Measuring Spatiotemporal Parameters on Treadmill Walking Using Wearable Inertial System
Abstract
:1. Introduction
2. Methods
2.1. Instrumentation
2.1.1. The OptogaitTM
2.1.2. The Xsens
- The Inverted Pendulum Model
- 2.
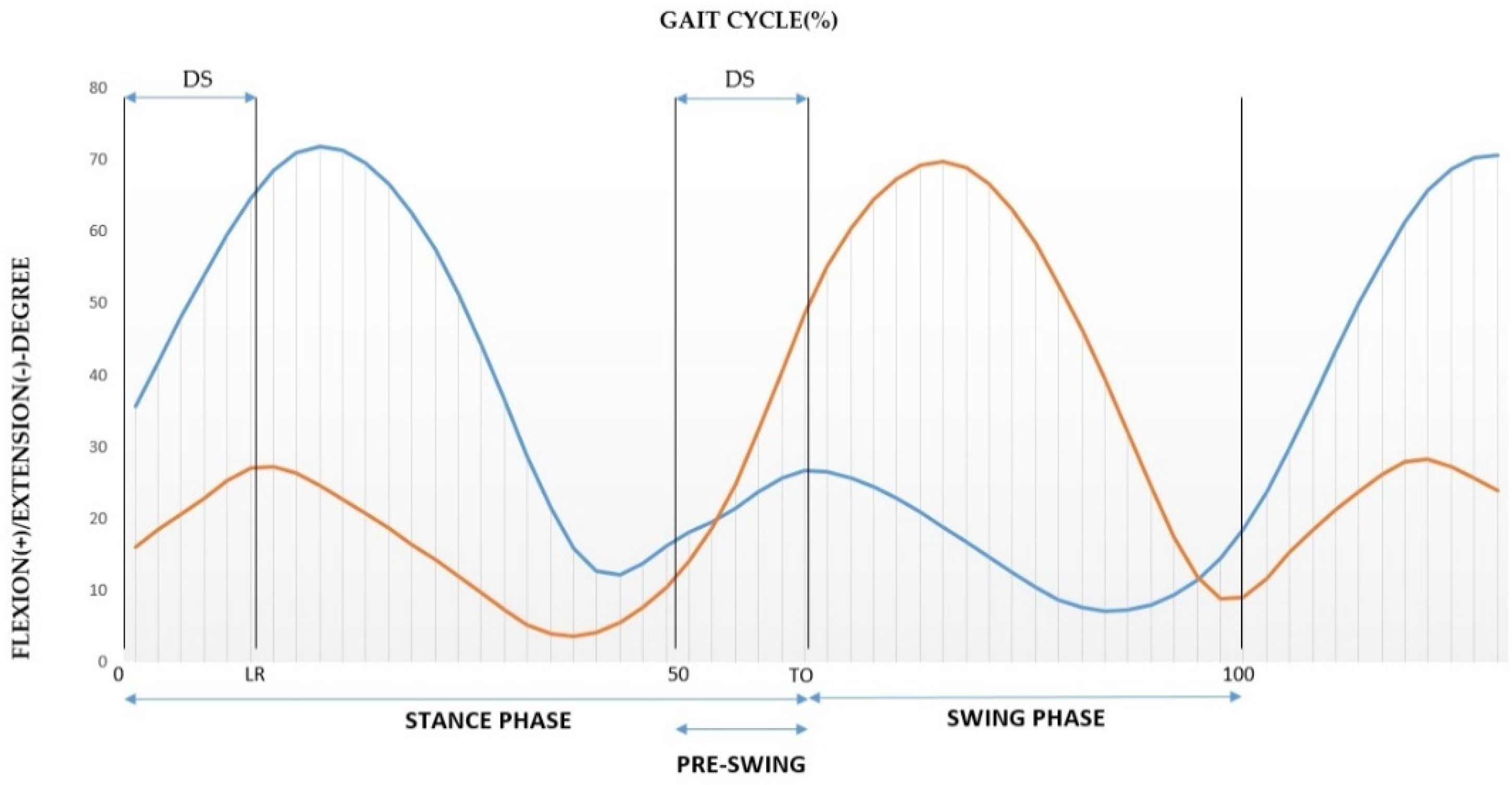
- Identification of Gait Phases and Sub-phases
2.1.3. The Anthropometric Approach
2.2. Statistical Analysis
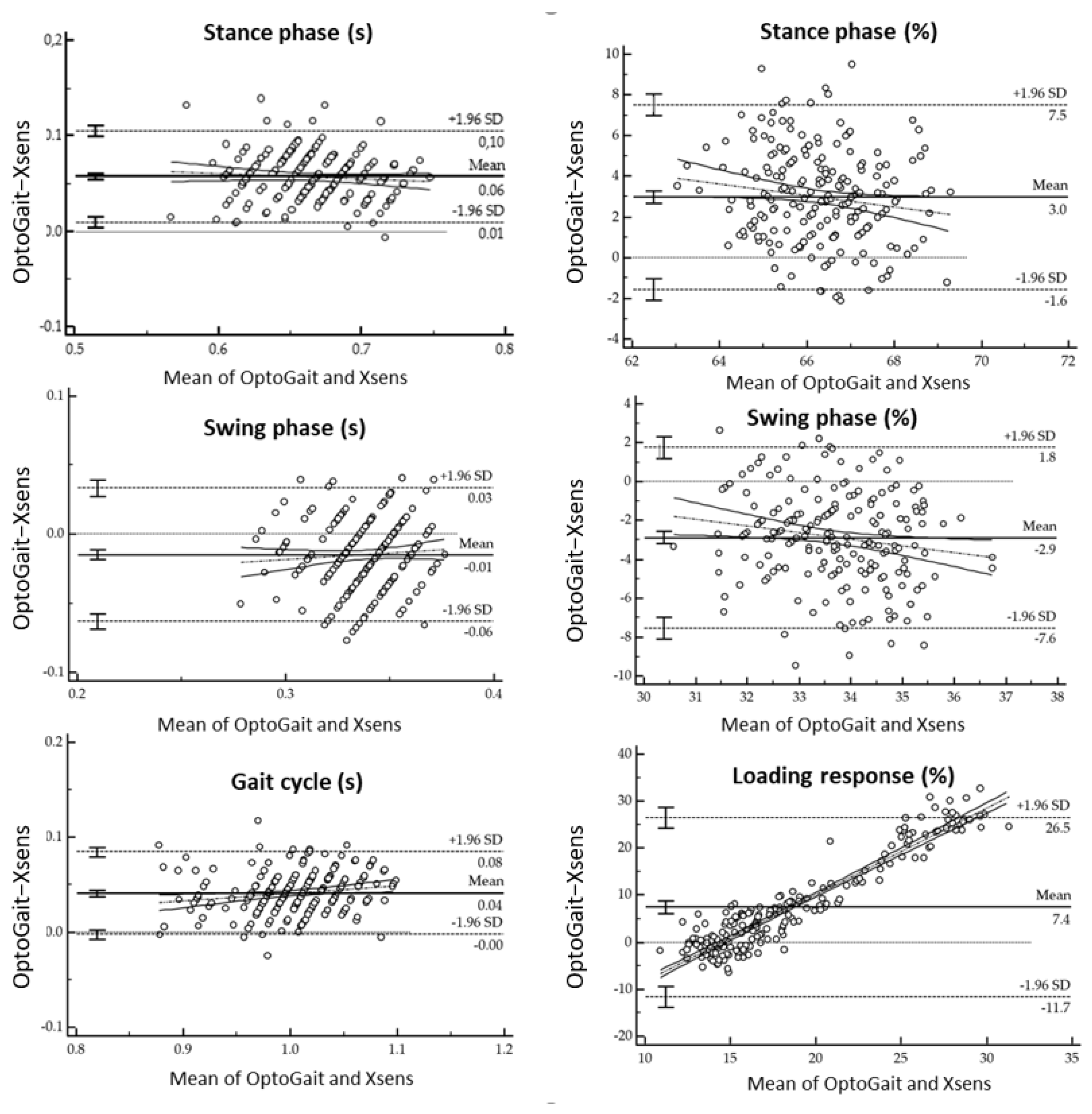
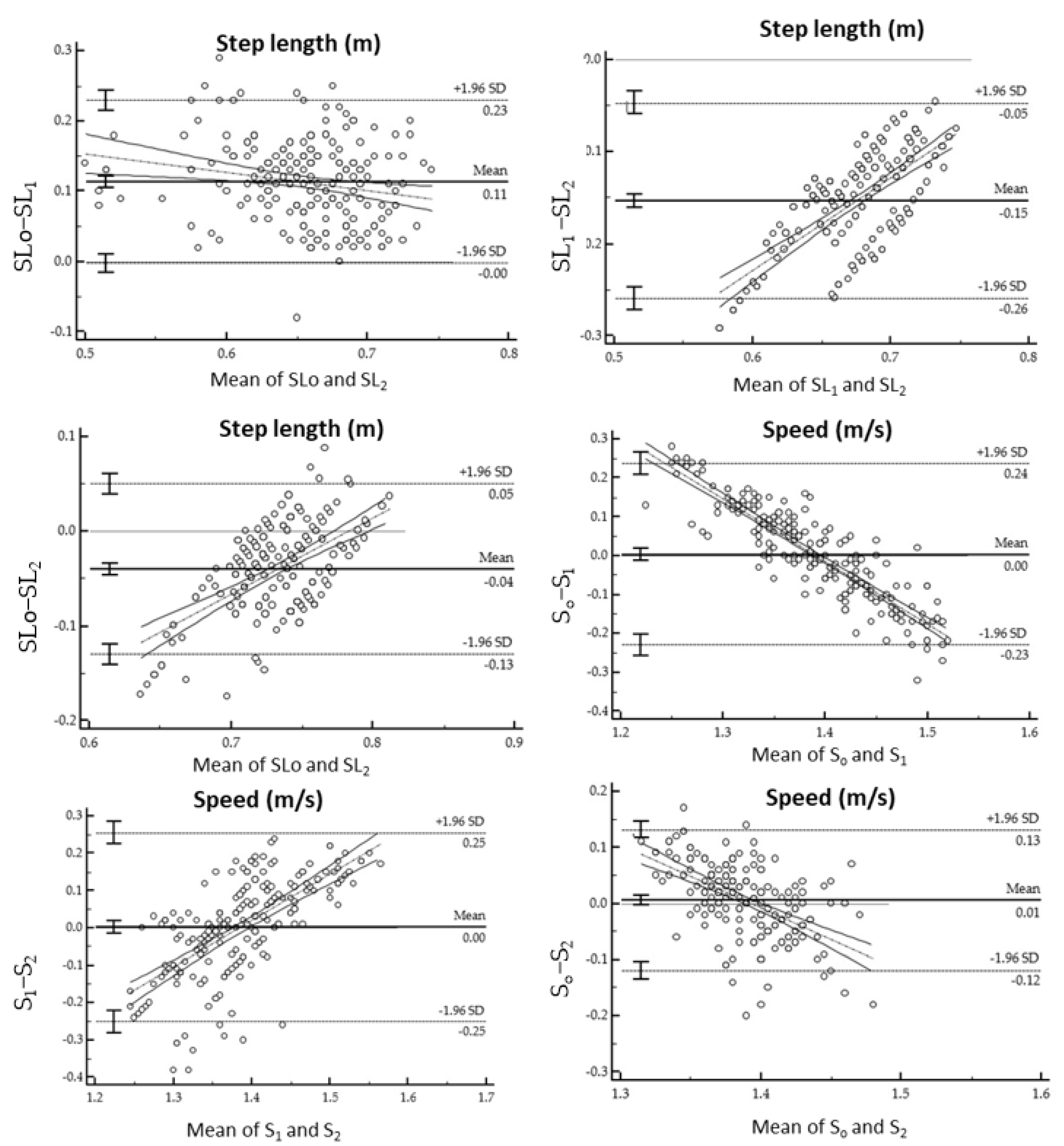
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SPT | spatiotemporal parameters |
| IMU | inertial measurement unit |
| IGA | instrumented gait analysis |
| SD | standard deviation |
| COM | center of mass |
| DS | double support |
| Min | minimum |
| Max | maximum |
| ICC | intraclass correlation coefficients |
| ICC_A | intraclass correlation coefficients reflect absolute agreement |
| ICC_C | intraclass correlation coefficients reflect consistency |
| MAD | mean absolute deviation |
| MSE | mean square error |
| CI | confidence interval |
References
- Caldas, R.; Mundt, M.; Potthast, W.; de Lima Neto, F.B.; Markert, B. A systematic review of gait analysis methods based on inertial sensors and adaptive algorithms. Gait Posture 2017, 57, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Legrain, F. Le Locomètre®: Analyse des Paramètres Spatio-Temporels de la Marche. Ph.D. Thesis, Université Lille 2, Lile, France, 2012. [Google Scholar]
- Najafi, S.; Rezasoltani, Z.; Abedi, M. Effects of Mechanical Low Back Pain in Spatiotemporal Parameters of Gait. J. Arch. Mil. Med. 2019, 6, e82816. [Google Scholar] [CrossRef] [Green Version]
- Mobbs, R.J. Gait velocity (walking speed) is an indicator of spine health, and objective measure of pre and post intervention recovery for spine care providers. J. Spine Surg. 2020, 6, 353–355. [Google Scholar] [CrossRef] [PubMed]
- Abid, M.; Mezghani, N.; Mitiche, A. Knee Joint Biomechanical Gait Data Classification for Knee Pathology Assessment: A Literature Review. Appl. Bionics Biomech. 2019, 2019, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Amir Rashedi Bonab, M.; Kuru Colak, T.; Toktas, Z.O.; Konya, D. Assessment of spatiotemporal gait parameters in patients with lumbar disc herniation and patients with chronic mechanical low back pain. Turk. Neurosurg. 2019, 3, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Soulard, J.; Vaillant, J.; Balaguier, R.; Baillet, A.; Gaudin, P.; Vuillerme, N. Foot-Worn Inertial Sensors Are Reliable to Assess Spatiotemporal Gait Parameters in Axial Spondyloarthritis under Single and Dual Task Walking in Axial Spondyloarthritis. Sensors 2020, 20, 6453. [Google Scholar] [CrossRef]
- Sprager, S.; Juric, M. Inertial Sensor-Based Gait Recognition: A Review. Sensors 2015, 15, 22089–22127. [Google Scholar] [CrossRef]
