2.1. The Clinical Needs for an Anesthesia Airway Management Robot
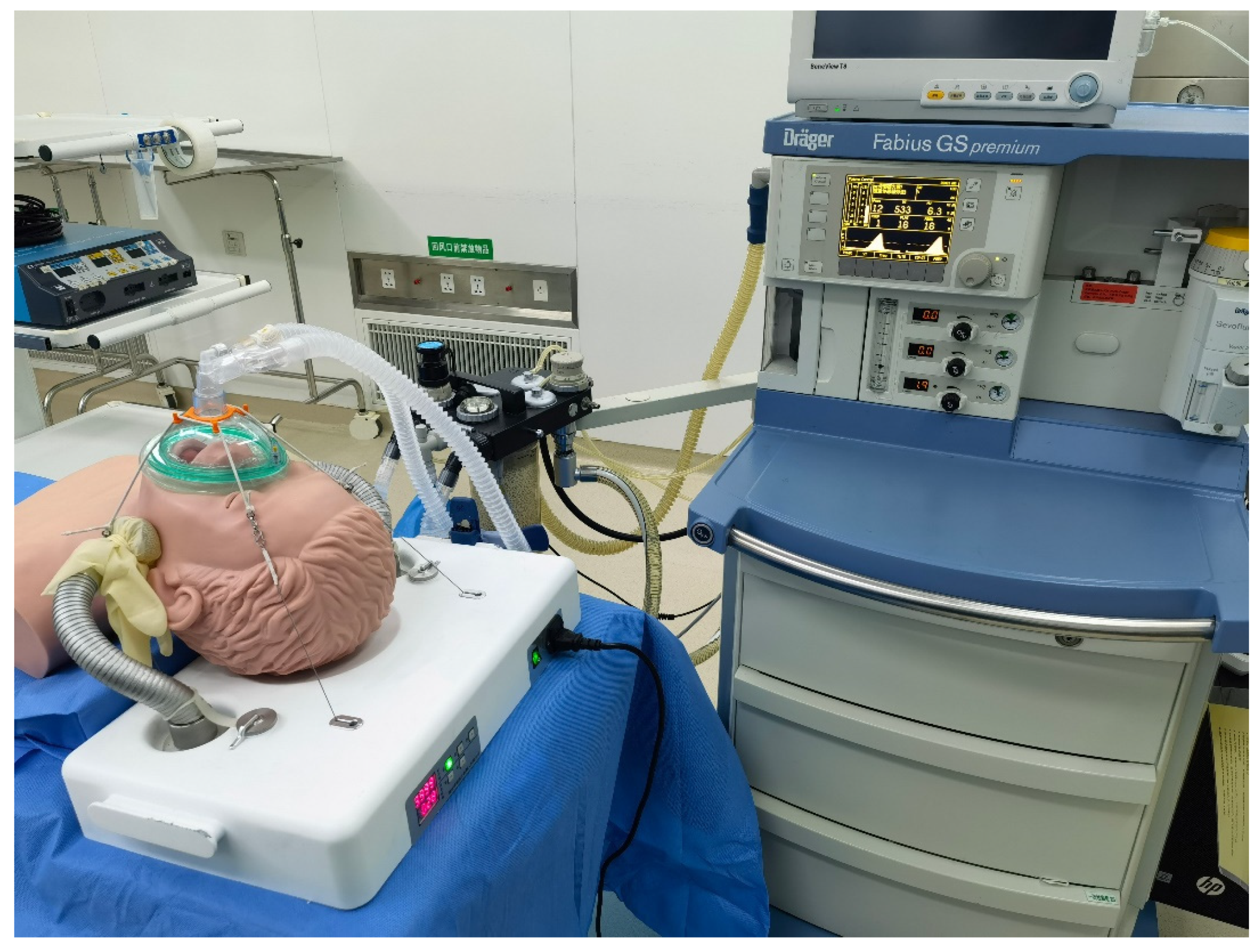
The robot should have functions equivalent to manual NPPV airway management. Additionally, it should be suitable for patients who have no risk of vomiting and aspiration in short general anesthesia operations. During the procedure, the mandible should be lifted to present the anatomical position of the mandibular reverse occlusion, so as to relieve the patient’s glossocoma after general anesthesia and ensure the airway is unobstructed. Meanwhile, the mask should be fastened tightly to the patient’s face to transmit air smoothly. If any risks occur during an operation, traditional IPPV methods can be used immediately as a remedy.
According to the above-presented clinical scenarios, the design of an anesthetic airway management robot should meet the following four requirements to achieve the auxiliary NPPV procedure:
Requirements for support strength. The designed manipulator should possess a convenient and robust locking function and provide sufficient support to ensure airway management motions. The joint locking strength of the manipulator should be able to resist the pressure of at least 30 N.
