Abstract
Advancements in motion sensing technology can potentially allow clinicians to make more accurate range-of-motion (ROM) measurements and informed decisions regarding patient management. The aim of this study was to systematically review and appraise the literature on the reliability of the Kinect, inertial sensors, smartphone applications and digital inclinometers/goniometers to measure shoulder ROM. Eleven databases were screened (MEDLINE, EMBASE, EMCARE, CINAHL, SPORTSDiscus, Compendex, IEEE Xplore, Web of Science, Proquest Science and Technology, Scopus, and PubMed). The methodological quality of the studies was assessed using the consensus-based standards for the selection of health Measurement Instruments (COSMIN) checklist. Reliability assessment used intra-class correlation coefficients (ICCs) and the criteria from Swinkels et al. (2005). Thirty-two studies were included. A total of 24 studies scored “adequate” and 2 scored “very good” for the reliability standards. Only one study scored “very good” and just over half of the studies (18/32) scored “adequate” for the measurement error standards. Good intra-rater reliability (ICC > 0.85) and inter-rater reliability (ICC > 0.80) was demonstrated with the Kinect, smartphone applications and digital inclinometers. Overall, the Kinect and ambulatory sensor-based human motion tracking devices demonstrate moderate–good levels of intra- and inter-rater reliability to measure shoulder ROM. Future reliability studies should focus on improving study design with larger sample sizes and recommended time intervals between repeated measurements.
1. Introduction
The clinical examination of individuals with shoulder pathology routinely involves the measurement of range-of-motion (ROM) to diagnose, evaluate treatment, and assess disease progression [1,2,3]. The shoulder complex involves the coordination of the acromioclavicular, glenohumeral and scapulothoracic joints, to allow motion in three biomechanical planes, specifically the sagittal, coronal, and axial planes [4]. Forward flexion and elevation occur in the sagittal plane; abduction and adduction occur in the coronal plane; and internal and external rotation occur along the long axis of the humerus [5].
The shoulder joint’s complex multiplanar motion presents a challenge for clinicians to accurately measure ROM and upper limb kinematics [6,7]. Prior attempts to implement a global coordinate system to describe shoulder movement and define arm positions in space [8] have failed to gain clinical consensus due to practical difficulties. The biomechanical complexity of the shoulder is demonstrated by the synergy of movements necessary for a person to perform activities of daily living. Activities such as reaching for a high shelf or hair washing requires a combination of flexion and adduction. Similarly, reaching behind the back pocket requires a combination of internal rotation, extension, and adduction. Although many models have been proposed in literature, it nevertheless remains difficult to determine the contribution of individual components of glenohumeral joint and scapulothoracic joint motions. Therefore, the reliability of any tools used for ROM measurement is important for clinicians to make informed decisions regarding patient management [9].
According to the American Academy of Orthopaedic Surgeons (AAOS), normal active ROM of the shoulder is 180° for flexion and abduction, and 90° for external rotation [10]. However, a number of age and health-related variables exist that can influence shoulder ROM, including factors such as gender, work history, and hand-dominance. Studies have demonstrated an overall reduction in ROM across all shoulder movements with age in subjects with no shoulder pathology [11,12]. Gill et al. [13] reported age-related decreases in right active shoulder flexion by 43° in males, and 40.6° in females, and right active shoulder abduction by 39.5° and 36.9°, respectively. Authors also noted a decline in external rotation range, particularly among females. The age-related causes of decreased ROM occur from sarcopenia (loss of muscle mass due to a decrease in Type-II fibres), changes in fat redistribution and slower collagen fibre reproduction, leading to reduced elasticity and shortened ligaments and tendons [14,15].
A goniometer is the most commonly used instrument by clinicians to measure joint position and ROM [16,17]. It is essentially a 360° protractor, comprising a stationary arm, a movable arm, and a fulcrum. When used correctly by a trained clinician, the benefits of goniometry’s low cost and portability [18,19] are offset by the disadvantages of low inter-reliability [20,21] and measurement variability between clinicians [22,23,24,25]. Furthermore, the two-handed requirement of using a goniometer makes it difficult to stabilise the trunk and scapula, resulting in an increased likelihood of measurement error [26]. Alternatively, inclinometers measure ROM relative to the line of gravity and demonstrate improved inter-rater reliability compared with goniometry when assessing shoulder measurements [27,28]. The drawbacks of inclinometery include higher cost, poorer accessibility, and possible technical errors due to misplacing body landmarks or not sustaining constant pressure with the device during movements.
With the increasing popularity, accessibility, and convenience of smartphones and similar devices [29], the potential exists for these electronics to become a clinician’s measuring tool of choice. Smartphones with inbuilt accelerometers and magnetometers can utilise inclinometer or sensor-based applications to calculate shoulder joint angles [30,31,32]. Similarly, digital inclinometers or goniometers are compact, portable, and lightweight. However, a degree of training is required for the clinician to accurately determine a zero point and limit measurement error [33]. Although more costly than traditional manual methods, digital inclinometers and smartphones eliminate the need for realignment and require only one hand to operate [34]. Additionally, the ability to transmit measurements may decrease transpositional or other manual entry errors.
Further advancements in technology over the last decade have led researchers to adopt hands-free motion sensing input devices to estimate human joint ROM [35]. The Microsoft Kinect sensor was originally developed as an add-on for the Xbox 360 gaming console (Microsoft Corp., Redmond, WA, USA) [36] and has since been modified for application in real-world settings including telehealth [37,38], education [39,40] and kinematic motion analysis [41,42,43]. The Kinect sensor combines a regular colour camera with a depth camera that comprises an infrared laser projector and infrared camera. The Windows Software Development Kit (SDK) 2.0 has allowed for the creation of applications that utilise the Kinect’s gesture recognition capability to implement joint orientation and skeletal tracking for 25 joint positions in the standing or seated positions [44,45]. Given its potential breadth of use, the Kinect is emerging as a promising clinical tool for kinematic analysis by virtue of its function as a markerless system to estimate the 3-D positions of several body joints [46].
Ambulatory sensor-based human motion tracking devices such as inertial measurement units (IMUs) comprise accelerometers, gyroscopes, and magnetometers. IMUs measure linear acceleration and angular velocities, combining data to obtain a 3-D position and orientation of a body [47]. The miniaturisation, wearability, and low cost of IMUs over the last decade has made it a desirable alternative to expensive motion-capturing systems for measuring joint angles [48,49,50]. Prior studies evaluating the precision of IMUs have reported mean average errors of <5.0° for upper limb measurements [51,52,53]. However, IMU accuracy varies depending on the amount of ROM a joint can produce [53], type of device [54], and fusion algorithm used [55].
Prior to using any device for ROM assessment in clinical practice, it is important to establish the measurement properties of validity and reliability [56]. Several studies have previously validated the Microsoft Kinect [57,58,59,60], IMUs [61,62,63], digital inclinometers [64,65,66,67] and smartphone applications [68,69,70] against a prescribed “gold standard” for shoulder ROM measurement.
For the purposes of this review, authors examined reliability, reflecting the degree to which measurements are consistent over time and across different observers or raters [71]. The two recognised types of reliability in the literature are: intra-rater reliability—the amount of agreement between repeated measurements of the same joint position or ROM by a single rater, and inter-rater reliability—the amount of agreement between repeated measurements of the same joint position or ROM by multiple raters [72].
Absolute reliability is considered equally important and indicates the amount of variability for repeated measurements between individuals [73,74]. Examples include the standard error of measurement (SEM), coefficient of variation (CV), and Bland and Altman’s 95% limits of agreement [74]. Absolute measures of reliability allow clinicians to evaluate the level of measurement error and determine whether any changes in ROM signify a real change in their patients [75,76].
Few studies have summarised or appraised the literature on the reliability of the Microsoft Kinect, IMUs, smartphones, and digital inclinometers for human joint ROM measurement. Previous systematic reviews have focused on applying the Kinect for stroke rehabilitation [77,78,79], and Parkinson’s disease [80,81,82]. Only one systematic review on reliability was identified, which examined using the Kinect to assess transitional movement and balance [83]. To our knowledge, no systematic appraisals of studies on the intra- and inter-rater reliability of the Kinect and ambulatory sensor-based motion tracking devices for shoulder ROM measurement have been conducted.
Therefore, the aim of this article is to review systematically, and appraise critically, the literature investigating the reliability of the Kinect and ambulatory sensor-based motion tracking devices for measuring shoulder ROM.
The specific study questions for this systematic review were:
- What is the intra- and inter-rater reliability of using the Microsoft Kinect, inertial sensors, smartphone applications, and digital inclinometers to calculate a joint angle in the shoulder?
