Reactive Exercises with Interactive Objects: Interim Analysis of a Randomized Trial on Task-Driven NMES Grasp Rehabilitation for Subacute and Early Chronic Stroke Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methodology for the Design of the System Concept
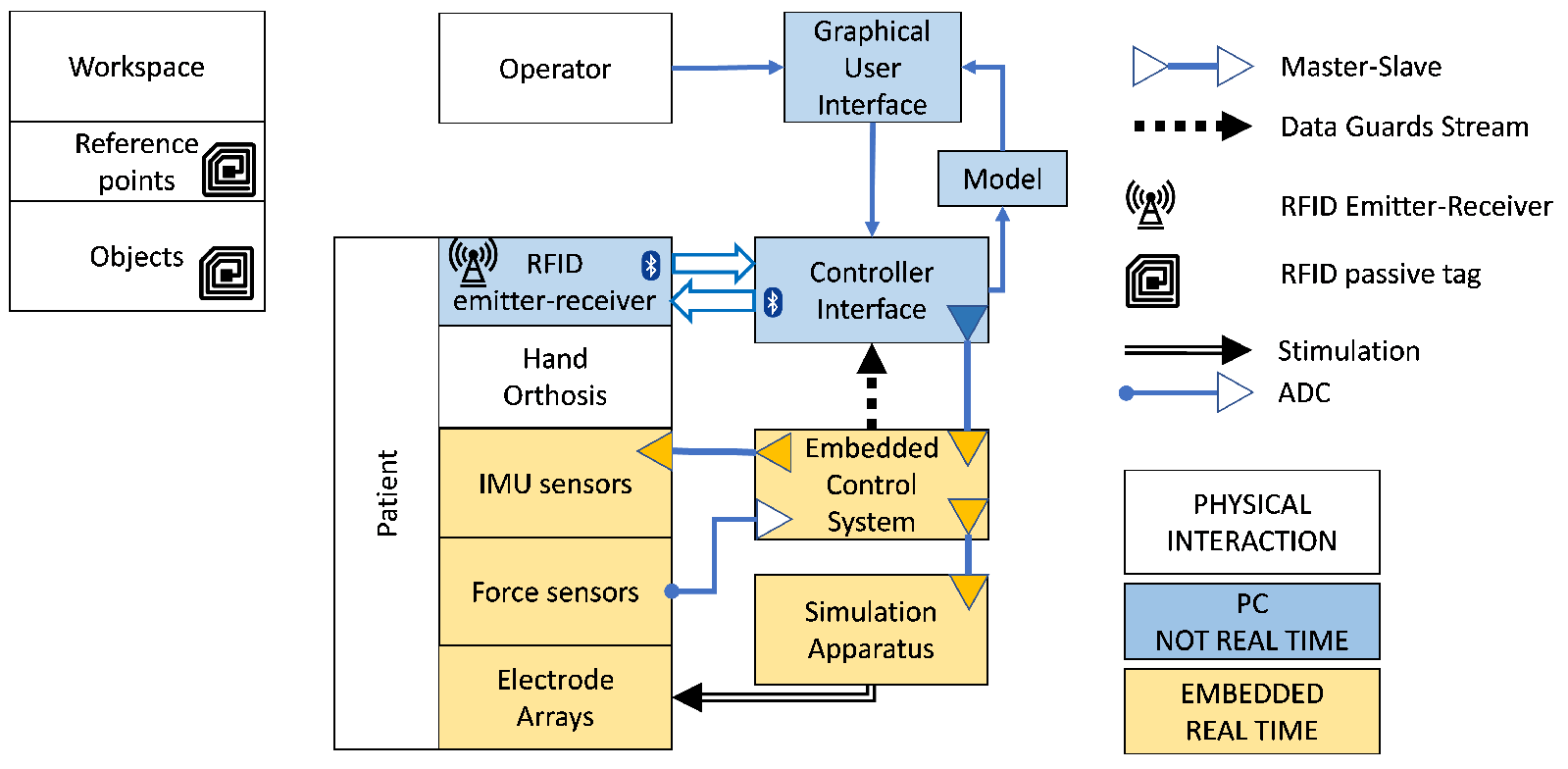
2.2. Technological Implementation
2.2.1. Wearable for NMES and Object Interactivity
2.2.2. Orthoses and Sensorized Components
2.2.3. NMES Controller
2.2.4. Stimulation Apparatus
2.2.5. RFID System for Environmental Interactivity
2.2.6. Control Interface and Embedded Control System
2.2.7. Description of a Training Session
2.3. Clinical Test on Sub-Acute Stroke Patient
2.3.1. Inclusion Criteria
2.3.2. Description of Exercises
2.3.3. Treatment Structure
2.3.4. Clinical Outcome Assessment
2.3.5. Usability Assessment
3. Results
3.1. ARAT Score
3.2. SUS and TAM Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| API | Application Programming Interface |
| ARAT | Action Research Arm Test |
| CI | Control Interface |
| GUI | Graphical User Interface |
| EA | Electrode Array |
| ECS | Embedded Control System |
| IMU | Inertial Measurement Units |
| MCID | minimal clinically important difference |
| MI | Motricity Index |
| MMSE | MiniMental State Examination |
| NMES | NeuroMuscular Electrical Stimulation |
| RCT | Randomised Clinical Trial |
| RSSI | Received Signal Strength Indicator |
| SUS | System Usability Scale |
| TAM | Technology Acceptance Model |
| UID | Unique IDentifier |
| VE | Virtual Electrodes |
References
- Taub, E.; Uswatte, G.; Mark, V.W.; Morris, D.M.M. The learned nonuse phenomenon: Implications for rehabilitation. Eur. Medicophys. 2006, 42, 241–256. [Google Scholar]
- Lemke, M.; Rodríguez Ramírez, E.; Robinson, B. Limited use only. How can the design of an everyday object help chronic stroke patients to overcome the learned nonuse of the upper limb? Des. J. 2017, 20, S2397–S2417. [Google Scholar] [CrossRef]
- Thrasher, T.A.; Zivanovic, V.; McIlroy, W.; Popovic, M.R. Rehabilitation of reaching and grasping function in severe hemiplegic patients using functional electrical stimulation therapy. Neurorehabil. Neural Repair 2008, 22, 706–714. [Google Scholar] [CrossRef]
- Béjot, Y.; Bailly, H.; Durier, J.; Giroud, M. Epidemiology of stroke in Europe and trends for the 21st century. La Presse Médicale 2016, 45, e391–e398. [Google Scholar] [CrossRef]
- Fifi, J.T.; Mocco, J. COVID-19 related stroke in young individuals. Lancet Neurol. 2020, 19, 713–715. [Google Scholar] [CrossRef]
- Qureshi, A.I.; Baskett, W.I.; Huang, W.; Shyu, D.; Myers, D.; Raju, M.; Lobanova, I.; Suri, M.F.K.; Naqvi, S.H.; French, B.R.; et al. Acute Ischemic Stroke and COVID-19. Stroke 2021, 52, 905–912. [Google Scholar] [CrossRef]
