Percentiles and Reference Values for the Accelerometric Assessment of Static Balance in Women Aged 50–80 Years
Abstract
1. Introduction
2. Materials and Methods
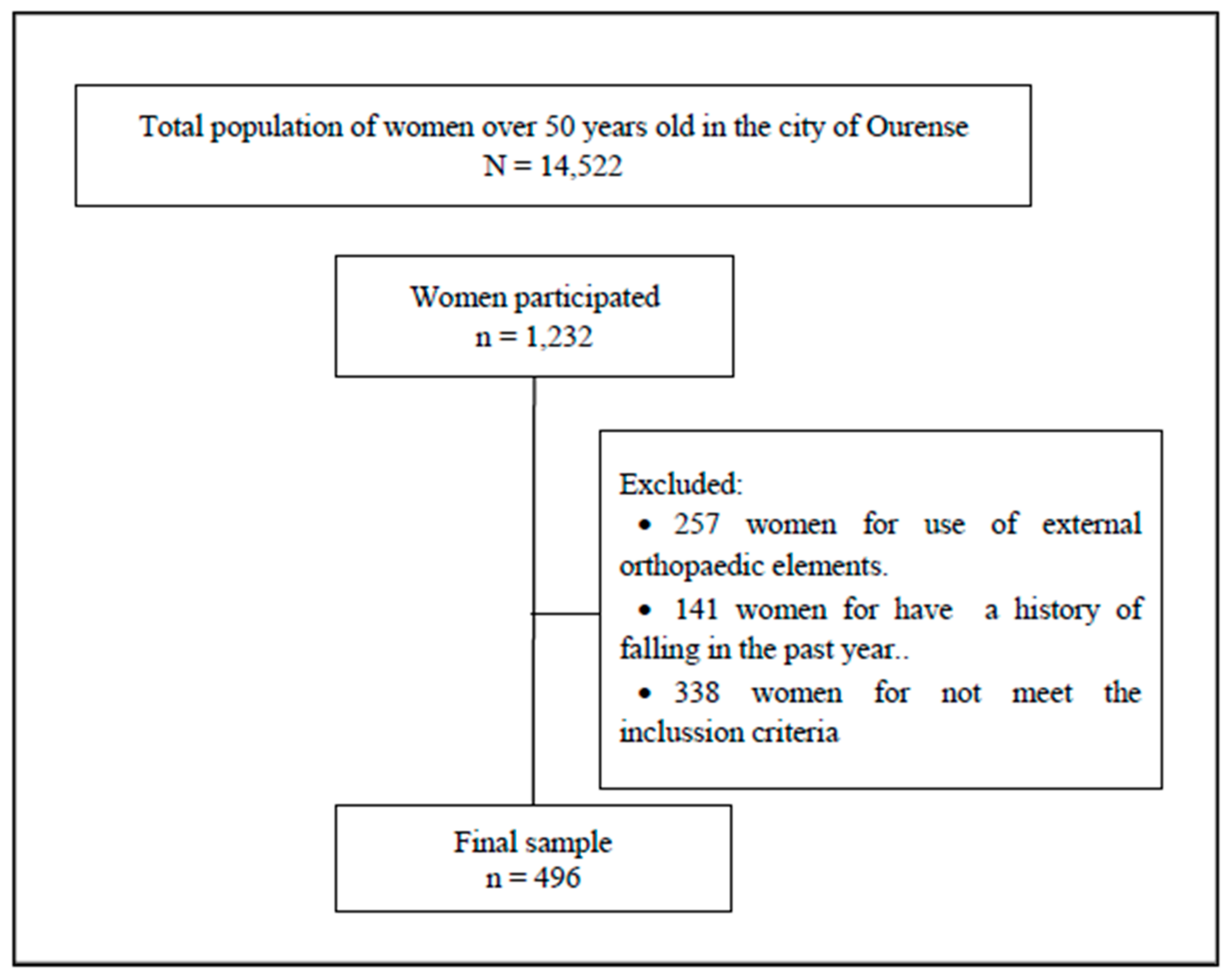
2.1. Sample
2.2. Procedure
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bischoff-Ferrari, H.; Orav, J.; Kanis, J.; Rizzoli, R.; Schlögl, M.; Staehelin, H.; Willett, W.C.; Dawson-Hughes, B. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporosis Int. 2015, 26, 2793–2802. [Google Scholar] [CrossRef] [PubMed]
- Tromp, A.; Pluijm, S.; Smit, J.; Deeg, D.; Bouter, L.; Lips, P. Fall-risk screening test: A prospective study on predictors for falls in community-dwelling elderly. J. Clin. Epidemiol. 2001, 54, 837–844. [Google Scholar] [CrossRef]
- Sterling, D.A.; O’Connor, J.A.; Bonadies, J. Geriatric falls: Injury severity is high and disproportionate to mechanism. J. Trauma. 2001, 50, 116–119. [Google Scholar] [CrossRef]
- Finlayson, M.L.; Peterson, E.W. Falls, aging, and disability. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 357–373. [Google Scholar] [CrossRef] [PubMed]
- Maki, B.E.; Sibley, K.M.; Jaglal, S.B.; Bayley, M.; Brooks, D.; Fernie, G.R.; Flint, A.J.; Gage, W.; Liu, B.A.; McIlroy, W.E.; et al. Reducing fall risk by improving balance control: Development, evaluation and knowledge-translation of new approaches. J. Safety Res. 2011, 42, 473–485. [Google Scholar] [CrossRef]
- Turner, A.J.; Chander, H.; Knight, A.C. Falls in geriatric populations and hydrotherapy as an intervention: A brief review. Geriatrics. 2018, 3, 71. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet. 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Mapelli, A.; Zago, M.; Fusini, L.; Galante, D.; Colombo, A.; Sforza, C. Validation of a protocol for the estimation of three-dimensional body center of mass kinematics in sport. Gait Posture 2014, 39, 460–465. [Google Scholar] [CrossRef]
- Hodges, P.; Gurfinkel, V.; Brumagne, S.; Smith, T.; Cordo, P. Coexistence of stability and mobility in postural control: Evidence from postural compensation for respiration. Exp. Brain Res. 2002, 144, 293–302. [Google Scholar] [CrossRef]
- Chen, T.; Chou, L. Altered center of mass control during sit-to-walk in elderly adults with and without history of falling. Gait Posture 2013, 38, 696–701. [Google Scholar] [CrossRef]
