the Coping Inventory for Stressful Situations into Chinese. Neuropsychiatr. Dis. Treat. 2017, 13, 1669–1675. [Google Scholar] [CrossRef]
- Van der Schatte Olivier, R.H.; Van’t Hullenaar, C.D.P.; Ruurda, J.P.; Broeders, I.A.M.J. Ergonomics, User Comfort, and Performance in Standard and Robot-Assisted Laparoscopic Surgery. Surg. Endosc. 2009, 23, 1365–1371. [Google Scholar] [CrossRef]
- Helton, W.S. Validation of a Short Stress State Questionnaire. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2016. [Google Scholar] [CrossRef]
- Wilson, M.R.; Poolton, J.M.; Malhotra, N.; Ngo, K.; Bright, E.; Masters, R.S.W. Development and Validation of a Surgical Workload Measure: The Surgery Task Load Index (SURG-TLX). World J. Surg. 2011, 35, 1961–1969. [Google Scholar] [CrossRef]
- Malhotra, N.; Poolton, J.M.; Wilson, M.R.; Fan, J.K.M.; Masters, R.S.W. Conscious Motor Processing and Movement Self-Consciousness: Two Dimensions of Personality That Influence Laparoscopic Training. J. Surg. Educ. 2014, 71, 798–804. [Google Scholar] [CrossRef]
- Abdelrahman, A.M.; Bingener, J.; Yu, D.; Lowndes, B.R.; Mohamed, A.; McConico, A.L.; Hallbeck, M.S. Impact of Single-Incision Laparoscopic Cholecystectomy (SILC) versus Conventional Laparoscopic Cholecystectomy (CLC) Procedures on Surgeon Stress and Workload: A Randomized Controlled Trial. Surg. Endosc. 2016, 30, 1205–1211. [Google Scholar] [CrossRef]
- Weigl, M.; Stefan, P.; Abhari, K.; Wucherer, P.; Fallavollita, P.; Lazarovici, M.; Weidert, S.; Euler, E.; Catchpole, K. Intra-Operative Disruptions, Surgeon’s Mental Workload, and Technical Performance in a Full-Scale Simulated Procedure. Surg. Endosc. 2016, 30, 559–566. [Google Scholar] [CrossRef]
- Berg, R.J.; Inaba, K.; Sullivan, M.; Okoye, O.; Siboni, S.; Minneti, M.; Teixeira, P.G.; Demetriades, D. The Impact of Heat Stress on Operative Performance and Cognitive Function during Simulated Laparoscopic Operative Tasks. Surgery 2015, 157, 87–95. [Google Scholar] [CrossRef]
- Weigl, M.; Antoniadis, S.; Chiapponi, C.; Bruns, C.; Sevdalis, N. The Impact of Intra-Operative Interruptions on Surgeons’ Perceived Workload: An Observational Study in Elective General and Orthopedic Surgery. Surg. Endosc. 2015, 29, 145–153. [Google Scholar] [CrossRef]
- Guru, K.A.; Esfahani, E.T.; Raza, S.J.; Bhat, R.; Wang, K.; Hammond, Y.; Wilding, G.; Peabody, J.O.; Chowriappa, A.J. Cognitive Skills Assessment during Robot-Assisted Surgery: Separating the Wheat from the Chaff. BJU Int. 2015, 115, 166–174. [Google Scholar] [CrossRef]
- Walters, C.; Webb, P.J. Maximizing Efficiency and Reducing Robotic Surgery Costs Using the NASA Task Load Index. AORN J. 2017, 106, 283–294. [Google Scholar] [CrossRef]
- Yu, D.; Dural, C.; Morrow, M.M.B.; Yang, L.; Collins, J.W.; Hallbeck, S.; Kjellman, M.; Forsman, M. Intraoperative Workload in Robotic Surgery Assessed by Wearable Motion Tracking Sensors and Questionnaires. Surg. Endosc. 2017, 31, 877–886. [Google Scholar] [CrossRef]
- Beulens, A.; Brinkman, W.; Koldewijn, E.; Hendrikx, A.; van Basten, J.; van Merriënboer, J.; Van der Poel, H.; Bangma, C.; Wagner, C. A Prospective, Observational, Multicentre Study Concerning Nontechnical Skills in Robot-Assisted Radical Cystectomy versus Open Radical Cystectomy. Eur. Urol. Open Sci. 2020, 19, 37–44. [Google Scholar] [CrossRef]
- Thangaratinam, S.; Redman, C.W. The Delphi Technique. Obstet. Gynaecol. 2005, 7, 120–125. [Google Scholar] [CrossRef]
- Catchpole, K.; Perkins, C.; Bresee, C.; Solnik, M.J.; Sherman, B.; Fritch, J.; Gross, B.; Jagannathan, S.; Hakami-Majd, N.; Avenido, R.; et al. Safety, Efficiency and Learning Curves in Robotic Surgery: A Human Factors Analysis. Surg. Endosc. 2016, 30, 3749–3761. [Google Scholar] [CrossRef]