- What are the types of inertial sensors, smartphone applications, and digital inclinometers currently used to calculate a joint angle in the shoulder?
- What clinical populations are utilising motion-tracking technology to calculate the joint angle in the shoulder?
- Which anatomical landmarks are used to assist the calculation of joint angle in the shoulder?
2. Materials and Methods
The protocol for this review was devised in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines [84], published with PROSPERO on the 8 December 2017 (CRD 42017081870).
The search strategy was developed and refined by previous systematic reviews investigating reliability [85,86]. A database search of Medline (via OvidSP), EMBASE (via OvidSP), EMCARE (via Elsevier), CINAHL (via Ebsco), SPORTSDiscus (via Ebsco), Compendex (via Engineering Village), IEEE Xplore (via IEEE), Web of Science (via Thomson Reuters), Proquest Science and Technology (via Proquest), Scopus (via Elsevier), and Pubmed was initially performed on 30 January 2020 by two independent reviewers (PB, DB). These databases were searched from their earliest records to 2020. An updated search was completed on 17 December 2020. Details of the search strategy are found in Supplementary S1. The reference lists of all included studies were screened manually for additional papers that met the a priori inclusion criteria.
2.1. Inclusion and Exclusion Criteria
Studies were included if they met the following criteria: published in peer-reviewed journals; measured human participants of all ages; used the Microsoft Kinect, inertial sensors, smartphone applications, or digital inclinometers to measure joint ROM of the shoulder joint and assessed the intra- and/or inter-rater reliability of these devices; published in English and had full text available. Case studies, abstracts only and “grey” literature was not included. Studies only investigating validity, scapular or functional shoulder movements were excluded, as the aim of the review was to examine the reliability of specific shoulder joint movements commonly measured in clinical practice.
The titles and abstracts of studies were retrieved using the search strategy (Supplementary S1) and screened independently by two review authors (PB, DB). Full text versions that met the selection criteria were uploaded to an online systematic review program (Covidence) for independent review by both reviewers (PB, DB). Any disagreements on eligibility were initially resolved by discussion between reviewers and resolved by a third reviewer (WRW), if necessary.
2.2. Data Extraction
A standardised, pre-piloted form was used to extract data from the included studies for assessment of study quality and evidence synthesis. The following information was extracted for each study: bibliometric (author, title, year of publication, funding sources); study methods (study design, country, setting, description and number of raters, type of shoulder joint movements; type of movement (active ROM (aROM) or passive (pROM)); number of sessions, session interval, type and description of technology); participants (recruitment source, number of drop outs, sample size, age, gender inclusion criteria); anatomical landmarks, statistical methods (type of reliability), and outcomes (intraclass correlation coefficient (ICC) values).
2.3. Evaluation of Reliability Results
Reliability was assessed using ICCs; an ICC value approaching 1 was indicative of higher reliability. The level of intra- and inter-rater reliability was determined by the criteria identified by Swinkels et al. [87]. Intra-rater reliability was considered good with an ICC > 0.85, moderate with ICCs 0.65–0.85, and poor with an ICC < 0.65. Inter-rater reliability was considered good with an ICC > 0.80, moderate with ICCs 0.60–0.80, and poor with an ICC < 0.60.
2.4. Evaluation of the Methodological Quality of the Studies
The two review authors independently assessed the methodological quality of each included paper using the latest (2020) Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) Risk of Bias tool [88]. The studies were rated against a specific set of criteria, with nine items assessing reliability standards and eight items assessing measurement error standards. To satisfy item seven of the measurement error standards, the study had to report absolute reliability statistics (standard error of measurement (SEM), smallest detectable change (SDC) or Limits of Agreement (LOA)). Each item was graded on a four-point scale as either very good, adequate, doubtful, or inadequate. The worst-score-count method was applied in accordance with the COSMIN protocol; the overall score was determined by the lowest score awarded for the measurement property, as used in previous studies [89,90].
2.5. Data Analysis
Meta-analyses of relative intra- and inter-rater reliability were performed for studies with outcome measures that reported comparable data. Pooled analysis was completed for maximal aROM and pROM. The right-hand dominant value for the healthy, asymptomatic population was included for analysis. Studies with multiple reliability values were pooled and one overall mean result was reported. If a single study reported values for more than one rater, the mean value was reported. Reflecting clinical practice, any reliability values taken in supine position were included in the pROM analysis, and the standing or sitting positions were included in the aROM analysis.
3. Results
3.1. Flow of Studies
A flowchart of the different stages of the article selection process is outlined in Figure 1. From the 2006 studies identified, 32 studies [91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122] were found to meet the criteria for inclusion. In total, nine studies reported reliability for the Microsoft Kinect; six studies for wearable inertial sensors; seven studies for smartphone/mobile applications; and ten studies for digital inclinometers or goniometers.
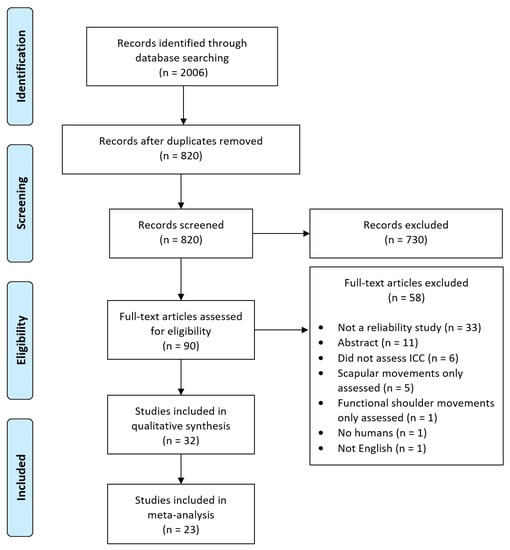
Figure 1.
Flow chart of the systematic review process.
3.2. Description of Studies
The characteristics of the included studies are summarised in Table 1. A total of 1117 participants were included in this review, with a mean age ranging from 17.0 to 56.1 years of age. The mean sample size was 35 participants with a considerable range (minimum, 1; maximum 155) and variance (SD, 32.1). Six studies recruited more than 50 participants and five studies recruited fewer than ten participants. In 13 of the studies, there was a higher percentage of women compared to men. Most studies (n = 26) recruited participants who were healthy and asymptomatic. Participants with shoulder pain or pathology were reported in six studies.

Table 1.
Characteristics of studies included in this review.
A physical therapist (PT) was the most reported type of rater (n = 12 studies). In six studies the rater was a medical practitioner (MP), and in two studies a PT student was the sole primary rater. Thirteen studies did not report the profession of the rater.
The shoulder movements assessed across all studies included flexion, extension, abduction, external rotation, internal rotation, and scaption. A total of 24 studies only assessed aROM; eight studies assessed pROM, and two assessed both. The most common measuring position was standing (n = 10 studies), followed by seated (n = 6 studies) and supine (n = 3 studies). There were twelve studies that used a combination of supine and standing, side-lying, prone or seated positions. Only one study did not report the position used.
The majority of studies (n = 25) reported two sessions; five studies had one session, and two studies involved three sessions. The time interval between assessments varied considerably from 10 s to 7 days. The most common consecutive measurements were on the same day (n = 13) followed by 7 days (n = 5).
3.3. Intra and Inter-Rater Reliability
Results for intra- and inter-rater reliability are shown in Table 2. The last column of Table 2 indicates the level of reliability, grouped by type of device, and includes the shoulder movement assessed.

Table 2.
Intra-rater and Inter-rater reliability (95% CI) for measurement of shoulder range of motion by device and movement direction.
3.3.1. The Microsoft Kinect
Six studies assessed intra-rater reliability [93,94,99,105,106,107], one study assessed inter-rater reliability [112] and another study assessed both [101]. Two studies reported good intra-rater reliability (ICC > 0.85) for all shoulder movements [105,107]. The remaining four studies reported varying levels of intra-rater reliability, ranging from poor (ICC < 0.65), moderate (ICC 0.65–0.85) to good, dependent on the shoulder movements assessed. Shoulder external and internal rotation demonstrated moderate to good levels of intra-rater reliability [94,99,106]. Two studies reported good inter-rater reliability (ICC > 0.80) for shoulder flexion, extension, and abduction [101,112]. Intra-rater reliability for coupling inertial sensors with the Kinect was moderate to good for flexion, and poor to moderate for abduction [92].