- Winter, D.A. Human balance and posture control during standing and walking. Gait Posture 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35, ii7–ii11. [Google Scholar] [CrossRef] [PubMed]
- McIlroy, W.E.; Maki, B.E. Age-related changes in compensatory stepping in response to unpredictable perturbations. J. Gerontol. A Biol. Sci. Med. Sci. 1996, 51, M289–M296. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Hsu, Y. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors 2010, 10, 7772–7788. [Google Scholar] [CrossRef]
- Turcot, K.; Allet, L.; Golay, A.; Hoffmeyer, P.; Armand, S. Investigation of standing balance in diabetic patients with and without peripheral neuropathy using accelerometers. Clin. Biomech. 2009, 24, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Goble, D.J.; Baweja, H.S. Normative data for the BTrackS balance test of postural sway: Results from 16,357 community-dwelling individuals who were 5 to 100 years old. Phys. Ther. 2018, 98, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Dabbs, N.C.; MacDonald, C.J.; Chander, H.; Lamont, H.S.; Garner, J.C. The effect of whole-body vibration on balance in elderly women. Med. Sport. 2014, 18, 10–15. [Google Scholar] [CrossRef]
- Shany, T.; Redmond, S.J.; Narayanan, M.R.; Lovell, N.H. Sensors-based wearable systems for monitoring of human movement and falls. IEEE Sens. J. 2012, 12, 658–670. [Google Scholar] [CrossRef]
- Mathie, M.J.; Coster, A.C.; Lovell, N.H.; Celler, B.G. Accelerometry: Providing an integrated, practical method for long-term, ambulatory monitoring of human movement. Physiol. Meas. 2004, 25, R1–R20. [Google Scholar] [CrossRef]
- Preece, S.J.; Goulermas, J.Y.; Kenney, L.P.; Howard, D.; Meijer, K.; Crompton, R. Activity identification using body-mounted sensors—A review of classification techniques. Physiol. Meas. 2009, 30, R1–R33. [Google Scholar] [CrossRef]
- Taraldsen, K.; Chastin, S.F.; Riphagen, I.I.; Vereijken, B.; Helbostad, J.L. Physical activity monitoring by use of accelerometer-based body-worn sensors in older adults: A systematic literature review of current knowledge and applications. Maturitas 2012, 71, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Leirós-Rodríguez, R.; Arce-Fariña, M.E.; Míguez-Álvarez, C.; García-Soidán, J. Definition of the proper placement point for balance assessment with accelerometers in older women. Rev. Andal. Med. Deport 2016, in press. [Google Scholar] [CrossRef]
