Towards Detecting Biceps Muscle Fatigue in Gym Activity Using Wearables
Abstract
1. Introduction
1.1. Background
1.1.1. The Invasive Approach
1.1.2. The Cardio-Respiratory Approach
1.1.3. The Wearable Approach
1.2. Our Contributions
- Highlighting a number of challenges and solutions related to data collection and processing
- Publishing a biceps muscle fatigue dataset in the form of a concentration curl exercise (bicep fatigue dataset—https://zenodo.org/record/3698242#.XmFZ5qhKguU).
2. Materials: Data Collection and Related Challenges
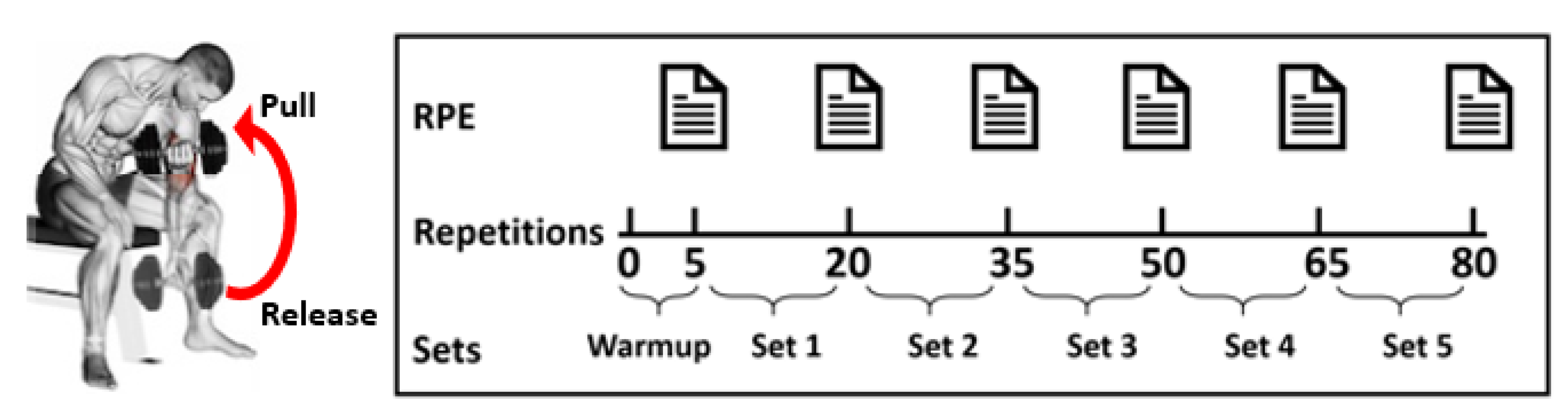
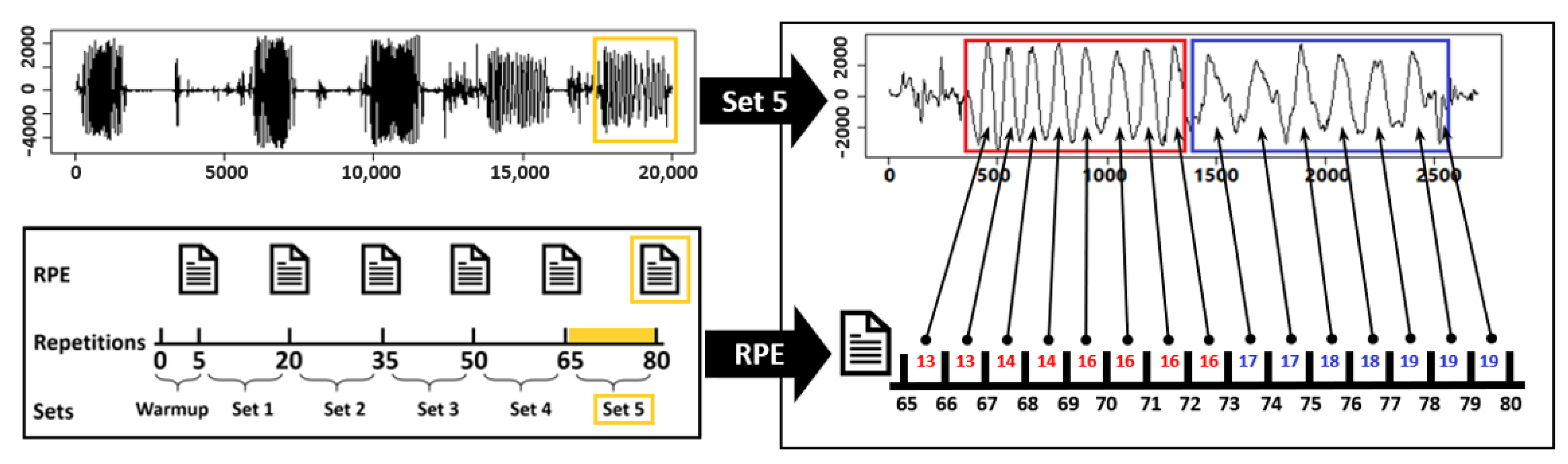
2.1. Collecting Data
- We ask the volunteer to sit down on a flat bench with bent knees and one dumbbell between the volunteer’s legs.
