Hip Lift Transfer Assistive System for Reducing Burden on Caregiver’s Waist
Abstract
1. Introduction
1.1. Background
1.2. Related Works
1.3. Positioning of This Study
- correspondence of elderly people with upper limb dysfunction
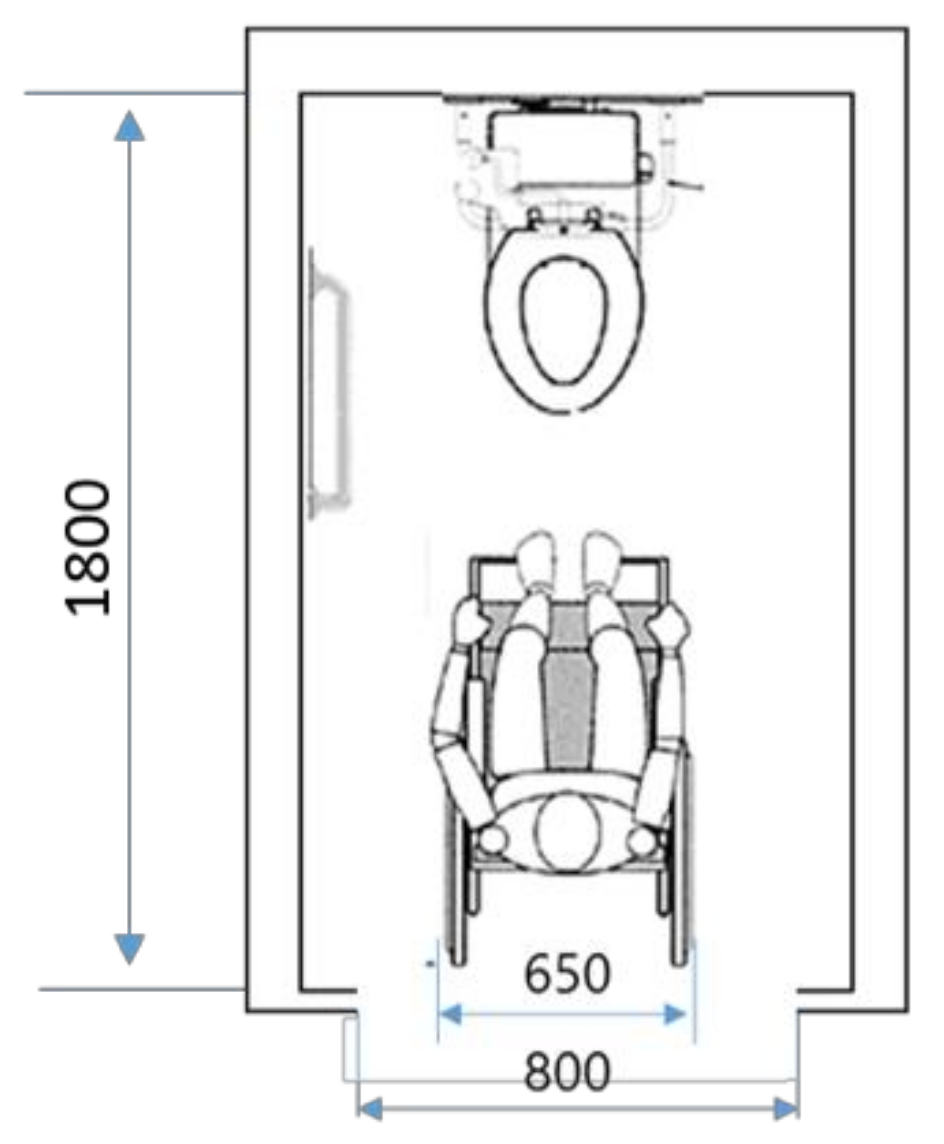
- device structures that can be used in toilet space
- ease of operation
- reduction of labor and time during use