- Leirós-Rodríguez, R.; Romo-Pérez, V.; Arce-Fariña, M.E.; García-Soidán, J.L. Associations between body composition and movements during gait in women. Rev. Int. Med. Cienc. Act. Fís. Deporte 2018, 18, 693–707. [Google Scholar] [CrossRef][Green Version]
- Leirós-Rodríguez, R.; Romo-Pérez, V.; García-Soidán, J.L. Validity and reliability of a tool for accelerometric assessment of static balance in women. Eur. J. Physiother. 2017, 19, 243–248. [Google Scholar] [CrossRef]
- Bouten, C.V.; Koekkoek, K.T.; Verduin, M.; Kodde, R.; Janssen, J.D. A triaxial accelerometer and portable data processing unit for the assessment of daily physical activity. IEEE Trans. Biomed. Eng. 1997, 44, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Preece, S.J.; Goulermas, J.Y.; Kenney, L.P.; Howard, D. A comparison of feature extraction methods for the classification of dynamic activities from accelerometer data. IEEE Trans. Biomed. Eng. 2009, 56, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, A.; Luzi, S.; Murer, K.; de Bie, R.A.; de Bruin, E.D. Concurrent validity of a trunk tri-axial accelerometer system for gait analysis in older adults. Gait Posture 2009, 29, 444–448. [Google Scholar] [CrossRef]
- Borghi, E.; de Onis, M.; Garza, C.; van den Broeck, J.; Frongillo, E.; Grummer-Strawn, L.; van Buuren, S.; Pan, H.; Molinari, L.; Martorell, R.; et al. Construction of the World Health Organization child growth standards: Selection of methods for attained growth curves. Stat. Med. 2006, 25, 247–265. [Google Scholar] [CrossRef]
- Rigby, R.A.; Stasinopoulos, D.M. The GAMLSS project: A flexible approach to statistical modelling. In New Trends in Statistical Modelling: Proceedings of the 16th International Workshop on Statistical Modelling, 1st ed.; Klein, B., Korsholm, L., Eds.; Statistical Modelling Society: Odense, Denmark, 2001; pp. 337–345. [Google Scholar]
- Buuren, S.V.; Fredriks, M. Worm plot: A simple diagnostic device for modelling growth reference curves. Stat. Med. 2001, 20, 1259–1277. [Google Scholar] [CrossRef]