- We ask the volunteer to pick up the dumbbell with the right hand while placing the right elbow on the top of the inner right thigh. This is the release position.
- We ask the volunteer to pull up the dumbbell by only moving the forearms and contracting the biceps while breathing out. Once the biceps are fully contracted, and the dumbbells are at shoulder level, we ask the volunteer to hold the pull position for a second to guarantee a good contraction.
- Finally, we ask the volunteer to slowly bring the dumbbells back to the release position while breathing in. Then, we ask the volunteer to repeat the exercise for 15 repetitions; after that, repeating the exercise with the left arm.
2.2. Data Collection Challenges
3. Methods: Data Processing and Experiment Setup
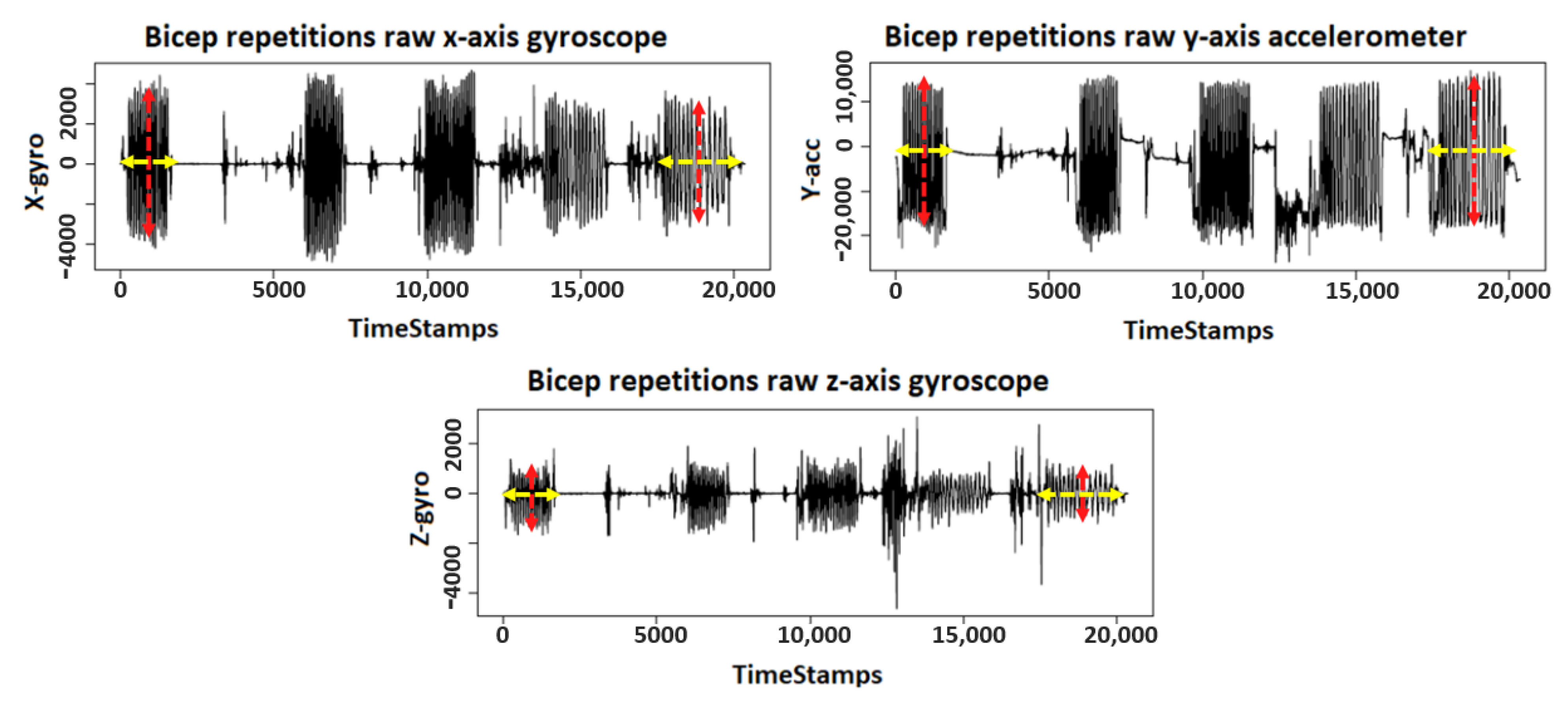