2. Development Requirements Adapted to Elderly Facilities Conditions
2.1. Visit Investigation to the Elderly Facilities
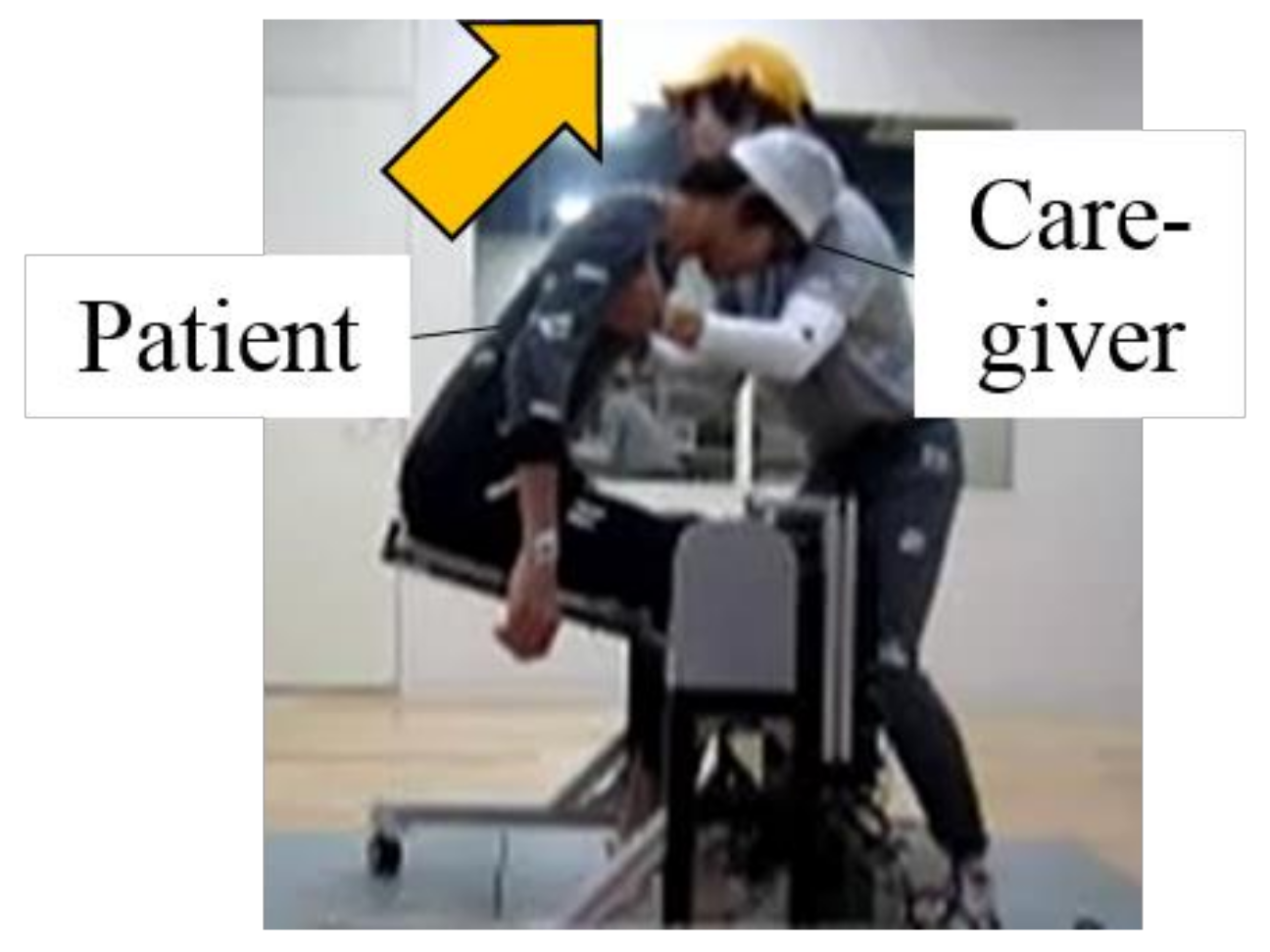
2.2. Current Status of Transferring in the Toilet
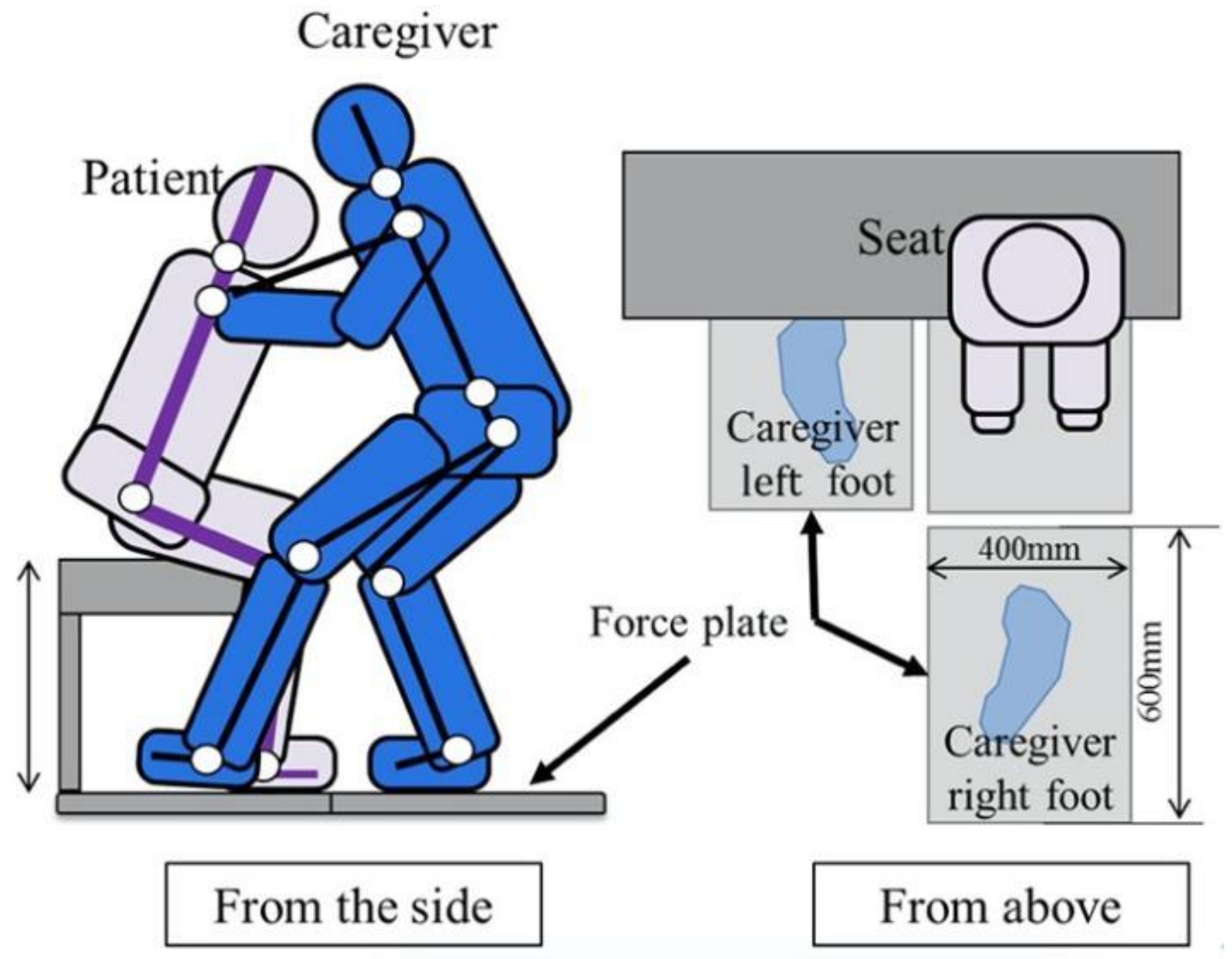
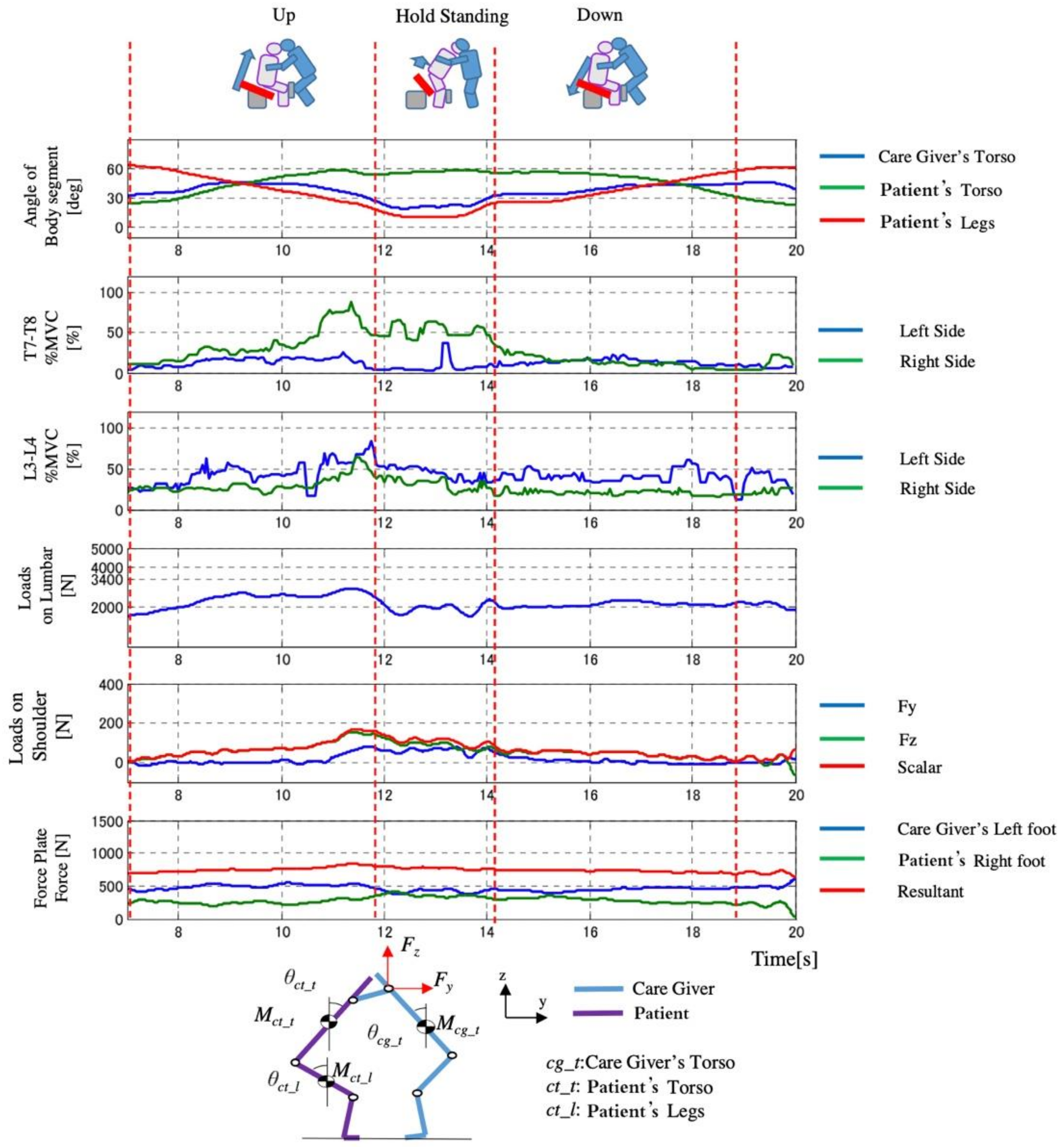
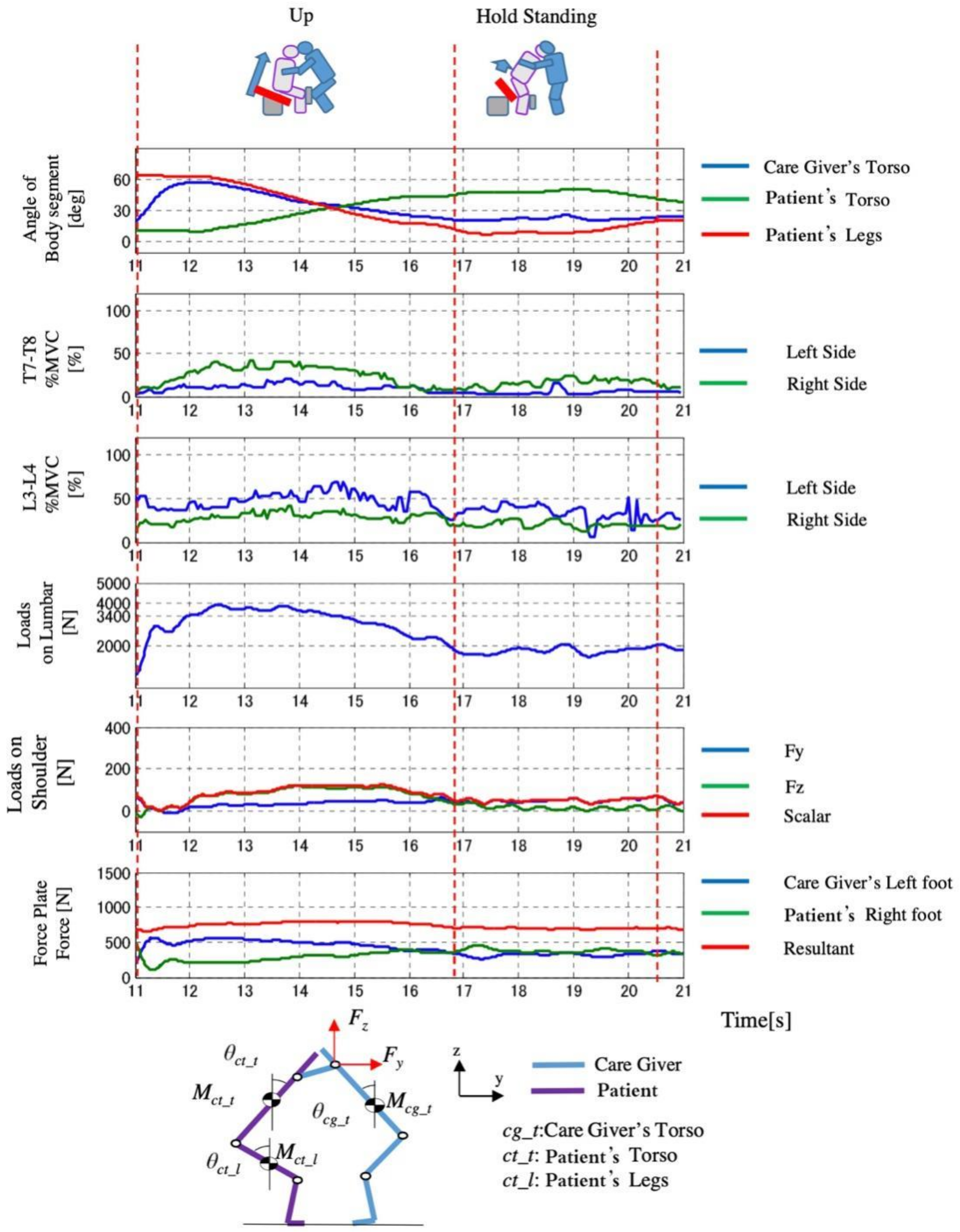
2.3. Lumbar Burden in the Transfer Movement
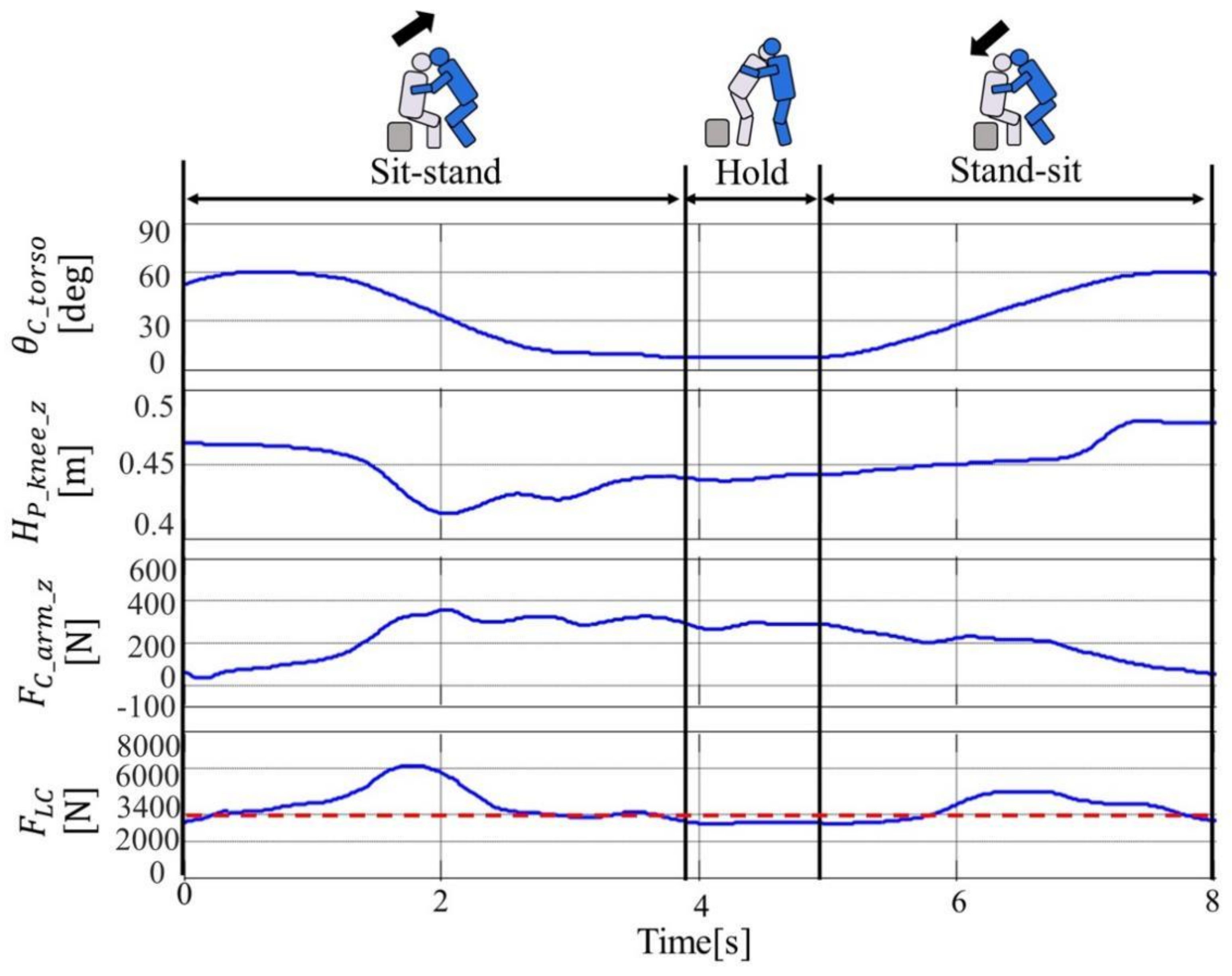