- Divani, A.A.; Andalib, S.; Di Napoli, M.; Lattanzi, S.; Hussain, M.S.; Biller, J.; McCullough, L.D.; Azarpazhooh, M.R.; Seletska, A.; Mayer, S.A.; et al. Coronavirus Disease 2019 and Stroke: Clinical Manifestations and Pathophysiological Insights. J. Stroke Cerebrovasc. Dis. 2020, 29, 104941. [Google Scholar] [CrossRef]
- Taquet, M.; Geddes, J.R.; Husain, M.; Luciano, S.; Harrison, P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. Lancet Psychiatry 2021, 8, 416–427. [Google Scholar] [CrossRef]
- Chriki, L.S.; Bullain, S.S.; Stern, T.A. The Recognition and Management of Psychological Reactions to Stroke: A Case Discussion. Prim. Care Companion J. Clin. Psychiatry 2006, 8, 234–240. [Google Scholar] [CrossRef] [Green Version]
- Jellema, S.; van Hees, S.; Zajec, J.; van der Sande, R.; Nijhuis-van der Sanden, M.W.; Steultjens, E.M. What environmental factors influence resumption of valued activities post stroke: A systematic review of qualitative and quantitative findings. Clin. Rehabil. 2016, 31, 936–947. [Google Scholar] [CrossRef]
- Knutson, J.S.; Fu, M.J.; Sheffler, L.R.; Chae, J. Neuromuscular Electrical Stimulation for Motor Restoration in Hemiplegia. Phys. Med. Rehabil. Clin. N. Am. 2015, 26, 729–745. [Google Scholar] [CrossRef] [Green Version]
- Crema, A.; Malesevic, N.; Furfaro, I.; Raschella, F.; Pedrocchi, A.; Micera, S. A Wearable Multi-Site System for NMES-Based Hand Function Restoration. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 428–440. [Google Scholar] [CrossRef]
- Mangold, S.; Schuster, C.; Keller, T.; Zimmermann-Schlatter, A.; Ettlin, T. Motor training of upper extremity with functional electrical stimulation in early stroke rehabilitation. Neurorehabil. Neural Repair 2009, 23, 184–190. [Google Scholar] [CrossRef]
- Takeda, K.; Tanino, G.; Miyasaka, H. Review of devices used in neuromuscular electrical stimulation for stroke rehabilitation. Med. Devices (Auckl.) 2017, 10, 207–213. [Google Scholar] [CrossRef] [Green Version]
- Pedrocchi, A.; Ferrante, S.; Ambrosini, E.; Gandolla, M.; Casellato, C.; Schauer, T.; Klauer, C.; Pascual, J.; Vidaurre, C.; Gföhler, M.; et al. MUNDUS project: MUltimodal Neuroprosthesis for daily Upper limb Support. J. Neuroeng. Rehabil. 2013, 10, 66. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.Y.; Lin, G.H.; Huang, Y.J.; Song, C.Y.; Lee, Y.C.; How, M.J.; Chen, Y.M.; Hsueh, I.P.; Chen, M.H.; Hsieh, C.L. Improving the utility of the Brunnstrom recovery stages in patients with stroke. Medicine 2016, 95. [Google Scholar] [CrossRef]
- Todorov, E. Optimality principles in sensorimotor control. Nat. Neurosci. 2004, 7, 907–915. [Google Scholar] [CrossRef] [Green Version]