3.1. Data Processing and Feature Extraction
- Total Acceleration: this is the vector sum of the tangential and centripetal accelerations, which makes it a place-independent signal, which means it does not rely on the exact attachment of the accelerometer because it combines x, y, and z acceleration signals at time to compute a total acceleration, defined as: .
- Exerted Force: is the exerted force by the a volunteer to lift the dumble. is calculated by multiplying the mass m of the lifted dumble by acceleration a.
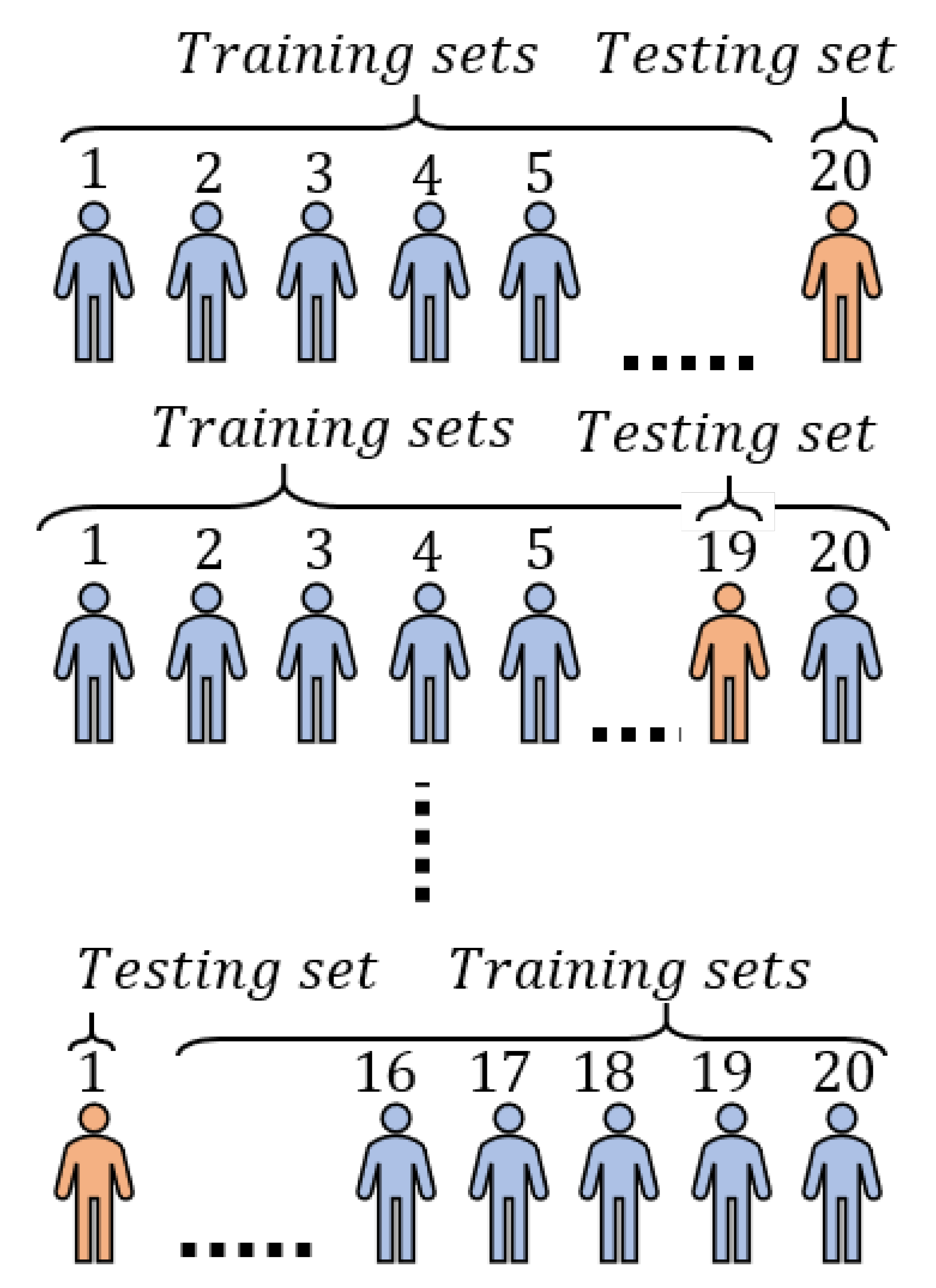
3.2. Experiment Setup
- Subject-specific model: this is a personalized model for each participant and it uses only the data of that participant. This model would work well if each subject had a unique pattern in response to fatigue accumulation.