- Zattoni, F.; Guttilla, A.; Crestani, A.; De Gobbi, A.; Cattaneo, F.; Moschini, M.; Vianello, F.; Valotto, C.; Dal Moro, F.; Zattoni, F. The Value of Open Conversion Simulations During Robot-Assisted Radical Prostatectomy: Implications for Robotic Training Curricula. J. Endourol. 2015, 29, 1282–1288. [Google Scholar] [CrossRef]
- Sevdalis, N.; Davis, R.; Koutantji, M.; Undre, S.; Darzi, A.; Vincent, C.A. Reliability of a Revised NOTECHS Scale for Use in Surgical Teams. Am. J. Surg. 2008, 196, 184–190. [Google Scholar] [CrossRef]
- Yule, S.; Flin, R.; Paterson-Brown, S.; Maran, N. Non-Technical Skills for Surgeons in the Operating Room: A Review of the Literature. Surgery 2006, 139, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Hull, L.; Arora, S.; Kassab, E.; Kneebone, R.; Sevdalis, N. Observational Teamwork Assessment for Surgery: Content Validation and Tool Refinement. J. Am. Coll. Surg. 2011, 212, 234–243.e5. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.W.; Ku, Y.; Kim, H.C. A Novel Wearable EEG and ECG Recording System for Stress Assessment. Sensors 2019, 19, 1991. [Google Scholar] [CrossRef]
- Herborn, K.A.; Graves, J.L.; Jerem, P.; Evans, N.P.; Nager, R.; McCafferty, D.J.; McKeegan, D.E. Skin Temperature Reveals the Intensity of Acute Stress. Physiol. Behav. 2015, 152, 225–230. [Google Scholar] [CrossRef]
- Pavlidis, I.; Tsiamyrtzis, P.; Shastri, D.; Wesley, A.; Zhou, Y.; Lindner, P.; Buddharaju, P.; Joseph, R.; Mandapati, A.; Dunkin, B.; et al. Fast by Nature—How Stress Patterns Define Human Experience and Performance in Dexterous Tasks. Sci. Rep. 2012, 2, 305. [Google Scholar] [CrossRef]
- How the Temperature of Your Nose Shows How Much Strain You Are under—The University of Nottingham. Available online: https://www.nottingham.ac.uk/news/pressreleases/2018/january/how-the-temperature-of-your-nose-shows-how-much-strain-you-are-under.aspx (accessed on 20 December 2019).
- Laetitia Lisetti, C.L.; Nasoz, F. Using Noninvasive Wearable Computers to Recognize Human Emotions from Physiological Signals. EURASIP J. Appl. Signal Process. 2004, 2004, 1672–1687. [Google Scholar] [CrossRef]
- Youngson, G.G. Nontechnical Skills in Pediatric Surgery: Factors Influencing Operative Performance. J. Pediatr. Surg. 2016, 51, 226–230. [Google Scholar] [CrossRef]
- Di Stasi, L.L.; McCamy, M.B.; Macknik, S.L.; Mankin, J.A.; Hooft, N.; Catena, A.; Martinez-Conde, S. Saccadic Eye Movement Metrics Reflect Surgical Residents’ Fatigue. Ann. Surg. 2014, 259, 824–829. [Google Scholar] [CrossRef]
- Law, B.; Atkins, M.S.; Kirkpatrick, A.E.; Lomax, A.J. Eye Gaze Patterns Differentiate Novice and Experts in a Virtual Laparoscopic Surgery Training Environment. In ETRA ’04: Proceedings of the 2004 Symposium on Eye Tracking Research & Applications; Association for Computing Machinery: San Antonio, TX, USA, 2004; pp. 41–48. [Google Scholar] [CrossRef]
- Shahbazi, M.; Poursartip, B.; Siroen, K.; Schlachta, C.M.; Patel, R.V. Robotics-Assisted Surgical Skills Evaluation Based on Electrocortical Activity. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; Volume 2018, pp. 3673–3676. [Google Scholar] [CrossRef]
- Sigl, J.C.; Chamoun, N.G. An Introduction to Bispectral Analysis for the Electroencephalogram. J. Clin. Monit. 1994, 10, 392–404. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Mylonas, G.P.; Kwok, K.W.; James, D.R.C.; Leff, D.; Orihuela-Espina, F.; Darzi, A.; Yang, G.Z. Gaze-Contingent Motor Channelling, Haptic Constraints and Associated Cognitive Demand for Robotic MIS. Med. Image Anal. 2012, 16, 612–631. [Google Scholar] [CrossRef]
- James, D.R.C.; Orihuela-Espina, F.; Leff, D.R.; Mylonas, G.P.; Kwok, K.W.; Darzi, A.W.; Yang, G.Z. Cognitive Burden Estimation for Visuomotor Learning with fNIRS. In International Conference on Medical Image Computing and Computer-Assisted Intervention; Springer: Berlin/Heidelberg, Germany, 2010; Volume 13, pp. 319–326. [Google Scholar] [CrossRef]