- Valtin, M.; Kociemba, K.; Behling, C.; Kuberski, B.; Becker, S.; Schauer, T. RehaMovePro: A Versatile Mobile Stimulation System for Transcutaneous FES Applications. Eur. J. Transl. Myol. 2016, 26, 6076. [Google Scholar] [CrossRef]
- Bohannon, R.W. Motricity Index Scores are Valid Indicators of Paretic Upper Extremity Strength Following Stroke. J. Phys. Ther. Sci. 1999, 11, 59–61. [Google Scholar] [CrossRef] [Green Version]
- Ciesla, N.; Dinglas, V.; Fan, E.; Kho, M.; Kuramoto, J.; Needham, D. Manual muscle testing: A method of measuring extremity muscle strength applied to critically ill patients. J. Vis. Exp. 2011, 2632. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Kang, M.; Ragan, B.G.; Park, J.H. Issues in outcomes research: An overview of randomization techniques for clinical trials. J. Athl. Train. 2008, 43, 215–221. [Google Scholar] [CrossRef] [Green Version]
- Timmermans, A.A.A.; Seelen, H.A.M.; Willmann, R.D.; Kingma, H. Technology-assisted training of arm-hand skills in stroke: Concepts on reacquisition of motor control and therapist guidelines for rehabilitation technology design. J. Neuroeng. Rehabil. 2009, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Jette, A.M. Toward a common language for function, disability, and health. Phys. Ther. 2006, 86, 726–734. [Google Scholar] [CrossRef]
- Hinkle, J.L.; Becker, K.J.; Kim, J.S.; Choi-Kwon, S.; Saban, K.L.; McNair, N.; Mead, G.E.; American Heart Association Council on Cardiovascular and Stroke Nursing and Stroke Council. Poststroke Fatigue: Emerging Evidence and Approaches to Management: A Scientific Statement for Healthcare Professionals From the American Heart Association. Stroke 2017, 48, e159–e170. [Google Scholar] [CrossRef] [Green Version]
- Seabold, S.; Perktold, J. Statsmodels: Econometric and statistical modeling with python. In Proceedings of the 9th Python in Science Conference, Austin, TX, USA, 28 June–3 July 2010; p. 92. [Google Scholar]
- Brooke, J. SUS—A quick and dirty usability scale. In Usability Evaluation in Industry; CRC Press: Boca Raton, FL, USA, 1996; pp. 4–7. [Google Scholar]
- Bangor, A.; Kortum, P.; Miller, J. Determining What Individual SUS Scores Mean: Adding an Adjective Rating Scale. J. Usability Stud. 2009, 4, 114–123. [Google Scholar]
- Holden, R.J.; Karsh, B.T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [Green Version]
- Legris, P.; Ingham, J.; Collerette, P. Why do people use information technology? A critical review of the technology acceptance model. Inf. Manag. 2003, 40, 191–204. [Google Scholar] [CrossRef]