- Cross-subject model: this is a single model for all participants. It leverages data from all participants following the assumption that multiple subjects will have similar changes in style as a response to fatigue.
3.2.1. RQ1: What Are the Most Significant Features to Detect Bicep Muscles Fatigue?
3.2.2. RQ2: How Accurately Can We Detect Biceps Muscles Fatigue Using Subject-Specific Model?
3.2.3. RQ3: Can We Build an Accurate Cross-Subject Model to Detect Biceps Muscles Fatigue?
4. Results
4.1. RQ1 Results: What Are the Most Significant Features to Detect Bicep Muscles Fatigue?
4.2. RQ2 Results: How Accurately Can We Predict Subject-Specific Biceps Fatigue?
4.3. RQ3 Results: Can We Build an Accurate Cross-Subject Fatigue Detection Model?
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Enoka, R.M.; Duchateau, J. Translating fatigue to human performance. Med. Sci. Sports Exerc. 2016, 48, 2228. [Google Scholar] [CrossRef] [PubMed]
- Gruet, M.; Temesi, J.; Rupp, T.; Levy, P.; Millet, G.; Verges, S. Stimulation of the motor cortex and corticospinal tract to assess human muscle fatigue. Neuroscience 2013, 231, 384–399. [Google Scholar] [CrossRef] [PubMed]
- De, C.L. Myoelectrical manifestations of localized muscular fatigue in humans. Crit. Rev. Biomed. Eng. 1984, 11, 251–279. [Google Scholar]
- Cifrek, M.; Medved, V.; Tonković, S.; Ostojić, S. Surface EMG based muscle fatigue evaluation in biomechanics. Clin. Biomech. 2009, 24, 327–340. [Google Scholar] [CrossRef]
- Opar, D.; Williams, M.; Shield, A. Hamstring Strain Injuries Factors that Lead to Injury and Re-Injury. Sports Med. (Auckland N. Z.) 2012, 42, 209–226. [Google Scholar] [CrossRef]
- Mueller-Wohlfahrt, H.W.; Haensel, L.; Mithoefer, K.; Ekstrand, J.; English, B.; McNally, S.; Orchard, J.; van Dijk, C.N.; Kerkhoffs, G.M.; Schamasch, P.; et al. Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br. J. Sports. Med. 2013, 47, 342–350. [Google Scholar] [CrossRef]
- Kellmann, M. Preventing overtraining in athletes in high-intensity sports and stress/recovery monitoring. Scand. J. Med. Sci. Sport. 2010, 20, 95–102. [Google Scholar] [CrossRef]
- Thalman, C.M.; Lam, Q.P.; Nguyen, P.H.; Sridar, S.; Polygerinos, P. A Novel Soft Elbow Exosuit to Supplement Bicep Lifting Capacity. In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018; pp. 6965–6971. [Google Scholar]
- Steffen, L.M.; Arnett, D.K.; Blackburn, H.; Shah, G.; Armstrong, C.; Luepker, R.V.; Jacobs, J.D. Population trends in leisure-time physical activity: Minnesota Heart Survey, 1980–2000. Med. Sci. Sports Exerc. 2006, 38, 1716–1723. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Bogart, B.I.; Ort, V.H. Elsevier’s Integrated Anatomy and Embryology; Book, Whole; Elsevier: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Nesterenko, S.; Domire, Z.J.; Morrey, B.F.; Sanchez-Sotelo, J. Elbow strength and endurance in patients with a ruptured distal biceps tendon. J. Shoulder Elb. Surg. 2010, 19, 184–189. [Google Scholar] [CrossRef]
- Mair, S.D.; Seaber, A.V.; Glisson, R.R.; Garrett, W.E., Jr. The role of fatigue in susceptibility to acute muscle strain injury. Am. J. Sports Med. 1996, 24, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Garrett, W.E., Jr. Muscle strain injuries. Am. J. Sports Med. 1996, 24, S2–S8. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Quarrie, K.L.; Hume, P.A. Risk factors and risk statistics for sports injuries. Clin. J. Sport Med. 2007, 17, 208–210. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J.; Maughan, R.J.; Gleeson, M. The Biochemical Basis of Sports Performance; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Robergs, R.A.; Ghiasvand, F.; Parker, D. Biochemistry of exercise-induced metabolic acidosis. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2004, 287, R502–R516. [Google Scholar] [CrossRef] [PubMed]