Degree of manipulator freedom requirement. The design of the manipulator should provide a universal support function with sufficient flexibility.
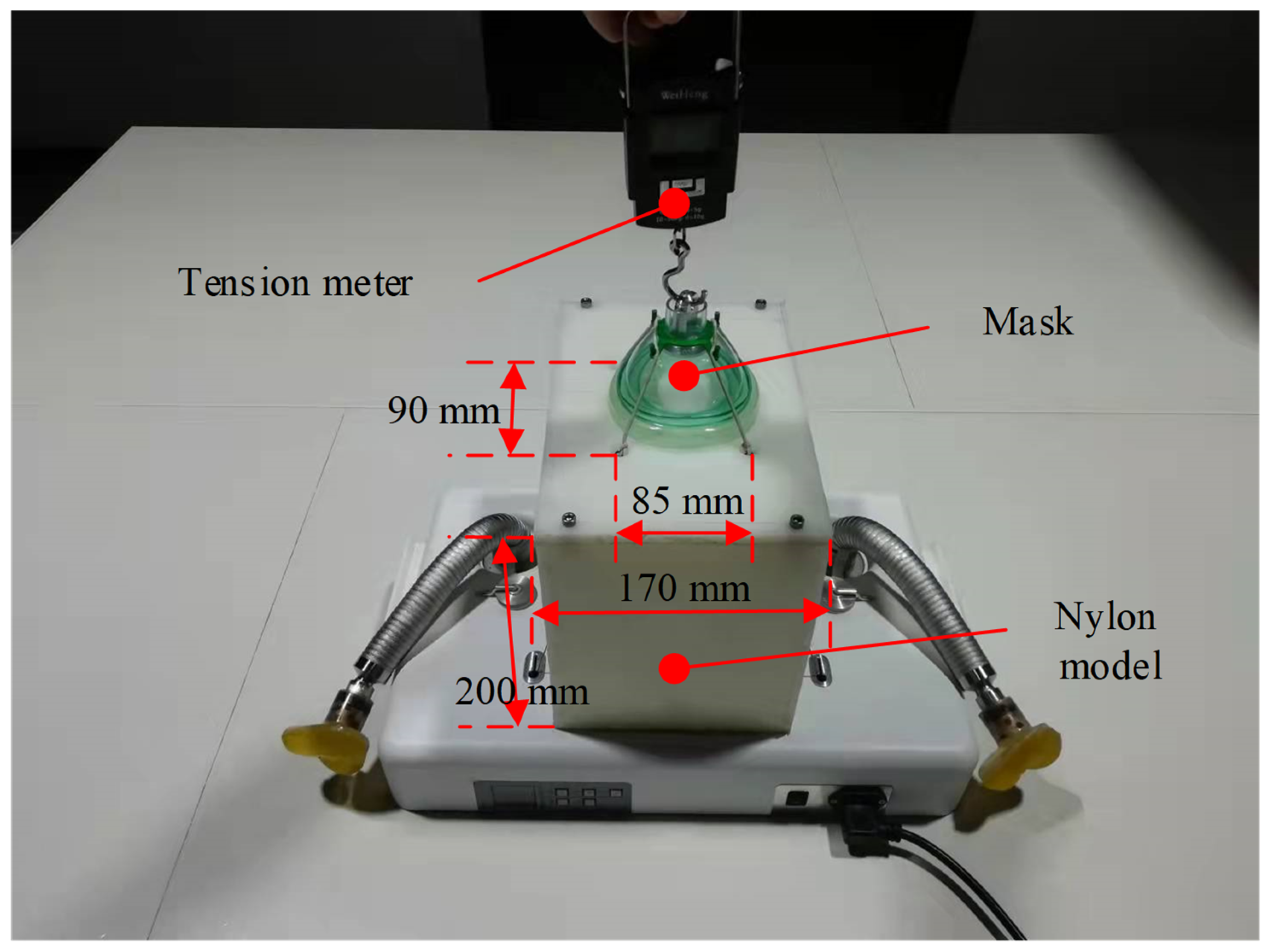
Requirement for mask fastening. The pressure provided by the mechanical structure to fasten the mask could be larger than 15 N.
Safety requirements. The manipulator should also provide a convenient and reliable manual unlocking function to prevent unexpected mechanical failures.