- Whittle, M.W. Applications of Gait Analysis. Gait Anal. 1991, 174–200. [Google Scholar]
- Lohman, E.B.; Balan Sackiriyas, K.S.; Swen, R.W. A comparison of the spatiotemporal parameters, kinematics, and biomechanics between shod, unshod, and minimally supported running as compared to walking. Phys. Ther. Sport 2011, 12, 151–163. [Google Scholar] [CrossRef]
- Muro-de-la-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait Analysis Methods: An Overview of Wearable and Non-Wearable Systems, Highlighting Clinical Applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef] [Green Version]
- Pradhan, A.; Oladi, S.; Kuruganti, U.; Chester, V. Classification of Elderly Fallers and Non-fallers Using Force Plate Parameters from Gait and Balance Tasks. Comput. Methods Imaging Vis. Biomech. Biomed. Eng. 2020, 36, 339–353. [Google Scholar]
- Colyer, S.L.; Evans, M.; Cosker, D.P.; Salo, A.I.T. A Review of the Evolution of Vision-Based Motion Analysis and the Integration of Advanced Computer Vision Methods Towards Developing a Markerless System. Sports Med. Open 2018, 4, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carbajales-Lopez, J.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Casado-Hernández, I.; Benito-De Pedro, M.; Rodríguez-Sanz, D.; Calvo-Lobo, C.; San Antolín, M. The OptoGait Motion Analysis System for Clinical Assessment of 2D Spatiotemporal Gait Parameters in Young Adults: A Reliability and Repeatability Observational Study. Appl. Sci. 2020, 10, 3726. [Google Scholar] [CrossRef]
- Medda, A.; Vaughan, A.; Liu, B.; Phelps, S. Activity recognition using statistical gait parameters from a single accelerometer. In Proceedings of the 48th Asilomar Conference on Signals, Systems and Computers, Pacific Grove, CA, USA, 2–5 November 2014; pp. 189–193. [Google Scholar]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward Pervasive Gait Analysis with Wearable Sensors: A Systematic Review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef]
- Teufl, W.; Lorenz, M.; Miezal, M.; Taetz, B.; Fröhlich, M.; Bleser, G. Towards Inertial Sensor Based Mobile Gait Analysis: Event-Detection and Spatiotemporal Parameters. Sensors 2018, 19, 38. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Sun, Y.; Li, Q.; Liu, T. Estimation of Step Length and Gait Asymmetry Using Wearable Inertial Sensors. IEEE Sens. J. 2018, 18, 3844–3851. [Google Scholar] [CrossRef]
- Martini, E.; Fiumalbi, T.; Dell’Agnello, F.; Ivanić, Z.; Munih, M.; Vitiello, N.; Crea, S. Pressure-Sensitive Insoles for Real-Time Gait-Related Applications. Sensors 2020, 20, 1448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scataglini, S.; Abran, G.; Roosens, E.; van Tiggelen, D.; Haelterman, R.; Verwulgen, S. Smart clothing for monitoring gait. In Proceedings of the 6th International Digital Human Modeling Symposium, DHM2020, Skovde, Sweden, 31 August–2 September 2020; Hanson, L., Högberg, D., Brolin, E., Eds.; IOS Press: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Scataglini, S.; Abran, G.; Roosens, E.; van Tiggelen, D.; Haelterman, R.; Verwulgen, S. Evaluation of Golden Gait Approximation Using Smart Clothing. Adv. Intell. Syst. Comput. 2020, 1206, 275–282. [Google Scholar]