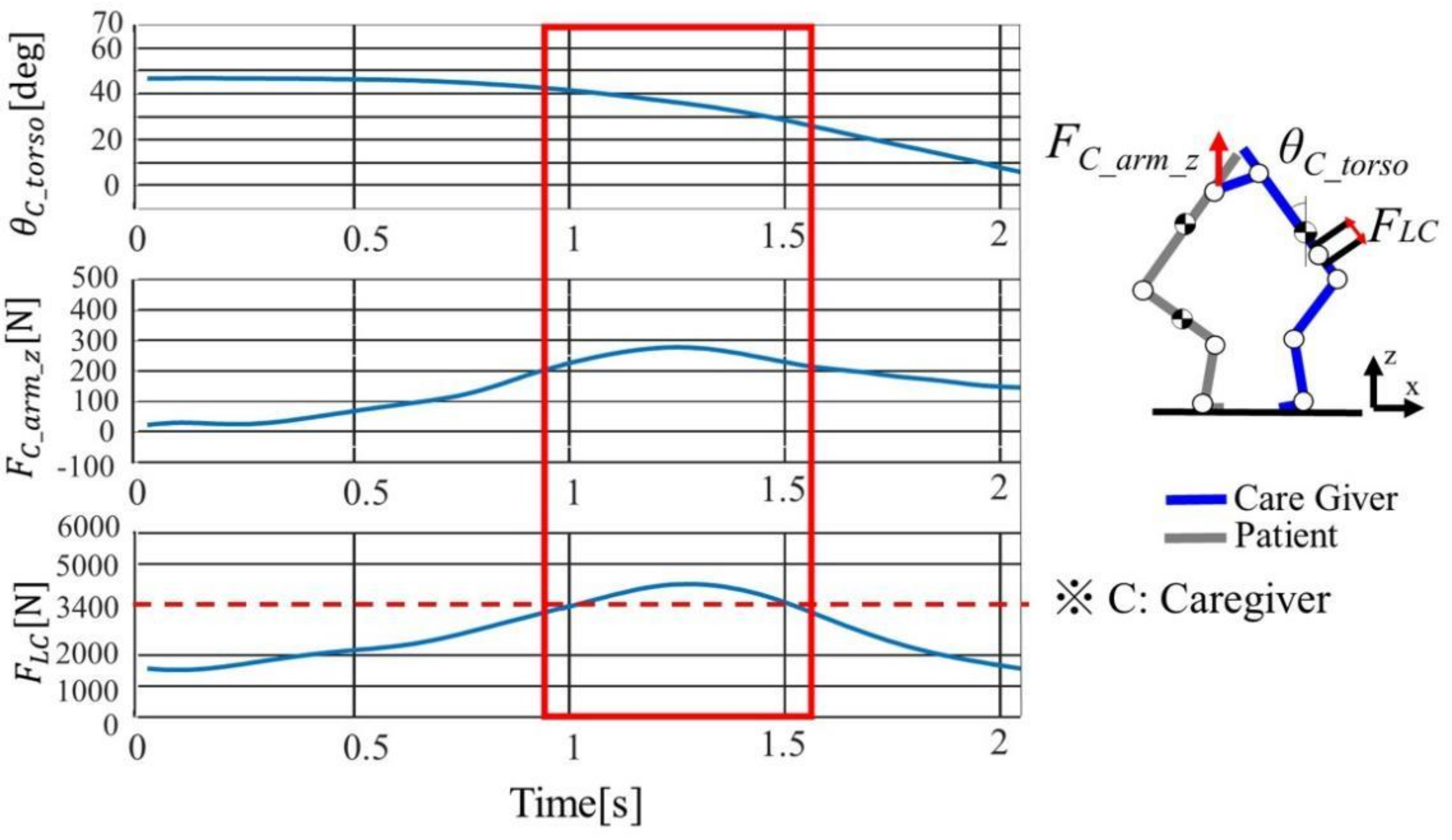
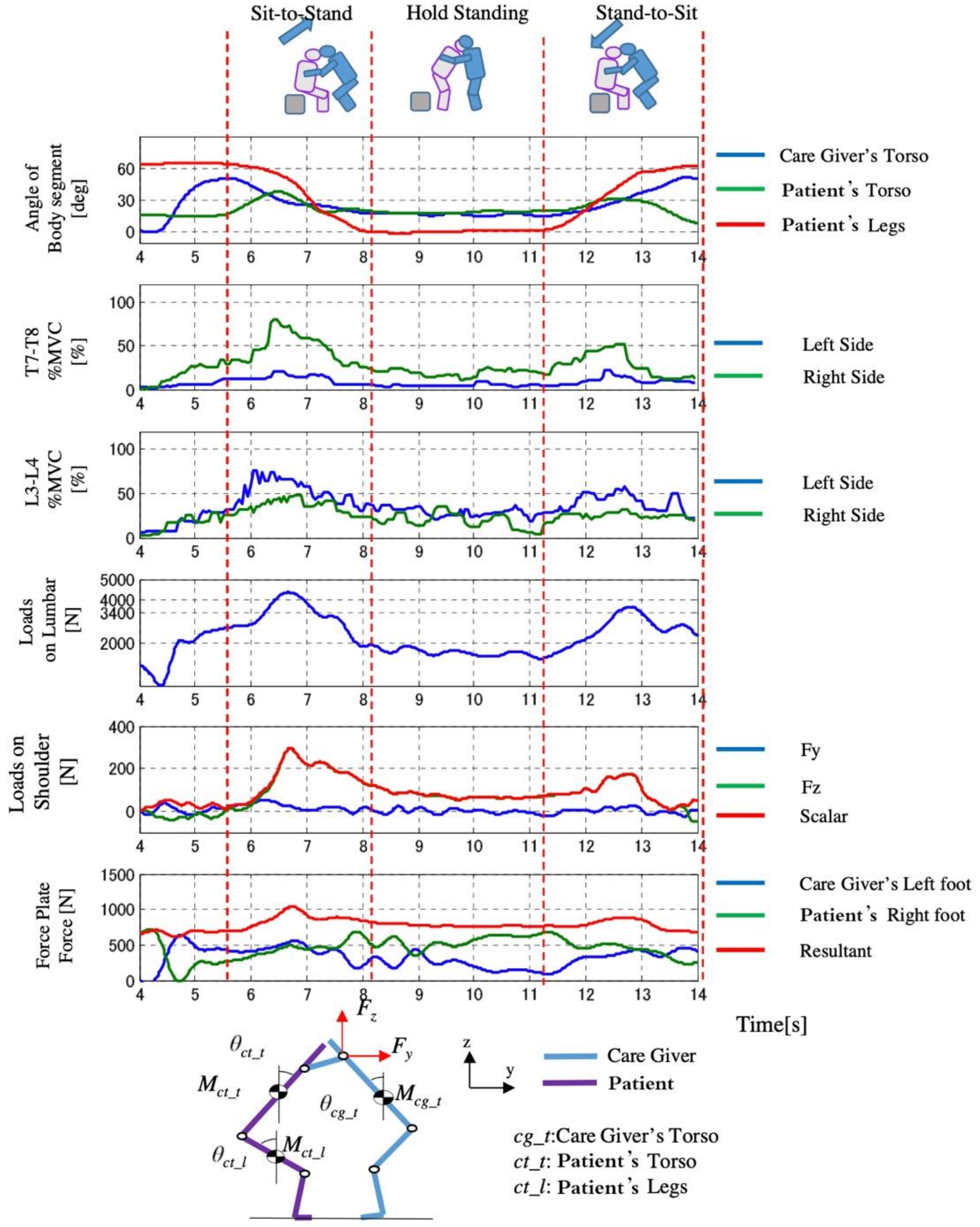
2.3.1. Grasping the Time When the Lumbar Burden Increases
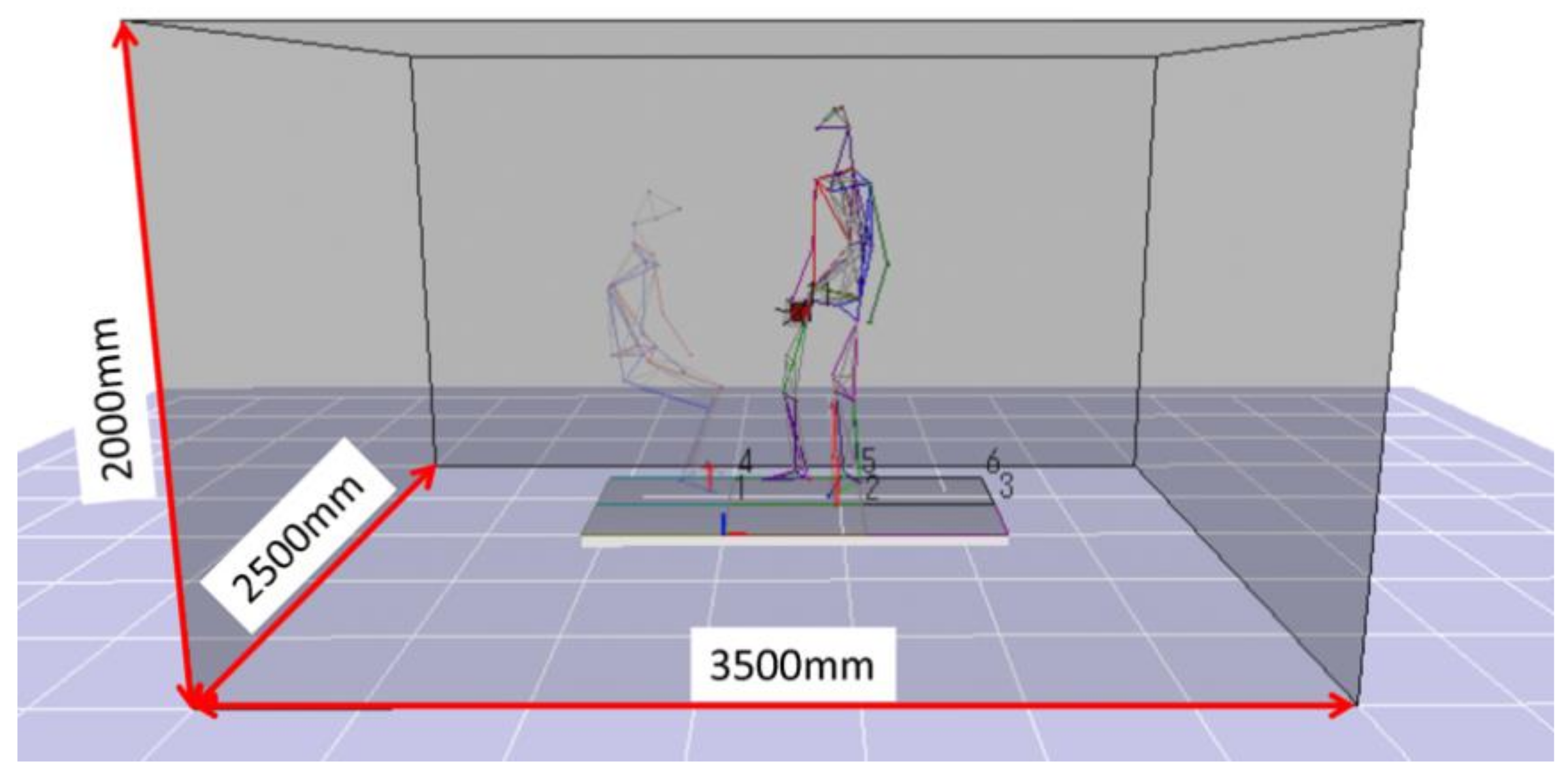
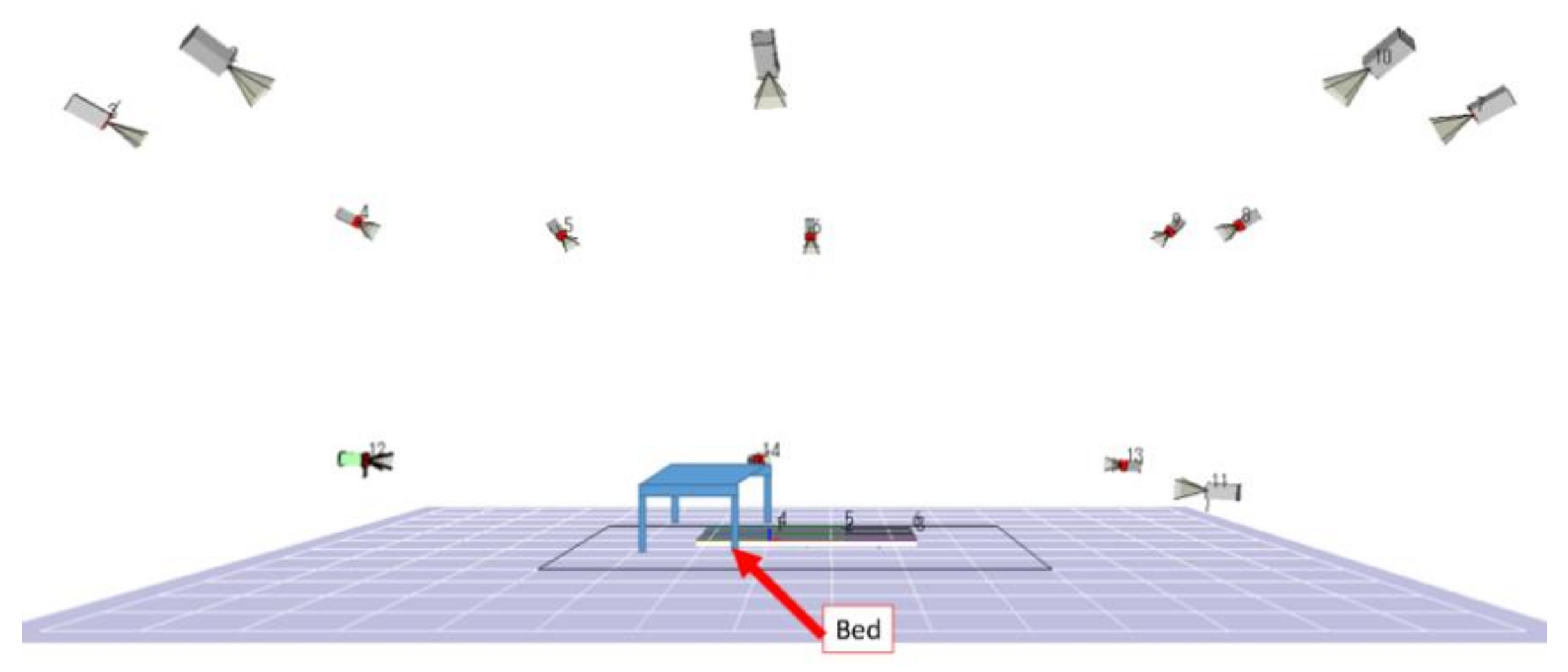
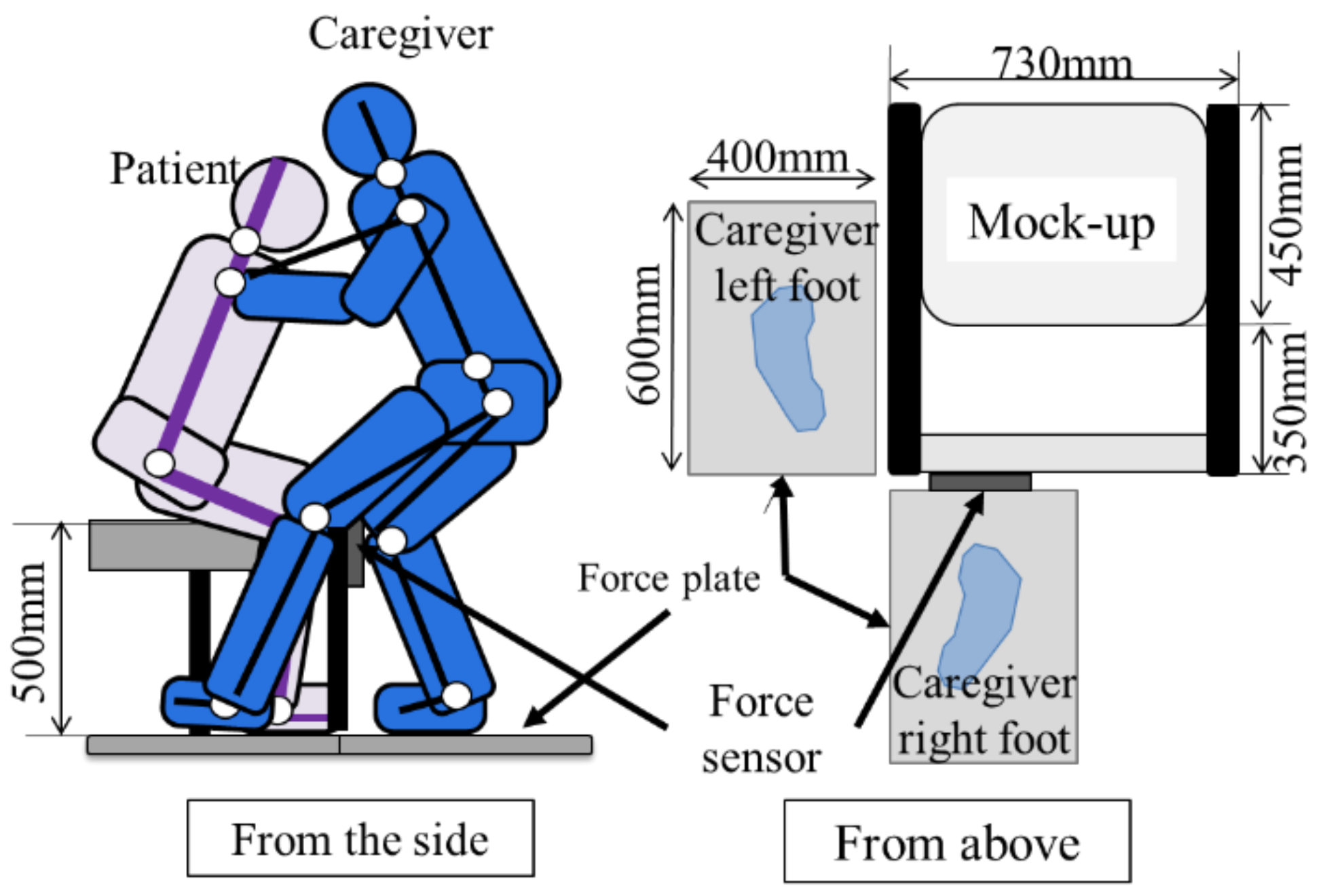
2.3.2. Three-Dimensional Motion Analysis Device
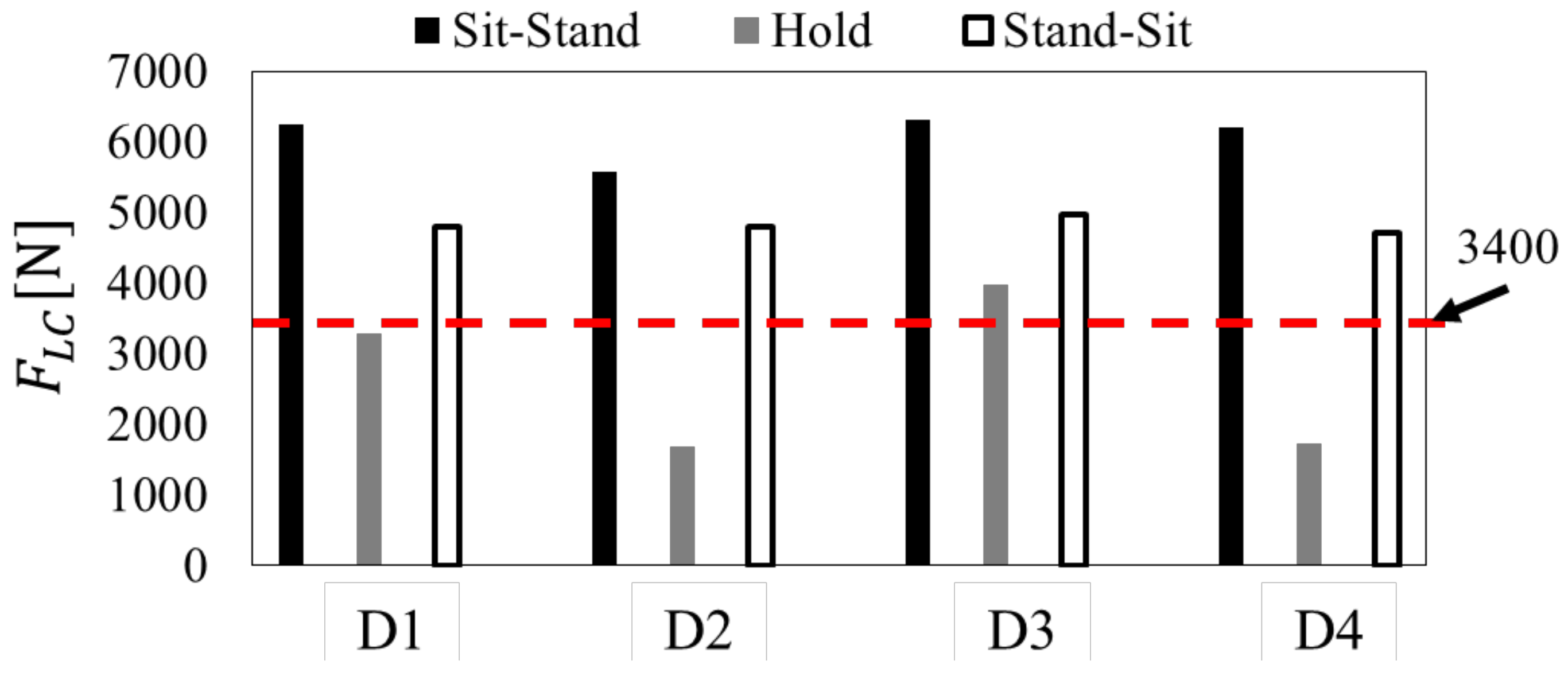
2.3.3. Experimental Results and Discussion