2.2. Structure Design of Anesthesia Airway Management Robot
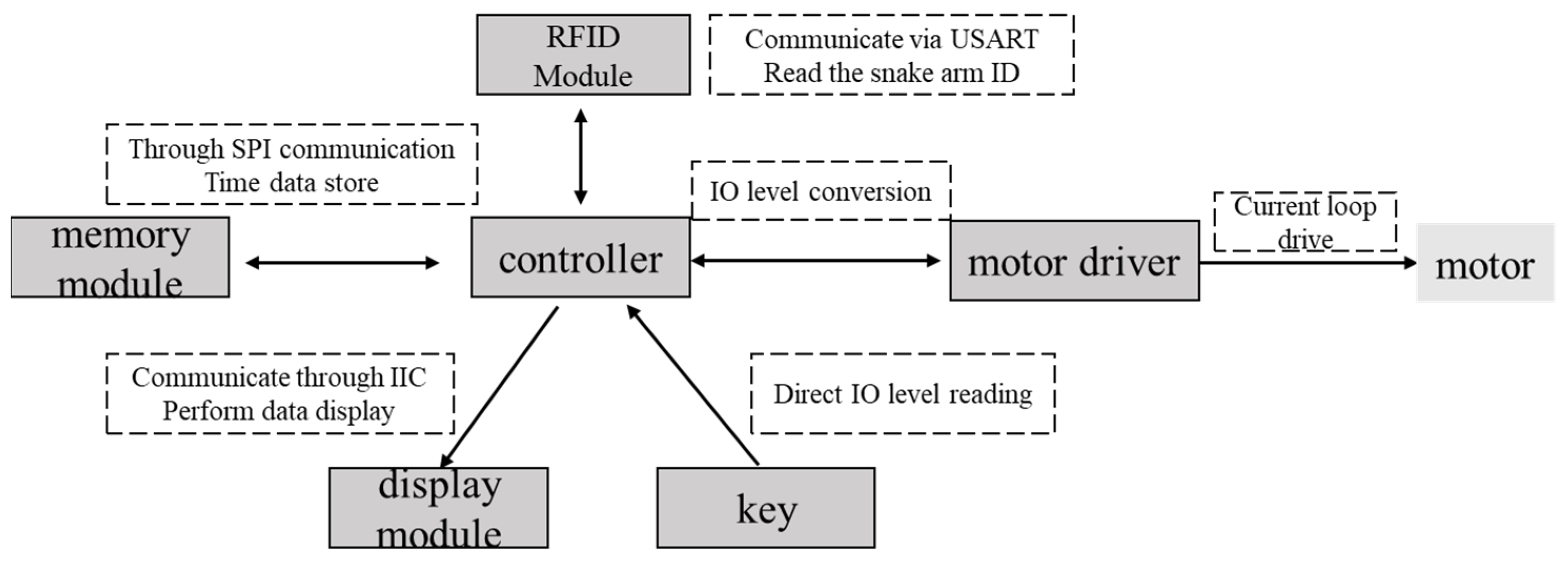
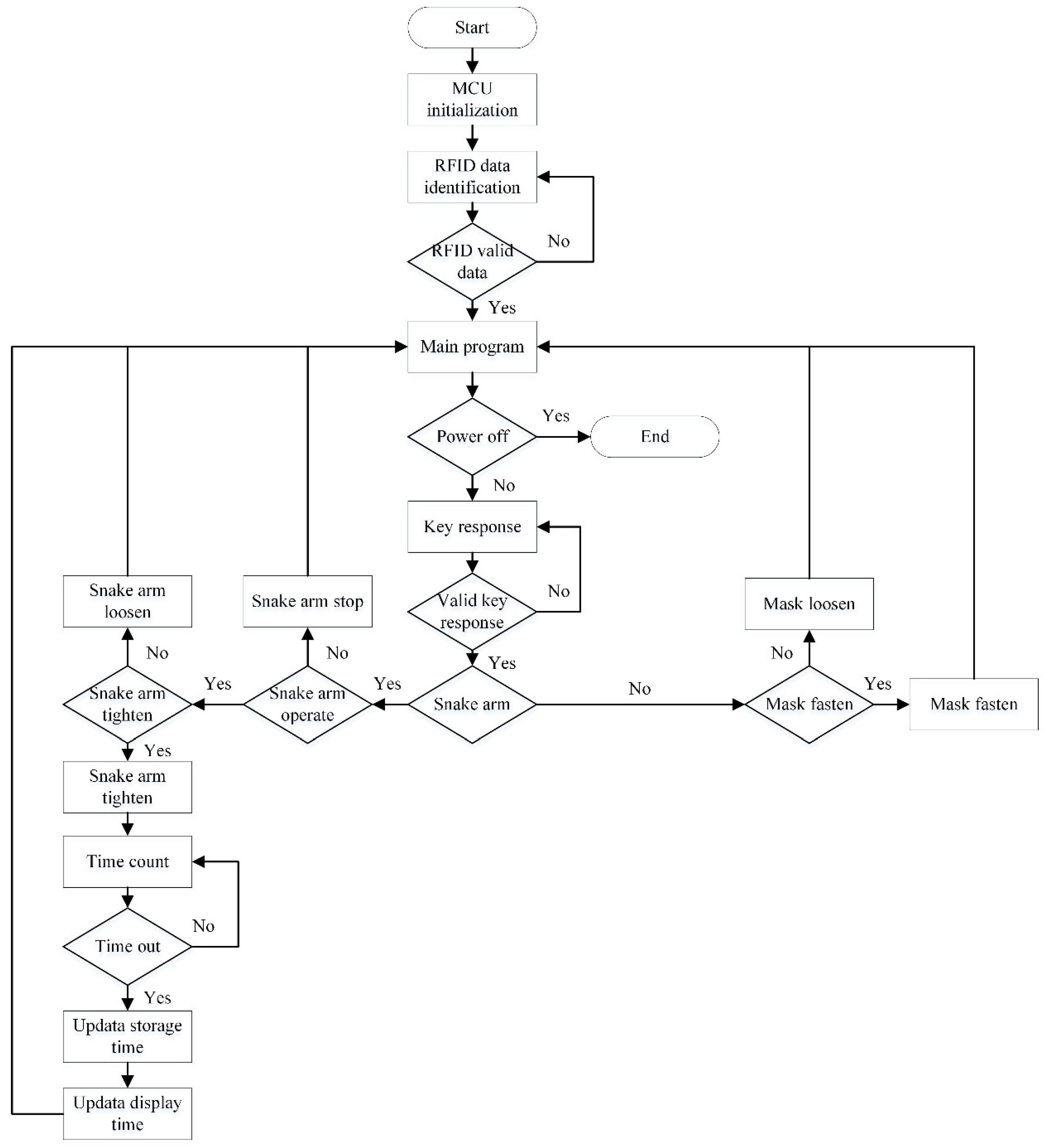
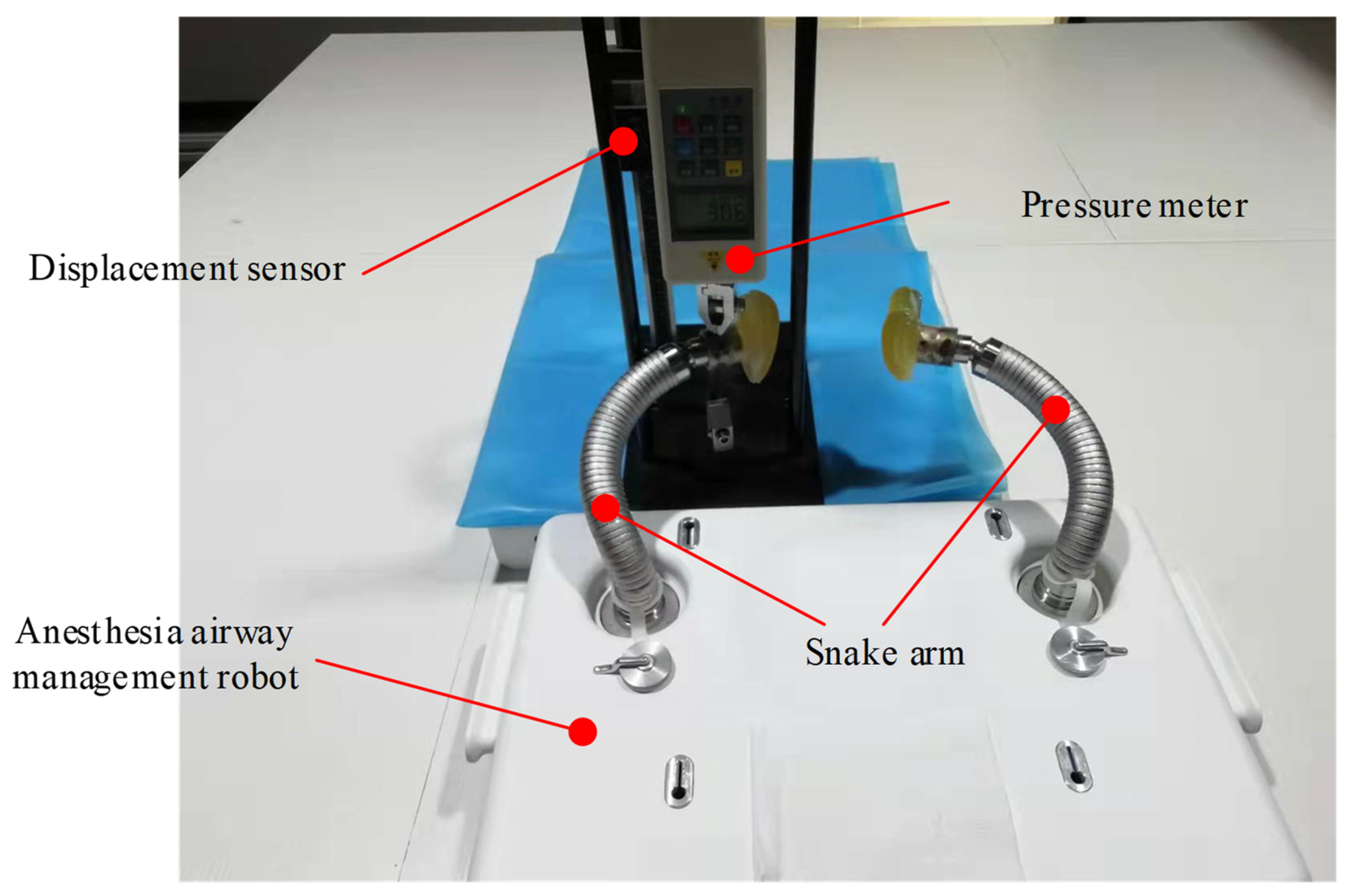
The anesthesia airway management robot has been designed to meet the design requirements mentioned above, as illustrated in
Figure 1. The designed robot mainly comprises a pair of snake arms with a universal support function, a mask-fastening module, and a headrest. Two snake arms are vertically installed on the baseplate of the headrest. A tentacle that lifts the jaw is set at the arm end to simulate the hand motions used to maintain airway management. Thus, the patient’s mandible can be supported, and the patient’s airway can maintain an opening state during the operation. The mask-fastening module is composed of a wire rope drive system and a mask. The motor inside the headrest controls the tightness of the wire rope, and thus the pressure applied to the patient’s face can be adjusted. The headrest supports the patient’s neck and head and helps patients in a supine position from a head back elevation posture. This headrest is equipped with both electric and manual unlocking functions of the snake arms to ensure the safety and reliability of the proposed system.
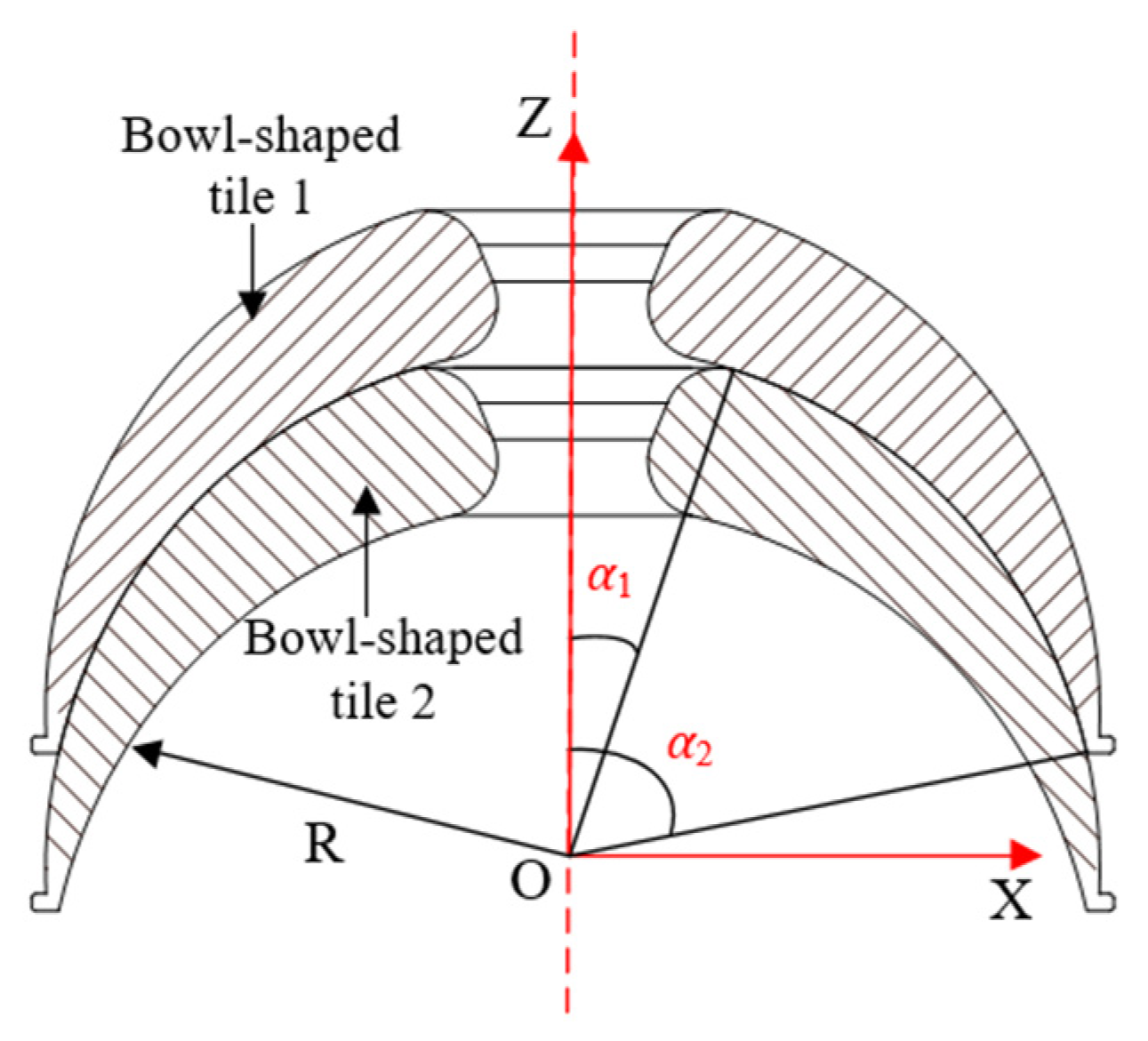