- Scataglini, S.; Moorhead, A.P.; Feletti, F. A systematic review of smart clothing in sports: Possible application to Extreme sports. Muscle Ligaments Tendons J. 2020, 10, 333. [Google Scholar] [CrossRef]
- Mariani, B.; Hoskovec, C.; Rochat, S.; Büla, C.; Penders, J.; Aminian, K. 3D gait assessment in young and elderly subjects using foot−worn inertial sensors. J. Biomech. 2010, 43, 2999–3006. [Google Scholar] [CrossRef]
- Sabatini, A.; Mannini, A. Ambulatory Assessment of Instantaneous Velocity during Walking Using Inertial Sensor Measurements. Sensors 2016, 16, 2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugiarto, T.; Lin, Y.J.; Chang, C.C.; Hsu, W.C. Gait analysis based on an inertial measurement unit sensor: Validation of spatiotemporal parameters calculation in healthy young and older adults. In Proceedings of the IEEE/SICE International Symposium on System Integration (SII), Tapei, Taiwan, 11–14 December 2017. [Google Scholar]
- Gomez Bernal, A.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E. Reliability of the OptoGait portable photoelectric cell system for the quantification of spatial-temporal parameters of gait in young adults. Gait Posture 2016, 50, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Lienhard, K.; Schneider, D.; Maffiuletti, N.A. Validity of the OptoGait photoelectric system for the assessment of spatiotemporal gait parameters. Med. Eng. Phys. 2013, 35, 500–504. [Google Scholar] [CrossRef]
- Laurens, J.; Awai, L.; Bockisch, C.J.; Hegemann, S.; van Hedel, H.J.A.; Dietz, V.; Straumann, D. Visual contribution to postural stability: Interaction between target fixation or tracking and static or dynamic large-field stimulus. Gait Posture 2010, 31, 37–41. [Google Scholar] [CrossRef] [Green Version]
- Rudisch, J.; Jöllenbeck, T.; Vogt, L.; Cordes, T.; Klotzbier, T.J.; Vogel, O.; Wollesen, B. Agreement and consistency of five different clinical gait analysis systems in the assessment of spatiotemporal gait parameters. Gait Posture 2021, 85, 55–64. [Google Scholar] [CrossRef]
- Kluge, F.; Gaßner, H.; Hannink, J.; Pasluosta, C.; Klucken, J.; Eskofier, B.M. Towards Mobile Gait Analysis: Concurrent Validity and Test-Retest Reliability of an Inertial Measurement System for the Assessment of Spatiotemporal Gait Parameters. Sensors 2017, 17, 1522. [Google Scholar] [CrossRef]