3.3.2. Inertial Sensors
One study assessed intra-rater reliability [114], three studies assessed inter-rater reliability [96,117,118] and two studies assessed both [100,102]. Three studies reported moderate to good intra-rater reliability using one, two or four wearable inertial sensors [100,102,114]. Inter-rater reliability was good or moderate in four studies for shoulder flexion, extension, abduction, external and internal rotation [96,102,117,118]. A wider range of poor (ICC < 0.60) to good inter-rater reliability was reported in two studies for shoulder abduction, external and internal rotation [100,102].
3.3.3. Smartphone/Mobile Applications
A total of five of seven studies [95,110,113,116,120] assessed intra-rater and inter-rater reliability. All shoulder movements across most of the studies demonstrated moderate or good levels of intra- and inter-rater reliability. Only one study reported a wider range of reliability values, between poor and good, for flexion and scaption [116].
3.3.4. Digital Inclinometer/Goniometer
Two studies assessed intra-rater reliability [104,121], one study assessed inter-rater reliability [103], and seven studies assessed both [91,97,98,108,109,115,119]. Intra-rater reliability was predominately moderate to good for all shoulder movements (n = 7). Two studies reported poor to moderate intra-rater reliability for external and internal rotation [91,104]. Poor inter-rater reliability was reported in five studies [91,103,108,115,119]. Only two studies reported good intra- and inter-rater reliability for all shoulder movements [97,109].
3.4. Methodological Evaluation of the Measurement Properties
Of the thirty-two included studies, only two [109,110] scored very good on all items of the COSMIN reliability standards checklist. A total of 24 studies scored adequate, five were rated doubtful and one was rated inadequate. Table 3 lists the COSMIN standards of reliability checklist and all subsequent scores.

Table 3.
Assessment of reliability using the COSMIN standards for studies on reliability checklist.
Using the COSMIN criteria, only one study [109] was found to have a very good score on all items for the measurement error standards. A total of 18 studies scored adequate, with two rated doubtful and 11 rated inadequate. Table 4 lists all items of the COSMIN standards on measurement error checklist and the subsequent paper scores.

Table 4.
Assessment of measurement error using the COSMIN standards for studies on measurement error checklist.
3.5. Synthesis of Results (Meta-Analysis)
ICC values were included from studies with n > 1 participant included in intra- and inter-rater reliability analysis. The ICC values for outcome measures (aROM or pROM for abduction, flexion, internal rotation, external rotation) were individually assessed based on motion and grouped by method (K, SP, DG, DI and IS) to produce a pooled correlation with a 95%CI (Figure 2, Figure 3 and Figure 4).
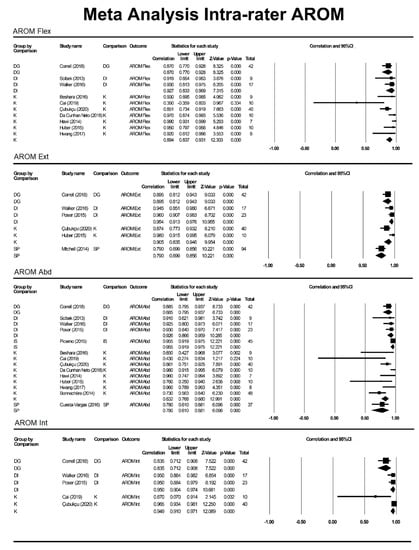
Figure 2.
Meta-analysis for intra-rater AROM. DG = digital goniometer, DI = digital inclinometer, IS = inertial sensor, K = Kinect, SP = smartphone, Abd = abduction, AROM = active range of motion, Int = internal rotation, Ext = external rotation.
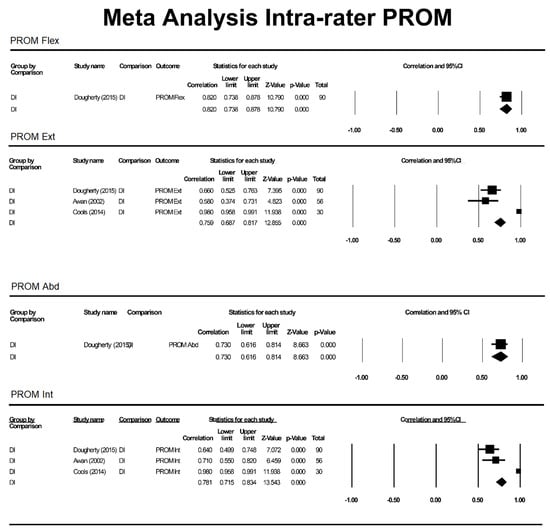
Figure 3.
Meta-analysis for intra-rater pROM. DI = digital inclinometer, PROM = passive range of motion, Flex = flexion, Int = internal rotation, Ext = external rotation.
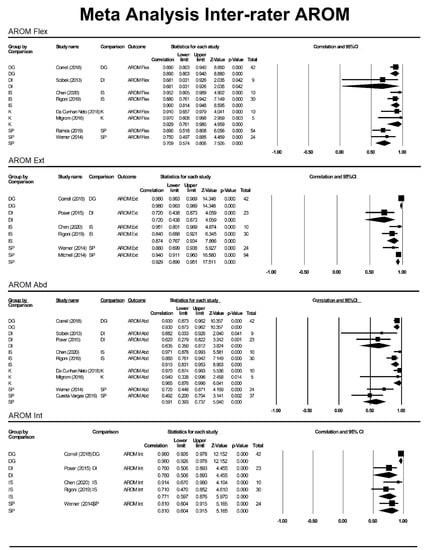
Figure 4.
Meta-analysis for inter-rater aROM. DG = digital goniometer, DI = digital inclinometer, IS = inertial sensor, K = Kinect, SP = smartphone, Abd = abduction, Int = internal rotation.
3.6. Anatomical Landmarks
Twenty-three studies identified the anatomical landmarks for each device and are summarised in Table 5. A total of six studies reported using a vector from the shoulder joint to the elbow for the Microsoft Kinect [92,93,94,105].

Table 5.
Anatomical landmarks by device.
Five studies identified the anatomical landmarks for inertial sensor placement [100,102,114,117,118]. All studies used a sensor located on the upper arm that was either unspecified (n = 2), placed on the middle third of the humerus (n = 3), or attached 10 cm distal to the lateral epicondyle (n = 1). Two studies placed a sensor on the flat part of the sternum [100,102]. Only two studies reported using a lower arm sensor on the wrist [102,118].
Anatomical positions for smartphone device placement were described in five studies [95,110,111,113,120]. The most common attachment was on the humerus (n = 3) followed by positions at the wrist (n = 2).
Seven studies reported anatomical landmarks for digital inclinometers [98,104,108,109,115,119,121]. Locations were predominately determined by the type of shoulder movement performed, orientation, and assessment position.
4. Discussion
Thirty-two studies investigating four different types of devices were included in this review. A thorough search of relevant literature found no previous systematic review of intra-rater and inter-rater reliability of the Microsoft Kinect and ambulatory sensor-based motion tracking devices to measure shoulder ROM.
Good intra-rater reliability for multiple types of shoulder movement was demonstrated with the Kinect [105,107], smartphone applications [95], and digital inclinometers [97]. The Kinect consistently demonstrated higher intra-rater ICC values over other devices for all shoulder movements. Only one study reported poor intra-rater reliability for measuring shoulder extension with the Kinect [99]. Overall, inertial sensors, smartphones, and digital inclinometers demonstrated moderate to good intra-rater reliability across all shoulder movements.
Good inter-rater reliability for more than one type of shoulder movement was demonstrated with the Kinect [101,112], smartphone applications [95,111], and a digital inclinometer/goniometer [97,98]. Inertial sensors predominately exhibited moderate to good inter-rater reliability across all types of shoulder movements. Broader ranges of inter-rater reliability (between poor to moderate) were more commonly reported with digital goniometers.
4.1. Quality of Evidence
All included studies and measurement properties were assessed for their methodological quality using the COSMIN tool. The methodological quality ranged from doubtful to very good for reliability standards. The strict COSMIN criteria of using the worst-score counts to denote the overall score resulted in only two very good studies [109,110], which reported moderate or good reliability for using a digital inclinometer and a smartphone device. An adequate rating was scored by five studies for the Kinect, six studies for inertial sensors, five studies for smartphone applications, and eight studies for digital inclinometers/goniometers.
Five studies missed achieving an overall very good rating due to receiving only an adequate score for the time interval between measurements (COSMIN item two). The authors acknowledge an appropriate time interval depends on the stability of the construct (COSMIN item one), and the target population [88]. The time interval must be adequately distanced to avoid recall bias, yet within a compact enough window to distinguish genuine differences in measurements from clinical change [123,124,125]. Studies had a time interval ranging from the same day (22/32) to 7 days (4/32) between two repeated measurements. Ideal time intervals of 2–7 days have been recommended to minimise the risk of a learning effect, random error, or other modifying factors that can affect the movement pattern [126,127].