2.4. Assistive Method Based on Motion Analysis
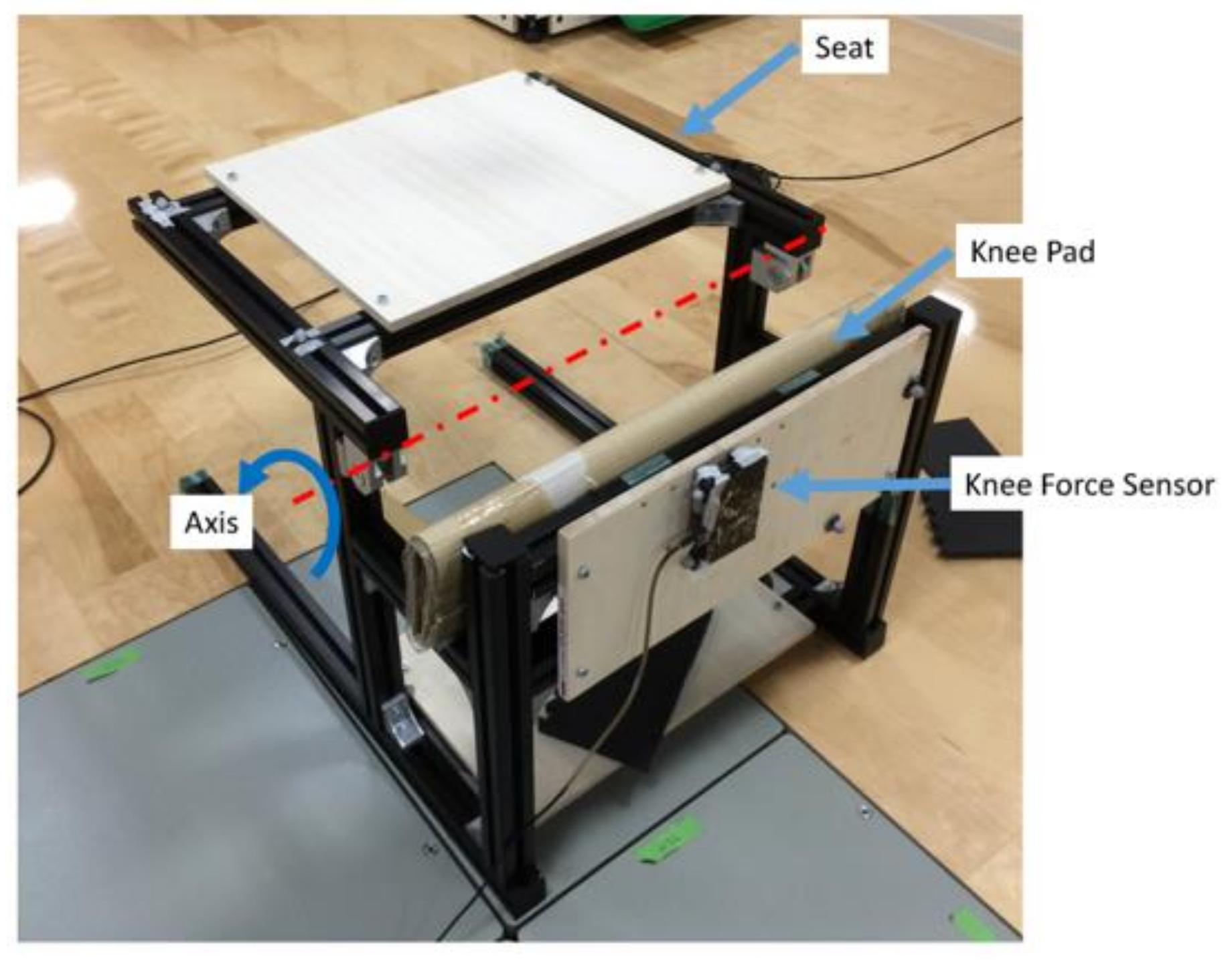
2.4.1. Mock-Up
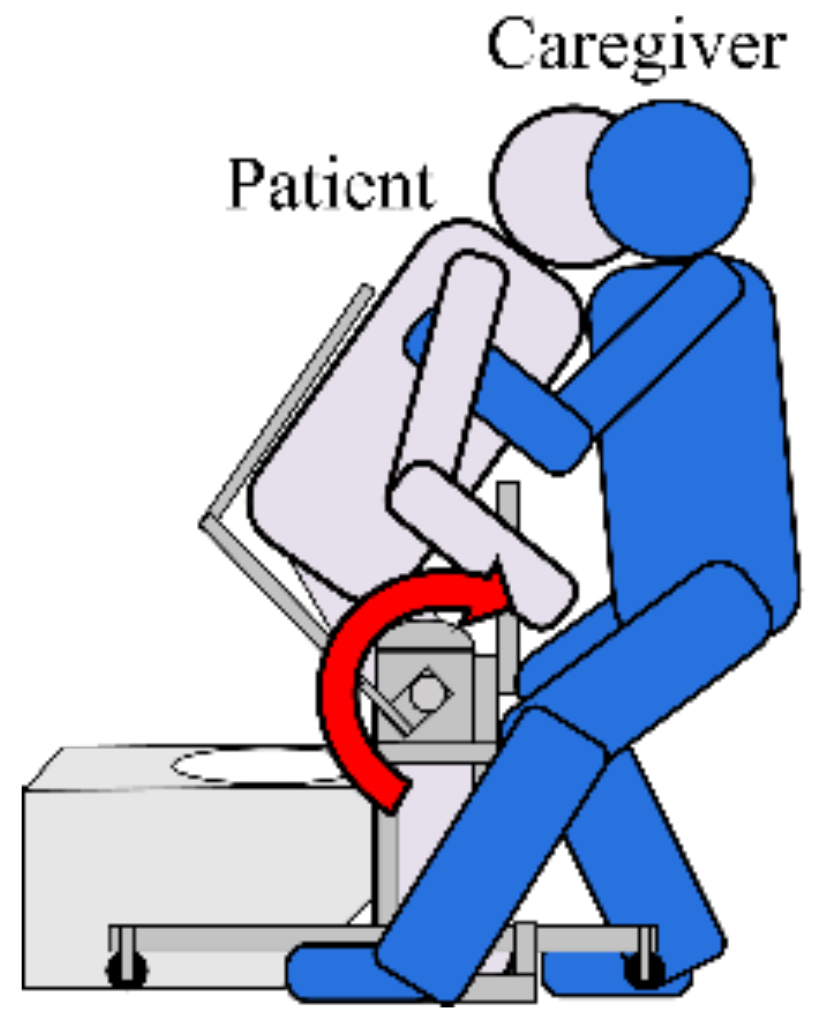
2.4.2. Movement Assisted by Device
2.4.3. Lumbar Burden Factor of Caregiver
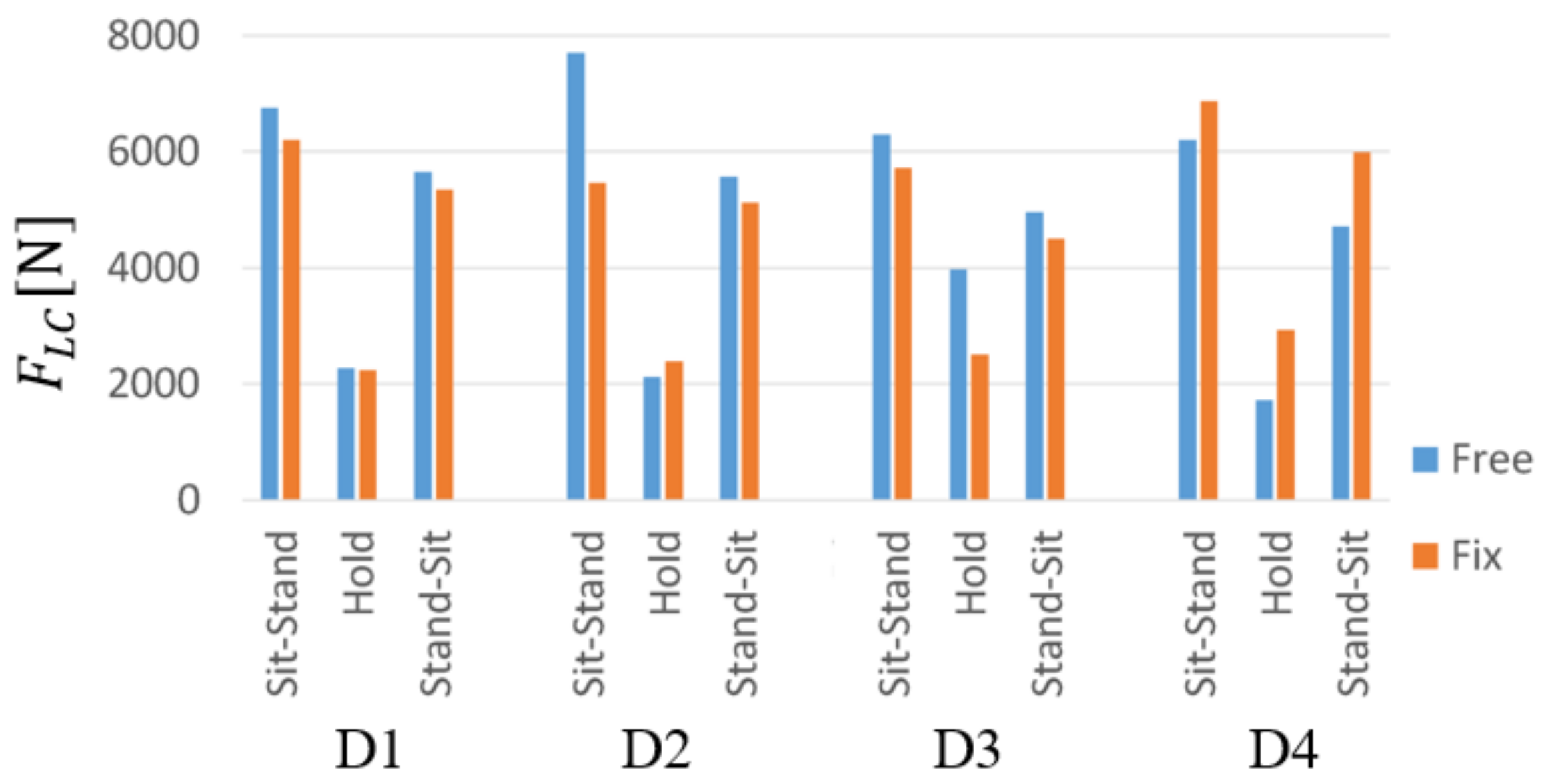
2.4.4. Extraction of Lumbar Burden Factor in Transfer Movement
2.4.5. Experimental Results and Discussion