- Lang, C.E.; Edwards, D.F.; Birkenmeier, R.L.; Dromerick, A.W. Estimating minimal clinically important differences of upper-extremity measures early after stroke. Arch. Phys. Med. Rehabil. 2008, 89, 1693–1700. [Google Scholar] [CrossRef] [Green Version]
- Mukaka, M. A guide to appropriate use of Correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]



| Group | Sex | Age (yr) | Days since Stroke | Affected Side | Stroke Type | ARAT T0 |
|---|---|---|---|---|---|---|
| C | M | 59 | 116 | R | I | 14 |
| C | M | 69 | 83 | L | I | 20 |
| C | M | 69 | 35 | L | I | 21 |
| C | M | 54 | 247 | L | H | 2 |
| C | M | 54 | 125 | R | I | 10 |
| E | F | 72 | 112 | R | I | 35 |
| E | M | 73 | 108 | L | I | 9 |
| E | F | 79 | 22 | L | I | 5 |
| E | F | 72 | 15 | L | I | 21 |
| E | F | 73 | 18 | R | H | 18 |
| E | M | 42 | 145 | R | H | 0 |
| Scale | Label | Conv | Exp | Baseline Test | Stat | p-Value |
|---|---|---|---|---|---|---|
| Sample size | 5 | 6 | ||||
| Age | 59 (54:69) | 72.5 (72:73) | SW | 0.8839 | 0.1168 | |
| MW | 5.0 | 0.0400 | ||||
| TT | −1.1165 | 0.2931 | ||||
| Interv. delay | 116 (83:125) | 65 (19:111) | SW | 0.8951 | 0.1607 | |
| MW | 8.0 | 0.1177 | ||||
| TT | 1.2433 | 0.2451 | ||||
| Affected side | L / R | 3/2 | 4/3 | F | 0.75 | 1 |
| ARAT Total | T0 | 14 (10:20) | 13.5 (6:20.25) | SW | 0.9513 | 0.6616 |
| MW | 14.5 | 0.5 | ||||
| T1 | 19 (14:27) | 36 (18.5:52) | ||||
| T2 | 35 (11:41) | 42.5 (19.5:49.75) |
| Scale | Model Comparison | F | p | Group C Coeff | p | Group R Coeff | p | Global Recovery Coeff | p | Significance Model | C | R | Global | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ARAT Total | 0.746 | 11.74 | 0.0042 | 1.77 | 0.7909 | 14.94 | 0.0494 | 1.39 | 0.0028 | ** | * | ** | ||
| 0.656 | 7.626 | 0.0140 | 8.71 | 0.2746 | 14.11 | 0.0943 | 1.42 | 0.0054 | * | + | ** | |||
| 0.856 | 23.69 | 0.0004 | 7.77 | 0.1310 | 0.32 | 0.9592 | 0.98 | 0.0002 | ** | *** | ||||
| ARAT Pinch | 0.310 | 1.801 | 0.2261 | 2.97 | 0.3636 | 8.68 | 0.0262 | 0.52 | 0.3618 | * | ||||
| 0.133 | 0.6122 | 0.5660 | 5.92 | 0.0995 | 7.09 | 0.0637 | 0.55 | 0.3507 | + | + | ||||
| 0.601 | 6.027 | 0.0253 | 3.78 | 0.1317 | 0.62 | 0.8452 | 0.79 | 0.0094 | * | ** | ||||
| ARAT Grasp | 0.738 | 11.28 | 0.0047 | 1.25 | 0.5188 | 4.15 | 0.0898 | 1.15 | 0.0037 | ** | + | ** | ||
| 0.472 | 3.572 | 0.0779 | 3.87 | 0.2730 | 3.23 | 0.4194 | 1.31 | 0.0309 | + | * | ||||
| 0.882 | 30.02 | 0.0002 | 1.62 | 0.3363 | −3.11 | 0.1863 | 1.29 | <0.0001 | *** | *** | ||||
| ARAT Grip | 0.513 | 4.222 | 0.0560 | 2.38 | 0.2616 | 4.32 | 0.0371 | 1.12 | 0.0222 | + | * | * | ||
| 0.404 | 2.717 | 0.126 | 2.52 | 0.3713 | 4.93 | 0.067 | 1.20 | 0.0557 | + | + | ||||
| 0.758 | 12.56 | 0.0034 | 0.06 | 0.9742 | 0.42 | 0.8354 | 1.05 | 0.0012 | ** | ** | ||||