Small sample sizes contributed to five studies scoring doubtful or inadequate, in accordance with COSMIN item six. An insufficient sample size may not detect true differences and reduces the power of the study to draw conclusions [128]. Of the 32 included studies, a power analysis for sample size calculation was reported in only four (12.5%) studies [97,98,100,104]. The latest COSMIN checklist has removed the standards for adequate sample sizes, as the authors suggested that several small high-quality studies can together provide good evidence for the measurement property [129]. The guidelines recommend a more nuanced approach that considers several factors including the type of ICC model. Studies with small sample sizes were considered acceptable if the authors justified the reasons outlining its adequacy [129]. Therefore, for methodological quality, reviewers scored sample sizes of 1 inadequate, ˂10 doubtful, <30 adequate and ≥30 very good. This criterion was based on literature citing a rule of thumb of recruiting 19–30 participants when conducting a reliability study [130,131,132].
With respect to measurement error assessment, just over one-half of the studies (18/32) scored adequate, and one scored very good for methodological quality. Eleven studies were rated inadequate, as they failed to calculate SEM, SDC, LoA or CV values (COSMIN item seven). Two studies [92,107] were rated doubtful due to minor methodological flaws (COSMIN item six); notably, this strict item offered reviewers no adequate option.
Reliability and measurement error are inextricably linked, and a highly reliable measurement contains little measurement error. A clinician can confidently verify real changes in patient status if the measured change from the last measurement is larger than the error associated with the measurement [133]. The minimal detectable clinical difference at a 90% confidence level (MDC90) is the minimal value to determine whether a change has occurred [72]. MDC values are open to interpretation and are based on clinical judgement. For shoulder ROM measurement, differences between observers which exceed 10° are deemed unacceptable for clinical purposes [103].
The Kinect and inertial sensors demonstrated low SEM and MDC values for measuring most types of shoulder movements [96,99,102,106]. Similarly, for the Kinect, low CV values (1.6%, 5.9%) were reported for shoulder abduction [93]. Smartphones had moderate SEM and MDC values, with better (smaller) errors demonstrated for intra-rater analysis [118], abduction and forward flexion [122], and higher target angles [116]. One study comparing smartphone measurements with universal goniometry, analysed Bland–Altman plots to indicate narrow LoA and excellent agreement, particularly for glenohumeral abduction [111]. Digital inclinometers demonstrated low MDC90 values, ranging from ≥2.82° to 5.47° [97], 4° to 9° [108], and 5° to 12° [121] for inter-rater analysis. Four studies reported acceptable differences between observers of <±10° [97,103,108,121] for most inclinometer measurements.
4.2. Clinical Implications
The Microsoft Kinect is an affordable depth imaging technology that can conveniently and reliably measure shoulder aROM. As a low-cost markerless system, the Kinect can provide clinicians with fast, real-time objective data to quantify shoulder kinematics. The Kinect’s visual feedback can aid in patient motivation by way of monitoring treatment and disease progression. The massive amounts of kinematic data generated allows clinicians to potentially analyse shoulder motion paths and correlate specific movement patterns to shoulder pathology [94]. Moreover, higher clinical efficiency arises from relying less on time and labour-intensive patient-reported outcome measures. The portability of the Microsoft Kinect over expensive motion capture systems permits its practical use in private clinics, rehabilitation centres, and home settings [107].
All studies were limited to motion performed along the anatomical planes. The simplicity of calculating the angles between two corresponding vectors does not take into account movements that occur outside the plane. In contrast to goniometric measurements, Lee et al. [60] found subjects could abduct their shoulders to a greater degree in front of the Kinect because their movements were not controlled in a given anatomical plane by an examiner. The authors performed a supplementary experiment that compared goniometric and Kinect shoulder measurements in rapid succession within three cardinal planes. Results demonstrated a significant decrease in 95% limit of agreement between both methods in all directions. It was concluded that the variability was due to the unrestricted motion of the Kinect.
With respect to reliability, one study reported lower repeatability with the Kinect in the frontal and transverse planes compared to the sagittal plane [94]. Another study reported large discrepancies for precise shoulder angle measurements with the Kinect [106].
Discrepancies between standing, sitting, and lying positions can also be a source of difference for shoulder ROM measurements [134,135]. One study [60] reported discrepancies between goniometric shoulder ROM measurements with seated subjects and Kinect ROM measurements for standing subjects. The authors attributed this result to the limitation of the Kinect’s skeletal tracking, which is optimised for standing rather than sitting. Moreover, better accuracy for the Kinect has been reported for standing postures [136]. Therefore, adequate patient positioning and protocol standardisations are essential to reduce measurement error [105]. Suggested examples include placing coloured footprints on the floor and fixating the Kinect sensor bar [105].
Wearability and usability are two aspects to consider for implementing sensor-based human motion tracking devices in clinical practice. For the included studies, IMUs were most often positioned on the upper arm with additional placements on the sternum and wrist. Methods of fixation included double-sided adhesive tape with an elastic cohesive [100], an elastic belt [114] and, velcro straps [118]. Smartphone devices were attached by commercial armbands [110,111,116,120] or were hand-held by the examiners [95,113,122]. Most notably, no studies reported any calibration issues, and only one study [111] reported attachment difficulties.
4.3. Limitations
There were some limitations in this review. First, no additional search was performed for grey literature, and only studies written in English were included. Although authors identified an additional six reliability studies, they were excluded because they did not assess ICCs.
Second, the authors acknowledge the limitations of the revised COSMIN methodological quality tool, as it was primarily developed to assess risk of bias and not study design. Although more user-friendly than the original version, the omission of a sample size criterion leaves open a wider interpretation as to what constitutes an adequate sample size. Furthermore, no standards exist regarding the types of patients, examiners (well-trained or otherwise), and testing procedures. Future studies can apply other tools such as the modified GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach to address these issues [137]. Additionally, because the revised COSMIN guidelines are relatively new update, caution should be exercised when interpreting and comparing these results with prior studies that used the original COSMIN checklist.
Third, our meta-analysis was limited by the heterogeneity of the studies, given the variance in sample sizes, protocols, shoulder positions, and number of raters. Several studies did not report the 95% confidence intervals for ICCs. Furthermore, the calculation methods for ROM angles with the Kinect represents a potential source of difference across studies. Therefore, the general conclusions should be interpreted with caution.
Lastly, for reasons mentioned earlier, the authors did not examine validity, the degree to which a tool measures what it claims to measure. However, given the potential variety and the lack of any agreed-upon “gold standard” tool identified in the literature, a separate review is warranted to address validity. Reliability should always be interpreted with validity in mind to provide a complete assessment of the clinical appropriateness of a measuring tool.
Future Directions
Future reliability studies should focus on improving study design, with larger sample sizes (>80 participants) [138] and set recommended time intervals (2–7 days) between repeated measurements to increase confidence with results. Moreover, further investigations should report on absolute measures of reliability or measurement error to improve the overall risk of bias.
5. Conclusions
The primary result of our systematic review is that the Kinect and ambulatory sensor-based human motion tracking devices demonstrate moderate to good levels of intra- and inter-rater reliability to measure shoulder ROM. The assessment of reliability is an initial step in recommending a measuring tool for clinical use. Future research including the Kinect and other devices should investigate validity in well-designed, high-quality studies.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/s21248186/s1. Supplementary S1: Full search strategy.
Author Contributions
Conceptualization, P.B., D.B.A. and W.R.W.; methodology, P.B. and D.B.A.; formal analysis, P.B., M.P.; investigation, P.B. and D.B.A.; writing—original draft preparation, P.B.; writing—review and editing, P.B., D.B.A., M.P. and W.R.W.; supervision, M.P. and W.R.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets presented in this study are openly available in [96,97,102,106].
