Noble Metal-Assisted Surface Plasmon Resonance Immunosensors
Abstract
1. Introduction
2. Analytical Methods for Protein Biomarkers
3. Analytical Methods for Viral Agents
4. Analytical Methods for Pathogenic Microbes
5. Analytical Methods for Extracellular Vesicles (EVs)
6. Future Perspective and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gong, C.; Leite, M.S. Noble Metal Alloys for Plasmonics. Acs Photonics 2016, 3, 507–513. [Google Scholar] [CrossRef]
- Haes, A.J.; Zou, S.L.; Schatz, G.C.; Van Duyne, R.P. Nanoscale optical biosensor: Short range distance dependence of the localized surface plasmon resonance of noble metal nanoparticles. J. Phys. Chem B 2004, 108, 6961–6968. [Google Scholar] [CrossRef]
- Sugawa, K.; Tahara, H.; Yamashita, A.; Otsuki, J.; Sagara, T.; Harumoto, T.; Yanagida, S. Refractive Index Susceptibility of the Plasmonic Palladium Nanoparticle: Potential as the Third Plasmonic Sensing Material. Acs Nano 2015, 9, 1895–1904. [Google Scholar] [CrossRef] [PubMed]
- Haes, A.J.; Zou, S.L.; Schatz, G.C.; Van Duyne, R.P. A nanoscale optical biosensor: The long range distance dependence of the localized surface plasmon resonance of noble metal nanoparticles. J. Phys. Chem B 2004, 108, 109–116. [Google Scholar] [CrossRef]
- Schasfoort, R.B. Handbook of surface plasmon resonance; Royal Society of Chemistry: London, UK, 2017. [Google Scholar]
- Rich, R.L.; Myszka, D.G. Advances in surface plasmon resonance biosensor analysis. Curr Opin Biotechnol 2000, 11, 54–61. [Google Scholar] [CrossRef]
- Yang, L.; Lee, J.H.; Rathnam, C.; Hou, Y.; Choi, J.W.; Lee, K.B. Dual-Enhanced Raman Scattering-Based Characterization of Stem Cell Differentiation Using Graphene-Plasmonic Hybrid Nanoarray. Nano Lett 2019, 19, 8138–8148. [Google Scholar] [CrossRef]
- Eustis, S.; El-Sayed, M.A. Why gold nanoparticles are more precious than pretty gold: Noble metal surface plasmon resonance and its enhancement of the radiative and nonradiative properties of nanocrystals of different shapes. Chem. Soc. Rev. 2006, 35, 209–217. [Google Scholar] [CrossRef]
- Jain, P.K.; Huang, X.; El-Sayed, I.H.; El-Sayad, M.A. Review of some interesting surface plasmon resonance-enhanced properties of noble metal nanoparticles and their applications to biosystems. Plasmonics 2007, 2, 107–118. [Google Scholar] [CrossRef]
- Nguyen, H.H.; Park, J.; Kang, S.; Kim, M. Surface plasmon resonance: a versatile technique for biosensor applications. Sensors 2015, 15, 10481–10510. [Google Scholar] [CrossRef]
- Brolo, A.G. Plasmonics for future biosensors. Nature Photon. 2012, 6, 709–713. [Google Scholar] [CrossRef]
- Belotelov, V.; Akimov, I.; Pohl, M.; Kalish, A.; Kasture, S.; Vengurlekar, A.; Gopal, A.; Kotov, V.; Yakovlev, D.; Zvezdin, A. Intensity magnetooptical effect in magnetoplasmonic crystals. In Proceedings of Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2011; p. 012038. [Google Scholar]
- Rizal, C.; Belotelov, V. Sensitivity comparison of surface plasmon resonance (SPR) and magneto-optic SPR biosensors. Eur. Phys. J. Plus 2019, 134, 435. [Google Scholar] [CrossRef]
- Singh, P. SPR Biosensors: Historical Perspectives and Current Challenges. Sensor Actuat. B-Chem. 2016, 229, 110–130. [Google Scholar] [CrossRef]
- Kim, D.; Choi, E.; Lee, C.; Choi, Y.; Kim, H.; Yu, T.; Piao, Y. Highly sensitive and selective visual detection of Cr(VI) ions based on etching of silver-coated gold nanorods. Nano. Converg. 2019, 6, 34. [Google Scholar] [CrossRef] [PubMed]
- Rizal, C.; Pisana, S.; Hrvoic, I. Improved magneto-optic surface plasmon resonance biosensors. In Proceedings of Photonics; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2018; p. 15. [Google Scholar]