The continuum snake arm consists of a tentacle, a spring seat, bowl-shaped tiles, a wire rope, and a guide bolt, as illustrated in
Figure 2. The universal support structure of the snake arm is the core part of the robotic system. It is designed with multiple joints to form the continuum configuration and is composed of several bowl-shaped tiles in a serial connection. A through hole has been made in the middle part of each bowl-shaped tile, enabling the driving wire rope to carry. The wire rope runs through each joint of the whole arm, and its tail has been fixed at the worm wheel stretching mechanism designed at the system base. When the worm gear is operated, the wire rope can be tightened, and the whole joint of the manipulator can be tightened and locked. On the contrary, when the wire rope is relaxed, the locking state of each joint of the snake arm will be released. The tentacle at the distal end of the snake arm is provided with a specific surface structure corresponding to the mandible contact part to ensure uniform pressure and protect the patient’s mandible. The spring seat that connects with the tentacle provides the elastic pressure and realizes elastic force application within a specific range.
The mask-fastening module comprises a motor, a mask, 6 wire wheels, and several steel wire ropes, as illustrated in
Figure 3. Two wires run through wheels to press the mask, and their tails have been fixed to the motor. Wires are tightened when the motor rotates; thus, pressure on the mask can be increased. If wires are released, the motor will power off.
With the designed system, the operating surgeon can manually adjust the snake arms and apply forces symmetrically to the bilateral mandibular of the patient through the distal tentacles. Subsequently, the driving motor can tighten the wire rope and fasten the snake arms to meet the airway management requirements. The mask will be pressed to fit the patient’s face, and the motor will rotate to tighten the wires to form suitable tension. The proposed robotic system can replace the manual action of airway management through the above modules.
2.3. Design Optimization of the Bowl-Shaped Tiles
The locking function of the snake arm is realized by controlling the motor to drive the worm part to tighten the wire rope. According to the operational characteristics of the snake arm, the tension required by the wire rope is closely related to the friction between the bowl-shaped tiles. Therefore, optimization of the bowl-shaped tiles can play an essential role in structure design. The frictional contact between two bowl-shaped tiles has been illustrated in
Figure 4.
Referring to the calculation method of spherical friction torque [
19], the friction torque of a bowl-shaped tile rotating around the
z-axis is:
where
R denotes the radius of the friction sphere,
μ denotes the friction coefficient between bowl-shaped tiles, and
F expresses the axial load.
α1 represents the angle between the connection line from the center of the ball to the upper edge of bowl-shaped tile 1 and the
z-axis, and
α2 is the angle between the connection line from the center of the ball to the lower edge of bowl-shaped tile 1 and the
z-axis.
Since
x and
y are interchangeable, the rotation torques of the tiles around the
x-axis and
y-axis are equal, that is,
Mx =
My. The friction torque of the bowl-shaped tile around the
x-axis is:
According to the design requirements, 15° < α1 < 40°, 60° < α2 < 80°, it is obtained that Mz is smaller than Mx after theoretical analysis. Besides, it can be found that the forms of the equations of Mz and Mx are very similar, which means that they also share a similar change tendency. Thus, considering the convenience of simulation analysis, it is better to choose the smaller one (Mz) as the working condition of simulation.