- Cabañero-Martínez, M.J.; Cabrero-García, J.; Richart-Martínez, M.; Muñoz-Mendoza, C.L. Structured review of activities of daily living measures in older people. Rev. Esp. Geriatr. Gerontol. 2008, 43, 271–283. [Google Scholar] [CrossRef]
- González-Montalvo, J.I.; Alarcón-Alarcón, T. Quality of functional evaluation instruments in geriatrics: From the invention of the wheel to the electronic age. Rev. Esp. Geriatr. Gerontol. 2008, 43, 265–267. [Google Scholar] [CrossRef] [PubMed]
- Lowry, K.; Lokenvitz, N.; Smiley-Oyen, A. Age-and speed-related differences in harmonic ratios during walking. Gait Posture 2012, 35, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Senden, R.; Savelberg, H.; Grimm, B.; Heyligers, I.; Meijer, K. Accelerometry-based gait analysis, an additional objective approach to screen subjects at risk for falling. Gait Posture 2012, 36, 296–300. [Google Scholar] [CrossRef]
- Lin, M.; Hwang, H.; Hu, M.; Wu, H.I.; Wang, Y.; Huang, F. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J. Am. Geriatr. Soc. 2004, 52, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.G.; Dingwell, J.B. Dynamic stability of superior vs. inferior segments during walking in young and older adults. Gait Posture 2009, 30, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Thiede, R.; Toosizadeh, N.; Mills, J.L.; Zaky, M.; Mohler, J.; Najafi, B. Gait and balance assessments as early indicators of frailty in patients with known peripheral artery disease. Clin. Biomech. 2015, 32, 1–7. [Google Scholar] [CrossRef]
- Helbostad, J.L.; Askim, T.; Moe-Nilssen, R. Short-term repeatability of body sway during quiet standing in people with hemiparesis and in frail older adults. Arch. Phys. Med. Rehabil. 2004, 85, 993–999. [Google Scholar] [CrossRef]
- Moe-Nilssen, R. A new method for evaluating motor control in gait under real-life environmental conditions. Parts I & II: The instrument & gait analysis. Clin. Biomech. 1998, 13, 320–335. [Google Scholar] [CrossRef]
| Age Group | N | Age (years) | Weight (kg) | Height (cm) | Body Mass Index (kg/m2) |
|---|---|---|---|---|---|
| All | 496 | 68.8 ± 10.4 | 65.6 ±10.1 | 153.9 ± 5.4 | 27.6 ± 4.1 |
| G1 (51–55 years) | 87 | 53.4 ± 4.4 | 63 ± 7.6 | 155.6 ± 5 | 26 ± 3.3 |
| G2 (56–60 years) | 72 | 57.4 ± 4.3 | 64 ± 6.5 | 154.6 ± 6 | 26.8 ± 5.3 |