- Enoka, R.M.; Duchateau, J. Muscle fatigue: What, why and how it influences muscle function. J. Physiol. 2008, 586, 11–23. [Google Scholar] [CrossRef]
- Allen, D.; Westerblad, H. Role of phosphate and calcium stores in muscle fatigue. J. Physiol. 2001, 536, 657–665. [Google Scholar] [CrossRef]
- Lorist, M.M.; Kernell, D.; Meijman, T.F.; Zijdewind, I. Motor fatigue and cognitive task performance in humans. J. Physiol. 2002, 545, 313–319. [Google Scholar] [CrossRef]
- Bigland-Ritchie, B.; Woods, J. Changes in muscle contractile properties and neural control during human muscular fatigue. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 1984, 7, 691–699. [Google Scholar] [CrossRef]
- Abbood, H.; Al-Nuaimy, W.; Al-Ataby, A.; Salem, S.A.; AlZubi, H.S. Prediction of driver fatigue: Approaches and open challenges. In Proceedings of the IEEE 2014 14th UK Workshop on Computational Intelligence (UKCI), Bradford, UK, 8–10 September 2014; pp. 1–6. [Google Scholar]
- Halson, S.L. Monitoring training load to understand fatigue in athletes. Sports Med. 2014, 44, 139–147. [Google Scholar] [CrossRef]
- Bosquet, L.; Léger, L.; Legros, P. Blood lactate response to overtraining in male endurance athletes. Eur. J. Appl. Physiol. 2001, 84, 107–114. [Google Scholar] [CrossRef]
- Stoudemire, N.M.; Wideman, L.; Pass, K.A.; Mcginnes, C.L.; Gaesser, G.A.; Weltman, A. The validity of regulating blood lactate concentration during running by ratings of perceived exertion. Med. Sci. Sports Exerc. 1996, 28, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, Y.; Takeuchi, T.; Hosoi, T.; Yoshizaki, H.; Loeppky, J.A. Effect of a marathon run on serum lipoproteins, creatine kinase, and lactate dehydrogenase in recreational runners. Res. Q. Exerc. Sport 2005, 76, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Crewe, H.; Tucker, R.; Noakes, T.D. The rate of increase in rating of perceived exertion predicts the duration of exercise to fatigue at a fixed power output in different environmental conditions. Eur. J. Appl. Physiol. 2008, 103, 569. [Google Scholar] [CrossRef] [PubMed]
- Robson-Ansley, P.J.; Gleeson, M.; Ansley, L. Fatigue management in the preparation of Olympic athletes. J. Sports Sci. 2009, 27, 1409–1420. [Google Scholar] [CrossRef] [PubMed]
- Billat, L.V.; Koralsztein, J.P. Significance of the velocity at VO 2max and time to exhaustion at this velocity. Sports Med. 1996, 22, 90–108. [Google Scholar] [CrossRef]
- Cannon, D.T.; White, A.C.; Andriano, M.F.; Kolkhorst, F.W.; Rossiter, H.B. Skeletal muscle fatigue precedes the slow component of oxygen uptake kinetics during exercise in humans. J. Physiol. 2011, 589, 727–739. [Google Scholar] [CrossRef]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the physiological and biochemical profile of the athlete. NPJ Digit. Med. 2019, 2, 1–16. [Google Scholar] [CrossRef]
- Op De Beéck, T.; Meert, W.; Schütte, K.; Vanwanseele, B.; Davis, J. Fatigue prediction in outdoor runners via machine learning and sensor fusion. In Proceedings of the 24th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, London, UK, 19–23 August 2018; pp. 606–615. [Google Scholar]