- Bunce, S.; Izzetoglu, M.; Izzetoglu, K.; Onaral, B.; Pourrezaei, K. Functional Near-Infrared Spectroscopy. IEEE Eng. Med. Biol. Mag. 2006, 25, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Venclove, S.; Daktariunas, A.; Ruksenas, O. Functional Near-Infrared Spectroscopy: A Continuous Wave Type Based System for Human Frontal Lobe Studies. EXCLI J. 2015, 14, 1145–1152. [Google Scholar] [CrossRef]
- Wilcox, T.; Biondi, M. fNIRS in the Developmental Sciences. Wiley Interdiscip. Rev. Cogn. Sci. 2015, 6, 263–283. [Google Scholar] [CrossRef]
- Frank, M.N.; Kinlaw, W.B. Indirect Measurement of Isovolumetric Contraction Time and Tension Period in Normal Subjects. Am. J. Cardiol. 1962, 10, 800–806. [Google Scholar] [CrossRef]
- How Will Sensor Technology Impact the Medical Robots of the Future?|MediSens Conference. Available online: https://medisens-conference.com/2018/01/22/how-sensor-technologies-will-transform-the-surgical-robots-of-the-future/ (accessed on 29 March 2021).
- Fu, G.; Azimi, E.; Kazanzides, P. Mobile Teleoperation: Evaluation of Wireless Wearable Sensing of the Operator’s Arm Motion. arXiv 2021, arXiv:2103.08119. Comment: 6 pages, 11 figures. Submitted to 2021 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), pending review. [Google Scholar]
- Abeywardena, S.; Yuan, Q.; Tzemanaki, A.; Psomopoulou, E.; Droukas, L.; Melhuish, C.; Dogramadzi, S. Estimation of Tool-Tissue Forces in Robot-Assisted Minimally Invasive Surgery Using Neural Networks. Front. Robot. AI 2019, 6. [Google Scholar] [CrossRef] [PubMed]
- Thai, M.T.; Phan, P.T.; Hoang, T.T.; Wong, S.; Lovell, N.H.; Do, T.N. Advanced Intelligent Systems for Surgical Robotics. Adv. Intell. Syst. 2020, 2, 1900138. [Google Scholar] [CrossRef]
- Mishra, A.; Catchpole, K.; Dale, T.; McCulloch, P. The Influence of Non-Technical Performance on Technical Outcome in Laparoscopic Cholecystectomy. Surg. Endosc. 2008, 22, 68–73. [Google Scholar] [CrossRef]
- Zia, A.; Essa, I. Automated Surgical Skill Assessment in RMIS Training. Int. J. Comput. Assist. Radiol. Surg. 2018, 13, 731–739. [Google Scholar] [CrossRef]
- Funke, I.; Mees, S.T.; Weitz, J.; Speidel, S. Video-Based Surgical Skill Assessment Using 3D Convolutional Neural Networks. Int. J. Comput. Assist. Radiol. Surg. 2019, 14, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Nagy, D.A.; Takács, K.; Rudas, I.J.; Haidegger, T. Employing Process Models for Surgical Training. In Proceedings of the 2020 IEEE 18th World Symposium on Applied Machine Intelligence and Informatics (SAMI), Herlany, Slovakia, 23–25 January 2020; pp. 101–104. [Google Scholar]
| Title | Endpoint | Description |
|---|---|---|
| Mental demands | low/high | How much mental activity was required? |
| Physical demands | low/high | How much physical activity was required? |
| Temporal demands | low/high | How much time pressure did you feel? |
| Effort | low/high | How hard did you have to work? |
| Performance | good/poor | How stressful do you think you were? |
| Frustration level | low/high | How frustrated did you feel? |
| Title | Endpoint | Description |
|---|---|---|
| Mental demands | low/high | How mentally fatiguing was the procedure? |
| Physical demands | low/high | How physically fatiguing was the procedure? |
| Temporal demands | low/high | How hurried or rushed was the pace of the procedure? |
| Task complexity | low/high | How complex was the procedure? |
| Situational stress | low/high | How anxious did you feel while performing the procedure? |
| Distractions | low/high | How distracting was the operating environment? |
| Revised NOTECHS | NOTSS | OTAS | ICARS | |
|---|---|---|---|---|
| Date | 2008 | 2006 | 2006 | 2017 |