As shown in Equations (1) and (2), the friction torque of bowl-shaped tiles is related to
R,
μ,
α1, and
α2. Because
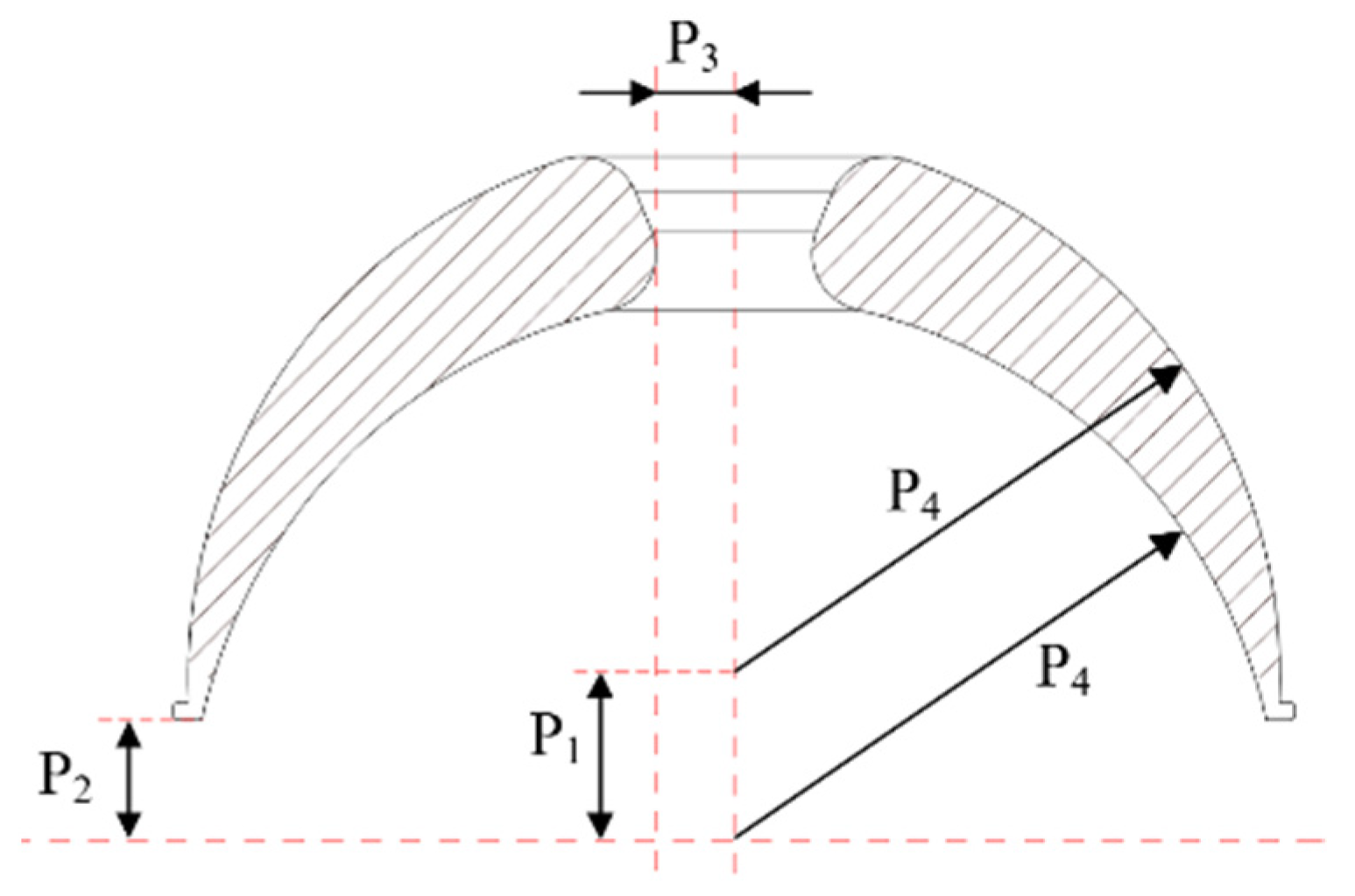
R is related to
α1 and
α2, it is hard to optimize with these parameters. Therefore, the inner and outer circle center distance, P
1,
z tangential distance, P
2, center hole radius, P
3, and inner and outer circle radii, P
4, are selected as the structural parameters to be optimized, as illustrated in
Figure 5.
The variation range of structural parameters is shown in
Table 1.
