1. Introduction
Oxygen is a substantial element in the sustenance of human life. Of the hundreds of tasks that oxygen performs in the human body, two stand out for their importance: detoxification and energy production. However, some diseases affect the ability of the lungs to perform the gas exchange necessary to incorporate oxygen into the bloodstream and to release carbon dioxide. In many situations, extra oxygen is needed when the respiratory system cannot maintain an adequate pulmonary exchange of physiological gases. This therapeutic use of supplemental oxygen is defined as oxygen therapy and it aims at increasing the inspired oxygen fraction (FiO
2). Therefore, when medically prescribed, oxygen is a drug. Oxygen therapy is an established treatment, and it continues to be one of the most important measures in the management patients with progressing chronic respiratory disease. In this case, the main objective of oxygen therapy is to improve tissue oxygenation and to correct the severe hypoxemia that these patients usually present with in the advanced stages of the disease [
1,
2]. The goal is to maintain oxygenation levels above the range of respiratory failure, defined by an O
2 blood partial pressure [PaO
2] > 60 mmHg, and an oxygen saturation measured by pulse oximetry [SpO2] > 90%.
Currently, clinical applications for the use of oxygen have extended beyond the hospital setting. When patients receive oxygen supplementation at home, the therapy is referred to as home oxygen therapy (HOT). HOT provided as long-term oxygen therapy (LTOT), that is, used on a daily basis and at least by 15 h per day, is recommended by current treatment guidelines since it has been shown to be effective in increasing survival in patients with chronic obstructive pulmonary disease (COPD) and respiratory failure [
3,
4,
5,
6]. In addition, ambulatory oxygen therapy improves physical performance in patients with COPD [
7].
Despite all these benefits of HOT for patients with respiratory failure, evidence that supports the prescription of HOT in other chronic conditions associated with hypoxemia is limited [
8]. While supplemental oxygen is valuable in clinical situations such as those aforementioned, the inappropriate use of this therapy can be detrimental. Hypoxemia is defined as the decrease in PaO
2 below the normal limits, variable for the subject’s age (normal PaO
2 ranges from 80 to 100 mmHg [
9]). There is evidence that both hypoxemia and hyperoxemia, which results from exposure to excessive O
2 flows for a prolonged period of time, can have serious consequences for patients with acute and chronic respiratory failure [
10,
11]. Although the risks for hypoxemia are well known [
12], there is growing evidence that excessive oxygen flow can be potentially harmful. In this regard, hyperoxemia has been associated with increased hospital mortality among patients admitted to intensive care units (ICUs) following cardiac arrest resuscitation [
13]. In this regard, hyperoxemia may be especially problematic in patients with COPD in the acute phase of exacerbation, because of its association with hypercapnia [
14,
15] and its potential to mask the onset of a worsening in lung function [
10]. In addition, toxicity caused by hyperoxemia in some patients with COPD receiving LTOT has received attention from researchers [
16].
Notwithstanding this, all the scientific evidence supports the idea that the proper use of supplemental oxygen therapy is an important factor that can positively influence clinical outcomes in patients with respiratory failure and severe hypoxemia [
17].
The administration of LTOT requires devoted delivery devices. The source of oxygen and the equipment for its administration, which will depend on the patient’s profile, his/her movability, the flow required, the time needed for oxygen therapy sessions, and above all, the proper correction of SpO
2 both at rest and during sleep or effort are also important factors [
18].
Until recently, the most common way to deliver LTOT to patients has been by using static sources, such as stationary oxygen concentrators or high-pressure cylinders. The shortcoming of such devices is that they prevent the patient from wandering or leaving home while therapy is being received. The heightened mobility and physical activity of these patients have resulted in the need for smaller, lighter, and more autonomous portable oxygen devices [
19]. For those reasons, a new generation of portable, lightweight devices has emerged in recent years. These devices, known as portable oxygen concentrators (POCs), have sufficient autonomy to enable the patient to live an active life outside the home. Unlike classical gaseous or liquid oxygen devices, POCs produce their own oxygen by removing nitrogen from atmospheric air. Before it goes into the concentrator through the inlet filter, air is composed of 80% nitrogen and 20% oxygen. Firstly, the POC compresses the oxygen using a compressor. The compressed air moves to a sieve bed of filters that separate the nitrogen from the oxygen. Then, the oxygen, now at around 90%–95% purity, is stored in a product tank within the device and is delivered to the patient via a delivery device (i.e., a nasal cannula).
POCs can deliver oxygen via continuous flow or pulse flow. Continuous flow units put out a specific adjustable dose measured in litres per minute. Pulse units pulse air through a cannula with each breath and their output is determined by the size of the individual pulse (millilitres per pulse) and the patient’s respiratory rate.
It is accepted that the oxygen flow, normally delivered in fixed doses to patients in oxygen therapy, is not always optimized [
19]. In fact, the oxygen requirements of patients under LTOT vary depending on the type, intensity and duration of the physical activity that is being carried out. Low blood oxygen levels may cause short-term symptoms, such as dyspnoea, and physio-pathological organic changes, such as tachycardia, increased respiratory rate, arterial hypertension and, in the long term, serious problems such as pulmonary hypertension and cor pulmonale, among others. On the other hand, excessive levels of blood oxygen can cause hypercapnic encephalopathy in some patients. In this regard, the patients receiving LTOT are generally instructed to adjust the oxygen flow according to the activities of daily living. Oxygen flow is therefore routinely targeted to maintaining the desired oxygenation range. However, this task places a burden on patients that often affects adherence to therapy, and the existing methods of oxygen delivery may not be sufficient when the patient’s activity, and therefore the demand of oxygen, increases [
20]. It has been reported that patients with COPD and moderate hypoxemia have frequent and eventually significant desaturations during activities of daily living and at night [
21].
Adapting oxygen therapy to dynamic patients’ needs appears to be a key challenge. Among the primary goals of the dynamic and adaptive oxygen flow adjustment are: (a) the optimization of therapy and safety by minimizing the number of desaturation episodes, preventing periods of hyperoxia and hyperoxia [
12]; (b) the customization of the oxygen flow to the individual needs of patients; and (c) oxygen consumption optimization.