- Washabaugh, E.P.; Kalyanaraman, T.; Adamczyk, P.G.; Claflin, E.S.; Krishnan, C. Validity and repeatability of inertial measurement units for measuring gait parameters. Gait Posture 2017, 55, 87–93. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.M.; Song, C.H.; Lee, K.J.; Jung, S.W.; Shin, D.C.; Shin, S.H. Concurrent Validity and Test−Retest Reliability of the OPTOGait Photoelectric Cell System for the Assessment of Spatiotemporal Parameters of the Gait of Young Adults. J. Phys. Ther. Sci. 2014, 26, 81–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hindle, B.R.; Keogh, J.W.L.; Lorimer, A.V. Inertial-Based Human Motion Capture: A Technical Summary of Current Processing Methodologies for Spatiotemporal and Kinematic Measures. Appl. Bionics Biomech. 2021, 2021, 6628320. [Google Scholar] [CrossRef] [PubMed]
- Najafi, B.; Khan, T.; Wrobel, J. Laboratory in a box: Wearable sensors and its advantages for gait analysis. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011. [Google Scholar]
- Routhier, F.; Duclos, N.C.; Lacroix, É.; Lettre, J.; Turcotte, E.; Hamel, N.; Michaud, F.; Duclos, C.; Philippe, S.; Archambault, F.S.; et al. Clinicians’ perspectives on inertial measurement units in clinical practice. PLoS ONE 2020, 15, e0241922. [Google Scholar] [CrossRef]
- Park, S.; Jayaraman, S. Wearable Sensor Systems: Opportunities and Challenges. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 1–4 September 2005. [Google Scholar]
- Díaz, S.; Stephenson, J.B.; Labrador, M.A. Use of Wearable Sensor Technology in Gait, Balance, and Range of Motion Analysis. Appl. Sci. 2020, 10, 234. [Google Scholar] [CrossRef] [Green Version]
- Lopez, X.; Afrin, K.; Nepal, B. Examining the design, manufacturing and analytics of smart wearables. Med. Devices Sens. 2020, 3. [Google Scholar] [CrossRef]
- Fusca, M.; Perego, P.; Andreoni, G. Method for Wearable Kinematic Gait Analysis Using a Harmonic Oscillator Applied to the Center of Mass. J. Sens. 2018, 2018, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Iosa, M.; Morone, G.; Paolucci, S. Golden Gait: An Optimization Theory Perspective on Human and Humanoid Walking. Front. Neurorob. 2017, 11, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogin, B.; Varela-Silva, M.I. Leg Length, Body Proportion, and Health: A Review with a Note on Beauty. Int. J. Environ. Res. Public Health 2010, 7, 1047–1075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Carrington, E. PT Exam Review—The essential guide for the foreign-trained physical therapist. Physiotherapy 1996, 82, 278. [Google Scholar] [CrossRef]
- Giavarina, D. Understanding Bland Altman analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar] [CrossRef] [Green Version]