| Reference | [100] | [101] | [102] | [22] |
| Non-technical skills |
|
|
|
|
| Content validity | ✓ | ✓ | ✓ | |
| Construct validity | ✓ | ✓ | ||
| Inter-rater reliability | ✓ | ✓ | ✓ | ✓ |
| Sensitivity | n.a. | not acceptable in some categories | n.a. | n.a. |
| Feasibility | ✓ (especially for self-assessment) | ✓ | limited to certain procedures | ✓ |
| NTS Category | NTS Group | NTS |
|---|---|---|
| Interpersonal skills | Communication and teamwork | Effective verbal communication |
| Appropriate interaction with bedside surgeon | ||
| Appropriate interaction with operating room staff | ||
| Engages/initiates in confirmatory feedback with OR staff | ||
| Leadership | Appropriate and polite instructions | |
| Effective workload management | ||
| Coordination of the team from the console | ||
| Coordination of the team at the bedside | ||
| Delegating tasks to team members | ||
| Maintenance of professional standards | ||
| Cognitive skills | Decision making | Appropriate decision making in case of equipment failure |
| Appropriate decision making at the bedside | ||
| Quick diagnosis of unexpected patient events | ||
| Quick decision making in case of emergency | ||
| Generation, selection and implementation of solutions | ||
| Outcome review of decision | ||
| Situation awareness | Awareness of patient status | |
| Ability to deal with patient at the bedside | ||
| Ability of quick adaptation to problems | ||
| Anticipation of potential problems | ||
| Role awareness of surrounding team members at the console | ||
| Personal resource skills | Cope with stress and distractors | Understands personal limitations and asks for help |
| (if necessary) | ||
| Identification of stressor | ||
| Maintenance of cognitive skills | ||
| Maintenance of technical skills | ||
| Professional and appropriate choice of resolution |
| Ref. | Date | Subj. | Environment | Input | Measured Feature/NTS | Conclusion | QoE |
|---|---|---|---|---|---|---|---|
| [30] | 2006 | 10 | Dry lab | Skin conductance Self-rating (custom) | Workload Stress | Stress is less in the case of RAMIS compared to traditional MIS. | mod. |
| [58] | 2006 | 5 | VR simulator | NASA-TLX | Workload | Workload can be increased in proportion to delay time with the proposed simulators. | low |
| [31] | 2008 | 15 | Dry lab | DSSQ MRQ CITS | Workload Stress | Stress is less, workload and stress coping strategies are the same in the case of RAMIS compared to traditional MIS. | low |
| [65] | 2009 | 20 | VR simulator | NASA-TLX | Workload | Mimic dV-Trainer shows reasonable workload results. | low |
| [60] | 2009 | 15 | Dry lab | NASA-TLX MRQ | Workload | The usage of the da Vinci 3D view causes less workload compared to the 2D view in some cases. | low |
| [67] | 2009 | 6 | VR simulator | NASA-TLX | Workload | Time delay in teleoperation can significantly increase the workload. | low |
| [85] | 2009 | 16 | Dry lab | MSSD PEP HRA SMEQ LED | Workload Stress | RAMIS causes less cognitive workload compared to traditional MIS. | low |
| [8] | 2010 | 34 | Live porcine | NASA-TLX | Workload | RAMIS poses less mental workload compared to traditional MIS. | mod. |
| [73] | 2010 | 3 | VR simulator | NASA-TLX | Workload | Workload is not improved under delays of 300 ms and 400 ms in the simulated environment. | low |
| [115] | 2010 | 21 | VR simulator | fNIRS | Workload | FNIRS can show the cognitive burden during training. | high |
| [78] | 2012 | 15 | Dry lab | MRQ DSSQ | Workload Stress | Novices have less stress when working with the da Vinci compared to traditional MIS. | low |
| [74] | 2012 | 12 | Dry lab | NASA-TLX | Workload | After the proposed training, mental workload is similar between novices and experts. | low |