In traditional flow oxygen delivery, the titration of oxygen therapy is generally performed manually by selecting the level of oxygen flow [
22]. In LTOT, this manual adjustment of oxygen flow is carried out by patients themselves to meet their changing needs. The current POCs have a manual flow regulator that is adjusted by prescription to a specific level of flow measured in litres or pulses. Existing flow regulators modify the flow mechanically, by manipulating a valve, or electronically, by means of a keypad integrated into the device. However, the manually continuous adjustment of the oxygen flow rate is a time-consuming task that requires experienced and trained patients [
23], and this can lead to the improper use of the device and consequently to a poor quality flow adjustment during the changing daily activities, which is usually linked to unintended delays and periods of desaturation [
24,
25]. Given the advanced average age of patients with COPD under LTOT [
26], the probability of inadequate use of the device is significant.
Very recently, the abovementioned limitations led to the search for new physiological closed-loop devices (PCLC) that timely adjust oxygen flow rates to the needs of patient automatically [
22]. PCLC medical devices use one or several physiological sensors to manipulate a physiological variable autonomously according to the guidelines given by clinicians [
27]. Exponents of PCLC in respiratory medicine are the novel intelligent portable oxygen concentrators. Most of the published articles on technologies for PCLC in oxygen therapy for adults are from post-2010, indicating that these devices are a relatively new field in the respiratory speciality. These devices may potentially optimize oxygen therapy, reduce the workload of health professionals, minimise medical error, shorten health care costs, and decrease mortality and morbidity [
28,
29].
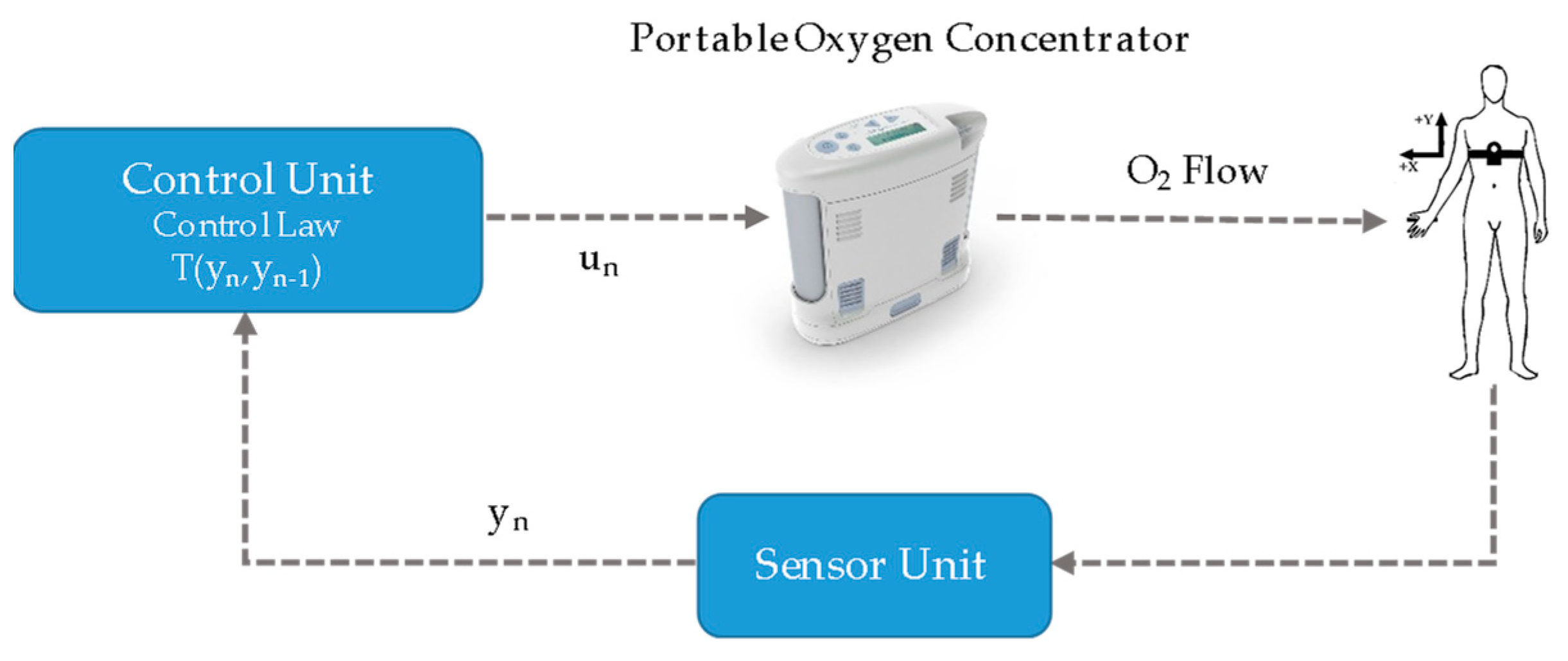
Intelligent POCs include three main components: a system for monitoring the patient’s oxygenation, an algorithm to estimate the O
2 flow settings to achieve the targeted oxygenation level, and an O
2 source [
20].
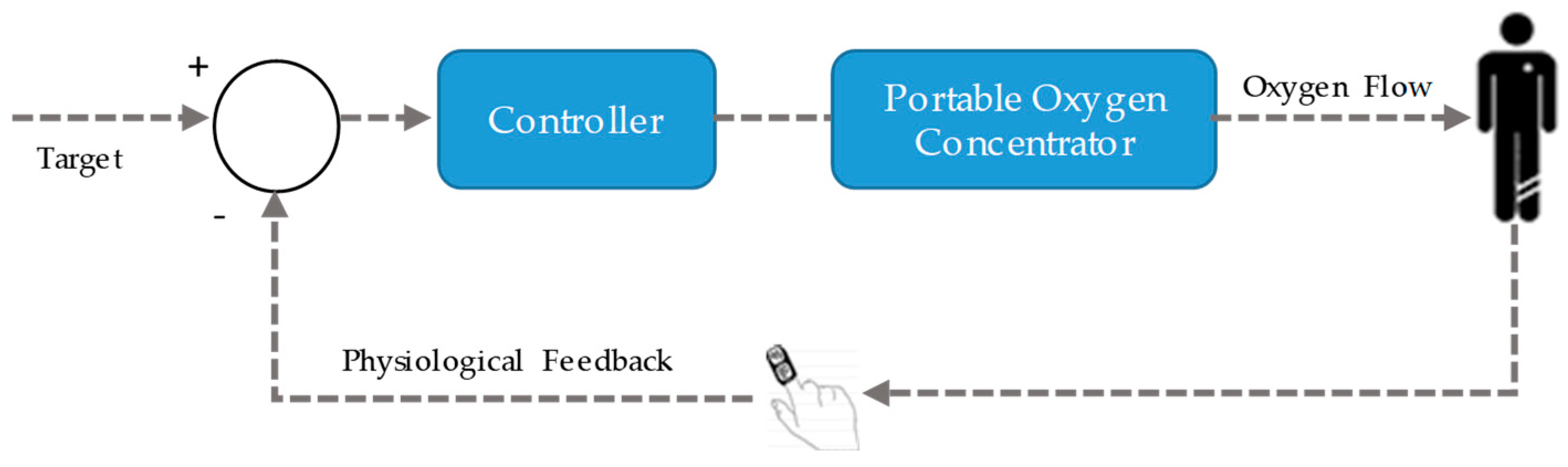
Figure 1 depicts the global architecture of a PCLC oxygen therapy device.