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Warner, J.J. Frozen Shoulder: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 1997, 5, 130–140. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Valentine, R.E.; Lewis, J.S. Intraobserver reliability of 4 physiologic movements of the shoulder in subjects with and without symptoms. Arch. Phys. Med. Rehabil. 2006, 9, 1242–1249. [Google Scholar] [CrossRef] [PubMed]
- Green, S.; Buchbinder, R.; Glazier, R.; Forbes, A. Interventions for shoulder pain. Cochrane Database Syst. Rev. 2002, 2. [Google Scholar] [CrossRef]
- Kapandji, I.A. Physiology of the Joints, 5th ed.; Upper Limb; Churchill Livingston: Oxford, UK, 1982; Volume 1. [Google Scholar]
- Wu, G.; van der Helm, F.C.; Veeger, H.E.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. International Society of Biomechanics. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Tondu, B. Estimating Shoulder-Complex Mobility. Appl. Bionics Biomech. 2007, 4, 19–29. [Google Scholar] [CrossRef]
- Muir, S.W.; Corea, C.L.; Beaupre, L. Evaluating change in clinical status: Reliability and measures of agreement for the assessment of glenohumeral range of motion. N. Am. J. Sports Phys. Ther. 2010, 5, 98–110. [Google Scholar] [PubMed]
- Pearl, M.L.; Jackins, S.; Lippitt, S.B.; Sidles, J.A.; Matsen, F.A., 3rd. Humeroscapular positions in a shoulder range-of-motion-examination. J. Shoulder Elb. Surg. 1992, 6, 296–305. [Google Scholar] [CrossRef]
- dos Santos, C.M.; Ferreira, G.; Malacco, P.L.; Sabino, G.S.; Moraes, G.F.D.S.; Felicio, D.C. Intra and inter examiner reliability and measurement error of goniometer and digital inclinometer use. Rev. Bras. Med. Esporte 2012, 18, 38–41. [Google Scholar]
- American Academy of Orthopaedic Surgeons. Joint Motion: Method of Measuring and Recording; AAOS: Chicago, IL, USA, 1965. [Google Scholar]
- Barnes, C.J.; Van Steyn, S.J.; Fischer, R.A. The effects of age, sex, and shoulder dominance on range of motion of the shoulder. J. Shoulder Elb. Surg. 2001, 3, 242–246. [Google Scholar] [CrossRef]
- Roldán-Jiménez, C.; Cuesta-Vargas, A.I. Age-related changes analyzing shoulder kinematics by means of inertial sensors. Clin. Biomech. 2016, 37, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.K.; Shanahan, E.M.; Tucker, G.R.; Buchbinder, R.; Hill, C.L. Shoulder range of movement in the general population: Age and gender stratified normative data using a community-based cohort. BMC Musculoskelet. Disord. 2020, 21, 676. [Google Scholar] [CrossRef] [PubMed]
- Walston, J.D. Sarcopenia in older adults. Curr. Opin. Rheumatol. 2012, 6, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Soucie, J.M.; Wang, C.; Forsyth, A.; Funk, S.; Denny, M.; Roach, K.E.; Boone, D. Hemophilia Treatment Center Network. Range of motion measurements: Reference values and a database for comparison studies. Haemophilia 2011, 3, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Hayes, K.; Walton, J.R.; Szomor, Z.L.; Murrell, G.A.C. Reliability of five methods for assessing shoulder range of motion. Aust. J. Physiother. 2001, 47, 289–294. [Google Scholar] [CrossRef]
- Riddle, D.L.; Rothstein, J.M.; Lamb, R.L. Goniometric reliability in a clinical setting. Shoulder measurements. Phys. Ther. 1987, 67, 668–673. [Google Scholar] [CrossRef]
- Gajdosik, R.L.; Bohannon, R.W. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys. Ther. 1987, 67, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Laupattarakasem, W.; Sirichativapee, W.; Kowsuwon, W.; Sribunditkul, S.; Suibnugarn, C. Axial rotation gravity goniometer. A simple design of instrument and a controlled reliability study. Clin. Orthop. Relat. Res. 1990, 251, 271–274. [Google Scholar]
- Boone, D.C.; Azen, S.P.; Lin, C.M.; Spence, C.; Baron, C.; Lee, L. Reliability of goniometric measurements. Phys. Ther. 1987, 58, 1355–1360. [Google Scholar] [CrossRef]
- Pandya, S.; Florence, J.M.; King, W.M.; Robison, J.D.; Oxman, M.; Province, M.A. Reliability of goniometric measurements in patients with Duchenne muscular dystrophy. Phys. Ther. 1985, 65, 1339–1342. [Google Scholar] [CrossRef]
- McVeigh, K.H.; Murray, P.M.; Heckman, M.G.; Rawal, B.; Peterson, J.J. Accuracy and Validity of Goniometer and Visual Assessments of Angular Joint Positions of the Hand and Wrist. J. Hand Surg. Am. 2016, 41, e21–e35. [Google Scholar] [CrossRef] [PubMed]
- Bovens, A.M.; van Baak, M.A.; Vrencken, J.G.; Wijnen, J.A.; Verstappen, F.T. Variability and reliability of joint measurements. Am. J. Sports Med. 1990, 18, 58–63. [Google Scholar] [CrossRef]
- Walker, J.M.; Sue, D.; Miles-Elkousy, N.; Ford, G.; Trevelyan, H. Active mobility of the extremities in older subjects. Phys. Ther. 1984, 64, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, J.; Clark, C.; Deakes, J.; Burdon, D.; Lawrence, C. Clinical methods of goniometry: A comparative study. Disabil. Rehabil. 1992, 14, 10–15. [Google Scholar] [CrossRef]
- Lea, R.D.; Gerhardt, J.J. Range-of-motion measurements. J. Bone Jt. Surg. Am. 1995, 77, 784–798. [Google Scholar] [CrossRef] [PubMed]
- Vafadar, A.K.; Côté, J.N.; Archambault, P.S. Interrater and Intrarater Reliability and Validity of 3 Measurement Methods for Shoulder-Position Sense. J. Sport Rehabil. 2016, 25. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.W.L.; Espinosa, H.G.; Grigg, J. Evolution of smart devices and human movement apps: Recommendations for use in sports science education and practice. J. Fit. Res. 2016, 5, 14–15. [Google Scholar]
- Mosa, A.S.M.; Yoo, I.; Sheets, L. A Systematic Review of Healthcare Applications for Smartphones. BMC. Med. Inform. Decis. Mak. 2012, 12, 67. [Google Scholar] [CrossRef]
- Bruyneel, A.V. Smartphone Applications for Range of Motion Measurement in Clinical Practice: A Systematic Review. Stud. Health Technol. Inform. 2020, 270, 1389–1390. [Google Scholar] [CrossRef] [PubMed]
- Vercelli, S.; Sartorio, F.; Bravini, E.; Ferriero, G. DrGoniometer: A reliable smartphone app for joint angle measurement. Br. J. Sports Med. 2017, 51, 1703–1704. [Google Scholar] [CrossRef]
- Kolber, M.J.; Hanney, W.J. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: A technical report. Int. J. Sports Phys. Ther. 2012, 7, 306–313. [Google Scholar] [PubMed]
- Rodgers, M.M.; Alon, G.; Pai, V.M.; Conroy, R.S. Wearable technologies for active living and rehabilitation: Current research challenges and future opportunities. J. Rehabil. Assist. Technol. Eng. 2019, 6, 2055668319839607. [Google Scholar] [CrossRef]
- Mourcou, Q.; Fleury, A.; Diot, B.; Franco, C.; Vuillerme, N. Mobile Phone-Based Joint Angle Measurement for Functional Assessment and Rehabilitation of Proprioception. Biomed. Res. Int. 2015, 2015, 328142. [Google Scholar] [CrossRef]
- Faisal, A.I.; Majumder, S.; Mondal, T.; Cowan, D.; Naseh, S.; Deen, M.J. Monitoring Methods of Human Body Joints: State-of-the-Art and Research Challenges. Sensors 2019, 19, 2629. [Google Scholar] [CrossRef]
- TechTarget. Kinect. Available online: http://searchhealthit.techtarget.com/definition/Kinect (accessed on 14 October 2021).