- Rizal, C.; Pisana, S.; Hrvoic, I.; Fullerton, E.E. Microstructure and magneto-optical surface plasmon resonance of Co/Au multilayers. J. Phys. Commun. 2018, 2, 055010. [Google Scholar] [CrossRef]
- Gupta, B.D.; Kant, R. [INVITED] Recent advances in surface plasmon resonance based fiber optic chemical and biosensors utilizing bulk and nanostructures. Opt. Laser Technol. 2018, 101, 144–161. [Google Scholar] [CrossRef]
- Masson, J.F. Surface Plasmon Resonance Clinical Biosensors for Medical Diagnostics. ACS Sens. 2017, 2, 16–30. [Google Scholar] [CrossRef]
- Piliarik, M.; Homola, J. Surface plasmon resonance (SPR) sensors: approaching their limits? Optics express. 2009, 17, 16505–16517. [Google Scholar] [CrossRef]
- Rippa, M.; Castagna, R.; Pannico, M.; Musto, P.; Zyss, J.; Petti, L. Multi-sensing meta nanostructures with surface-enhanced Raman scattering and surface plasmon resonance functionalities. In Proceedings of the 19th Italian National Conference on Photonic Technologies (Fotonica 2017), Padua, Italy, 3–5 May 2017. [Google Scholar]
- Hasan, M.R.; Akter, S.; Rifat, A.A.; Rana, S.; Ahmed, K.; Ahmed, R.; Subbaraman, H.; Abbott, D. Spiral photonic crystal fiber-based dual-polarized surface plasmon resonance biosensor. IEEE Sens. J. 2017, 18, 133–140. [Google Scholar] [CrossRef]
- Cheng, C.; Chen, H.-Y.; Wu, C.-S.; Meena, J.S.; Simon, T.; Ko, F.-H. A highly sensitive and selective cyanide detection using a gold nanoparticle-based dual fluorescence–colorimetric sensor with a wide concentration range. Sens. Actuators B Chem. 2016, 227, 283–290. [Google Scholar] [CrossRef]
- Mauriz, E.; Garcia-Fernandez, M.C.; Lechuga, L.M. Towards the design of universal immunosurfaces for SPR-based assays: A review. Trac-Trend Anal. Chem. 2016, 79, 191–198. [Google Scholar] [CrossRef]
- Guo, T.; Gonzalez-Vila, A.; Loyez, M.; Caucheteur, C. Plasmonic Optical Fiber-Grating Immunosensing: A Review. Sensors 2017, 17, 2732. [Google Scholar] [CrossRef]
- Sahu, V.; Gupta, A.; Kumar, R.; Gupta, T.; Mohan, A.; Dey, S. Quantification of Rac1 and Rac1b in serum of non small cell lung cancer by label free real time assay. Clin. Chim. Acta 2016, 460, 231–235. [Google Scholar] [CrossRef]
- Vashist, S.K.; Schneider, E.M.; Luong, J.H. Surface plasmon resonance-based immunoassay for human C-reactive protein. Analyst 2015, 140, 4445–4452. [Google Scholar] [CrossRef]
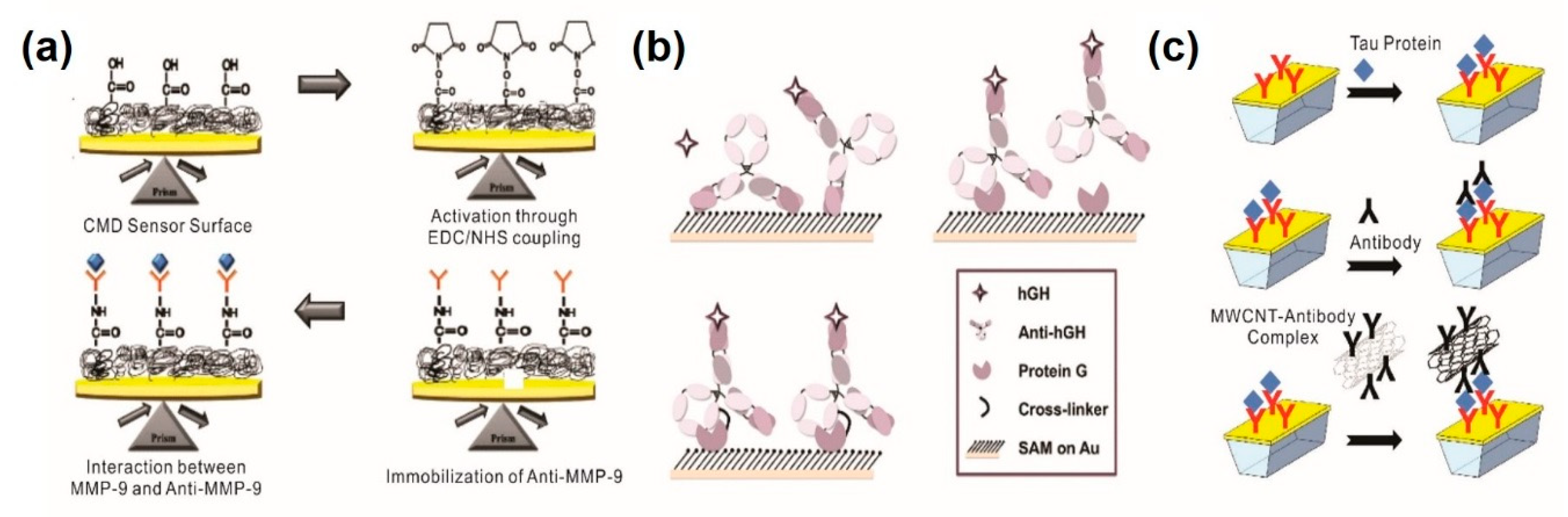
- Mohseni, S.; Moghadam, T.T.; Dabirmanesh, B.; Jabbari, S.; Khajeh, K. Development of a label-free SPR sensor for detection of matrixmetalloproteinase-9 by antibody immobilization on carboxymethyldextran chip. Biosen.s Bioelectron. 2016, 81, 510–516. [Google Scholar] [CrossRef]
- Makaraviciute, A.; Ramanavicius, A.; Ramanaviciene, A. Development of a reusable protein G based SPR immunosensor for direct human growth hormone detection in real samples. Anal. Methods 2015, 7, 9875–9884. [Google Scholar] [CrossRef]
- Lisi, S.; Scarano, S.; Fedeli, S.; Pascale, E.; Cicchi, S.; Ravelet, C.; Peyrin, E.; Minunni, M. Toward sensitive immuno-based detection of tau protein by surface plasmon resonance coupled to carbon nanostructures as signal amplifiers. Biosens. Bioelectron. 2017, 93, 289–292. [Google Scholar] [CrossRef]
- Kausaite-Minkstimiene, A.; Ramanaviciene, A.; Kirlyte, J.; Ramanavicius, A. Comparative study of random and oriented antibody immobilization techniques on the binding capacity of immunosensor. Anal. Chem. 2010, 82, 6401–6408. [Google Scholar] [CrossRef]