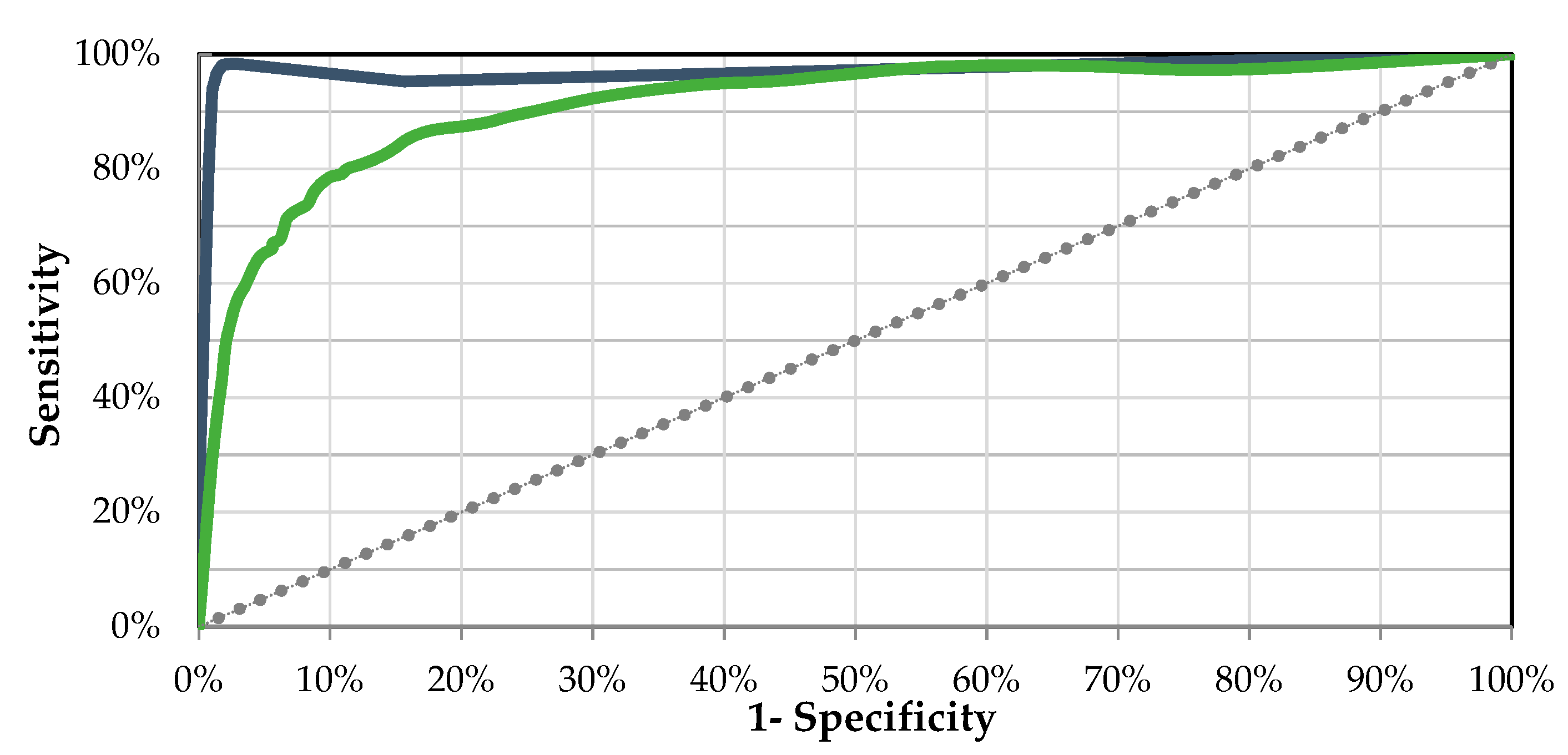
In the most common approach, the process variable is selected to be SpO
2, since it is a non-invasive measure that does not require calibration. A recent systematic review reported that SpO
2 (pulse oximeter) was used in 100% of studies on PCLC systems for automatic oxygen delivery in patients with COPD [
25]. Concerning the algorithms, the review concluded that continuous control by applying conventional classical proportional-integral-derivative (PID), proportional-integral (PI), and rule-based controllers have been proposed in the context of LTOT systems [
30,
31,
32,
33]. In these studies, the most significant findings were related to the shortening of hypoxemia and hyperoxemia episodes when PCLCs were used. However, a challenge in these algorithms is related to stability and robustness, associated with the system capacity to discriminate between real abnormal oxygenation events and ghost episodes caused by motion artefacts or a poor-quality oximetry signal. This major challenge has not been overcome, and, at present, there are only a few commercial systems available (i.e., Optisat AccuO2
® [
34], the O2 Flow Regulator
® [
33], and the FreeO2
® [
19]). The existing systems require the patients to be continuously connected to a pulse oximeter, which becomes the primary source of information for the algorithm. Current pulse oximetry technology is marked by the instability of the sensor relating to movements or by the physiological delay in the measurements, which may reduce its clinical effectiveness. Additionally, this technology presents very limited effectiveness in assessing hyperoxia and promptly detecting respiratory depression [
22]. Moreover, pulse oximeters are known to be inaccurate in conditions that decrease arterial blood perfusion or cause the presence of elevated concentrations of carboxyhaemoglobin (CoHb) and methaemoglobin (metHb).