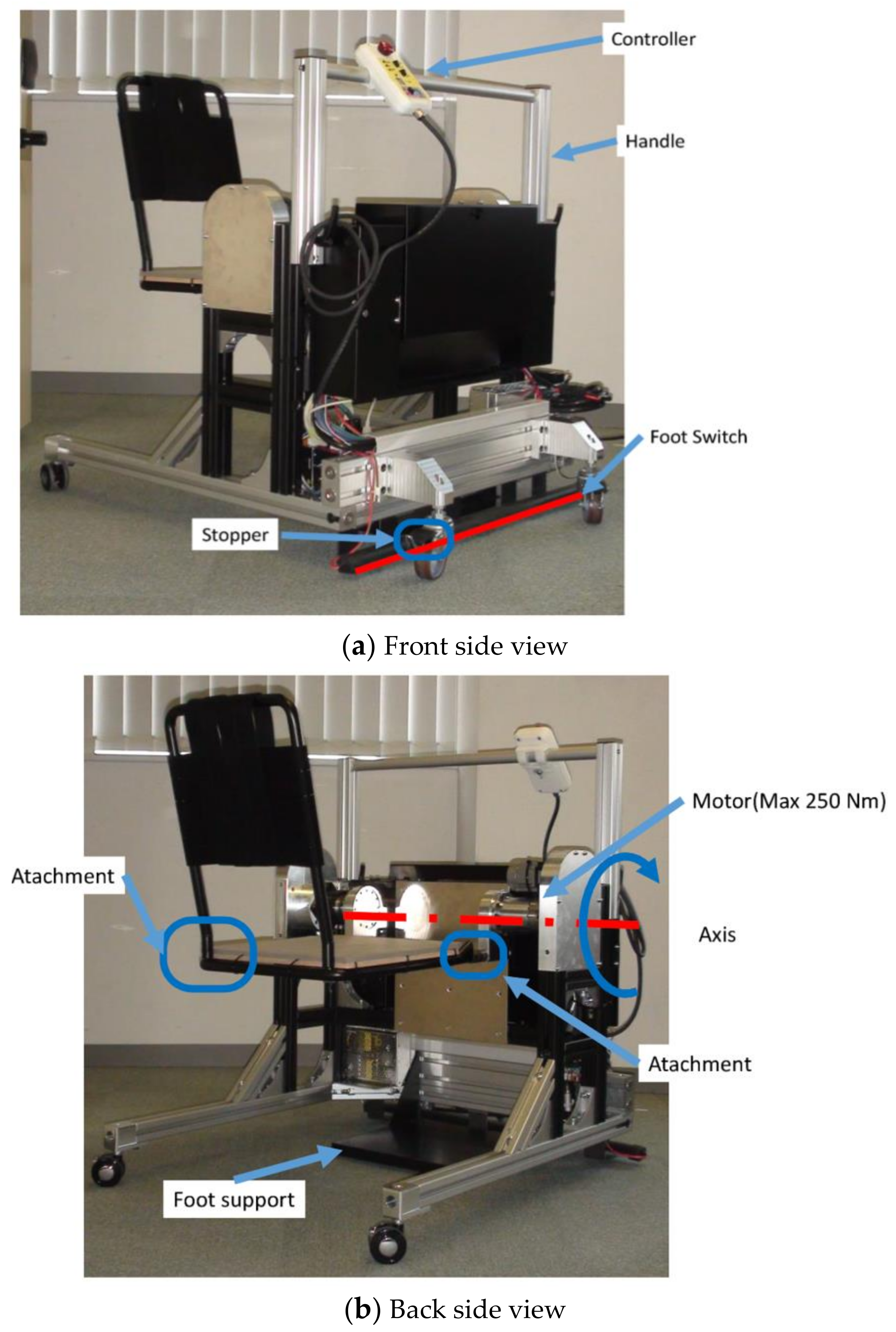
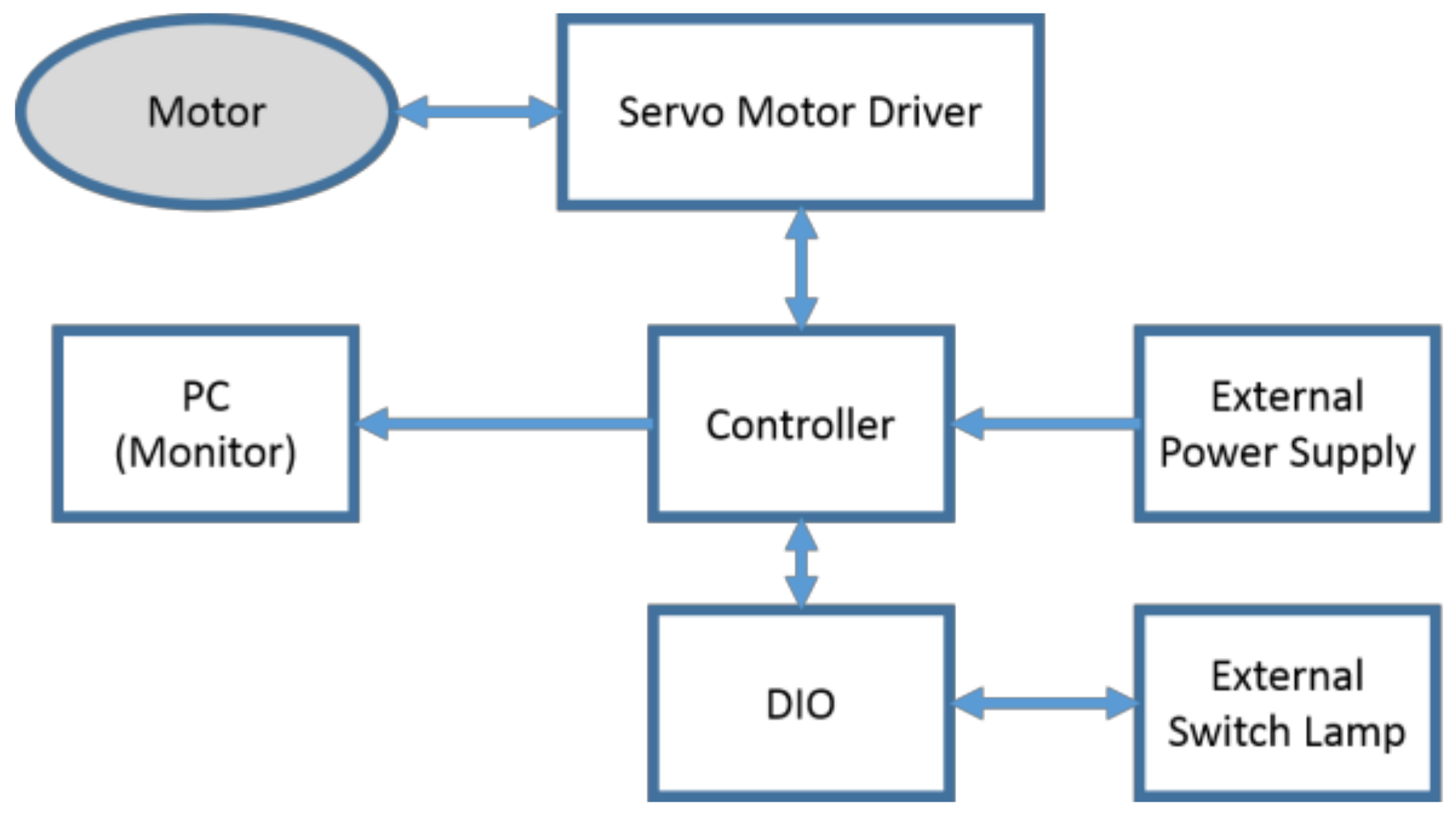
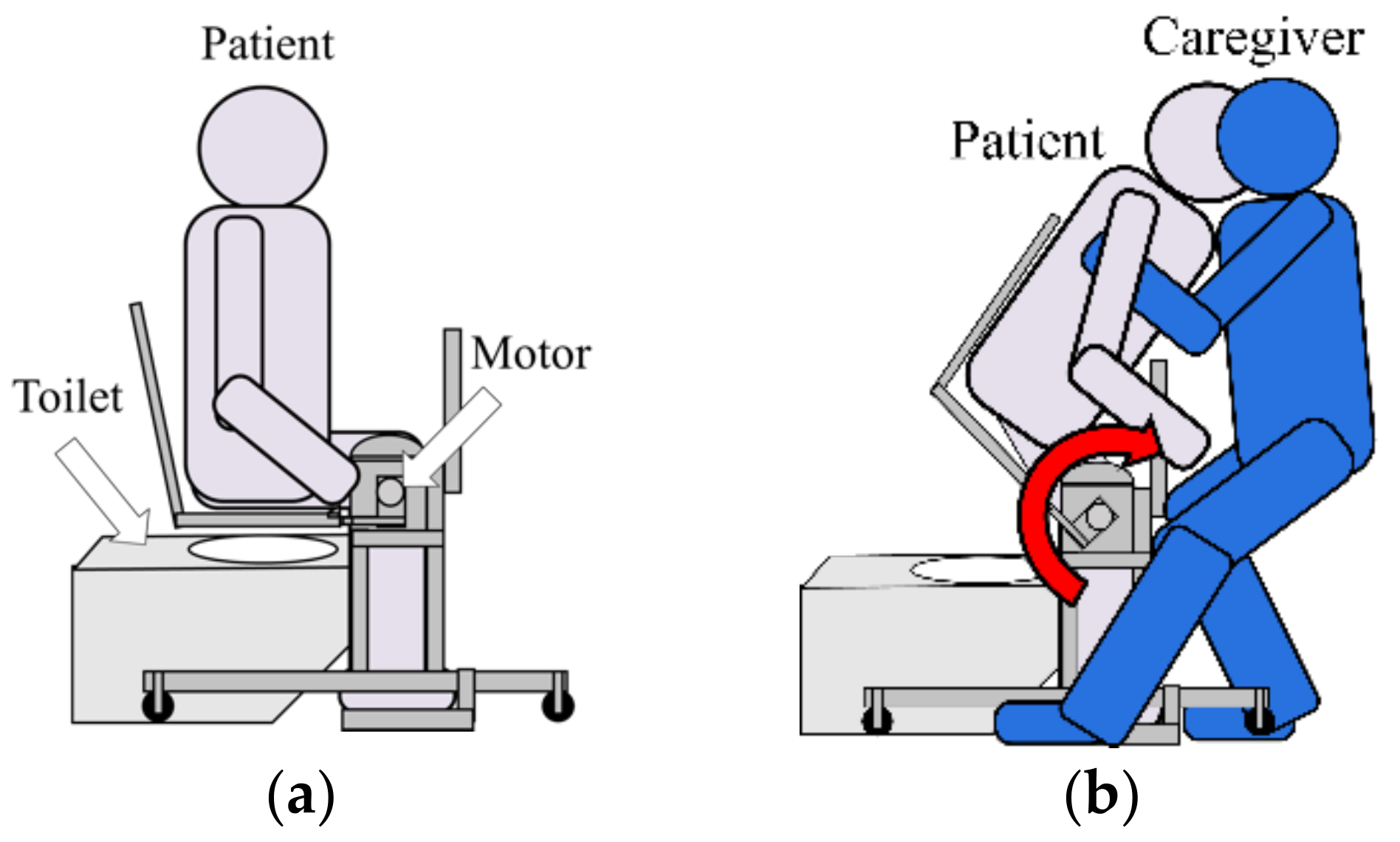
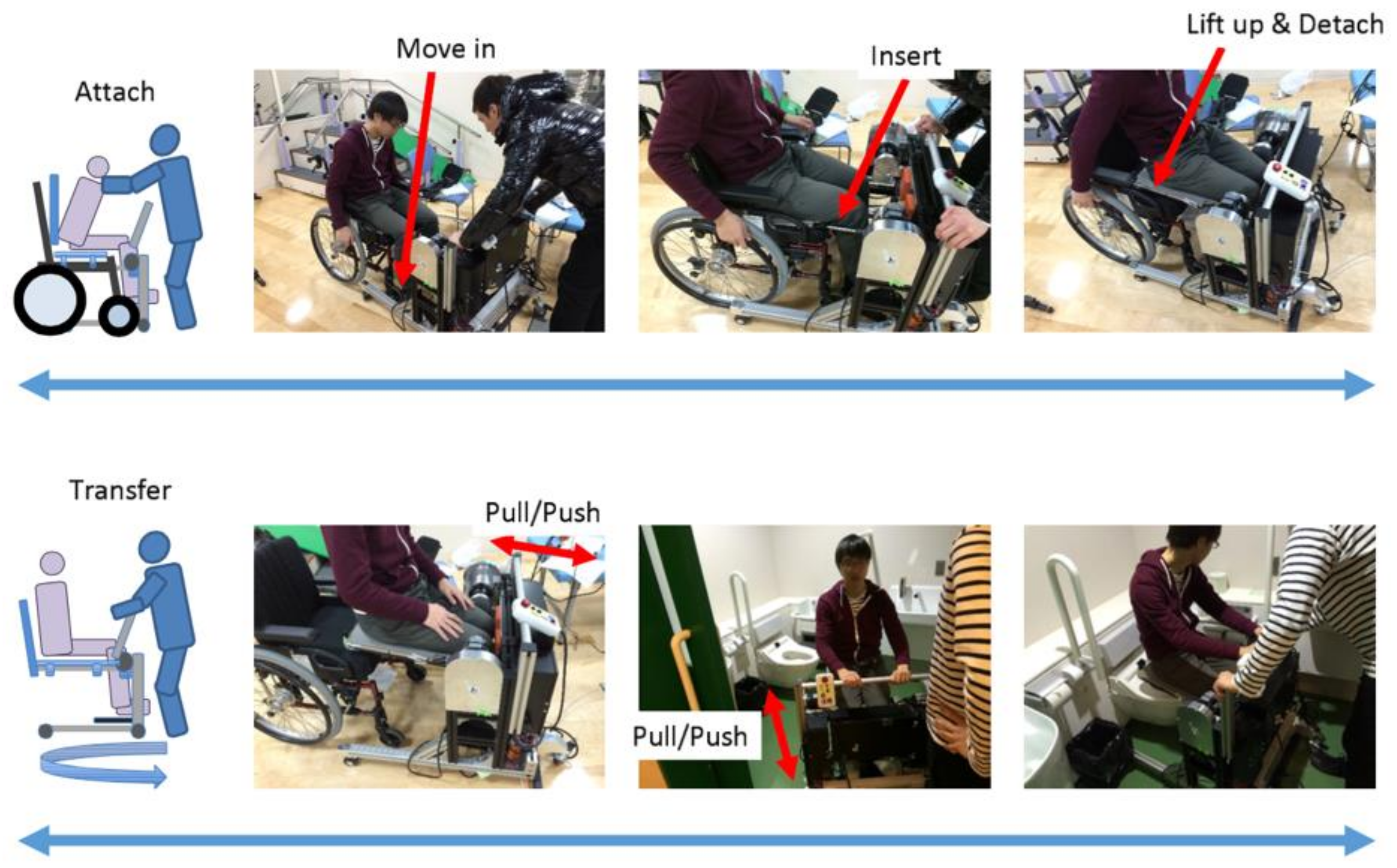
3. Development of Transfer Assistive Device
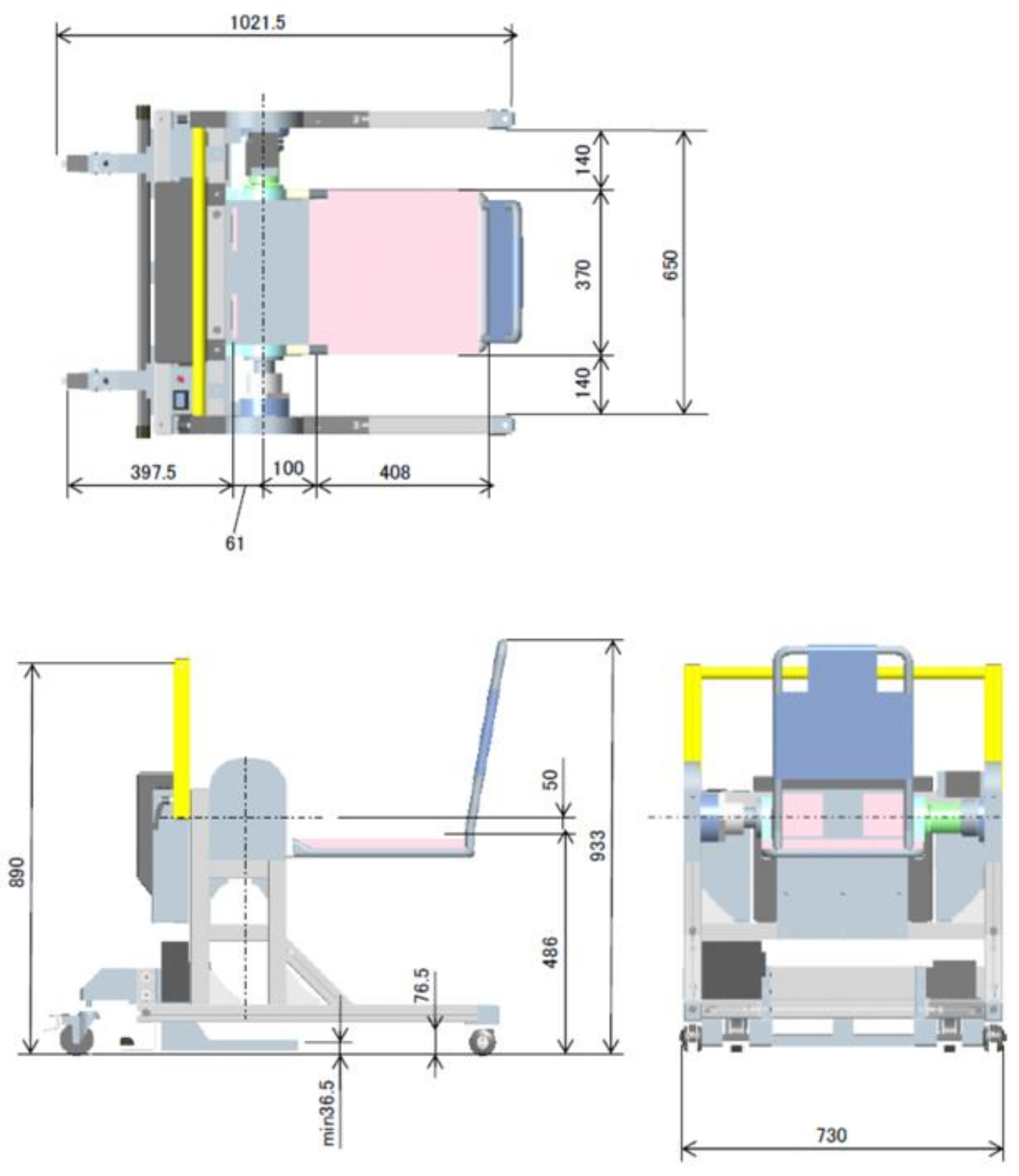
3.1. Functional Requirements
- Standing/sitting motion assistance
- Standing hold assistance
- Mobility assistance
- Seat attachment/detachment
3.2. Device Specifications