- Anton, D.; Berges, I.; Bermúdez, J.; Goñi, A.; Illarramendi, A. A Telerehabilitation System for the Selection, Evaluation and Remote Management of Therapies. Sensors 2018, 18, 1459. [Google Scholar] [CrossRef]
- Antón, D.; Nelson, M.; Russell, T.; Goñi, A.; Illarramendi, A. Validation of a Kinect-based telerehabilitation system with total hip replacement patients. J. Telemed. Telecare 2016, 22, 192–197. [Google Scholar] [CrossRef]
- Kang, Y.S.; Chang, Y.J.; Howell, S.R. Using a kinect-based game to teach oral hygiene in four elementary students with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2021, 34, 606–614. [Google Scholar] [CrossRef]
- Boutsika, E. Kinect in Education: A Proposal for Children with Autism. Procedia Comput. Sci. 2014, 27, 123–129. [Google Scholar] [CrossRef]
- Pfister, A.; West, A.M.; Bronner, S.; Noah, J.A. Comparative abilities of Microsoft Kinect and Vicon 3D motion capture for gait analysis. J. Med. Eng. Technol. 2014, 38, 274–280. [Google Scholar] [CrossRef]
- Mangal, N.K.; Tiwari, A.K. Kinect v2 tracked Body Joint Smoothing for Kinematic Analysis in Musculoskeletal Disorders. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 5769–5772. [Google Scholar] [CrossRef]
- Bonnechère, B.; Sholukha, V.; Omelina, L.; Van Sint Jan, S.; Jansen, B. 3D Analysis of Upper Limbs Motion during Rehabilitation Exercises Using the Kinect Sensor: Development, Laboratory Validation and Clinical Application. Sensors 2018, 18, 2216. [Google Scholar] [CrossRef]
- Moon, S.; Park, Y.; Ko, D.W.; Suh, I.H. Multiple Kinect Sensor Fusion for Human Skeleton Tracking Using Kalman Filtering. Int. J. Adv. Robot. Syst. 2016, 13, 65. [Google Scholar] [CrossRef]
- Wiedemann, L.G.; Planinc, R.; Nemec, I.; Kampel, M. Performance evaluation of joint angles obtained by the Kinect V2. In Proceedings of the IET International Conference on Technologies for Active and Assisted Living (TechAAL), London, UK, 5 November 2015; pp. 1–6. [Google Scholar] [CrossRef]
- Zerpa, C.; Lees, C.; Patel, P.; Pryzsucha, E. The Use of Microsoft Kinect for Human Movement Analysis. Int. J. Sports Sci. 2015, 5, 120–127. [Google Scholar] [CrossRef]
- Zhang, Z.; Ji, L.; Huang, Z.; Wu, J. Adaptive Information Fusion for Human Upper Limb Movement Estimation. IEEE Trans. Syst. Man. Cybern. Part A Syst. Hum. 2012, 42, 1100–1108. [Google Scholar] [CrossRef]
- Saber-Sheikh, K.; Bryant, E.C.; Glazzard, C.; Hamel, A.; Lee, R.Y. Feasibility of using inertial sensors to assess human movement. Man. Ther. 2010, 15, 122–125. [Google Scholar] [CrossRef]
- Carnevale, A.; Longo, U.G.; Schena, E.; Massaroni, C.; Lo Presti, D.; Berton, A.; Candela, V.; Denaro, V. Wearable systems for shoulder kinematics assessment: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 546. [Google Scholar] [CrossRef] [PubMed]
- Robert-Lachaine, X.; Mecheri, H.; Muller, A.; Larue, C.; Plamondon, A. Validation of a low-cost inertial motion capture system for whole-body motion analysis. J. Biomech. 2020, 99, 109520. [Google Scholar] [CrossRef]
- Bewes, R.; Callaway, A.; Williams, J. Inertial sensor measurement of shoulder joint position sense: Reliability and consistency. Physiotherapy 2020, 107, e114. [Google Scholar] [CrossRef]
- Walmsley, C.P.; Williams, S.A.; Grisbrook, T.; Elliott, C.; Imms, C.; Campbell, A. Measurement of Upper Limb Range of Motion Using Wearable Sensors: A Systematic Review. Sports Med. Open 2018, 4, 53. [Google Scholar] [CrossRef] [PubMed]
- Garimella, R.; Peeters, T.; Beyers, K.; Truijen, S.; Huysmans, T.; Verwulgen, S. Capturing Joint Angles of the Off-site Human Body. In Proceedings of the IEEE Sensors, New Delhi, India, 28–31 October 2018; pp. 1–4. [Google Scholar]
- Kuhlmann, T.; Garaizar, P.; Reips, U.D. Smartphone sensor accuracy varies from device to device in mobile research: The case of spatial orientation. Behav. Res. 2021, 53, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.; Wang, J.; Lin, Y.; Chen, S.; Tsai, Y.; Chu, C.; Chang, C. A wearable inertial-sensing-based body sensor network for shoulder range of motion assessment. In Proceedings of the 2013 1st International Conference on Orange Technologies (ICOT), Tainan, Taiwan, 12–16 March 2013; pp. 328–331. [Google Scholar] [CrossRef]
- Streiner, D.; Norman, G. Health Measurement Scales: A Practical Guide to Their Development and Use, 3rd ed.; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Scano, A.; Mira, R.M.; Cerveri, P.; Molinari Tosatti, L.; Sacco, M. Analysis of Upper-Limb and Trunk Kinematic Variability: Accuracy and Reliability of an RGB-D Sensor. Multimodal Technol. Interact. 2020, 4, 14. [Google Scholar] [CrossRef]
- López, N.; Perez, E.; Tello, E.; Rodrigo, A.; Valentinuzzi, M.E. Statistical Validation for Clinical Measures: Repeatability and Agreement of Kinect-Based Software. BioMed Res. Int. 2018, 2018, 6710595. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.D.; Khan-Perez, J.; Marley, D.; Buttress, S.; Walton, M.; Li, B.; Roy, B. Can shoulder range of movement be measured accurately using the Microsoft Kinect sensor plus Medical Interactive Recovery Assistant (MIRA) software? J. Shouder Elb. Surg. 2017, 26, e382–e389. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Yoon, C.; Chung, S.G.; Kim, H.C.; Kwak, Y.; Park, H.; Kim, K. Measurement of shoulder range of motion in patients with adhesive capsulitis using a kinect. PLoS ONE 2015, 10, e0129398. [Google Scholar] [CrossRef] [PubMed]
- Poitras, I.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.S. Validity of Wearable Sensors at the Shoulder Joint: Combining Wireless Electromyography Sensors and Inertial Measurement Units to Perform Physical Workplace Assessments. Sensors 2019, 19, 1885. [Google Scholar] [CrossRef] [PubMed]
- Morrow, M.M.B.; Lowndes, B.; Fortune, E.; Kaufman, K.R.; Hallbeck, M.S. Validation of Inertial Measurement Units for Upper Body Kinematics. J. Appl. Biomech. 2017, 33, 227–232. [Google Scholar] [CrossRef]
- Lin, Y.C.; Tsai, Y.J.; Hsu, Y.L.; Yen, M.H.; Wang, J.S. Assessment of Shoulder Range of Motion Using a Wearable Inertial Sensor Network. IEEE Sens. J. 2021, 21, 15330–15341. [Google Scholar] [CrossRef]
- Carey, M.A.; Laird, D.E.; Murray, K.A.; Stevenson, J.R. Reliability, validity, and clinical usability of a digital goniometer. Work 2010, 36, 55–66. [Google Scholar] [CrossRef]
- Hannah, D.C.; Scibek, J.S. Collecting shoulder kinematics with electromagnetic tracking systems and digital inclinometers: A review. World J. Orthop. 2015, 6, 783–794. [Google Scholar] [CrossRef] [PubMed]
- Scibek, J.S.; Carcia, C.R. Assessment of scapulohumeral rhythm for scapular plane shoulder elevation using a modified digital inclinometer. World J. Orthop. 2012, 3, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.P.; McClure, P.W.; Karduna, A.R. New method to assess scapular upward rotation in subjects with shoulder pathology. J. Orthop. Sports Phys. Ther. 2001, 31, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Pichonnaz, C.; Aminian, K.; Ancey, C.; Jaccard, H.; Lécureux, E.; Duc, C.; Farron, A.; Jolles, B.M.; Gleeson, N. Heightened clinical utility of smartphone versus body-worn inertial system for shoulder function B-B score. PLoS ONE 2017, 12, e0174365. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.B.; Sumner, S.; Duong, T.; Yan, P.; Bajcsy, R.; Abresch, R.T.; de Bie, E.; Han, J.J. Validity and reliability of smartphone magnetometer-based goniometer evaluation of shoulder abduction—A pilot study. Man. Ther. 2015, 20, 777–782. [Google Scholar] [CrossRef]
- Keogh, J.W.L.; Cox, A.; Anderson, S.; Liew, B.; Olsen, A.; Schram, B.; Furness, J. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PLoS ONE 2019, 14, e0215806. [Google Scholar] [CrossRef]
- McDowell, I. Measuring Health: A Guide to Rating Scales and Questionnaires, 3rd ed.; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