As a consequence, the development of innovative physiological sensors and predictors of oxygen desaturations to enable autonomous therapy and support its clinical validity is still an on-going challenge [
35].
In addition to technological matters, patient perceptions on usability and adequacy of POCs is an issue. In a recent study, 51% of the patients under LTOT consulted reported oxygen problems related to equipment malfunction, a lack of physically manageable portable systems, and a lack of portable systems with high flow rates [
36]. In that study, 44% of respondents referred to the limitations in activities outside the home imposed by inadequate portable oxygen systems.
In summary, despite their potential and the existing end-users (patients) demand, PCLC oxygen therapy devices are scarcely found in real clinical applications. The robustness of control algorithms, the limited reliability of sensors, safety and usability issues, among others, can underlie this lack of clinical implementation [
25].
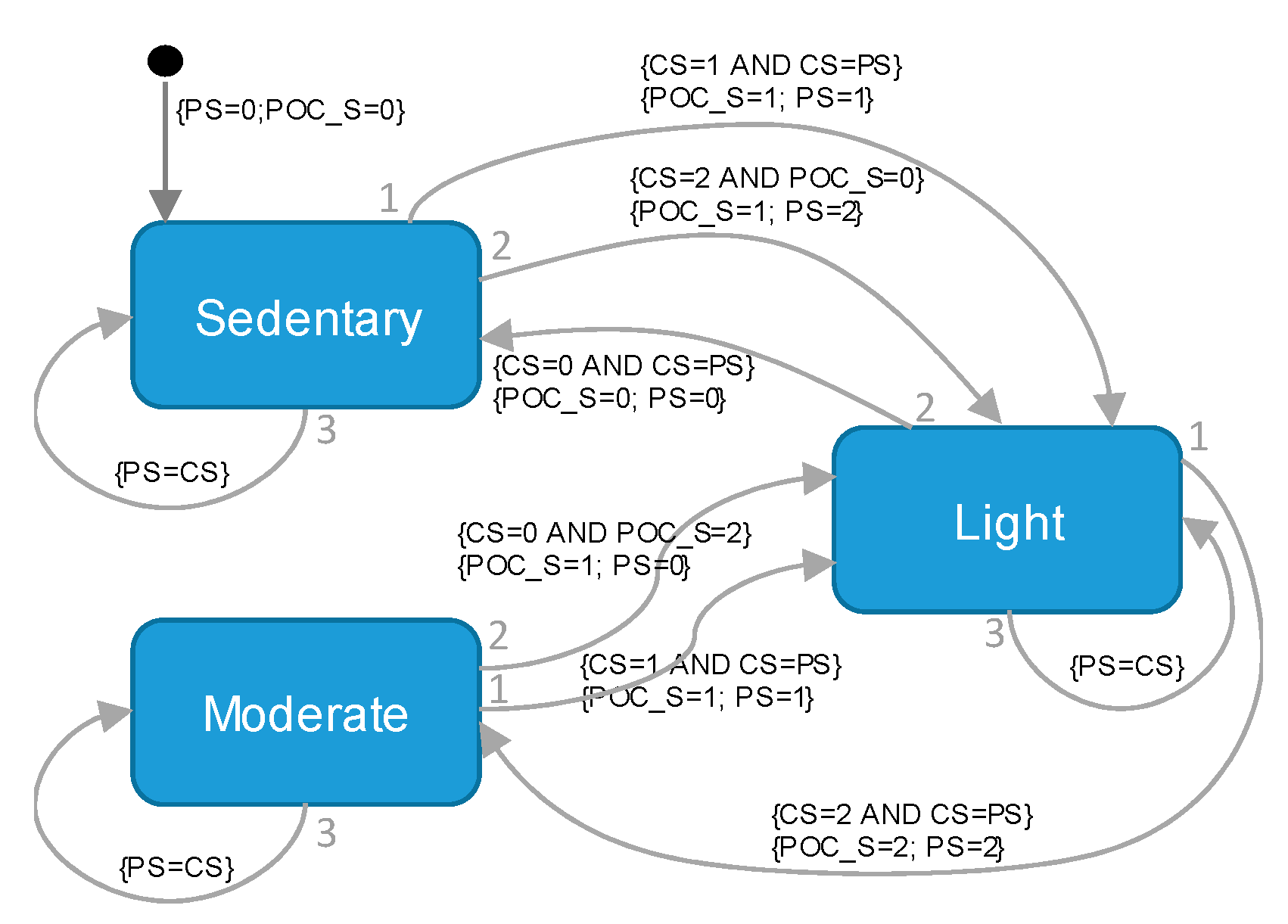
In this work, we propose an alternative approach that enables a POC to be transformed into an intelligent POC (iPOC) to adjust the oxygen flow automatically in patients with COPD and respiratory failure that receive LTOT. The proposed system is based on the automatic classification of the intensity of the patient’s physical activity and can adjust the oxygen flow to individual real-time needs autonomously. It is a transdisciplinary work, rooted in the field of respiratory medicine, with contributions from electronics, control theory, computer science and artificial intelligence.