- Barnhart, H.X.; Barborial, D.P. Applications of the repeatability of quantitative imaging biomarkers: A review of statistical analysis of repeat data sets. Transl. Oncol. 2009, 2, 231–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bland, J.M.; Altman, D.G. Statistical method for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Comparing methods of measurement: Why plotting difference against standard method is misleading. Lancet 1995, 346, 1085–1087. [Google Scholar] [CrossRef] [Green Version]
- Doğan, N.Ö. Bland-Altman analysis: A paradigm to understand correlation and agreement. Turk. J. Emerg. Med. 2018, 18, 139–141. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.W.; Goldsmith, C.H. Use of the Standard Error as a Reliability Index of Interest: An Applied Example Using Elbow Flexor Strength Data. Phys. Ther. 1997, 77, 745–750. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rose, J.; Gamble, J.C. Human Walking, 3rd ed.; Wolters Kluwer: Philadelphia, PA, USA, 2015. [Google Scholar]
- Liu, J.; Tang, W.; Chen, G.; Lu, Y.; Feng, C.; Tu, X.M. Correlation and agreement: Overview and clarification of competing concepts and measures. Shanghai Arch. Psychiatry 2016, 28, 115–120. [Google Scholar]
- Donath, L.; Faude, O.; Lichtenstein, E.; Nüesch, C.; Mündermann, A. Validity and reliability of a portable gait analysis system for measuring spatiotemporal gait characteristics: Comparison to an instrumented treadmill. J. Neuroeng. Rehabil. 2016, 13, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.; Song, C.; Lee, K.; Shin, D.; Shin, S. Agreement between the spatio−temporal gait parameters from treadmill−based photoelectric cell and the instrumented treadmill system in healthy young adults and stroke patients. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2014, 20, 1210–1219. [Google Scholar]
- Zhou, L.; Tunca, C.; Fischer, E.; Brahms, C.M.; Ersoy, C.; Granacher, U.; Arnrich, B. Validation of an IMU Gait Analysis Algorithm for Gait Monitoring in Daily Life Situations. In Proceedings of the 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020. [Google Scholar]
- Jaén-Carrillo, D.; García-Pinillos, F.; Cartón-Llorente, A.; Almenar-Arasanz, A.J.; Bustillo-Pelayo, J.A.; Roche-Seruendo, L.E. Test-Retest reliability of the OptoGait system for the analysis of spatiotemporal running gait parameters and lower body stiffness in healthy adults. Proc. Inst. Mech. Eng. Part P J. Sports Eng. Technol. 2020, 234, 154–161. [Google Scholar] [CrossRef]
- Marmelat, V.; Duncan, A.; Meltz, S. Effect of sampling frequency on fractal fluctuations during treadmill walking. PLoS ONE 2019, 14, e0218908. [Google Scholar] [CrossRef] [Green Version]
- Murray, M.P.; Drought, A.B.; Kory, R.C. Walking patterns of normal men. J. Bone Jt. Surg. 1964, 46, 335–360. [Google Scholar] [CrossRef]