- Jebelli, H.; Lee, S. Feasibility of Wearable Electromyography (EMG) to Assess Construction Workers’ Muscle Fatigue. In Advances in Informatics and Computing in Civil and Construction Engineering; Mutis, I., Hartmann, T., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 181–187. [Google Scholar]
- U.S. Bureau of Labor Statistics. Nonfatal occupational injuries and illnesses requiring days away from work. In Technical Report USDL-16-2130; United States Department of Labor: Washington, DC, USA, 2016; pp. 1–4. [Google Scholar]
- Leigh, J.P. Economic Burden of Occupational Injury and Illness in the United States. Milbank Q. 2011, 89, 728–772. [Google Scholar] [CrossRef]
- Orizio, C.; Gobbo, M.; Diemont, B.; Esposito, F.; Veicsteinas, A. The surface mechanomyogram as a tool to describe the influence of fatigue on biceps brachii motor unit activation strategy. Historical basis and novel evidence. Eur. J. Appl. Physiol. 2003, 90, 326–336. [Google Scholar] [CrossRef]
- Smith, I.C.H.; Newham, D.J. Fatigue and functional performance of human biceps muscle following concentric or eccentric contractions. J. Appl. Physiol. 2007, 102, 207–213. [Google Scholar] [CrossRef][Green Version]
- Sadoyama, T.; Miyano, H. Frequency analysis of surface EMG to evaluation of muscle fatigue. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 47, 239–246. [Google Scholar] [CrossRef]
- Adirim, T.A.; Cheng, T.L. Overview of injuries in the young athlete. Sports Med. 2003, 33, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Burt, C.W.; Overpeck, M.D. Emergency visits for sports-related injuries. Ann. Emerg. Med. 2001, 37, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A.M.; Jebb, S.A. Beyond body mass index. Obes. Rev. 2001, 2, 141–147. [Google Scholar] [CrossRef]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998; pp. 1–97. [Google Scholar]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sport Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Yoo, S.; Ackad, C.; Heywood, T.; Kay, J. Evaluating the actual and perceived exertion provided by virtual reality games. In Proceedings of the 2017 CHI Conference Extended Abstracts on Human Factors in Computing Systems, Denver, CO, USA, 6–11 May 2017; pp. 3050–3057. [Google Scholar]
- Lee, C.B.; Eun, D.; Kim, K.H.; Park, J.W.; Jee, Y.S. Relationship between cardiopulmonary responses and isokinetic moments: The optimal angular velocity for muscular endurance. J. Exerc. Rehabil. 2017, 13, 185. [Google Scholar] [CrossRef] [PubMed]
- González-Badillo, J.J.; Yañez-García, J.M.; Mora-Custodio, R.; Rodríguez-Rosell, D. Velocity loss as a variable for monitoring resistance exercise. Int. J. Sports Med. 2017, 38, 217–225. [Google Scholar] [CrossRef]
- Morán-Navarro, R.; Martínez-Cava, A.; Sánchez-Medina, L.; Mora-Rodríguez, R.; González-Badillo, J.J.; Pallarés, J.G. Movement velocity as a measure of level of effort during resistance exercise. J. Strength Cond. Res. 2019, 33, 1496–1504. [Google Scholar] [CrossRef]
- Kuhn, M. Building predictive models in R using the caret package. J. Stat. Softw. 2008, 28, 1–26. [Google Scholar] [CrossRef]
- Zhou, S.; Ogihara, A.; Nishimura, S.; Jin, Q. Analysis of Health and Physiological Index Based on Sleep and Walking Steps by Wearable Devices for the Elderly. In Proceedings of the 2017 IEEE 10th Conference on Service-Oriented Computing and Applications (SOCA), Kanazawa, Japan, 22–25 November 2017; pp. 245–250. [Google Scholar]