- Ermini, M.L.; Chadtova Song, X.; Springer, T.; Homola, J. Peptide Functionalization of Gold Nanoparticles for the Detection of Carcinoembryonic Antigen in Blood Plasma via SPR-Based Biosensor. Front. Chem. 2019, 7, 40. [Google Scholar] [CrossRef]
- Pawula, M.; Altintas, Z.; Tothill, I.E. SPR detection of cardiac troponin T for acute myocardial infarction. Talanta 2016, 146, 823–830. [Google Scholar] [CrossRef]
- Ashaduzzaman, M.; Deshpande, S.R.; Murugan, N.A.; Mishra, Y.K.; Turner, A.P.; Tiwari, A. On/off-switchable LSPR nano-immunoassay for troponin-T. Sci. Rep. 2017, 7, 44027. [Google Scholar] [CrossRef]
- Ben Haddada, M.; Hu, D.; Salmain, M.; Zhang, L.; Peng, C.; Wang, Y.; Liedberg, B.; Boujday, S. Gold nanoparticle-based localized surface plasmon immunosensor for staphylococcal enterotoxin A (SEA) detection. Anal. Bioanal. Chem. 2017, 409, 6227–6234. [Google Scholar] [CrossRef] [PubMed]
- Loiseau, A.; Zhang, L.; Hu, D.; Salmain, M.; Mazouzi, Y.; Flack, R.; Liedberg, B.; Boujday, S. Core-Shell Gold/Silver Nanoparticles for Localized Surface Plasmon Resonance-Based Naked-Eye Toxin Biosensing. ACS Appl Mater. Interfaces 2019, 11, 46462–46471. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.U.; Nguyen, A.H.; Sim, S.J. A nanoplasmonic biosensor for label-free multiplex detection of cancer biomarkers. Biosens. Bioelectron. 2015, 74, 341–346. [Google Scholar] [CrossRef]
- Jia, K.; Khayway, M.; Li, Y.; Bijeon, J.-L.; Adam, P.-M.; Déturche, R.; Guelorget, B.; François, M.; Louarn, G.; Ionescu, R.E. Strong improvements of LSPR sensitivity by using Au/Ag bi-metallic nanostructures modified with poly-dopamine films. ACS Appl. Mater. Interfaces 2014, 6, 219–227. [Google Scholar] [CrossRef] [PubMed]
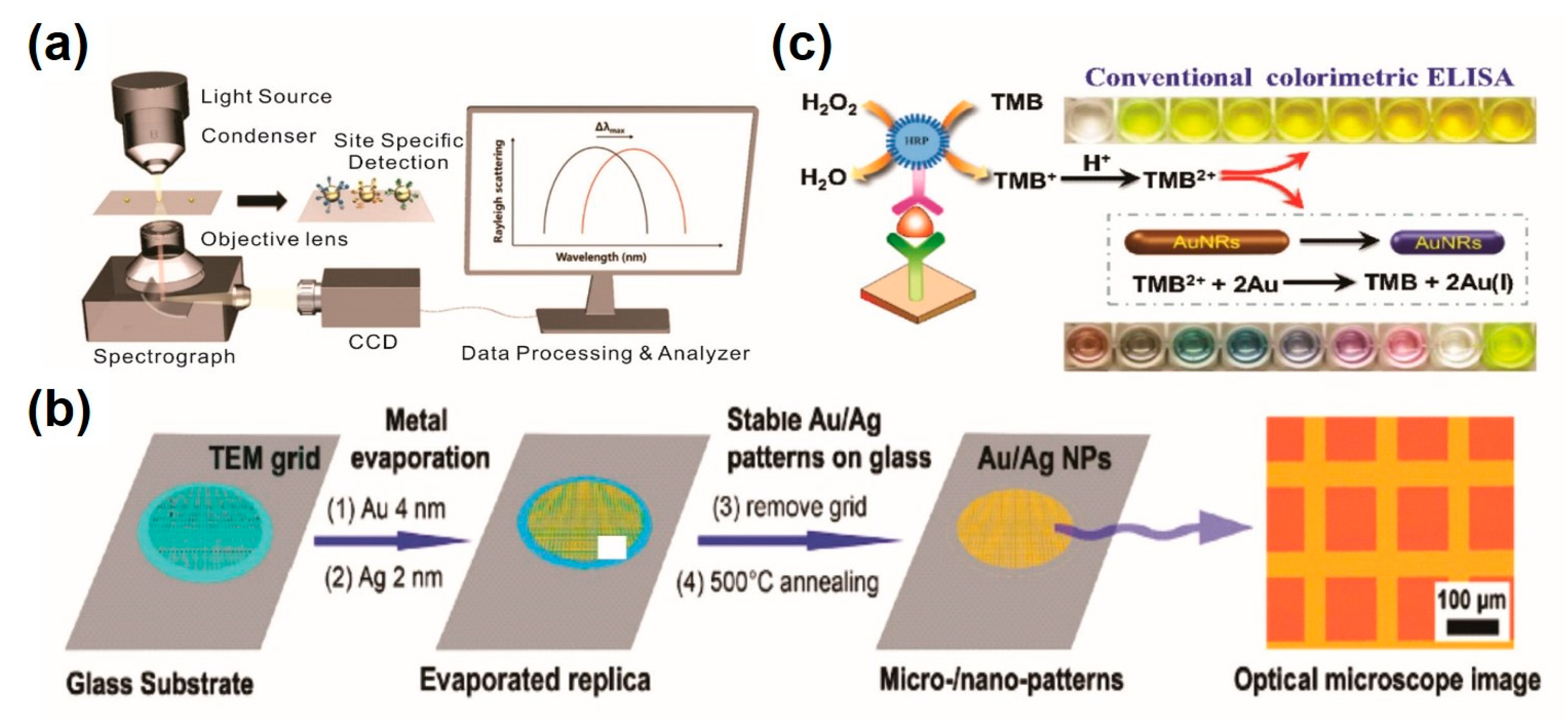
- Ma, X.; Lin, Y.; Guo, L.; Qiu, B.; Chen, G.; Yang, H.H.; Lin, Z. A universal multicolor immunosensor for semiquantitative visual detection of biomarkers with the naked eyes. Biosens. Bioelectron. 2017, 87, 122–128. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, H.; Chen, Z.; Wang, X.; Choo, J.; Chen, L. Plasmonic colorimetric sensors based on etching and growth of noble metal nanoparticles: Strategies and applications. Biosens. Bioelectron. 2018, 114, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Inci, F.; Tokel, O.; Wang, S.; Gurkan, U.A.; Tasoglu, S.; Kuritzkes, D.R.; Demirci, U. Nanoplasmonic quantitative detection of intact viruses from unprocessed whole blood. ACS Nano 2013, 7, 4733–4745. [Google Scholar] [CrossRef]
- Akira, S.; Uematsu, S.; Takeuchi, O. Pathogen recognition and innate immunity. Cell 2006, 124, 783–801. [Google Scholar] [CrossRef]
- Feldmann, H.; Geisbert, T.W. Ebola haemorrhagic fever. Lancet 2011, 377, 849–862. [Google Scholar] [CrossRef]
- World Health Organization. Dengue and Severe Dengue; World Health Organization. Regional Office for the Eastern Mediterranean: Cairo, Egypt, 2014. [Google Scholar]
- Lee, J.H.; Oh, B.K.; Choi, J.W. Development of a HIV-1 Virus Detection System Based on Nanotechnology. Sensors 2015, 15, 9915–9927. [Google Scholar] [CrossRef]
- Caygill, R.L.; Blair, G.E.; Millner, P.A. A review on viral biosensors to detect human pathogens. Anal. Chim. Acta 2010, 681, 8–15. [Google Scholar] [CrossRef] [PubMed]
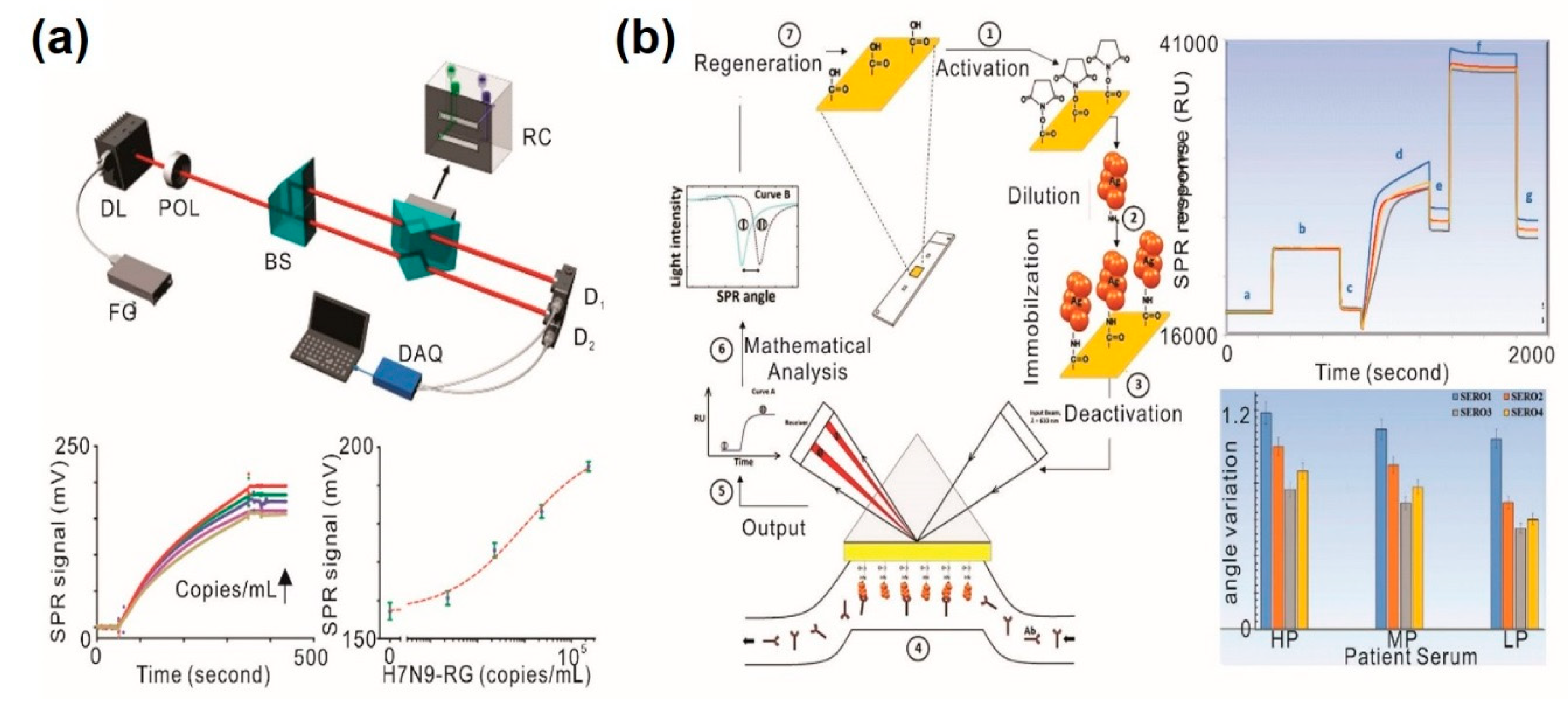
- Chang, Y.F.; Wang, W.H.; Hong, Y.W.; Yuan, R.Y.; Chen, K.H.; Huang, Y.W.; Lu, P.L.; Chen, Y.H.; Chen, Y.A.; Su, L.C.; et al. Simple Strategy for Rapid and Sensitive Detection of Avian Influenza A H7N9 Virus Based on Intensity-Modulated SPR Biosensor and New Generated Antibody. Anal. Chem 2018, 90, 1861–1869. [Google Scholar] [CrossRef]