- Norkin, C.C.; White, D.J.; Torres, J.; Greene, M.J.; Grochowska, L.L.; Malone, T.W. Measurement of Joint Motion: A Guide to Goniometry; F.A. Davis: Philadelphia, PA, USA, 1995. [Google Scholar]
- Altman, D.G.; Bland, J.M. Measurement in medicine: The analysis of method comparison studies. Statistician 1983, 32, 307–317. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- de Vet, H.C.; Terwee, C.B.; Knol, D.L.; Bouter, L.M. When to use agreement versus reliability measures. J. Clin. Epidemiol. 2006, 10, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.W. Getting more from the literature: Estimating the standard error of measurement from reliability studies. Physiother. Can. 2004, 56, 27–30. [Google Scholar] [CrossRef]
- Webster, D.; Celik, O. Systematic review of Kinect applications in elderly care and stroke rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 108. [Google Scholar] [CrossRef]
- Xavier-Rocha, T.B.; Carneiro, L.; Martins, G.C.; Vilela-JÚnior, G.B.; Passos, R.P.; Pupe, C.C.B.; Nascimento, O.J.M.D.; Haikal, D.S.; Monteiro-Junior, R.S. The Xbox/Kinect use in poststroke rehabilitation settings: A systematic review. Arq. Neuropsiquiatr. 2020, 78, 361–369. [Google Scholar] [CrossRef]
- Knippenberg, E.; Verbrugghe, J.; Lamers, I.; Palmaers, S.; Timmermans, A.; Spooren, A. Markerless motion capture systems as training device in neurological rehabilitation: A systematic review of their use, application, target population and efficacy. J. Neuroeng. Rehabil. 2017, 14, 61. [Google Scholar] [CrossRef]
- Garcia-Agundez, A.; Folkerts, A.K.; Konrad, R.; Caserman, P.; Tregel, T.; Goosses, M.; Göbel, S.; Kalbe, E. Recent advances in rehabilitation for Parkinson’s Disease with Exergames: A Systematic Review. J. Neuroeng. Rehabil. 2019, 16, 17. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Indino, A.; de Scorpio, G.; Moggio, L.; Ammendolia, A. Nintendo Wii versus Xbox Kinect for functional locomotion in people with Parkinson’s disease: A systematic review and network meta-analysis. Disabil. Rehabil. 2020, 1–6. [Google Scholar] [CrossRef]
- Barry, G.; Galna, B.; Rochester, L. The role of exergaming in Parkinson’s disease rehabilitation: A systematic review of the evidence. J. NeuroEng. Rehabil. 2014, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Puh, U.; Hoehlein, B.; Deutsch, J.E. Validity and Reliability of the Kinect for Assessment of Standardized Transitional Movements and Balance: Systematic Review and Translation into Practice. Phys. Med. Rehabil. Clin. N. Am. 2019, 30, 399–422. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- van de Pol, R.J.; van Trijffel, E.; Lucas, C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: A systematic review. J. Physiother. 2010, 56, 7–17. [Google Scholar] [CrossRef]
- Denteneer, L.; Stassijns, G.; De Hertogh, W.; Truijen, S.; Van Daele, U. Inter- and Intrarater Reliability of Clinical Tests Associated with Functional Lumbar Segmental Instability and Motor Control Impairment in Patients with Low Back Pain: A Systematic Review. Arch. Phys. Med. Rehabil. 2017, 98, 151–164.e6. [Google Scholar] [CrossRef] [PubMed]
- Swinkels, R.; Bouter, L.; Oostendorp, R.; van den Ende, C. Impairment measures in rheumatic disorders for rehabilitation medicine and allied health care: A systematic review. Rheumatol. Int. 2005, 25, 501–512. [Google Scholar] [CrossRef][Green Version]
- Mokkink, L.B.; Boers, M.; van der Vleuten, C.P.M.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; de Vet, H.C.W.; Terwee, C.B. COSMIN Risk of Bias tool to assess the quality of studies on reliability or measurement error of outcome measurement instruments: A Delphi study. BMC Med. Res. Methodol. 2020, 20, 293. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.B.; Mathieson, S.; Eyles, J.; Maher, C.G.; Van Gelder, J.M.; Tomkins-Lane, C.C.; Ammendolia, C.; Bella, V.; Ferreira, M.L. Measurement properties of walking outcome measures for neurogenic claudication: A systematic review and meta-analysis. Spine J. 2019, 19, 1378–1396. [Google Scholar] [CrossRef]
- Dobson, F.; Hinman, R.S.; Hall, M.; Terwee, C.B.; Roos, E.M.; Bennell, K.L. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: A systematic review. Osteoarthr. Cartil. 2012, 12, 1548–1562. [Google Scholar] [CrossRef] [PubMed]
- Awan, R.; Smith, J.; Boon, A.J. Measuring shoulder internal rotation range of motion: A comparison of 3 techniques. Arch. Phys. Med. Rehabil. 2002, 83, 1229–1234. [Google Scholar] [CrossRef] [PubMed]
- Beshara, P.; Chen, J.; Lagadec, P.; Walsh, W.R. Test-Retest and Intra-rater Reliability of Using Inertial Sensors and Its Integration with Microsoft Kinect™ to Measure Shoulder Range-of-Motion. In Internet of Things Technologies for HealthCare; Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering Series; Springer International Publishing: Cham, Switzerland, 2016; Volume 187. [Google Scholar]
- Bonnechère, B.; Jansen, B.; Salvia, P.; Bouzahouene, H.; Omelina, L.; Moiseev, F.; Sholukha, V.; Cornelis, J.; Rooze, M.; Van Sint Jan, S. Validity and reliability of the Kinect within functional assessment activities: Comparison with standard stereophotogrammetry. Gait Posture 2014, 39, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Cai, L.; Ma, Y.; Xiong, S.; Zhang, Y. Validity and Reliability of Upper Limb Functional Assessment Using the Microsoft Kinect V2 Sensor. Appl. Bionics Biomech. 2019, 2019, 175240. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.; Sihler, E.; Kijek, T.; Miller, B.S.; Hughes, R.E. A mobile computing tool for collecting clinical outcomes data from shoulder patients. J. Musculoskelet. Res. 2010, 13, 127–136. [Google Scholar] [CrossRef]
- Chen, Y.P.; Lin, C.Y.; Tsai, M.J.; Chuang, T.Y.; Lee, O.K. Wearable Motion Sensor Device to Facilitate Rehabilitation in Patients with Shoulder Adhesive Capsulitis: Pilot Study to Assess Feasibility. J. Med. Internet Res. 2020, 22, e17032. [Google Scholar] [CrossRef] [PubMed]
- Cools, A.M.; De Wilde, L.; Van Tongel, A.; Ceyssens, C.; Ryckewaert, R.; Cambier, D.C. Measuring shoulder external and internal rotation strength and range of motion: Comprehensive intra-rater and inter-rater reliability study of several testing protocols. J. Shoulder Elb. Surg. 2014, 23, 1454–1461. [Google Scholar] [CrossRef] [PubMed]
- Correll, S.; Field, J.; Hutchinson, H.; Mickevicius, G.; Fitzsimmons, A.; Smoot, B. Reliability and Validity of the Halo Digital goniometer for shoulder range of motion in healthy subjects. Int. J. Sports Phys. Ther. 2018, 13, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Çubukçu, B.; Yüzgeç, U.; Zileli, R.; Zileli, A. Reliability and validity analyzes of Kinect V2 based measurement system for shoulder motions. Med. Eng. Phys. 2020, 76, 20–31. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; Roldán-Jiménez, C. Validity and reliability of arm abduction angle measured on smartphone: A cross-sectional study. BMC Musculoskelet. Disord. 2016, 17, 93. [Google Scholar] [CrossRef] [PubMed]
- Da Cunha Neto, J.S.; Rebouças Filho, P.P.; Da Silva, G.P.F.; Da Cunha Olegario, N.B.; Duarte, J.B.F.; De Albuquerque, V.H.C. Dynamic Evaluation and Treatment of the Movement Amplitude Using Kinect Sensor. IEEE Access 2018, 6, 17292–17305. [Google Scholar] [CrossRef]
- De Baets, L.; Vanbrabant, S.; Dierickx, C.; van der Straaten, R.; Timmermans, A. Assessment of Scapulothoracic, Glenohumeral, and Elbow Motion in Adhesive Capsulitis by Means of Inertial Sensor Technology: A Within-Session, Intra-Operator and Inter-Operator Reliability and Agreement Study. Sensors 2020, 20, 876. [Google Scholar] [CrossRef]