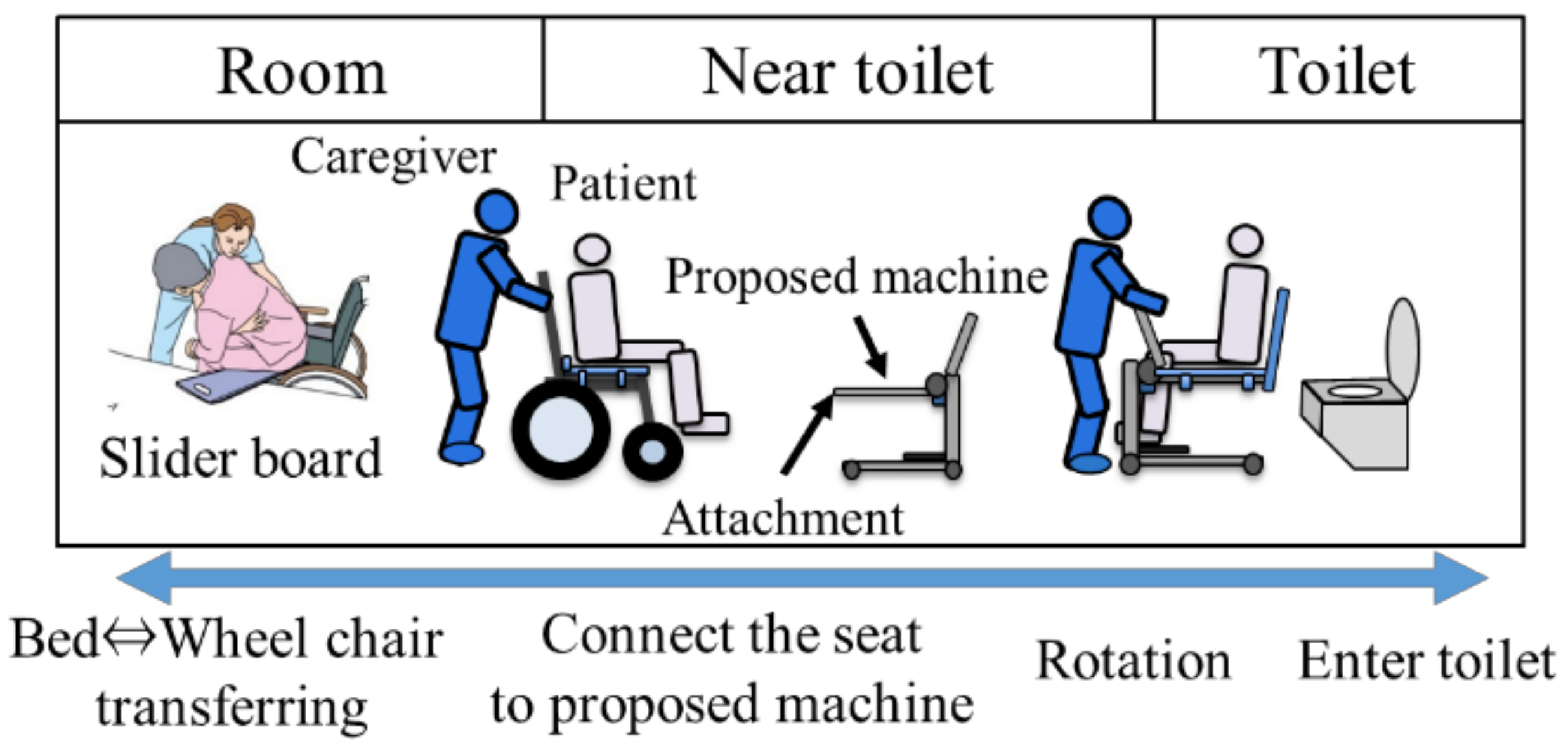
3.3. Usage Method and Scenario
4. Experiments: Operation Evaluation Using Transfer Assistive Device
4.1. Assistive Movement Evaluation
4.1.1. Experimental Setup
4.1.2. Experimental Method
- Control Condition
- Automatic Lifting
- Assist Rise
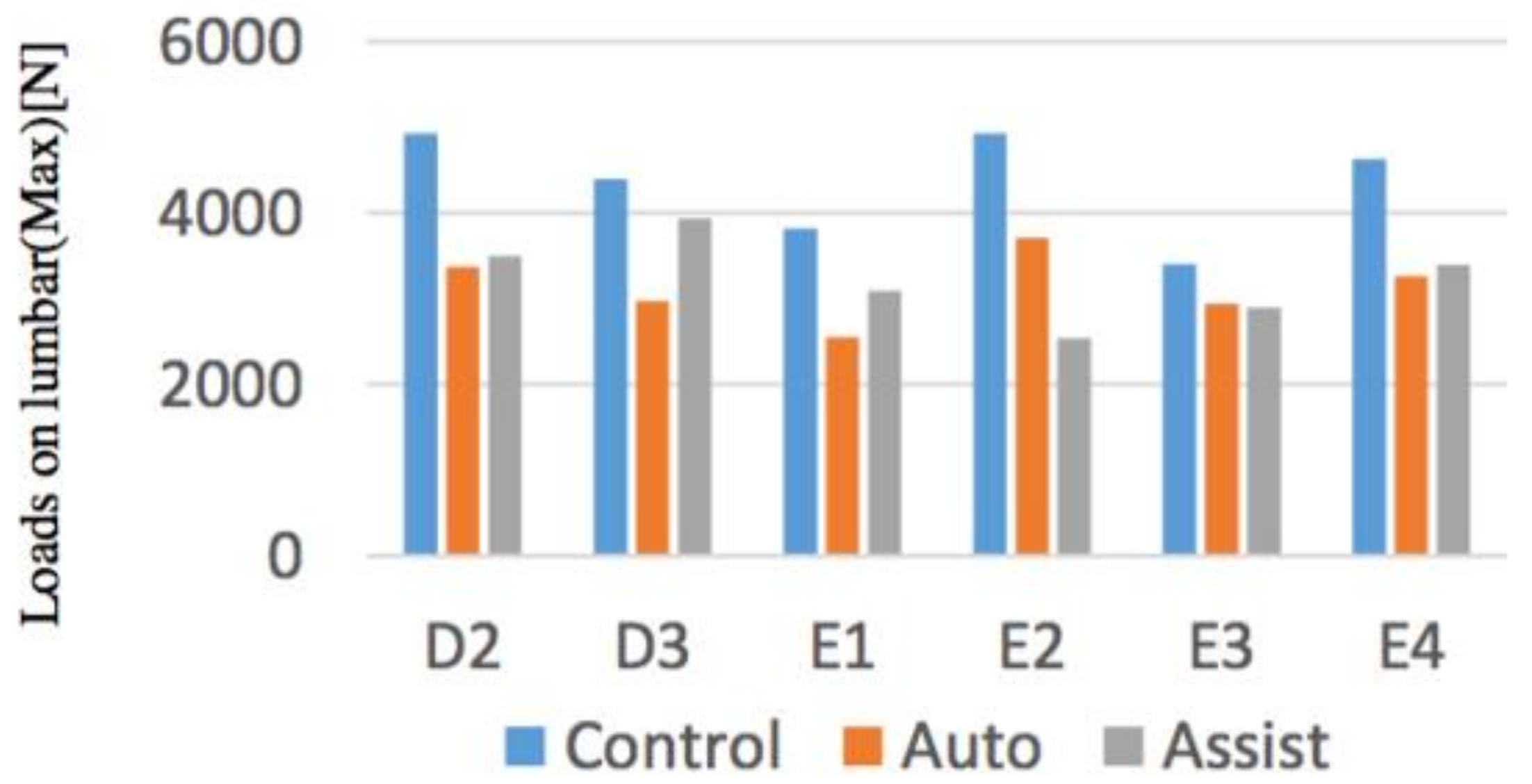
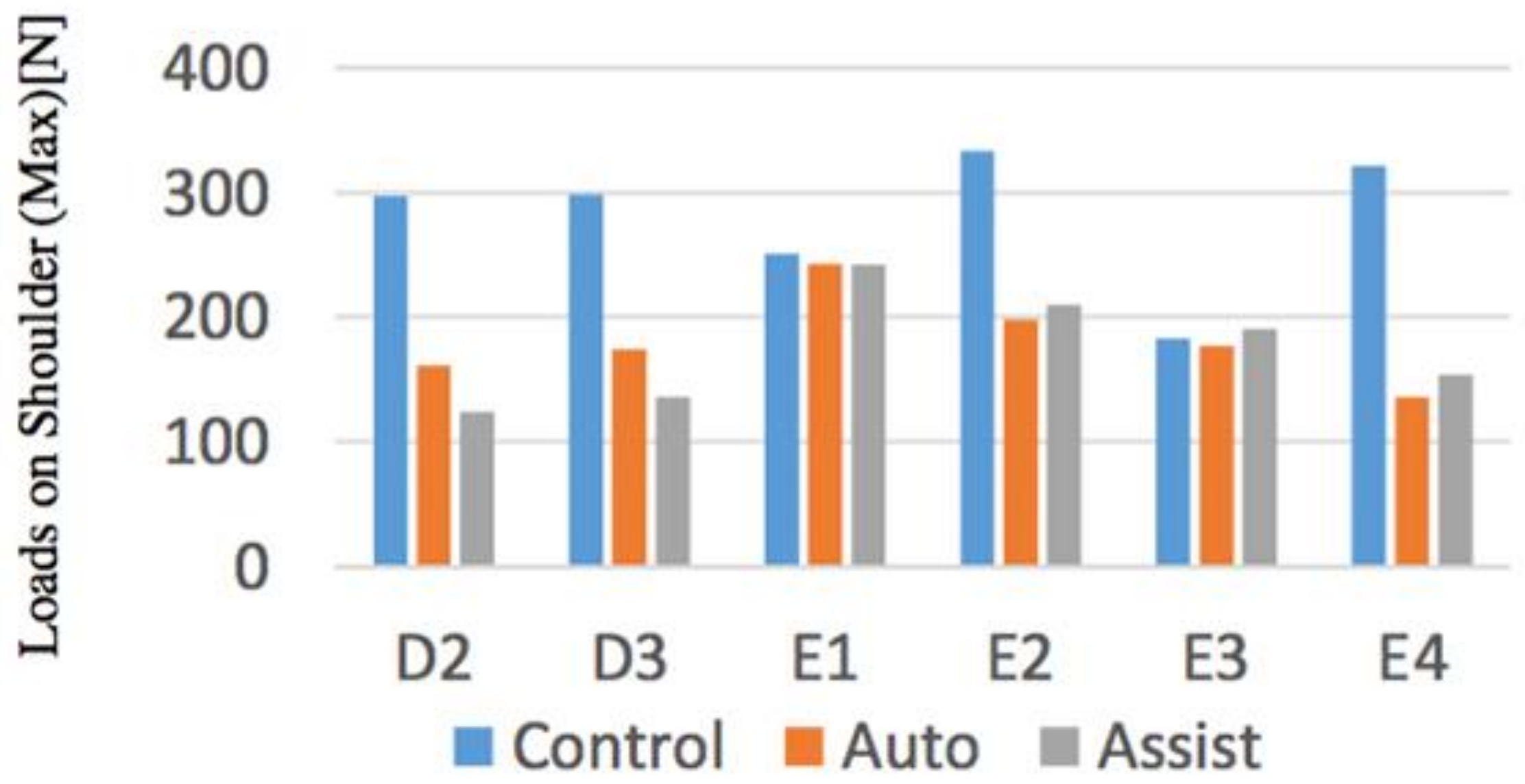
4.1.3. Experimental Results
4.1.4. Discussion
- Comparison of both conditions
- Assist operation
- Seat raising and lowering operation in general
4.2. Operation in the Toilet
4.2.1. Experimental Setup
4.2.2. Experimental Results
- It is useful for transferring to the toilet of elderly people with reduced sitting abilities, which was difficult to transfer to the toilet, and can be used for many elderly residents.