- Jahanshahi, P.; Zalnezhad, E.; Sekaran, S.D.; Adikan, F.R. Rapid immunoglobulin M-based dengue diagnostic test using surface plasmon resonance biosensor. Sci. Rep. 2014, 4, 3851. [Google Scholar] [CrossRef]
- Loureiro, F.C.C.L.; Neff, H.; Melcher, E.U.K.; Roque, R.A.; de Figueiredo, R.M.P.; Thirstrup, C.; Borre, M.B.; Lima, A.M.N. Simplified immunoassay for rapid Dengue serotype diagnosis, revealing insensitivity to non-specific binding interference. Sensing and Bio-Sensing Research 2017, 13, 96–103. [Google Scholar] [CrossRef]
- Luo, B.; Xu, Y.; Wu, S.; Zhao, M.; Jiang, P.; Shi, S.; Zhang, Z.; Wang, Y.; Wang, L.; Liu, Y. A novel immunosensor based on excessively tilted fiber grating coated with gold nanospheres improves the detection limit of Newcastle disease virus. Biosens. Bioelectron. 2018, 100, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, B.C.; Oh, B.K.; Choi, J.W. Highly sensitive localized surface plasmon resonance immunosensor for label-free detection of HIV-1. Nanomedicine 2013, 9, 1018–1026. [Google Scholar] [CrossRef]
- Kim, J.; Oh, S.Y.; Shukla, S.; Hong, S.B.; Heo, N.S.; Bajpai, V.K.; Chun, H.S.; Jo, C.H.; Choi, B.G.; Huh, Y.S.; et al. Heteroassembled gold nanoparticles with sandwich-immunoassay LSPR chip format for rapid and sensitive detection of hepatitis B virus surface antigen (HBsAg). Biosens. Bioelectron. 2018, 107, 118–122. [Google Scholar] [CrossRef]
- Salyers, A.A.; Whitt, D.D.; Whitt, D.D. Bacterial Pathogenesis: A Molecular Approach; ASM Press: Washington, DC, USA, 1994; Volume 3. [Google Scholar]
- Park, Y.M.; Lim, S.Y.; Jeong, S.W.; Song, Y.; Bae, N.H.; Hong, S.B.; Choi, B.G.; Lee, S.J.; Lee, K.G. Flexible nanopillar-based electrochemical sensors for genetic detection of foodborne pathogens. Nano Converg. 2018, 5, 15. [Google Scholar] [CrossRef]
- Alsan, M.; Schoemaker, L.; Eggleston, K.; Kammili, N.; Kolli, P.; Bhattacharya, J. Out-of-pocket health expenditures and antimicrobial resistance in low-income and middle-income countries: an economic analysis. Lancet. Infect. Dis. 2015, 15, 1203–1210. [Google Scholar] [CrossRef]
- Adegbola, R.A.; DeAntonio, R.; Hill, P.C.; Roca, A.; Usuf, E.; Hoet, B.; Greenwood, B.M. Carriage of Streptococcus pneumoniae and other respiratory bacterial pathogens in low and lower-middle income countries: a systematic review and meta-analysis. PLoS ONE 2014, 9, e103293. [Google Scholar] [CrossRef]
- Kim, D.W.; Chun, H.J.; Kim, J.H.; Yoon, H.; Yoon, H.C. A non-spectroscopic optical biosensor for the detection of pathogenic Salmonella Typhimurium based on a stem-loop DNA probe and retro-reflective signaling. Nano. Converg. 2019, 6, 16. [Google Scholar] [CrossRef]
- Lazcka, O.; Del Campo, F.J.; Munoz, F.X. Pathogen detection: a perspective of traditional methods and biosensors. Biosens. Bioelectron. 2007, 22, 1205–1217. [Google Scholar] [CrossRef]
- Mansfield, L.; Forsythe, S. The detection of Salmonella using a combined immunomagnetic separation and ELISA end-detection procedure. Lett. Appl. Microbiol. 2000, 31, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.H.; Irudayaraj, J. In-situ immuno-gold nanoparticle network ELISA biosensors for pathogen detection. Int. J. Food Microbiol. 2013, 164, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Torun, O.; Hakki Boyaci, I.; Temur, E.; Tamer, U. Comparison of sensing strategies in SPR biosensor for rapid and sensitive enumeration of bacteria. Biosens. Bioelectron. 2012, 37, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Rushworth, J.V.; Hirst, N.A.; Millner, P.A. Biosensors for whole-cell bacterial detection. Clin. Microbiol. Rev. 2014, 27, 631–646. [Google Scholar] [CrossRef] [PubMed]