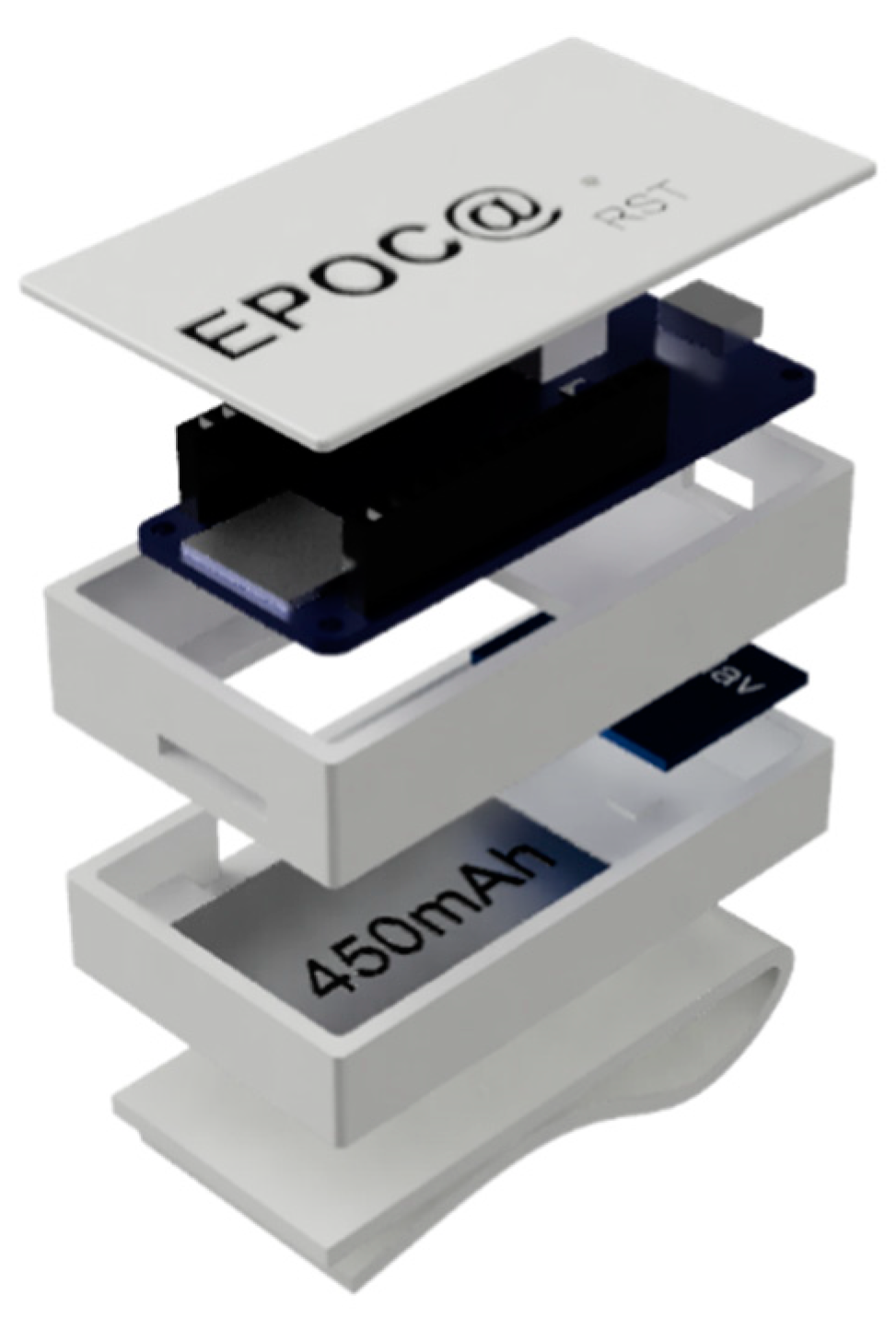
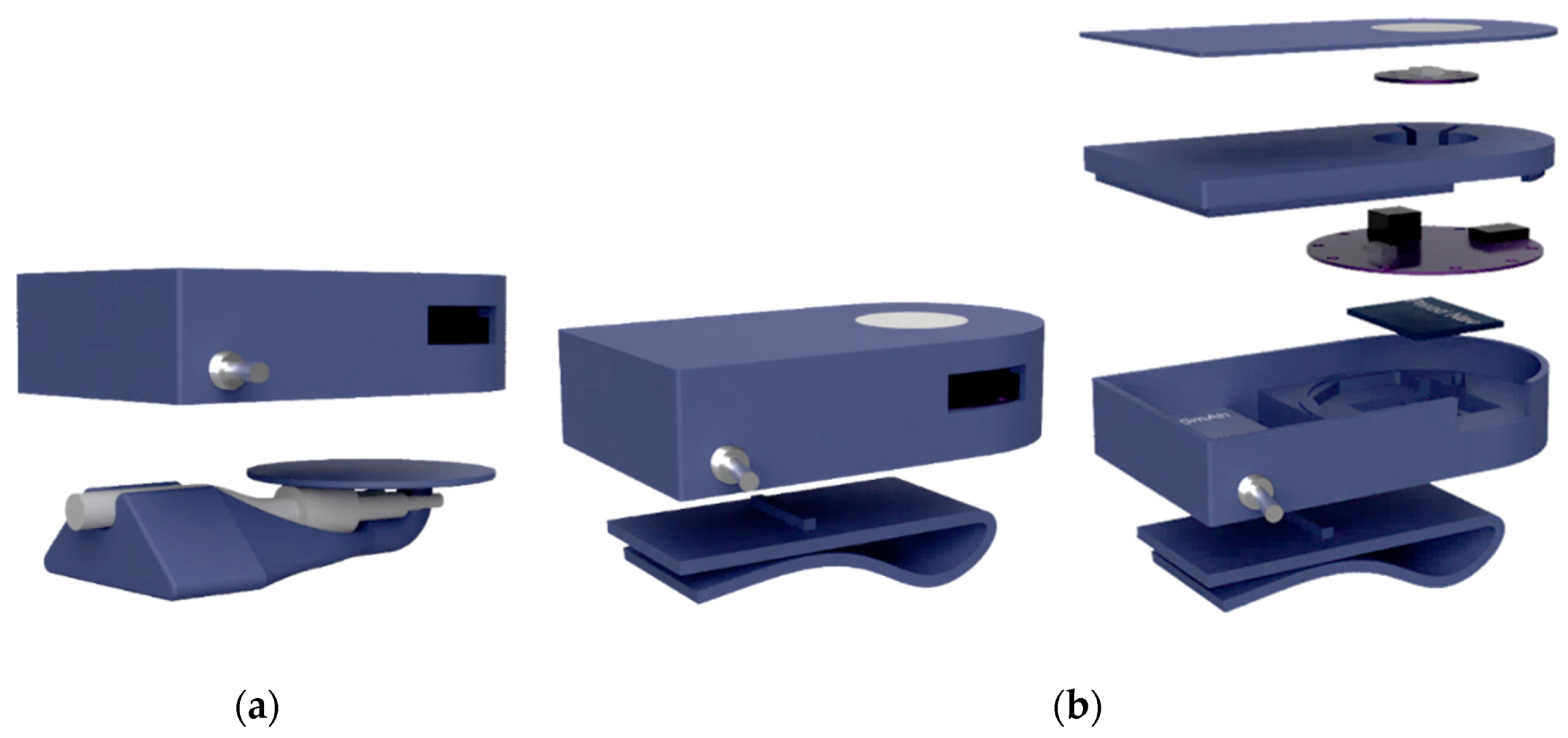
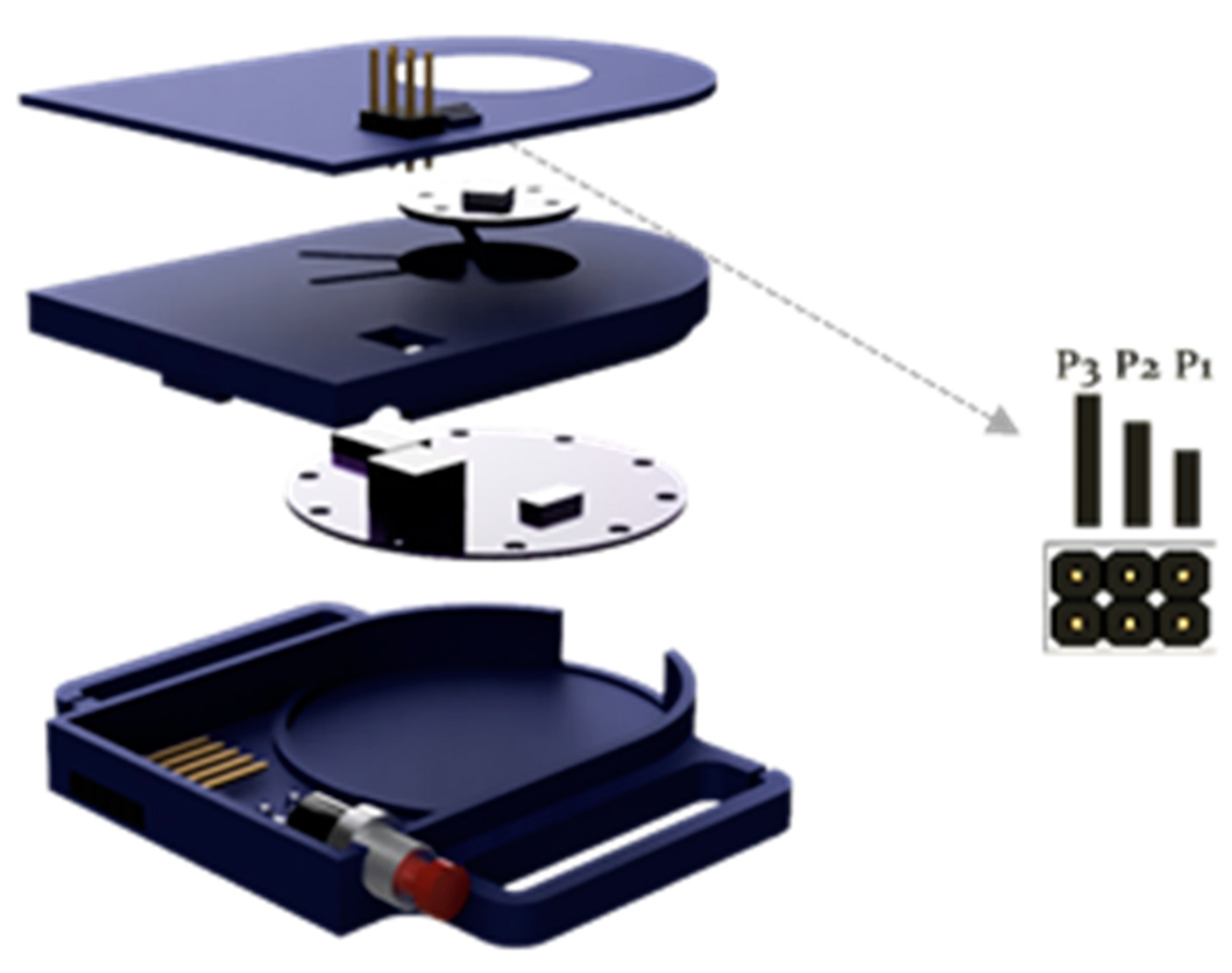
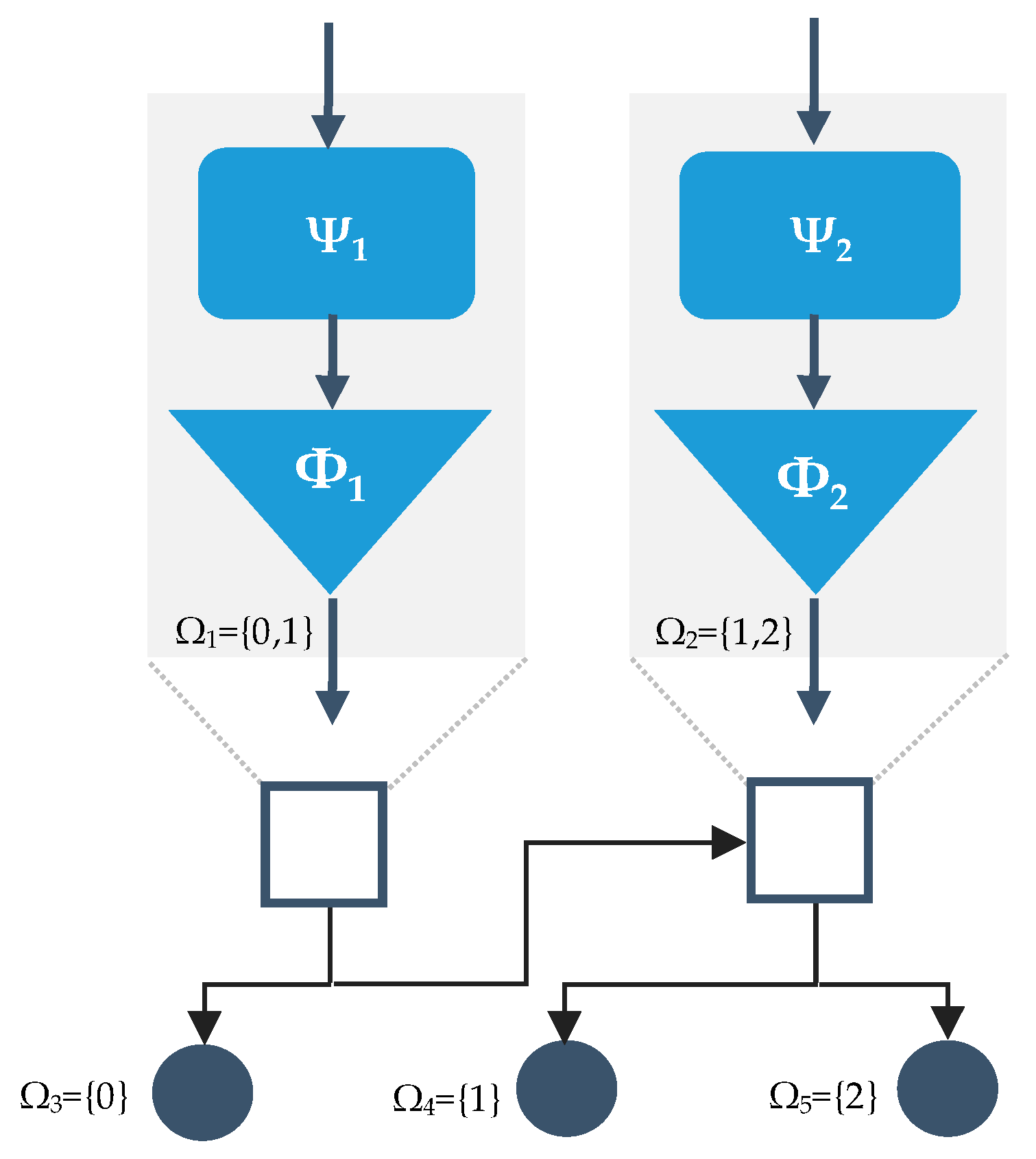
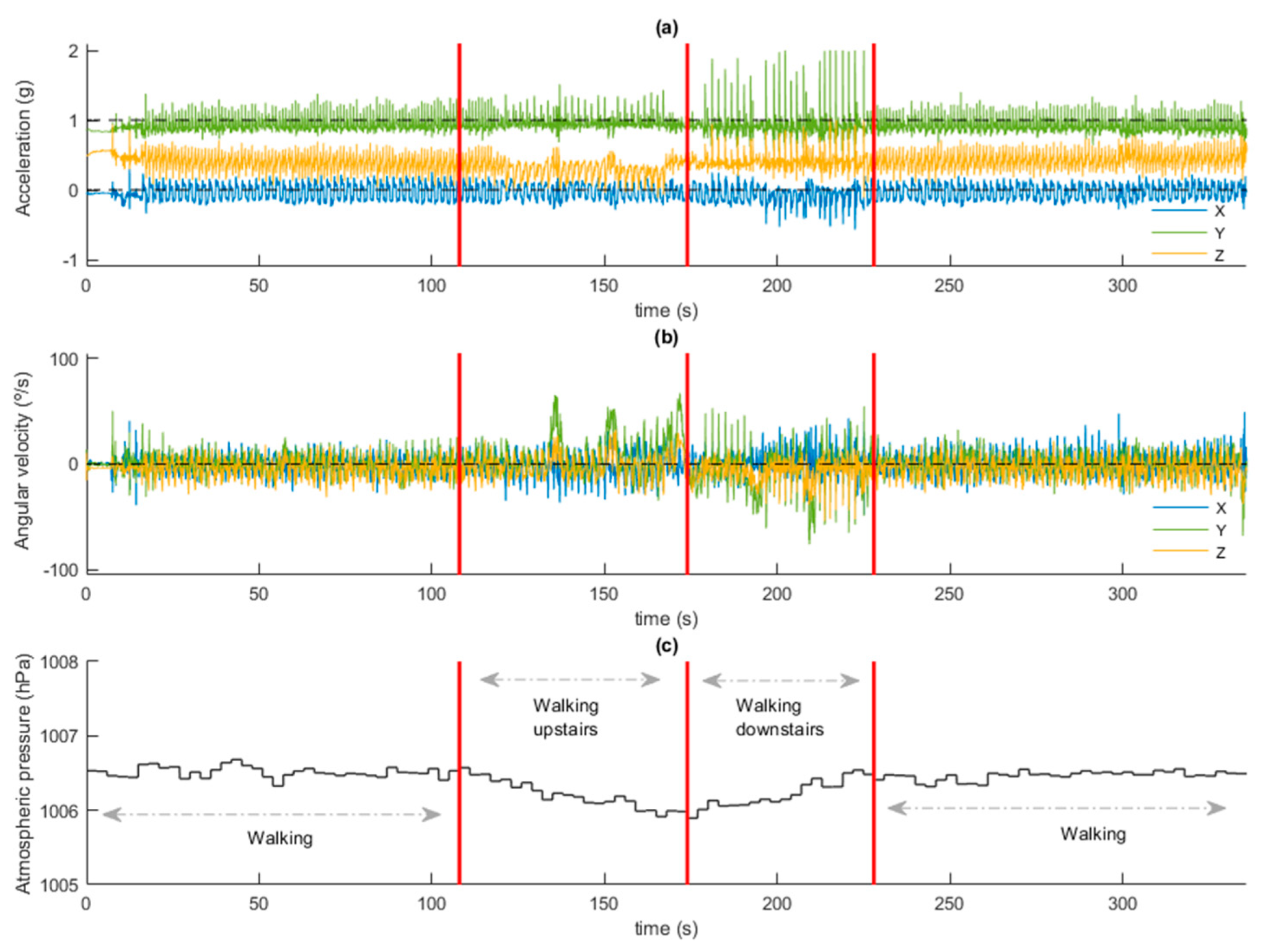
An external portable electronic system was designed and integrated into a commercially available POC. The system comprised two units: 1) a sensor unit attached to the patient, that classifies the physical activity in real-time; and 2) a receiver unit, interfaced to the POC, that adjusts the oxygen flow according to the input from the sensor unit automatically. The algorithm for the automatic recognition of physical activity was trained and validated using machine learning techniques. A circuit was designed to gather data for personalizing models and to evaluate the system performance in a group of patients with COPD and respiratory failure receiving LTOT.