- Elderly people who have begun to lose their standing ability due to the low possibility of knee breaks and backward falls will be able to go to the bathroom with peace of mind with almost independent movements.
- By adjusting the operation method and the strength of assistance, according to the caregiver and the elderly, the burden on the caregiver can be reduced, the independence of the elderly can be maintained. It is also useful for maintaining ADL for a long time from the viewpoint of disease prevention.
4.2.3. Discussion
- Steering sits difficult with the elderly on the device, and it is necessary to simplify the approaching motion to the toilet and wheelchair.
- When transferring the elderly who has a low sitting hold ability and an unstable trunk, arm support during movement is required.
- It is necessary to consider the method of attaching and detaching the seat surface. In addition, the seat surface must be a soft component because it does not interfere with wheelchair seating (such as the use of cushions suitable for the elderly).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reiwa 1st Edition White Paper on Aging Society (Whole Version). Available online: https://www8.cao.go.jp/kourei/whitepaper/w-2019/zenbun/01pdf_index.html (accessed on 22 February 2021).
- Yang, Y.; Zheng, R.; Zhao, L. Population aging, health investment and economic growth: Based on a cross-country panel data analysis. Int. J. Environ. Res. Public Health 2021, 18, 1801. [Google Scholar] [CrossRef] [PubMed]
- Mehrdad, R.; Shams-Hosseini, N.S.; Aghdaei, S.; Yousefian, M. Prevalence of low back pain in health care workers and comparison with other occupational categories in Iran: A systematic review. Iran. J. Med. Sci. 2016, 41, 467. [Google Scholar]
- Rasmussen, C.D.; Holtermann, A.; Mortensen, O.S.; Søgaard, K.; Jørgensen, M.B. Prevention of low back pain and its consequences among nurses’ aides in elderly care: A stepped-wedge multi-faceted cluster-randomized controlled trial. BMC Public Health 2013, 13, 1088. [Google Scholar] [CrossRef] [PubMed]
- Kurumatani, N.; Morita, N. Work related movement disorders of nurses—Basic of prevention and Countermeasures (special collection of human care services and ergonomics). J. Labor Sci. 2004, 59, 709–713. [Google Scholar]
- Study Group Report on Revision and Spread of Low Back Pain Prevention Measures Guidelines in the Workplace. Ministry of Health, Labor and Welfare. 2013. Available online: https://www.mhlw.go.jp/stf/shingi/2r98520000034qqlatt/2r98520000034qs-0.pdf (accessed on 22 February 2021).
- Haya, M.A.; Ichikawa, S.; Wakabayashi, H.; Takemura, Y. Family Caregivers’ Perspectives for the Effect of Social Support on their Care Burden and Quality of Life: A Mixed-Method Study in Rural and Sub-Urban Central Japan. Tohoku J. Exp. Med. 2019, 247, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa Kiyoshi, Basic Knowledge of Selection and Utilization of Lift and other Moving Supplies. Available online: https://hcr.or.jp/cms/wp-content/uploads/howto_2020_1_2.pdf (accessed on 2 September 2021).
- Sasaki, H.; Katsuhira, J.; Watanabe, H.; Saijou, F.; Saito, A. Low Back Load of Caregiver During Transfer Movement Using Assistive Devices. Phys. Ther. 2007, 34, 294–301. [Google Scholar]
- Satoh, H. Transferring-care assistance with robot suit HAL. Trans. Jpn. Soc. Mech. Eng. Ser. C 2010, 76, 227–235. [Google Scholar] [CrossRef]
- Sato, Y.; He, J.; Kobayashi, H.; Muramatsu, Y.; Hashimoto, T.; Kobayashi, H. Development and Quantitative Performance Estimation of the Back Support Muscle Suit. Jpn. Soc. Mech. Eng. Proc. C 2012, 78, 2987–2999. [Google Scholar] [CrossRef]
- Keiroka, Y.I. Device Smart Suit Lite with Trunk Stabilizing Effect and Muscle Assistive Effect. Ph.D. Thesis, Hokkaido University, Sapporo, Japan, 25 March 2014. [Google Scholar]
- Sankai, Y. HAL: Hybrid assistive limb based on cybernics. In Robotics Research; Springer: Berlin/Heidelberg, Germany, 2010; pp. 25–34. [Google Scholar]
- Ai Ijo-Kun Mobile Assistance Robot, Art Plan Co., Ltd. Available online: http://www.artplan.ne.jp/fukusikiki-syouhinsetumei.html (accessed on 22 February 2021).
- Transfer Care Assist, Toyota Motor Corporation. Available online: https://global.toyota/jp/download/2829198/ (accessed on 2 September 2021).
- Komawarisan-J, Hearts-Eiko. Available online: https://www.scrio.co.jp/fs/kaigo/2240 (accessed on 2 September 2021).
- Skylift, I-Sonex. Available online: https://www.scrio.co.jp/fs/kaigo/4775 (accessed on 2 September 2021).
- Molift Quick Raiser 1, Molift. Available online: https://www.etac.com/products/patient-handling/hoists/molift-quick-raiser-1/ (accessed on 2 September 2021).
- Tomioka, K.; Kumagai, S.; Kosaka, H.; Yoshida, J.; Tabuchi, T.; Kosaka, J.; Arai, Y. Equipment at the special nursing homes for the elderly: A workplace survey of new nursing homes in Osaka Prefecture. Sangyo Eiseigaku Zasshi = J. Occup. Health 2006, 48, 49–55. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sivakanthan, S.; Blaauw, E.; Greenhalgh, M.; Koontz, A.M.; Vegter, R.; Cooper, R.A. Person transfer assist systems: A literature review. Disabil. Rehabil. Assist. Technol. 2021, 16, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, R.H.; Pugazhenthi, S. Design and development of a robotic self-transfer device for wheelchair users. J. Enabling Technol. 2017, 11, 59–72. [Google Scholar] [CrossRef]
- Ulrey, B.L.; Fathallah, F.A. Subject-specific, whole-body models of the stooped posture with a personal weight transfer device. J. Electromyogr. Kinesiol. 2013, 23, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Blaauw, E.R.; Greenhalgh, M.; Vegter, R.; Bass, S.; Kulich, H.; Grindle, G.G.; Cooper, R.; Koontz, A.M.; Cooper, R.A. Assessment of Muscle Activation of Caregivers Performing Dependent Transfers with a Novel Robotic-Assisted Transfer Device Compared with the Hoyer Advance. Am. J. Phys. Med. Rehabil. 2021, 100, 885–894. [Google Scholar] [CrossRef] [PubMed]
- Elderly Care Fact-Finding Results, Ministry of Health, Labor and Welfare. 2007. Available online: https://www.mhlw.go.jp/shing-i/2007/11/dl/s1109-10.html (accessed on 2 September 2021).
- Hattori, K.; Yamaguchi, M.; Michiko, M.; Junko, S.; Makiko, O.; Nagano, M. Study of Knowledge Supporting Basic Nursing Arts (2): Philological Research on Elimination. J. Juntendo Med. Coll. Nurs. 2000, 11, 72–87. [Google Scholar]
- Ministry of Land, Infrastructure, Transport and Tourism: Architectural Design Standard that Considers the Smooth Movement of the Elderly and Disabled. Available online: https://www.mlit.go.jp/jutakukentiku/build/barrier-free.files/guideline12.pdf (accessed on 22 February 2021).
- JIST9201: 2016 Manual Wheelchair. Available online: https://kikakurui.com/t9/T9201-2016-01.html (accessed on 22 February 2021).
- Yamazaki, N.; Yamamoto, S.; Inoue, T. Measurement of transferring motions and evaluation of caregiver’s lower-back load. Biomechanisms 2002, 16, 195–205. [Google Scholar] [CrossRef][Green Version]
- NIOSH, National Institute for Occupational Safe and Health. Work Practices Guide for Manual Lifting; No. 81-122; Dept. Health and Human Services: Cincinnati, OH, USA, 1981. [Google Scholar]
- Okada, H.; Ae, M.; Fujii, N.; Morioka, Y. Body segment inertia properties of Japanese elderly. Biomechanisms 1996, 13, 125–139. [Google Scholar] [CrossRef]
- AIST Human Body Dimension Database 1991–1992. Available online: https://www.airc.aist.go.jp/dhrt/91-92/ (accessed on 22 February 2021).
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [PubMed]
- Wu, J.; Shino, M. Development of Transfer Assist Equipment by Lower Back Burden Reduction Method of Caregiver. In Proceedings of the 2018 IEEE International Conference on Robotics and Biomimetics (ROBIO), Kuala Lumpur, Malaysia, 12–15 December 2018; pp. 691–696. [Google Scholar]

| ID | Average Nursing Care Level | Numbers of Elderly | Numbers of Caregivers in the Daytime | Ration of Caregivers Having a Backache (%) | Number of Transfers for One Elderly Person (1 Day) |
|---|---|---|---|---|---|
| A1 | 4.1 | 60 | 14 | Not clear | 8 |
| A2 | 3.9 | 60 | 8 | 30 | 16 |
| A3 | 3.9 | 80 | 6.5 | Not clear | 8 |
| A4 | 4.1 | 220 | 30 | Not clear | 8 |
| A5 | 4.3 | 60 | 8 | 20 | 8 |
| A6 | 4 | 38 | 4 | 80 | 18 |
| A7 | 3.9 | 100 | 12 | Not clear | 8 |
| B1 | 4.1 | 96 | 12 | 55 | 8 |
| C1 | 4.1 | 140 | Not clear | 70 | More than 8 |
| Requirements | Mechanisms |
|---|---|
| Can be used in toilet | Proper size (width 730 mm) |
| Prevent rotation | Caster |
| Can be used for patients who have upper limbs or torso disorder | Caregivers can touch patients Assist from patient thighs |
| Prevent patients’ knee fold | Fix patients’ knee |
| Support patient’s weight | Assist of servo motor |
| D2 | D3 | E1 | E2 | E3 | E4 | |
|---|---|---|---|---|---|---|
| Height (cm) | 177 | 179 | 170 | 172 | 170 | 172 |
| Weight (kg) | 67 | 74 | 60 | 55 | 51 | 61 |
| Qualification | PT | Social worker | Stu | Stu | Stu | Stu |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, J.; Shino, M. Hip Lift Transfer Assistive System for Reducing Burden on Caregiver’s Waist. Sensors 2021, 21, 7548. https://doi.org/10.3390/s21227548
Wu J, Shino M. Hip Lift Transfer Assistive System for Reducing Burden on Caregiver’s Waist. Sensors. 2021; 21(22):7548. https://doi.org/10.3390/s21227548
Chicago/Turabian StyleWu, Jiang, and Motoki Shino. 2021. "Hip Lift Transfer Assistive System for Reducing Burden on Caregiver’s Waist" Sensors 21, no. 22: 7548. https://doi.org/10.3390/s21227548
APA StyleWu, J., & Shino, M. (2021). Hip Lift Transfer Assistive System for Reducing Burden on Caregiver’s Waist. Sensors, 21(22), 7548. https://doi.org/10.3390/s21227548