- Oh, B.K.; Lee, W.; Chun, B.S.; Bae, Y.M.; Lee, W.H.; Choi, J.W. The fabrication of protein chip based on surface plasmon resonance for detection of pathogens. Biosens. Bioelectron. 2005, 20, 1847–1850. [Google Scholar] [CrossRef] [PubMed]
- Jyoung, J.Y.; Hong, S.H.; Lee, W.; Choi, J.W. Immunosensor for the detection of Vibrio cholerae O1 using surface plasmon resonance. Biosens. Bioelectron. 2006, 21, 2315–2319. [Google Scholar] [CrossRef]
- Taheri, R.A.; Rezayan, A.H.; Rahimi, F.; Mohammadnejad, J.; Kamali, M. Development of an immunosensor using oriented immobilized anti-OmpW for sensitive detection of Vibrio cholerae by surface plasmon resonance. Biosens. Bioelectron. 2016, 86, 484–488. [Google Scholar] [CrossRef]
- Makhneva, E.; Farka, Z.; Skladal, P.; Zajickova, L. Cyclopropylamine plasma polymer surfaces for label-free SPR and QCM immunosensing of Salmonella. Sensor Actuat. B-Chem. 2018, 276, 447–455. [Google Scholar] [CrossRef]
- Chen, J.; Park, B. Label-free screening of foodborne Salmonella using surface plasmon resonance imaging. Anal. Bioanal. Chem. 2018, 410, 5455–5464. [Google Scholar] [CrossRef] [PubMed]
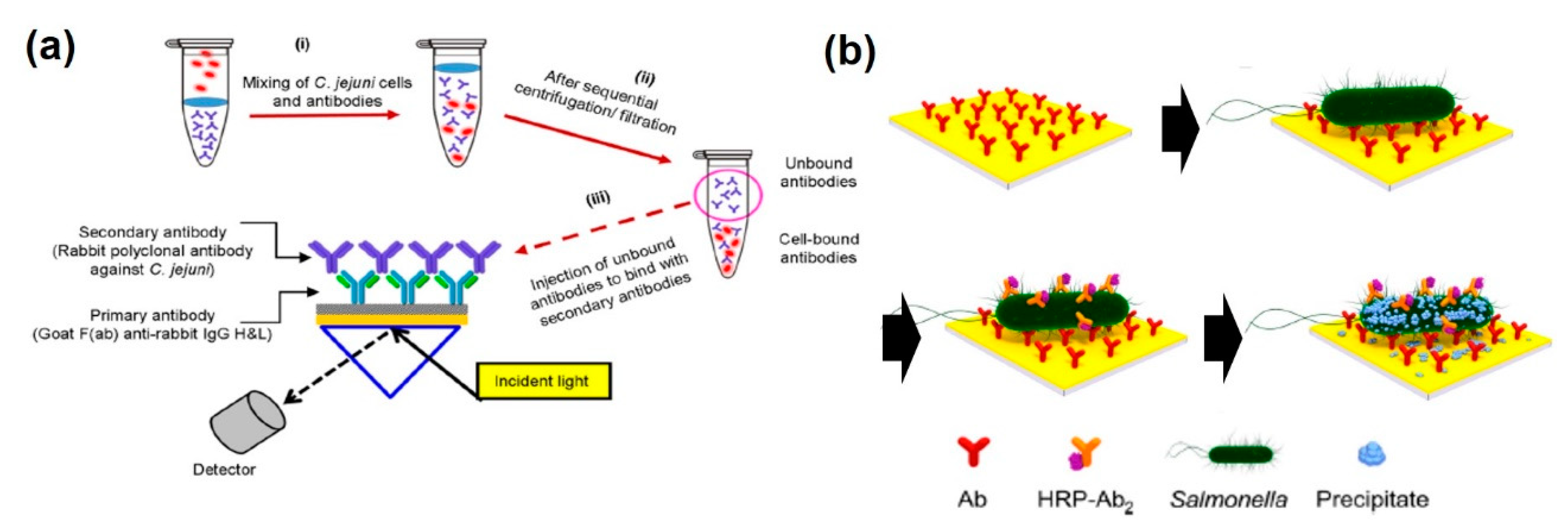
- Masdor, N.A.; Altintas, Z.; Shukor, M.Y.; Tothilll, I.E. Subtractive inhibition assay for the detection of Campylobacter jejuni in chicken samples using surface plasmon resonance. Scientific Reports 2019, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Farka, Z.; Jurik, T.; Pastucha, M.; Skladal, P. Enzymatic Precipitation Enhanced Surface Plasmon Resonance Immunosensor for the Detection of Salmonella in Powdered Milk. Anal. Chem. 2016, 88, 11830–11836. [Google Scholar] [CrossRef] [PubMed]
- Zou, F.; Wang, X.X.; Qi, F.J.; Kohn, K.; Lee, J.; Zhou, H.J.; Chen, H.X. Magneto-plamonic nanoparticles enhanced surface plasmon resonance TB sensor based on recombinant gold binding antibody. Sensor Actuat. B-Chem. 2017, 250, 356–363. [Google Scholar] [CrossRef]
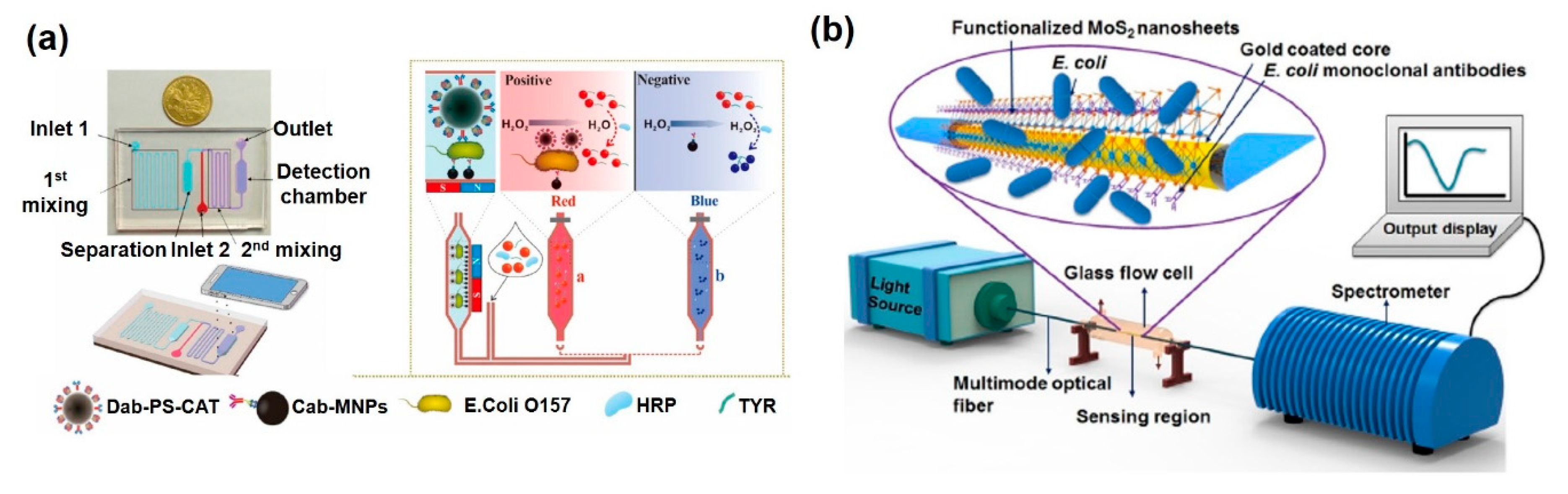
- Zheng, L.; Cai, G.; Wang, S.; Liao, M.; Li, Y.; Lin, J. A microfluidic colorimetric biosensor for rapid detection of Escherichia coli O157: H7 using gold nanoparticle aggregation and smart phone imaging. Biosens. Bioelectron. 2019, 124, 143–149. [Google Scholar] [CrossRef]
- Zhang, L.; Salmain, M.l.; Liedberg, B.; Boujday, S. Naked Eye Immunosensing of Food Biotoxins Using Gold Nanoparticle-Antibody Bioconjugates. ACS Appl. Nano Mater. 2019, 2, 4150–4158. [Google Scholar] [CrossRef]
- Arcas, A.D.S.; Dutra, F.D.S.; Allil, R.; Werneck, M.M. Surface Plasmon Resonance and Bending Loss-Based U-Shaped Plastic Optical Fiber Biosensors. Sensors 2018, 18, 648. [Google Scholar] [CrossRef]
- Kaushik, S.; Tiwari, U.K.; Pal, S.S.; Sinha, R.K. Rapid detection of Escherichia coli using fiber optic surface plasmon resonance immunosensor based on biofunctionalized Molybdenum disulfide (MoS2) nanosheets. Biosens. Bioelectron. 2019, 126, 501–509. [Google Scholar] [CrossRef]
- Mulcahy, L.A.; Pink, R.C.; Carter, D.R. Routes and mechanisms of extracellular vesicle uptake. J. Extracell Vesicles 2014, 3, 24641. [Google Scholar] [CrossRef]
- Witwer, K.W.; Buzas, E.I.; Bemis, L.T.; Bora, A.; Lasser, C.; Lotvall, J.; Nolte-’t Hoen, E.N.; Piper, M.G.; Sivaraman, S.; Skog, J.; et al. Standardization of sample collection, isolation and analysis methods in extracellular vesicle research. J. Extracell Vesicles 2013, 2, 20360. [Google Scholar] [CrossRef]
- Wiklander, O.P.; Nordin, J.Z.; O’Loughlin, A.; Gustafsson, Y.; Corso, G.; Mäger, I.; Vader, P.; Lee, Y.; Sork, H.; Seow, Y. Extracellular vesicle in vivo biodistribution is determined by cell source, route of administration and targeting. J. Extracell Vesicles 2015, 4, 26316. [Google Scholar] [CrossRef]