The rest of the paper is organised as follows.
Section 2 details the participants, materials, devices and methodology applied to develop the iPOC system and to conduct the experiments. In
Section 3, the results achieved are presented and discussed. Finally,
Section 4 captures the conclusions and future works.
4. Conclusions
The long-term benefits of oxygen have been proven since the 1980s in certain respiratory conditions such as COPD. Very recently, future research in oxygen therapy has been pointed at developing and evaluating new models for therapeutic oxygen patient education and improving portable oxygen devices [
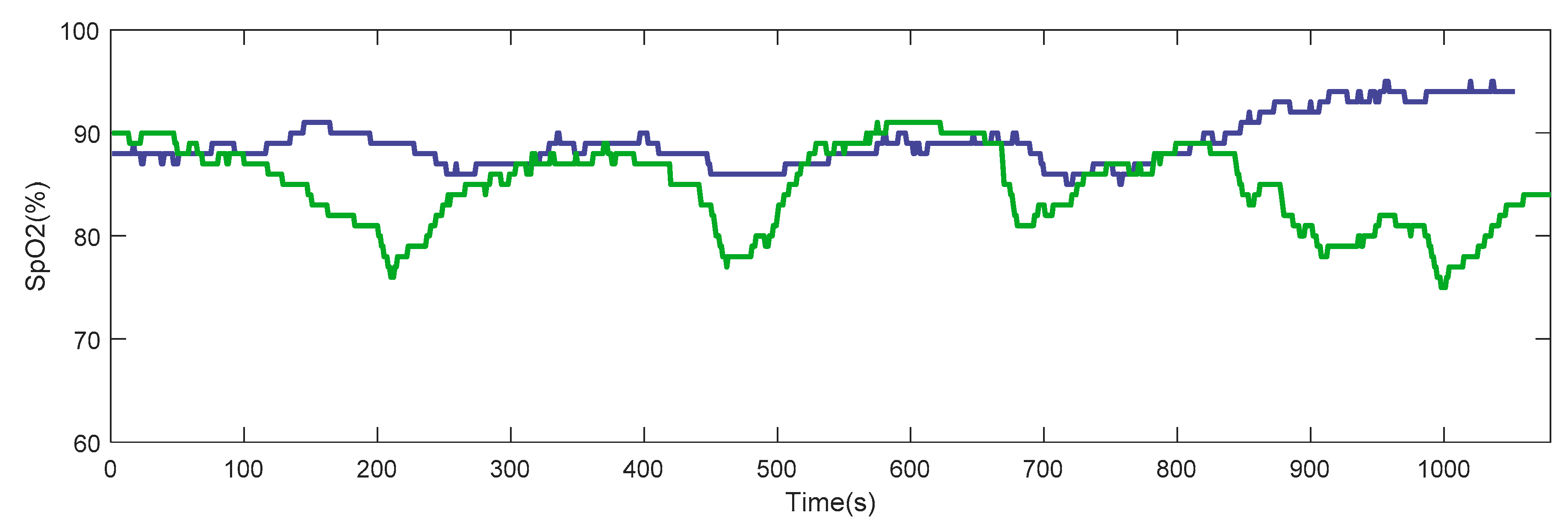
53]. It has been reported that, when compared to the conventional POCs, the closed-loop POCs can maintain higher saturation levels, spend less time below the target saturation, and save O
2 resources [
25]. The correction of exercise hypoxemia in lung diseases like COPD is crucial and challenging [
54], and automatic POCs can contribute to the individualized adjustment of oxygen flow.
Currently, the challenge of designing closed-loop portable devices which are able to adjust O2 flow automatically is being faced by mainly using indirectly measured blood oxygen saturation as a process variable to close the loop. However, the robustness of control algorithms and the limited reliability of current oximetry sensors are hindering the effectiveness of this approach.
In line with all the above-mentioned factors, this study presents the proof of concept of an alternative approach: a system to transform a conventional POC into a closed-loop controlled device capable of automatically self-adjusting, in real time, the oxygen flow supplied to the patient according to the intensity of the physical activity carried out by the user under LTOT.
A sensor unit capable of detecting the physical intensity developed by the patient (in real time) has been developed and evaluated. This sensor unit can wirelessly connect to the POC for the self-adjustment of the oxygen flow. The system has been designed with the flexibility to customize up to seven different oxygen therapy profiles. The developed iPOC was tested with a widely used commercial POC unit. For this purpose, a treadmill circuit was designed that included basic physical activities most common in the daily practice of elderly patients with respiratory disorders. Different models were trained and validated using artificial intelligence techniques, a wrapper approach, 98 time-domain features, and data from 18 patients with COPD and respiratory failure. A final meta-classifier (BHC) was designed and deployed in the sensor unit to operate in real-time. A weighted accuracy of 91.1% was achieved in the technical pilot test with five patients. A reduction in the number of desaturation events was achieved in 80% of patients as well as improved minimum and average blood oxygen saturation values compared to the POC in manual operating mode. In these cases, CT90 and CT85 also showed a promising better response when the iPOC was used. Finally, all interviewed patients (N = 33) considered that the proposed iPOC satisfied them, and could promote their physical activity outside the home.
Among the limitations of this study were those related to hypoxia. In this regard, the combination of the proposed system with the novel oxygen reserve index (ORI) included in the new generation of pulse oximeters that use multi-wavelength pulse co-oximetry might improve oxygen titration and enable the prevention of unintended hyperoxia [
55].
A closed-loop control system, like the proposed iPOC, has clear potential benefits, including improved oxygenation regardless of physical activity and enhanced patient follow-up and compliance with therapy recommendations. In addition, closed-loop oxygen supply systems have shown that they can potentially reduce medical error, improve morbidity and mortality, and reduce care costs [
22].
Future research steps include the miniaturization of the sensor unit, expanding the study sample, and the home monitoring of the patients while using IPOC during daily tasks in an unsupervised environment, in order to obtain clinical evidence of the impact that this approach may have on the targeted patient population.