| [114] | 2012 | 21 | VR simulator | fNIRS | Cortical activity | There is a significant difference between expert and non-expert subjects with Gaze-Contingent Motor Channeling. | mod. |
| [7] | 2014 | 2 | OR | HR HRV | Stress | RAMIS poses less mental workload compared to traditional MIS. Workload measurement with HRV is cumbersome. | mod. |
| [55] | 2014 | 28 | Dry lab | NASA-TLX | Workload | RAMIS poses significantly better workload perception compared to traditional MIS. | low |
| [54] | 2014 | 13 | Dry lab | NASA-TLX | Workload | Physiological and cognitive ergonomics with robotic surgery are significantly less challenging compared to traditional MIS. | low |
| [53] | 2014 | 52 | VR simulator | NASA-TLX | Workload | Urethrovesical anastomosis VR training improves technical skill acquisition with cognitive demand. | mod. |
| [93] | 2015 | 10 | Dry lab | EEG | Cognitive engagement Mental workload Mental state | Cognitive assessment can define the expertise levels. | high |
| [42] | 2015 | 32 | Dry lab | SURG-TLX RSME Heart rate monitor | Workload HRV | RAMIS poses less mental workload compared to traditional MIS. | mod. |
| [99] | 2015 | 6 | Simulated OR | Expert rating (custom) | Communication Leadership | Repeated simulations and increased leadership mean faster and less flawed conversions in the OR. | mod. |
| [64] | 2015 | 24 | Image display | NASA-TLX | Workload | Increasing the level of cognitive load is significantly increasing the inattention blindness. | mod. |
| [45] | 2015 | 1 | OR | EEG NASA-TLX | Workload Distractions Mental state | Expert surgeons use different mental resources based on their needs. | mod. |
| [98] | 2016 | 89 | OR | Expert rating (custom) | Communication Decision making | RAMIS increases communication requirements for the team of the OR. | mod. |
| [63] | 2016 | 28 | VR simulator | NASA-TLX | Workload | Xperience Team Trainer emphasizes the importance of teamwork. | mod. |
| [81] | 2016 | 32 | OR | PTICSQ SAQ | Communication | There is a significant correlation between team communication and surgical outcome. | mod. |
| [43] | 2016 | 1 | OR | EEG NASA-TLX | Workload | A surgical expert during mentoring concerned while he was observed the surgery. | low |
| [40] | 2016 | 89 | OR | Expert rating (custom) NASA-TLX | Communication Workload | The proposed method is capable of capturing team activities during RAMIS. | mod. |
| [56] | 2016 | 21 | Live porcine VR simulator | NASA-TLX | Workload | Live animal and VR simulator training provide a comparable workload. | low |
| [70] | 2016 | 8 | VR simulator | EEG NASA-TLX | Procedural memory Attention level Workload | EEG can show the learning progress in the case of RAMIS. | high |
| [59] | 2017 | 55 | OR | NASA-TLX | Workload | The study proposes a workload variety analysis with different members of the OR. | mod. |
| [94] | 2017 | 25 p. | OR | NASA-TLX | Workload | NASA-TLX is a useful tool for determining the appropriate staff member mix for RAMIS procedures. | mod. |
| [95] | 2017 | 10 | OR | SURG-TLX | Workload | Mental demands are higher for surgeons at the console than are assisting. | mod. |
| [66] | 2018 | 24 | Live porcine | NASA-TLX | Workload | Single-site access surgery can significantly reduce the workload. | mod. |
| [34] | 2018 | 27 | VR simulator | EEG NASA-TLX | Cognitive features Mental workload Engagement Asymmetry index Brain functional features Communication Integration Recruitment Workload | EEG features can be used for objective non-technical skill assessment. | high |
| [61] | 2018 | 27 | OR | OR efficiency (custom) NASA-TLX | Communication Workload | Anticipation causes shorter operating time. Team familiarity causes less inconveniences. Less anticipation causes less cognitive load. | mod. |
| [62] | 2018 | 32 | VR simulator | NASA-TLX SSSQ MRQ | Workload Stress | Training with a VR simulator can decrease the workload and stress. | mod. |