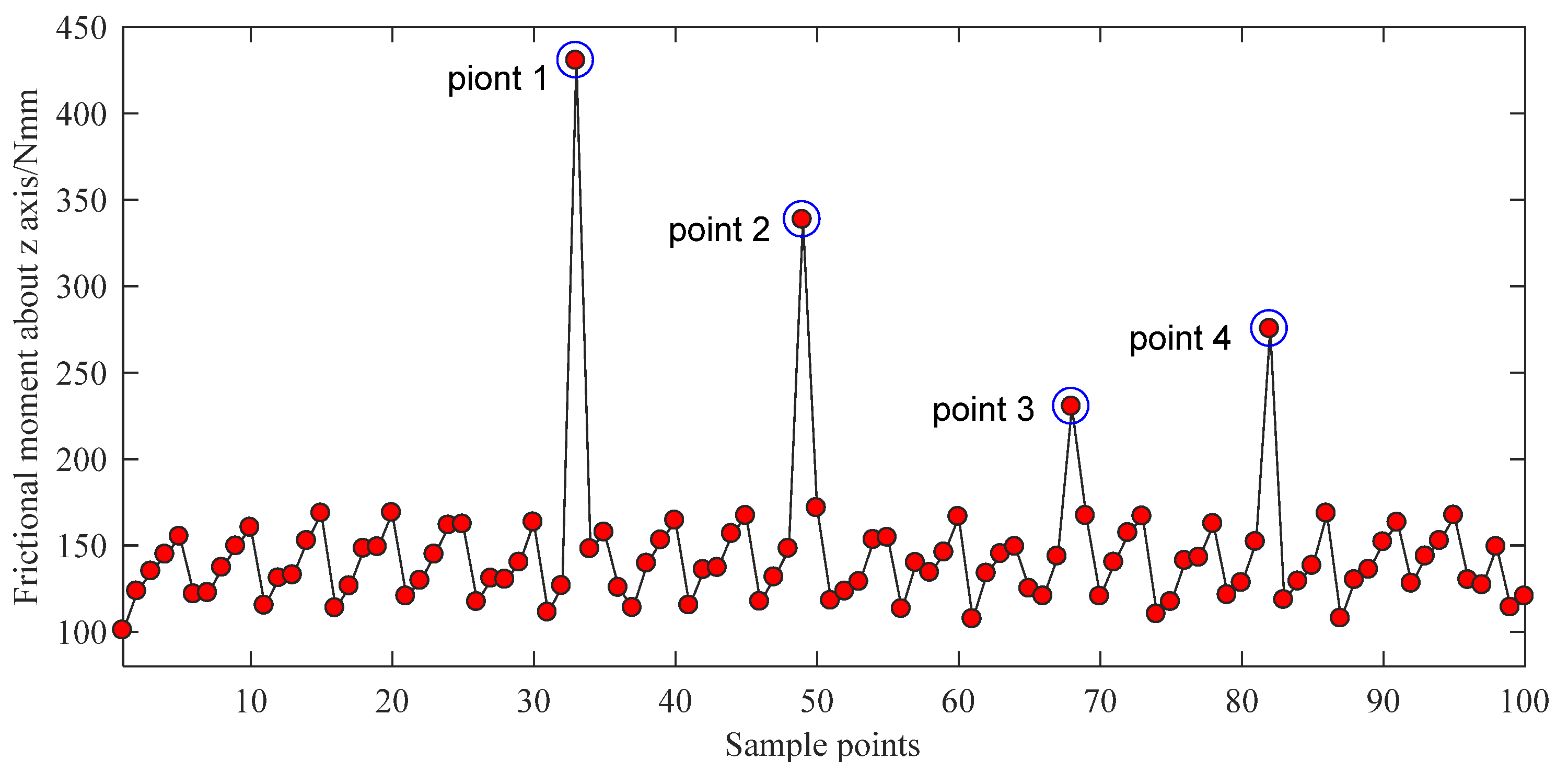
For the material of the bowl-shaped tiles 17-4PH is chosen, and 100 N of axial force is applied on the surface of bowl-shaped tiles. The design optimization process is conducted using ANSYS Workbench 17.0 (ANSYS Inc., Pittsburgh, PA, USA). The direct optimization method has been utilized and requires an appropriate sample size to make the calculation accurate. Therefore, the best adaptive tetrahedral mesh division approach is adopted. The element size on the top of the bowl-shaped tiles is set as 1.5 mm, and the element size in the bottom of the bowl-shaped tiles is set as 1 mm. The maximum friction torque is selected as the main optimization objective. The screening method is selected as the optimization algorithm. The equivalent stress of the material is selected as the constrained condition. According to the variation range of optimized parameters, 100 groups of data are selected as samples through ANSYS software. The optimization results are shown in
Figure 6 and
Figure 7.
As shown in
Figure 6 and
Figure 7, there are five singular points for the optimization analysis. Models were built using the parameters of these five singular points. It is found that the extreme values are caused by two main factors. First, some models have extremely thin edges. Second, some singular points of the grid are found on the other models. Therefore, the data of these five points should be abandoned. By reordering the rest results, the optimal parameters P
1 = 4.1551, P
2 = 3.1031, P
3 = 2.0355, and P
4 = 13.836 can be easily found. After rounding this dataset, the optimal structural parameters of the bowl-shaped tiles are obtained, as shown in
Table 2.