- Ng, S.S.M.; Tse, M.M.Y.; Kwong, P.W.H.; Fong, I.C.K.; Chan, S.H.; Cheung, T.C.H.; Lai, K.H.M.; David, M.H.; Cynthia, Y.Y. Reliability of the Maximal Step Length Test and Its Correlation with Motor Function in Chronic Stroke Survivors. BioMed. Res. Int. 2018, 2018, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scataglini, S.; Paul, G. Digital Human Modelling and Posturography; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Scataglini, S.; Danckaers, F.; Haelterman, R.; Huysmans, T.; Sijbers, J. Moving Statistical Body Shape Models Using Blender. In Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018), Florence, Italy, 26–30 August 2018; pp. 28–38. [Google Scholar]
- Scataglini, S.; Danckaers, F.; Huysmans, T.; Sijbers, J.; Andreoni, G. Design smart clothing using digital human models. In DHM and Posturography; Scataglini, S., Paul, G., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 683–698. [Google Scholar]
- Paul, G.; Scataglini, S. (Eds.) Open-source software to create a kinematic model in digital human modeling. In DHM and Posturography; Elsevier: Amsterdam, The Netherlands, 2019; pp. 201–213. [Google Scholar]
- Rasmussen, J. The AnyBody Modeling System. In DHM and Posturography; Scataglini, S., Paul, G., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 85–96. [Google Scholar]



| Mean (SD) | |
|---|---|
| Age (years) | 25.42 (5.83) |
| Stature (m) | 1.81 (0.06) |
| Body mass (kg) | 74.92 (7.40) |
| BMI (kg/m2) | 22.80 (1.36) |
| Leg length (m) | 0.94 (0.05) |
| SPT | Mean (SD) OptoGaitTM | Mean (SD)Xsens | Mean Diff | 95% CI | p | ICC_A Mean | 95% CI | ICC_C Mean | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| Stance phase (s) | 0.69 (0.002) | 0.63 (0.002) | 0.056 | 0.053 to 0.0602 | <0.0001 | 0.512 | −0.153 to 0.819 | 0.87 | 0.829 to 0.901 |
| Swing phase (s) | 0.33 (0.001) | 0.34 (0.001) | −0.014 | −0.018 to −0.011 | <0.0001 | 0.527 | 0.236 to 0.691 | 0.60 | 0.479 to 0.697 |
| Stance phase (%) | 67.80 (0.107) | 64.83 (0.124) | 2.971 | 2.655 to 3.287 | <0.0001 | 0.026 | −0.082 to 0.140 | 0.06 | −0.224 to 0.289 |
| Swing phase (%) | 32.27 (0.104) | 35.16 (0.124) | −2.888 | −3.213 to −2.564 | <0.0001 | −0.028 | −0.147 to 0.094 | −0.074 | −0.041 to 0.189 |
| Gait cycle (s) | 1.02 (0.003) | 0.98 (0.003) | 0.041 | 0.038 to 0.044 | <0.0001 | 0.796 | −0.167 to 0.940 | 0.945 | 0.928 to 0.958 |
| Double support (%) | 35.53 (0.171) | 29.64 (0.188) | 5.884 | 5.391 to 6.378 | <0.0001 | 0.016 | −0.061 to 0.101 | 0.056 | −0.023 to 0.241 |
| Time of Double support (s) | 0.36 (0.002) | 0.29 (0.002) | 0.072 | 0.067 to 0.077 | <0.0001 | 0.149 | −0.123 to 0.403 | 0.461 | 0.293 to 0.590 |
| Loading response (%) | 22.27 (0.673) | 14.85 (0.115) | 7.423 | 6.093 to 8.752 | <0.0001 | 0.028 | −0.014 to 0.193 | 0.044 | −0.254 to 0.272 |
| Time of loading response (s) | 0.15 (0.004) | 0.14 (0.001) | 0.008 | −0.0005 to 0.017 | 0.0660 | 0.137 | −0.129 to 0.341 | 0.138 | −0.131 to 0.343 |
| Pre−swing (%) | 17.80 (0.114) | 16.11 (0.321) | 1.686 | 0.995 to 2.377 | <0.0001 | −0.122 | −0.433 to 0.125 | −0.137 | −0.491 to 0.133 |