| [33] | 2018 | 62 | Dry lab Simulated OR | NOTSS | Situational awareness Decision making Leadership Communication Teamwork | Motor imaginary training technique is not effective in non-technical skill training. | mod. |
| [44] | 2018 | 8 | Dry lab | fNIRS SURG-TLX HRV | Prefrontal activation Workload Stress response | RAMIS improves performance during high workload conditions. | high |
| [69] | 2018 | 4 | OR | EEG NASA-TLX | Cognitive features Functional features Mental workload Mental load Engagement Situation awareness Blink rate Asymmetry index Completion time Communication | During a simple surgical task, functional brain features are sufficient to classify mentor–trainee trust. | high |
| [111] | 2018 | 32 | VR simulator | EEG | Electrocortical activity in temporoparietal and left frontal regions | There are significant differences in electrocortical activity between novices and experts. | high |
| [72] | 2018 | 12 | VR simulator | HRV NASA-TLX Wrist motion EMG Electrodermal EEG | Workload Expertise | The proposed skill and workload evaluation framework is accurate. | high |
| [32] | 2019 | 20 | OR | NOTSS NASA-TLX | Situational awareness Decision making Leadership Communication Teamwork Workload | Non-technical skills are associated with team efficiency, surgical flow disruptions and self-perceived performance. | high |
| [75] | 2019 | 5 | OR | NASA-TLX | Workload | Workload is less in the case of robot-assisted submucosal dissection compared to the traditional case. | low |
| [68] | 2019 | 31 | VR simulator | NASA-TLX | Workload | Specific self-directed robotic simulation curriculum was introduced, which can significantly decrease the workload. | mod. |
| [41] | 2019 | 8 | VR simulator | NASA-TLX Eye movements | Workload | Eye movements correlate with the workload. | high |
| [71] | 2019 | 264 p. | OR | NASA-TLX | Workload | Mental workload is similar in the case of RAMIS, traditional MIS, hand-assisted MIS and open surgery. | mod. |
| [57] | 2019 | 30 | Wet lab | NASA-TLX PVT WCST | Workload Concentration Cognitive function | Robotic assistance does not provide less mental workload with novices. Robotic assistance may be mentally taxing for robotic novices. | mod. |
| [76] | 2020 | 7 | OR | NASA-TLX | Workload | RAMIS requires less mental demand and effort compared to open access surgery and traditional MIS. | mod. |
| [46] | 2020 | 26 | Dry lab | Task-evoked pupillary response | Workload | Under high cognitive workload, there can be a divergence in robotic movement profiles between expertise levels. | high |
| [96] | 2020 | n.a. | OR | OTAS NOTSS ICARS NOTECHS II | Situation awareness Decision making Communication Teamwork Leadership Stress | The study proposed a structured approach to the analysis of non-technical skill using extracorporeal videos of both open radical cystectomy and RAMIS radical cystectomy | mod. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagyné Elek, R.; Haidegger, T. Non-Technical Skill Assessment and Mental Load Evaluation in Robot-Assisted Minimally Invasive Surgery. Sensors 2021, 21, 2666. https://doi.org/10.3390/s21082666
Nagyné Elek R, Haidegger T. Non-Technical Skill Assessment and Mental Load Evaluation in Robot-Assisted Minimally Invasive Surgery. Sensors. 2021; 21(8):2666. https://doi.org/10.3390/s21082666
Chicago/Turabian StyleNagyné Elek, Renáta, and Tamás Haidegger. 2021. "Non-Technical Skill Assessment and Mental Load Evaluation in Robot-Assisted Minimally Invasive Surgery" Sensors 21, no. 8: 2666. https://doi.org/10.3390/s21082666
APA StyleNagyné Elek, R., & Haidegger, T. (2021). Non-Technical Skill Assessment and Mental Load Evaluation in Robot-Assisted Minimally Invasive Surgery. Sensors, 21(8), 2666. https://doi.org/10.3390/s21082666