- Bu, J.; Shim, J.E.; Lee, T.H.; Cho, Y.H. Multi-modal liquid biopsy platform for cancer screening: screening both cancer-associated rare cells and cancer cell-derived vesicles on the fabric filters for a reliable liquid biopsy analysis. Nano Converg. 2019, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, S.; Li, L.; Li, M.; Guo, C.; Yao, J.; Mi, S. Exosome and exosomal microRNA: trafficking, sorting, and function. Genomics Proteomics Bioinformatics 2015, 13, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Théry, C.; Zitvogel, L.; Amigorena, S. Exosomes: composition, biogenesis and function. Nat. Rev. Immunol. 2002, 2, 569. [Google Scholar] [CrossRef] [PubMed]
- Alderton, G.K. Exosomes drive premetastatic niche formation. Nat. Rev. Cancer 2012, 12, 447. [Google Scholar] [CrossRef] [PubMed]
- Azmi, A.S.; Bao, B.; Sarkar, F.H. Exosomes in cancer development, metastasis, and drug resistance: a comprehensive review. Cancer Metastasis Rev. 2013, 32, 623–642. [Google Scholar] [CrossRef] [PubMed]
- Brinton, L.T.; Sloane, H.S.; Kester, M.; Kelly, K.A. Formation and role of exosomes in cancer. Cell Mol. Life Sci. 2015, 72, 659–671. [Google Scholar] [CrossRef]
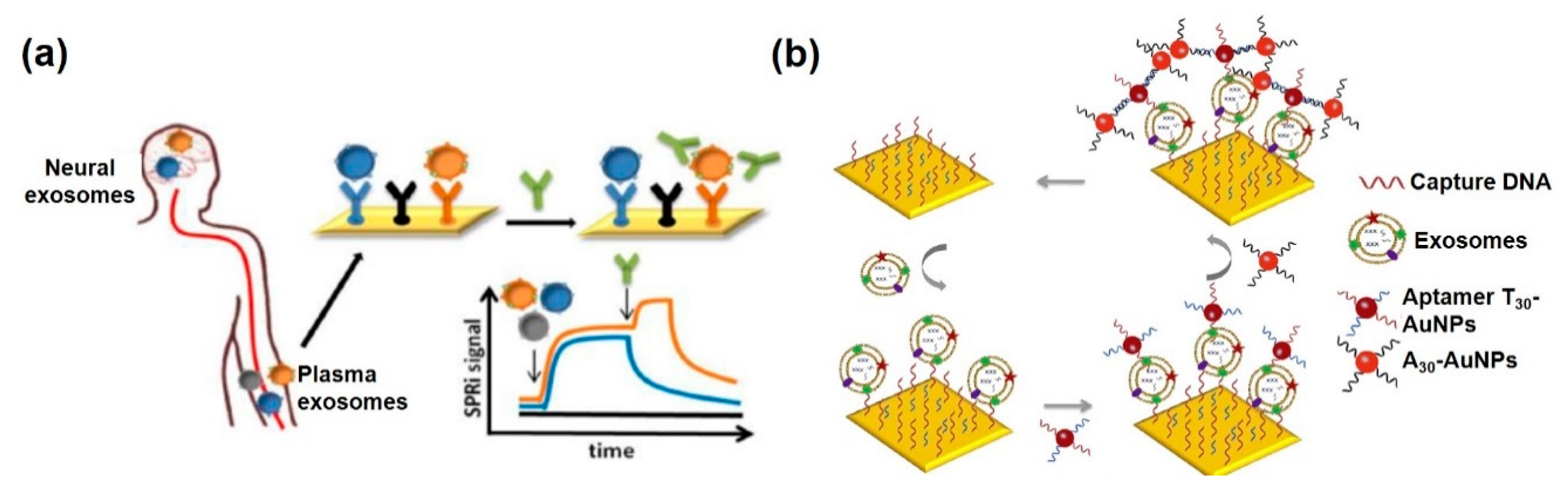
- Picciolini, S.; Gualerzi, A.; Vanna, R.; Sguassero, A.; Gramatica, F.; Bedoni, M.; Masserini, M.; Morasso, C. Detection and Characterization of Different Brain-Derived Subpopulations of Plasma Exosomes by Surface Plasmon Resonance Imaging. Anal. Chem 2018, 90, 8873–8880. [Google Scholar] [CrossRef]
- Sina, A.A.I.; Vaidyanathan, R.; Wuethrich, A.; Carrascosa, L.G.; Trau, M. Label-free detection of exosomes using a surface plasmon resonance biosensor. Anal. Bioanal. Chem. 2019, 411, 1311–1318. [Google Scholar] [CrossRef]
- Wang, Q.; Zou, L.; Yang, X.; Liu, X.; Nie, W.; Zheng, Y.; Cheng, Q.; Wang, K. Direct quantification of cancerous exosomes via surface plasmon resonance with dual gold nanoparticle-assisted signal amplification. Biosens. Bioelectron. 2019, 135, 129–136. [Google Scholar] [CrossRef]
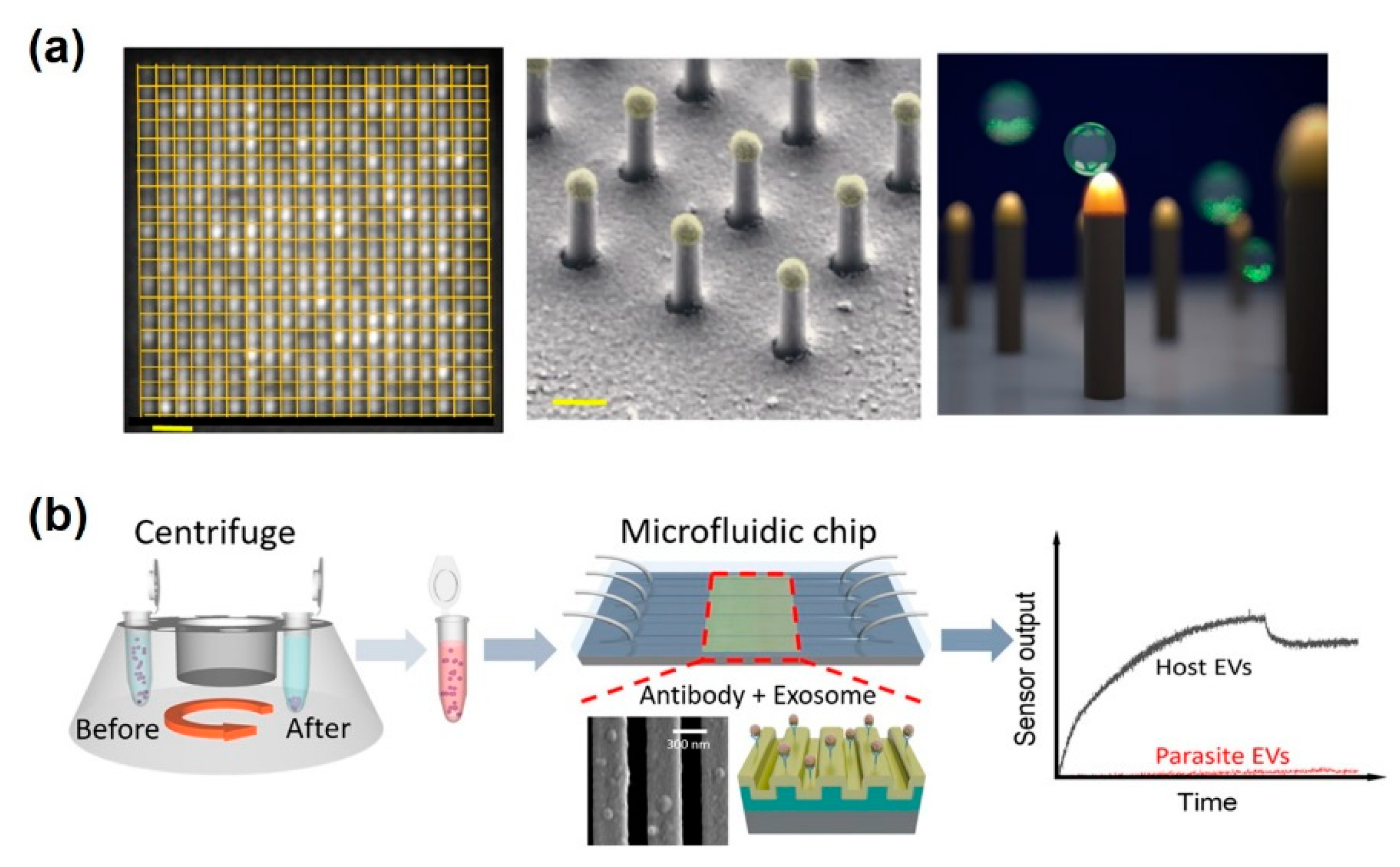
- Im, H.; Shao, H.; Park, Y.I.; Peterson, V.M.; Castro, C.M.; Weissleder, R.; Lee, H. Label-free detection and molecular profiling of exosomes with a nano-plasmonic sensor. Nat. Biotechnol 2014, 32, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Thakur, A.; Qiu, G.; Ng, S.P.; Guan, J.; Yue, J.; Lee, Y.; Wu, C.L. Direct detection of two different tumor-derived extracellular vesicles by SAM-AuNIs LSPR biosensor. Biosens. Bioelectron. 2017, 94, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Bathini, S.; Raju, D.; Badilescu, S.; Kumar, A.; Ouellette, R.J.; Ghosh, A.; Packirisamy, M. Nano-Bio Interactions of Extracellular Vesicles with Gold Nanoislands for Early Cancer Diagnosis. Research (Wash D C) 2018, 2018, 3917986. [Google Scholar] [CrossRef] [PubMed]
- Raghu, D.; Christodoulides, J.A.; Christophersen, M.; Liu, J.L.; Anderson, G.P.; Robitaille, M.; Byers, J.M.; Raphael, M.P. Nanoplasmonic pillars engineered for single exosome detection. PLoS ONE 2018, 13, e0202773. [Google Scholar] [CrossRef]
- Wang, Y.F.; Yuan, W.; Kimber, M.; Lu, M.; Dong, L. Rapid Differentiation of Host and Parasitic Exosome Vesicles Using Microfluidic Photonic Crystal Biosensor. Acs Sens. 2018, 3, 1616–1621. [Google Scholar] [CrossRef]
- Kotlarek, D.; Vorobii, M.; Ogieglo, W.; Knoll, W.; Rodriguez-Emmenegger, C.; Dostalek, J. Compact Grating-Coupled Biosensor for the Analysis of Thrombin. ACS Sens. 2019, 4, 2109–2116. [Google Scholar] [CrossRef]