| Time of pre−swing (s) | 0.18 (0.001) | 0.14 (0.001) | 0.036 | 0.033 to 0.039 | <0.0001 | 0.138 | −0.118 to 0.362 | 0.362 | 0.162 to 0.514 |
| Cadence (step/min) | 117.50 (0.410) | 122.39 (0.416) | −4.888 | −5.256 to −4.520 | <0.0001 | 0.804 | −0.164 to 0.942 | 0.946 | 0.925 to 0.959 |
| SPT (O-X) | Parameter | Coefficient | SE | t | p | 95% CI | CR | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Stance phase (s) | Intercept | 0.096 | 0.033 | 2.900 | 0.0041 | 0.030 to 0.162 | 0.121 | 0.110 to 0.134 |
| Slope | −0.059 | 0.049 | −1.192 | 0.2346 | −0.157 to 0.038 | |||
| Swing phase (s) | Intercept | −0.046 | 0.029 | −1.569 | 0.1182 | −0.104 to 0.011 | 0.056 | 0.0514 to 0.0623 |
| Slope | 0.093 | 0.087 | 1.065 | 0.2878 | −0.079 to 0.265 | |||
| Stance phase (%) | Intercept | 21.820 | 8.805 | 2.478 | 0.0140 | 4.461 to 39.180 | 7.378 | 6.733 to 8.160 |
| Slope | −0.284 | 0.132 | −2.141 | 0.0334 | −0.545 to −0.0225 | |||
| Swing phase (%) | Intercept | 8.821 | 4.792 | 1.840 | 0.0671 | −0.627 to 18.269 | 7.327 | 6.687 to 8.104 |
| Slope | −0.347 | 0.142 | −2.444 | 0.0153 | −0.627 to −0.0672 | |||
| Gait Cycle (s) | Intercept | −0.039 | 0.032 | −1.219 | 0.2239 | −0.102 to 0.0242 | 0.091 | 0.083 to 0.101 |
| Slope | 0.080 | 0.032 | 2.496 | 0.0133 | 0.016 to 0.143 | |||
| Double support (s) | Intercept | 0.127 | 0.033 | 3.826 | 0.0002 | 0.061 to 0.193 | 0.158 | 0.144 to 0.175 |
| Slope | −0.168 | 0.101 | −1.666 | 0.0971 | −0.368 to 0.030 | |||
| Double support (%) | Intercept | 11.653 | 4.390 | 2.654 | 0.0086 | 2.997 to 20.308 | 13.531 | 12.349 to 14.966 |
| Slope | −0.177 | 0.134 | −1.316 | 0.1896 | −0.442 to 0.088 | |||
| Pre-swing (s) | Intercept | 0.054 | 0.018 | 2.964 | 0.0034 | 0.018 to 0.089 | 0.0834 | 0.076 to 0.0927 |
| Slope | −0.108 | 0.110 | −0.977 | 0.3295 | −0.326 to 0.110 | |||
| Pre-swing (%) | Intercept | 29.749 | 1.602 | 18.564 | <0.0001 | 26.590 to 32.909 | 10.447 | 9.534 to 11.554 |
| Slope | −1.654 | 0.093 | −17.682 | <0.0001 | −1.839 to −1.470 | |||
| Loading response (%) | Intercept | −26.826 | 0.864 | −31.042 | <0.0001 | −28.529 to −25.122 | 23.984 | 21.889 to 26.527 |
| Slope | 1.844 | 0.044 | 41.031 | <0.0001 | 1.756 to 1.933 | |||
| Cadence (step/min) | Intercept | −2.893 | 3.864 | −0.748 | 0.4549 | −10.512 to 4.725 | 10.935 | 9.980 to 12.095 |
| Slope | −0.016 | 0.032 | −0.516 | 0.6058 | −0.080 to 0.046 |
| SPT | Mean A | Mean B | Mean Diff | 95% CI | p | ICC_A Mean | 95% CI | ICC_C Mean | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| SLo (m), SL1 (m) | 0.71 (0.50) | 0.59 (0.721) | 0.113 | 0.105 to 0.121 | <0.0001 | 0.22 | −0.156 to 0.534 | 0.579 | 0.447 to 0.679 |
| SLo (m), SL2 (m) | 0.71 (0.50) | 0.75 (0.151) | −0.039 | −0.046 to −0.033 | <0.0001 | 0.366 | −0.033 to 0.588 | 0.491 | 0.338 to 0.616 |