- Alsheikh, M.A.; Selim, A.; Niyato, D.; Doyle, L.; Lin, S.; Tan, H.P. Deep activity recognition models with triaxial accelerometers. In Proceedings of the Workshops at the Thirtieth AAAI Conference on Artificial Intelligence, Phoenix, AZ, USA, 12–17 February 2016. [Google Scholar]
- Xu, L.; Yang, W.; Cao, Y.; Li, Q. Human activity recognition based on random forests. In Proceedings of the 2017 IEEE 13th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD), Guilin, China, 29–31 July 2017; pp. 548–553. [Google Scholar]
- Jeong, G.M.; Truong, P.H.; Choi, S.I. Classification of three types of walking activities regarding stairs using plantar pressure sensors. IEEE Sens. J. 2017, 17, 2638–2639. [Google Scholar] [CrossRef]
- Soro, A.; Brunner, G.; Tanner, S.; Wattenhofer, R. Recognition and repetition counting for complex physical exercises with deep learning. Sensors 2019, 19, 714. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Sawchuk, A.A. A feature selection-based framework for human activity recognition using wearable multimodal sensors. In Proceedings of the 2011 6th International Conference on Body Area Networks (BodyNets ’11), ICST (Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering), Brussels, Belgium, 7–8 November 2011; pp. 92–98. [Google Scholar]
- Suto, J.; Oniga, S.; Sitar, P.P. Feature analysis to human activity recognition. Int. J. Comput. Commun. Control 2017, 12, 116–130. [Google Scholar] [CrossRef]
- Al-Mulla, M.R.; Sepulveda, F.; Colley, M. An autonomous wearable system for predicting and detecting localised muscle fatigue. Sensors 2011, 11, 1542–1557. [Google Scholar] [CrossRef] [PubMed]
- Subasi, A.; Kiymik, M.K. Muscle fatigue detection in EMG using time–frequency methods, ICA and neural networks. J. Med. Syst. 2010, 34, 777–785. [Google Scholar] [CrossRef]
- Lan, N.; Feng, H.Q.; Crago, P.E. Neural network generation of muscle stimulation patterns for control of arm movements. IEEE Trans. Rehabil. Eng. 1994, 2, 213–224. [Google Scholar]
- González-Izal, M.; Malanda, A.; Gorostiaga, E.; Izquierdo, M. Electromyographic models to assess muscle fatigue. J. Electromyogr. Kinesiol. 2012, 22, 501–512. [Google Scholar] [CrossRef]
- Ghazal, M.; Haeyeh, Y.A.; Abed, A.; Ghazal, S. Embedded Fatigue Detection Using Convolutional Neural Networks with Mobile Integration. In Proceedings of the IEEE 2018 6th International Conference on Future Internet of Things and Cloud Workshops (FiCloudW), Barcelona, Spain, 6–8 August 2018; pp. 129–133. [Google Scholar]
- Koutsos, E.; Cretu, V.; Georgiou, P. A Muscle Fibre Conduction Velocity Tracking ASIC for Local Fatigue Monitoring. IEEE Trans. Biomed. Circuits Syst. 2016, 10, 1119–1128. [Google Scholar] [CrossRef][Green Version]
- Mokaya, F.; Lucas, R.; Noh, H.Y.; Zhang, P. Burnout: A wearable system for unobtrusive skeletal muscle fatigue estimation. In Proceedings of the IEEE 2016 15th ACM/IEEE International Conference on Information Processing in Sensor Networks (IPSN), Vienna, Austria, 11–14 April 2016; pp. 1–12. [Google Scholar]
- Triwiyanto, T.; Wahyunggoro, O.; Nugroho, H.A.; Herianto, H. Muscle fatigue compensation of the electromyography signal for elbow joint angle estimation using adaptive feature. Comput. Electr. Eng. 2018, 71, 284–293. [Google Scholar] [CrossRef]