- de Winter, A.F.; Heemskerk, M.A.; Terwee, C.B.; Jans, M.P.; Devillé, W.; van Schaardenburg, D.J.; Scholten, R.J.; Bouter, L.M. Inter-observer reproducibility of measurements of range of motion in patients with shoulder pain using a digital inclinometer. BMC Musculoskelet. Disord. 2004, 5, 18. [Google Scholar] [CrossRef]
- Dougherty, J.; Walmsley, S.; Osmotherly, P.G. Passive range of movement of the shoulder: A standardized method for measurement and assessment of intrarater reliability. J. Manip. Physiol. Ther. 2015, 38, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Hawi, N.; Liodakis, E.; Musolli, D.; Suero, E.M.; Stuebig, T.; Claassen, L.; Kleiner, C.; Krettek, C.; Ahlers, V.; Citak, M. Range of motion assessment of the shoulder and elbow joints using a motion sensing input device: A pilot study. Technol. Health Care 2014, 22, 289–295. [Google Scholar] [CrossRef]
- Huber, M.E.; Seitz, A.L.; Leeser, M.; Sternad, D. Validity and reliability of Kinect skeleton for measuring shoulder joint angles: A feasibility study. Physiotherapy 2015, 101, 389–393. [Google Scholar] [CrossRef]
- Hwang, S.; Tsai, C.Y.; Koontz, A.M. Feasibility study of using a Microsoft Kinect for virtual coaching of wheelchair transfer techniques. Biomed. Tech. 2017, 62, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Kolber, M.J.; Vega, F.; Widmayer, K.; Cheng, M.S. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother. Theory Pract. 2011, 27, 176–184. [Google Scholar] [CrossRef]
- Kolber, M.J.; Fuller, C.; Marshall, J.; Wright, A.; Hanney, W.J. The reliability and concurrent validity of scapular plane shoulder elevation measurements using a digital inclinometer and goniometer. Physiother. Theory Pract. 2012, 28, 161–168. [Google Scholar] [CrossRef]
- Lim, J.Y.; Kim, T.H.; Lee, J.S. Reliability of measuring the passive range of shoulder horizontal adduction using a smartphone in the supine versus the side-lying position. J. Phys. Ther. Sci. 2015, 10, 3119–3122. [Google Scholar] [CrossRef] [PubMed]
- Mejia-Hernandez, K.; Chang, A.; Eardley-Harris, N.; Jaarsma, R.; Gill, T.K.; McLean, J.M. Smartphone applications for the evaluation of pathologic shoulder range of motion and shoulder scores-a comparative study. JSES Open Access 2018, 2, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, R.; Foreman, M.; Standeven, J.; Engsberg, J.R.; Morgan, K.A. Reliability and validity of the Microsoft Kinect for assessment of manual wheelchair propulsion. J. Rehabil. Res. Dev. 2016, 53, 901–918. [Google Scholar] [CrossRef]
- Mitchell, K.; Gutierrez, S.B.; Sutton, S.; Morton, S.; Morgenthaler, A. Reliability and validity of goniometric iPhone applications for the assessment of active shoulder external rotation. Physiother. Theory Pract. 2014, 30, 521–525. [Google Scholar] [CrossRef]
- Picerno, P.; Viero, V.; Donati, M.; Triossi, T.; Tancredi, V.; Melchiorri, G. Ambulatory assessment of shoulder abduction strength curve using a single wearable inertial sensor. J. Rehabil. Res. Dev. 2015, 52, 171–180. [Google Scholar] [CrossRef]
- Poser, A.; Ballarin, R.; Piu, P.; Venturin, D.; Plebani, G.; Rossi, A. Intra and inter examiner reliability of the range of motion of the shoulder in asymptomatic subjects, by means of digital inclinometers. Sci. Riabil. 2015, 17, 17–25. [Google Scholar]
- Ramos, M.M.; Carnaz, L.; Mattiello, S.M.; Karduna, A.R.; Zanca, G.G. Shoulder and elbow joint position sense assessment using a mobile app in subjects with and without shoulder pain-between-days reliability. Phys. Ther. Sport 2019, 37, 157–163. [Google Scholar] [CrossRef]
- Rigoni, M.; Gill, S.; Babazadeh, S.; Elsewaisy, O.; Gillies, H.; Nguyen, N.; Pathirana, P.N.; Page, R. Assessment of Shoulder Range of Motion Using a Wireless Inertial Motion Capture Device—A Validation Study. Sensors 2019, 19, 1781. [Google Scholar] [CrossRef]
- Schiefer, C.; Kraus, T.; Ellegast, R.P.; Ochsmann, E. A technical support tool for joint range of motion determination in functional diagnostics—An inter-rater study. J. Occup. Med. Toxicol. 2015, 10, 16. [Google Scholar] [CrossRef]
- Scibek, J.S.; Carcia, C.R. Validation and repeatability of a shoulder biomechanics data collection methodology and instrumentation. J. Appl. Biomech. 2013, 29, 609–615. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shin, S.H.; Lee, O.S.; Oh, J.H.; Kim, S.H. Within-day reliability of shoulder range of motion measurement with a smartphone. Man. Ther. 2012, 17, 298–304. [Google Scholar] [CrossRef]
- Walker, H.; Pizzari, T.; Wajswelner, H.; Blanch, P.; Schwab, L.; Bennell, K.; Gabbe, B. The reliability of shoulder range of motion measures in competitive swimmers. Phys. Ther. Sport 2016, 21, 26–30. [Google Scholar] [CrossRef]
- Werner, B.C.; Holzgrefe, R.E.; Griffin, J.W.; Lyons, M.L.; Cosgrove, C.T.; Hart, J.M.; Brockmeier, S.F. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J. Shoulder Elb. Surg. 2014, 23, e275–e282. [Google Scholar] [CrossRef] [PubMed]
- Frost, M.H.; Reeve, B.B.; Liepa, A.M.; Stauffer, J.W.; Hays, R.D. Mayo/FDA Patient-Reported Outcomes Consensus Meeting Group. What is sufficient evidence for the reliability and validity of patient-reported outcome measures? Value Health 2007, S94–S105. [Google Scholar] [CrossRef] [PubMed]
- Fayers, P.; Machin, D. Quality of Life. Assessment, Analysis and Interpretation, 2nd ed.; John Wiley & Sons: Chichester, UK, 2007. [Google Scholar]
- Sim, J.; Wright, C.C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Monnier, A.; Heuer, J.; Norman, K.; Ang, B.O. Inter- and intra-observer reliability of clinical movement-control tests for marines. BMC Musculoskelet. Disord. 2012, 13, 263. [Google Scholar] [CrossRef] [PubMed]
- Tegern, M.; Aasa, U.; Äng, B.O.; Harms-Ringdahl, K.; Larsson, H. Inter-rater and test-retest reliability of movement control tests for the neck, shoulder, thoracic, lumbar, and hip regions in military personnel. PLoS ONE 2018, 13, e0204552. [Google Scholar] [CrossRef]
- Nayak, B.K. Understanding the relevance of sample size calculation. Indian J. Ophthalmol. 2010, 58, 469–470. [Google Scholar] [CrossRef]
- Mokkink, L.B.; de Vet, H.C.W.; Prinsen, C.A.C.; Patrick, D.L.; Alsonso, J.; Bouter, L.M.; Terwee, C.B. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual. Life Res. 2018, 27, 1171–1179. [Google Scholar] [CrossRef]
- Carter, R.E.; Lubinsky, J.; Domholdt, E. Rehabilitation Research: Principles and Applications, 4th ed.; Elsevier Inc.: St. Louis, MO, USA, 2011. [Google Scholar]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Hobart, J.C.; Cano, S.J.; Warner, T.T.; Thompson, A.J. What sample sizes for reliability and validity studies in neurology? J. Neurol. 2012, 259, 2681–2694. [Google Scholar] [CrossRef]
- Wright, J.G.; Feinstein, A.R. Improving the reliability of orthopaedic measurements. J. Bone Jt. Surg. Br. 1992, 74, 287–291. [Google Scholar] [CrossRef][Green Version]
- Sabari, J.S.; Maltzev, I.; Lubarsky, D.; Liszkay, E.; Homel, P. Goniometric assessment of shoulder range of motion: Comparison of testing in supine and sitting positions. Arch. Phys. Med. Rehabil. 1998, 6, 64751. [Google Scholar] [CrossRef]
- Kim, B.R.; Yi, D.; Yim, J. Effect of postural change on shoulder joint internal and external rotation range of motion in healthy adults in their 20s. Phys. Ther. Rehabil. Sci. 2019, 8, 152–157. [Google Scholar] [CrossRef]
- Xu, X.; McGorry, R.W. The validity of the first and second generation Microsoft Kinect for identifying joint center locations during static postures. Appl. Ergon. 2015, 49, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, C.A.C.; Mokkink, L.B.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; de Vet, H.C.W.; Terwee, C.B. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef] [PubMed]
- Bujang, M.A.; Baharum, N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: A review. Arch. Orofac. Sci. 2017, 12, 1–11. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).