| SL1 (m), SL2 (m) | 0.59 (0.721) | 0.75 (0.151) | −0.153 | −0.160 to −0.145 | <0.0001 | 0.088 | −0.075 to 0.140 | 0.463 | 0.295 to 0.591 |
| So (m/s), S1 (m/s) | 1.39 (0.18) | 1.38 (3.701) | 0.003 | −0.012 to 0.020 | 0.6421 | 0.171 | −0.089 to 0.369 | 0.171 | −0.088 to 0.368 |
| So (m/s), S2 (m/s) | 1.39 (0.18) | 1.38 (0.631) | 0.006 | −0.002 to 0.014 | 0.1700 | 0.093 | −0.434 to 0.167 | −0.093 | −0.435 to 0.167 |
| S1 (m/s), S2 (m/s) | 1.38 (3.701) | 1.38 (0.631) | 0.002 | −0.015 to 0.019 | 0.8012 | 0.122 | −0.153 to 0.332 | 0.122 | −0.152 to 0.331 |
| Parameter | Coefficient | SE | t | p | 95% CI | CR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| SLo (m), SL1 (m) | Intercept | 0.282 | 0.058 | 4.863 | <0.0001 | 0.168 to 0.397 | 0.250 | 0.228 to 0.277 |
| Slope | −0.258 | 0.088 | −2.921 | 0.0039 | −0.433 to −0.084 | |||
| SLo (m), SL2 (m) | Intercept | −0.629 | 0.059 | −10.577 | <0.0001 | −0.746 to −0.51 | 0.119 | 0.108 to 0.131 |
| Slope | 0.805 | 0.081 | 9.915 | < 0.0001 | 0.645 to 0.965 | |||
| SL1 (m), SL2 (m) | Intercept | −0.831 | 0.050 | −16.598 | <0.0001 | −0.930 to −0.732 | 0.318 | 0.290 to 0.352 |
| Slope | 1.004 | 0.074 | 13.558 | <0.0001 | 0.858 to 1.150 | |||
| So (m/s), S1 (m/s) | Intercept | 2.252 | 0.080 | 27.974 | <0.0001 | 2.093 to 2.411 | 0.232 | 0.212 to 0.257 |
| Slope | −1.618 | 0.057 | −27.957 | <0.0001 | −1.732 to −1.503 | |||
| S1 (m/s), S2 (m/s) | Intercept | −1.726 | 0.135 | −12.702 | <0.0001 | −1.9943 to −1.458 | 0.252 | 0.230 to 0.278 |
| Slope | 1.246 | 0.097 | 12.734 | <0.0001 | 1.053 to 1.439 | |||
| So (m/s), S2(m/s) | Intercept | −0.629 | 0.059 | −10.577 | <0.0001 | −0.746 to −0.512 | 0.119 | 0.108 to 0.131 |
| Slope | 0.805 | 0.081 | 9.915 | <0.0001 | 0.645 to 0.965 |
| S1 | S2 | SO | |
|---|---|---|---|
| MSE (m/s) | 0.014 | 0.003 | 0.0008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scataglini, S.; Verwulgen, S.; Roosens, E.; Haelterman, R.; Van Tiggelen, D. Measuring Spatiotemporal Parameters on Treadmill Walking Using Wearable Inertial System. Sensors 2021, 21, 4441. https://doi.org/10.3390/s21134441
Scataglini S, Verwulgen S, Roosens E, Haelterman R, Van Tiggelen D. Measuring Spatiotemporal Parameters on Treadmill Walking Using Wearable Inertial System. Sensors. 2021; 21(13):4441. https://doi.org/10.3390/s21134441
Chicago/Turabian StyleScataglini, Sofia, Stijn Verwulgen, Eddy Roosens, Robby Haelterman, and Damien Van Tiggelen. 2021. "Measuring Spatiotemporal Parameters on Treadmill Walking Using Wearable Inertial System" Sensors 21, no. 13: 4441. https://doi.org/10.3390/s21134441
APA StyleScataglini, S., Verwulgen, S., Roosens, E., Haelterman, R., & Van Tiggelen, D. (2021). Measuring Spatiotemporal Parameters on Treadmill Walking Using Wearable Inertial System. Sensors, 21(13), 4441. https://doi.org/10.3390/s21134441