- Cong, S.; Yuan, Y.; Chen, Z.; Hou, J.; Yang, M.; Su, Y.; Zhang, Y.; Li, L.; Li, Q.; Geng, F.; et al. Noble metal-comparable SERS enhancement from semiconducting metal oxides by making oxygen vacancies. Nat. Commun. 2015, 6, 7800. [Google Scholar] [CrossRef]
- Choi, J.H.; El-Said, W.A.; Choi, J.-W. Highly sensitive surface-enhanced Raman spectroscopy (SERS) platform using core/double shell (Ag/polymer/Ag) nanohorn for proteolytic biosensor. Appl. Surf. Sci. 2019, 144669. [Google Scholar] [CrossRef]
- El-Said, W.A.; Yoon, J.; Choi, J.W. Nanostructured surfaces for analysis of anticancer drug and cell diagnosis based on electrochemical and SERS tools. Nano Converg. 2018, 5, 11. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, J.H.; Chueng, S.D.; Pongkulapa, T.; Yang, L.; Cho, H.Y.; Choi, J.W.; Lee, K.B. Nondestructive Characterization of Stem Cell Neurogenesis by a Magneto-Plasmonic Nanomaterial-Based Exosomal miRNA Detection. ACS Nano 2019, 13, 8793–8803. [Google Scholar] [CrossRef]
- Mohammadi, S.; Salimi, A.; Hamd-Ghadareh, S.; Fathi, F.; Soleimani, F. A FRET immunosensor for sensitive detection of CA 15-3 tumor marker in human serum sample and breast cancer cells using antibody functionalized luminescent carbon-dots and AuNPs-dendrimer aptamer as donor-acceptor pair. Anal. Biochem. 2018, 557, 18–26. [Google Scholar] [CrossRef] [PubMed]

| Method | Working Principle | Target | Correlation Range | Detection Limit | Ref |
|---|---|---|---|---|---|
| PSPR | Site-directed antibody immobilization based on protein A/G | C-reactive protein (CRP) | 1.2~80 ng/mL | 1.2 ng/mL | [27] |
| Antibody immobilization based on EDC/NHS coulping | metalloproteinases-9 (MMP-9) | 10~200 ng/mL | 8 pg/mL | [28] | |
| Site-directed antibody immobilization based on protein G | human growth hormone (hGH) | 66.4~199 ng/mL * | 21.9 ng/mL * | [29] | |
| Sandwich assay based on AuNP-antibody conjugate | Carcinoembryonic Antigen (CEA) | 0~2.5 ng/mL | 17.8 pg/mL | [32] | |
| Sandwich assay based on MWCNT-antibody conjugate | Tau Protein | 9.87~78.9 ng/mL * | 9.87 ng/mL * | [30] | |
| Sandwich assay based on AuNP-antibody conjugate | Cardiac troponin T (cTnT) | 0.5~40 ng/mL | 0.5 ng/mL | [33] | |
| LSPR | nanorods (GNR) functionalized with poly (N-isopropylacrylamide) (PNIPAAM) | Troponin-T (TnT) | 7.6~9.1 × 1011 fg/mL | 8.4 fg/mL | [34] |
| LSPR band shift based on interparticle crosslinking | Staphylococcal enterotoxin A (SEA) | 0~250 ng/mL | 5 ng/mL | [35] | |
| Core/shell nanoparticle Au@AgNPs and Ag@AuNPs | Staphylococcal enterotoxin A (SEA) | 0~500 ng/mL | 5.4 ng/mL | [36] | |
| Single AuNP | α-fetoprotein (AFP) | 69~6.9 × 107 fg/mL * | 6.28 pg/mL * | [37] | |
| Single AuNP | Carcinoembryonic antigen (CEA) | 180~1.8 × 108 fg/mL * | 16.9 pg/mL * | [37] | |
| Single AuNP | Prostate specific antigen (PSA) | 28.4~2.84 × 106 fg/mL * | 284 fg/mL * | [37] | |
| Au/Ag Bimetallic nanostructures modified with polydopamine films | Bovine serum albumin (BSA) | 0.01~100 ng/mL | 0.01 ng/mL | [38] | |
| LSPR band shift based on the GNR etching resulted by TMB reaction | Carcinoembryonic antigen (CEA) | 0~60 ng/mL | 2.5 ng/mL | [39] | |
| LSPR band shift based on the GNR etching resulted by TMB reaction | Prostate specific antigen (PSA) | 0~1275 pg/mL | 75 pg/mL | [39] |
| Method | Working Principle | Target | Correlation Range | Detection Limit | Ref |
|---|---|---|---|---|---|
| PSPR | Generation of new antibody | Avian Influenza A H7N9 Virus | 2.3 × 102~2.3 × 105 copies/mL | 402 copies/mL | [47] |
| Antibody immobilization based on neutravidin-biotin | Dengue Virus Serotype 2 & 3 | Not stated | 2 × 104 particles/mL | [49] | |