| Perceived Exertion | Borg Rating | Examples |
|---|---|---|
| None | 6 | Reading a book, watching television |
| Very, very light | 7 to 8 | Tying shoes |
| Very light | 9 to 10 | Chores like folding clothes that seem to take little effort |
| Fairly light | 11 to 12 | Walking through the grocery store (without speeding up your breathing) |
| Somewhat hard | 13 to 14 | Brisk walking (moderate effort and speeding up your breathing) |
| Hard | 15 to 16 | Bicycling, swimming, (vigorous effort and get the heart pounding) |
| Very hard | 17 to 18 | The highest level of activity you can sustain |
| Very, very hard | 19 to 20 | A finishing kick in a race or activity that you cannot maintain for long |
| Axis-Sensor | 2nd Set | 3rd Set | 4th Set | 5th Set | Avg. |
|---|---|---|---|---|---|
| X-Gyroscope | +2.0% | +6.0% | +17.0% | +33.0% | +14.5% |
| Z-Gyroscope | +1.7% | +11.0% | +15.0% | +45.0% | +18.2% |
| Y-Accelerometer | +1.5% | +7.4% | +11.0% | +15.0% | +8.7% |
| ine Avg./set | +1.7% | +8.1% | +14.3% | +31.0% |
| Axis-Sensor | 2nd Set | 3rd Set | 4th Set | 5th Set | Avg. |
|---|---|---|---|---|---|
| X-Gyroscope | +0.7% | +1.2% | −6.3% | −5.2% | −2.4% |
| Z-Gyroscope | +0.5% | +1.7% | −10.4% | −7.5% | −3.9% |
| Y-Accelerometer | +0.6% | +0.3% | +0.3% | +0.4% | 0.4% |
| ine Avg./set | +0.6% | +1.1% | −5.5% | −4.1% |
| Actual | |||
|---|---|---|---|
| Fatigue ∈ [17,20] | Non-Fatigue ∈ [6,16] | ||
| Predict | Fatigue ∈ [17,20] | TRUE Fatigue | FALSE Fatigue |
| Non-Fatigue ∈ [6,16] | FALSE Non-Fatigue | TRUE Non-Fatigue | |
| Fatigue Subset | Complete Dataset | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | AAD | Mean | SD | AAD | |||
| Sensors and Axes | Gyro. | X-axis | × | × | × | × | × | × |
| Y-axis | ✓ | × | ✓ | ✓ | ✓ | × | ||
| Z-axis | ✓ | ✓ | ✓ | ✓ | ✓ | × | ||
| Mag. | X-axis | × | × | × | × | × | × | |
| Y-axis | × | ✓ | × | × | × | × | ||
| Z-axis | × | × | ✓ | × | ✓ | ✓ | ||
| Acc. | X-axis | ✓ | ✓ | ✓ | × | × | × | |
| Y-axis | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Z-axis | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Total | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Ex. Force | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Models | Subject-Specific | |||
|---|---|---|---|---|
| Precision | Recall | Accuracy | F1 | |
| GLM | 86% | 83% | 84% | 84% |
| LR | 81% | 77% | 79% | 79% |
| RF | 78% | 76% | 76% | 77% |
| DT | 66% | 61% | 58% | 63% |
| FNN | 95% | 93% | 94% | 94% |
| Models | Cross-Subject | |||
|---|---|---|---|---|
| Precision | Recall | Accuracy | F1 | |
| GLM | 78% | 71% | 75% | 74% |
| LR | 73% | 74% | 76% | 73% |
| RF | 69% | 73% | 70% | 71% |
| DT | 47% | 49% | 43% | 48% |
| FNN | 87% | 89% | 88% | 88% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elshafei, M.; Shihab, E. Towards Detecting Biceps Muscle Fatigue in Gym Activity Using Wearables. Sensors 2021, 21, 759. https://doi.org/10.3390/s21030759
Elshafei M, Shihab E. Towards Detecting Biceps Muscle Fatigue in Gym Activity Using Wearables. Sensors. 2021; 21(3):759. https://doi.org/10.3390/s21030759
Chicago/Turabian StyleElshafei, Mohamed, and Emad Shihab. 2021. "Towards Detecting Biceps Muscle Fatigue in Gym Activity Using Wearables" Sensors 21, no. 3: 759. https://doi.org/10.3390/s21030759
APA StyleElshafei, M., & Shihab, E. (2021). Towards Detecting Biceps Muscle Fatigue in Gym Activity Using Wearables. Sensors, 21(3), 759. https://doi.org/10.3390/s21030759