| ARAT GrossM | 0.545 | 4.786 | 0.0431 | 0.93 | 0.6116 | 4.29 | 0.0093 | 0.85 | 0.0258 | * | ** | * | ||
| 0.472 | 3.581 | 0.0775 | 2.92 | 0.0784 | 5.37 | 0.0008 | 0.60 | 0.0481 | + | + | *** | * | ||
| 0.858 | 24.19 | 0.0004 | 2.26 | 0.0098 | 2.34 | 0.0222 | 0.71 | 0.0002 | *** | ** | * | *** |
| Measure | Median | IQR | Correlations SUS | TAM Usefulness | TAM Ease | TAM External Control | TAM Enjoyment | ARAT Total T0 |
|---|---|---|---|---|---|---|---|---|
| SUS | 55% | (52.5%:72.5%) | ∖ | // | // | // | // | // |
| TAM Usefulness | 50% | (21.25%:67.5%) | ∖ | = −0.8117 | = 0.8872 | = 0.9209 | ||
| p = 0.0498 | p = 0.0183 | p = 0.0091 | ||||||
| TAM Ease | 69% | (59.5%:78/5%) | ∖ | // | = −0.8878 | = −0.8744 | ||
| p = 0.0182 | p = 0.0227 | |||||||
| TAM ExternalControl | 35.5% | (14%:57%) | ∖ | = 0.7991 | ||||
| p = 0.0564 | ||||||||
| TAM Enjoyment | 78.5% | (28.5%:86%) | ∖ | = 0.8202 | ||||
| p = 0.0456 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crema, A.; Furfaro, I.; Raschellà, F.; Rossini, M.; Zajc, J.; Wiesener, C.; Baccinelli, W.; Proserpio, D.; Augsten, A.; Immick, N.; et al. Reactive Exercises with Interactive Objects: Interim Analysis of a Randomized Trial on Task-Driven NMES Grasp Rehabilitation for Subacute and Early Chronic Stroke Patients. Sensors 2021, 21, 6739. https://doi.org/10.3390/s21206739
Crema A, Furfaro I, Raschellà F, Rossini M, Zajc J, Wiesener C, Baccinelli W, Proserpio D, Augsten A, Immick N, et al. Reactive Exercises with Interactive Objects: Interim Analysis of a Randomized Trial on Task-Driven NMES Grasp Rehabilitation for Subacute and Early Chronic Stroke Patients. Sensors. 2021; 21(20):6739. https://doi.org/10.3390/s21206739
Chicago/Turabian StyleCrema, Andrea, Ivan Furfaro, Flavio Raschellà, Mauro Rossini, Johannes Zajc, Constantin Wiesener, Walter Baccinelli, Davide Proserpio, Andreas Augsten, Nancy Immick, and et al. 2021. "Reactive Exercises with Interactive Objects: Interim Analysis of a Randomized Trial on Task-Driven NMES Grasp Rehabilitation for Subacute and Early Chronic Stroke Patients" Sensors 21, no. 20: 6739. https://doi.org/10.3390/s21206739
APA StyleCrema, A., Furfaro, I., Raschellà, F., Rossini, M., Zajc, J., Wiesener, C., Baccinelli, W., Proserpio, D., Augsten, A., Immick, N., Becker, S., Weber, M., Schauer, T., Krakow, K., Gasperini, G., Molteni, F., Russold, M. F., Bulgheroni, M., & Micera, S. (2021). Reactive Exercises with Interactive Objects: Interim Analysis of a Randomized Trial on Task-Driven NMES Grasp Rehabilitation for Subacute and Early Chronic Stroke Patients. Sensors, 21(20), 6739. https://doi.org/10.3390/s21206739