| LSPR | Electrochemically deposited AuNPs | Human immunodeficiency Virus | 0~200 pg/mL | 25 pg/mL | [51] |
| hetero-assembled AuNP based on sandwich-immunoassay | Hepatitis B surface antigen | 200~1.25 × 105 fg/mL | 200 fg/mL | [52] | |
| Tilted fiber grating coated with AuNP | Newcastle disease virus | 100~1 × 106 fg/mL | 100 fg/mL | [50] |
| Method | Working Principle | Target | Correlation Range (CFU/mL) | Detection Limit (CFU/mL) | Ref |
|---|---|---|---|---|---|
| PSPR | Immobilization of antibody against recombinant outer membrane protein (anti-OmpW) of Vibrio cholerae on Au chip | Vibrio Cholerae | 101–105 | 10 | [65] |
| Functionalization of plasma polymers (PPs) on Au surface for a stable immobilization of antibodies | Salmonella Typhimurium | 105–108 | 105 | [66] | |
| Immobilization of antibody using microarray spotter and flowed the samples on the Au chip | Salmonella Typhimurium | 5.14 × 106–5.14 × 108 | 2.1 × 106 | [67] | |
| Detection of unbounded anti-Campylobacter Jejuni by the anti-rabbit IgG on Au chip | Campylobacter Jejuni | 5–5 × 107 | 131 ± 4 | [68] | |
| Measurement of precipitated 4-chloro-1-naphthol by the HRP-tagged anti-Salmonella | Salmonella Typhimurium | 102–106 | 102 | [69] | |
| Light escaping from optic fiber due to immunocapture of Escherichia coli | Escherichia coli O157:H7 | Not stated | 1.5 × 103 | [73] | |
| Functionalization of MoS2 nanosheet and anti- Escherichia coli on Au-coated optical fiber | Escherichia coli O157:H7 | 1 × 104–8 × 104 | 94 | [74] | |
| LSPR | Color change by the tyramine-functionalized Au nanoparticles and catalases-functionalized polystyrene beads, immobilized by Escherichia coli | Escherichia coli O157:H7 | 5 × 101–5 × 104 | 50 | [71] |
| Method | Working Principle | Target | Correlation Range | Detection Limit | Ref |
|---|---|---|---|---|---|
| PSPR | Immobilization of spotted anti-CD81 and -GM1 on Au chip | Exosomes from diverse neuronal cells | 1–10 µg/mL | Not stated | [84] |
| Immobilization of anti-HER2 on Au chip for detection of breast cancer-derived exosome | Breast cancer–derived exosomes | 0.83–3.31 × 107/mL | 0.83 × 107/mL | [85] | |
| LSPR | Functionalization of PEG and anti-CD63 on periodic Au nanohole | Ovarian cancer–derived exosomes | 4.03 × 105–1.32 × 109/mL | 4.03 × 105/mL | [87] |
| Immobilized anti-CD9 on self-assembly Au islands for exosome detection | Exosomes from A-549 and SH-SY5Y cells | 0.194–100 μg/mL | 0.194 μg/mL | [88] | |
| Venceremin-functionalized Au nanoparticles on Au islands for capture the exosomes | Breast cancer-derived exosomes | Not stated | 9 /μm2 | [89] | |
| Functionalization of anti-CD63 on nanopillar array | Breast cancer–derived exosomes | Not stated | 1 × 105/mL | [90] | |
| Line shaped-Au nanopatterns with immobilization of anti-CD63 | Murine macrophage–derived exosomes | 2 × 109–2 × 1011/mL | 2.18 × 109/mL | [91] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.-H.; Lee, J.-H.; Son, J.; Choi, J.-W. Noble Metal-Assisted Surface Plasmon Resonance Immunosensors. Sensors 2020, 20, 1003. https://doi.org/10.3390/s20041003
Choi J-H, Lee J-H, Son J, Choi J-W. Noble Metal-Assisted Surface Plasmon Resonance Immunosensors. Sensors. 2020; 20(4):1003. https://doi.org/10.3390/s20041003
Chicago/Turabian StyleChoi, Jin-Ha, Jin-Ho Lee, Joohyung Son, and Jeong-Woo Choi. 2020. "Noble Metal-Assisted Surface Plasmon Resonance Immunosensors" Sensors 20, no. 4: 1003. https://doi.org/10.3390/s20041003
APA StyleChoi, J.-H., Lee, J.-H., Son, J., & Choi, J.-W. (2020). Noble Metal-Assisted Surface Plasmon Resonance Immunosensors. Sensors, 20(4), 1003. https://doi.org/10.3390/s20041003