| G3 (61–65 years) | 85 | 64.2 ± 2.7 | 66.4 ± 11.1 | 154 ± 5.5 | 28 ± 4.7 |
| G4 (66–70 years) | 92 | 68.4 ± 3.8 | 63.8 ± 9.6 | 152.9 ± 6.1 | 29 ± 6.3 |
| G5 (71–75 years) | 87 | 74.2 ± 4.6 | 66.5 ± 10.1 | 151.8 ± 5.2 | 28.3 ± 3.2 |
| G6 (76–80 years) | 73 | 77.6 ± 2.2 | 68.1 ± 11.7 | 151.3 ± 4.2 | 29.2 ± 1.8 |
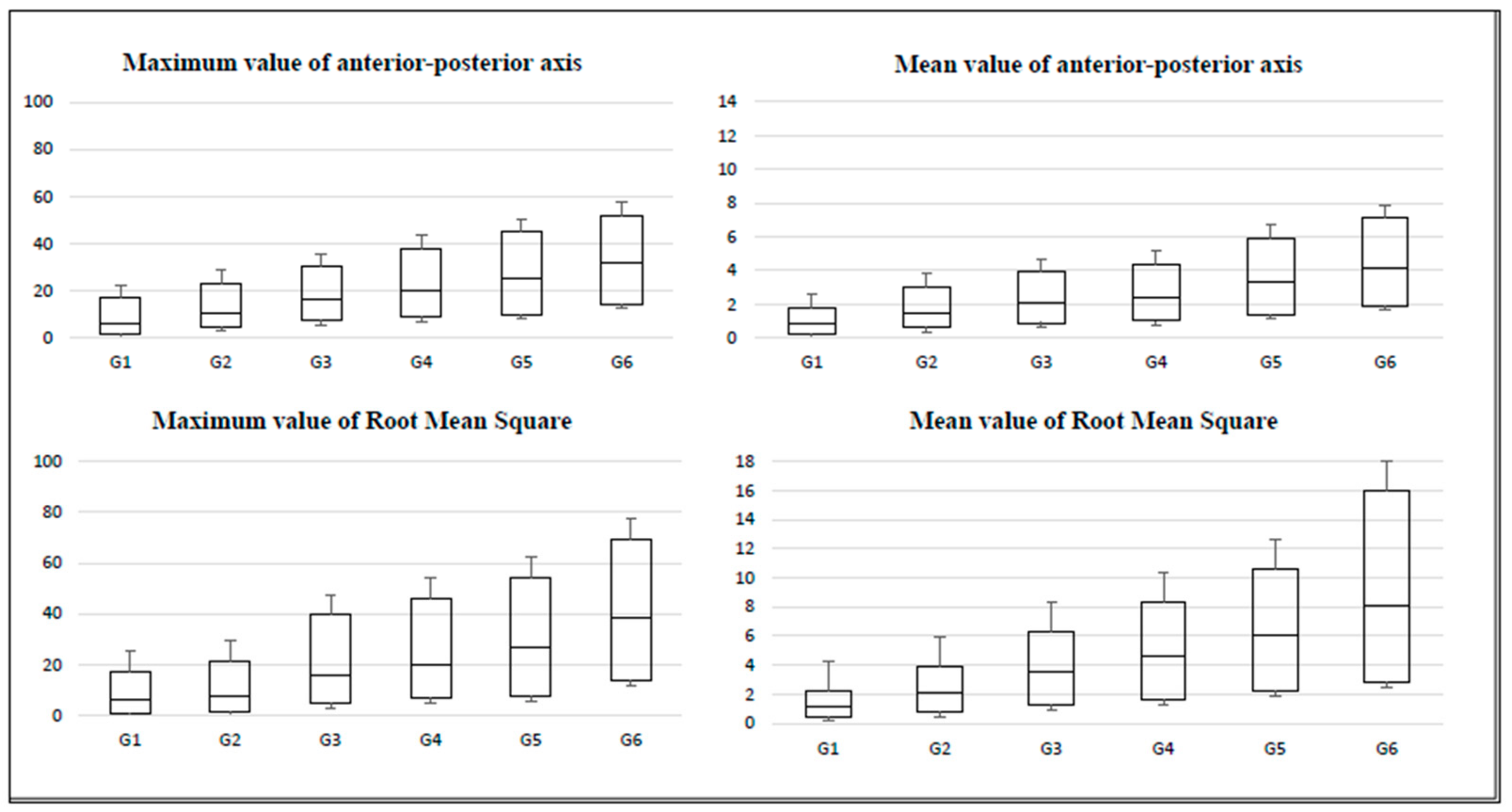
| Variable | G1 (n = 87) | G2 (n = 72) | G3 (n = 85) | G4 (n = 92) | G5 (n = 87) | G6 (n = 73) |
|---|---|---|---|---|---|---|
| Maximum value of anterior-posterior axis | ||||||
| Mean ± standard deviation | 4.4 ± 6 | 6.2 ± 8.7 | 8.5 ± 8.2 | 9.1 ± 9.1 | 13.7 ± 9.9 | 13.9 ± 9.5 |
| Kurtosis | 4.9 | 4.4 | 4.4 | 5.4 | 2.4 | 2.2 |
| Percentile 25 | 2 | 5 | 7.3 | 8.8 | 10.2 | 14.6 |
| Percentile 50 (median) | 4.2 | 5.7 | 9.5 | 11.6 | 15.2 | 17.5 |
| Percentile 75 | 11 | 12.7 | 13.5 | 17.6 | 19.8 | 20 |
| Interquartile range | 9 | 7.7 | 6.2 | 8.8 | 9.6 | 5.4 |
| Mean value of anterior-posterior axis | ||||||
| Mean ± standard deviation | 0.4 ± 0.8 | 0.5 ± 0.8 | 0.8 ± 1.1 | 1 ± 1.3 | 1.5 ± 1.2 | 1.8 ± 1.5 |
| Kurtosis | 13.4 | 5.7 | 14.9 | 5.2 | 3.6 | 2.2 |
| Percentile 25 | 0.2 | 0.6 | 0.9 | 1 | 1.4 | 1.9 |
| Percentile 50 (median) | 0.7 | 0.9 | 1.2 | 1.4 | 1.9 | 2.2 |
| Percentile 75 | 0.9 | 1.5 | 1.8 | 2 | 2.6 | 3 |
| Interquartile range | 0.7 | 0.9 | 0.9 | 1 | 1.2 | 1.1 |
| Maximum value of the Root Mean Square of accelerations | ||||||
| Mean ± standard deviation | 7.8 ± 9.5 | 9.6 ± 12.3 | 15.3 ± 12.9 | 16.8 ± 14.2 | 23 ± 15 | 25 ± 17.2 |
| Kurtosis | 4.1 | 5.4 | 2.5 | 3.4 | 3.6 | 2.3 |
| Percentile 25 | 0.8 | 1.3 | 4.8 | 7.1 | 7.6 | 13.6 |
| Percentile 50 (median) | 5.3 | 6.2 | 11.1 | 12.7 | 19.5 | 25.1 |
| Percentile 75 | 11.1 | 13.9 | 23.6 | 26.2 | 27.4 | 30.5 |
| Interquartile range | 10.3 | 12.6 | 18.8 | 19.1 | 19.8 | 16.9 |
| Mean value of the Root Mean Square of accelerations | ||||||
| Mean ± standard deviation | 0.9 ± 1.4 | 1 ± 1.7 | 1.8 ± 2.4 | 2.2 ± 2.7 | 3.1 ± 2.9 | 4.4 ± 3.2 |
| Kurtosis | 7.4 | 8.2 | 9.5 | 4.8 | 9.6 | 1.7 |
| Percentile 25 | 0.5 | 0.8 | 1.3 | 1.6 | 2.2 | 2.8 |
| Percentile 50 (median) | 0.7 | 1.3 | 2.2 | 3 | 3.9 | 5.3 |
| Percentile 75 | 1 | 1.8 | 2.8 | 3.7 | 4.5 | 7.9 |
| Interquartile range | 0.5 | 1 | 1.5 | 2.1 | 2.3 | 5.1 |
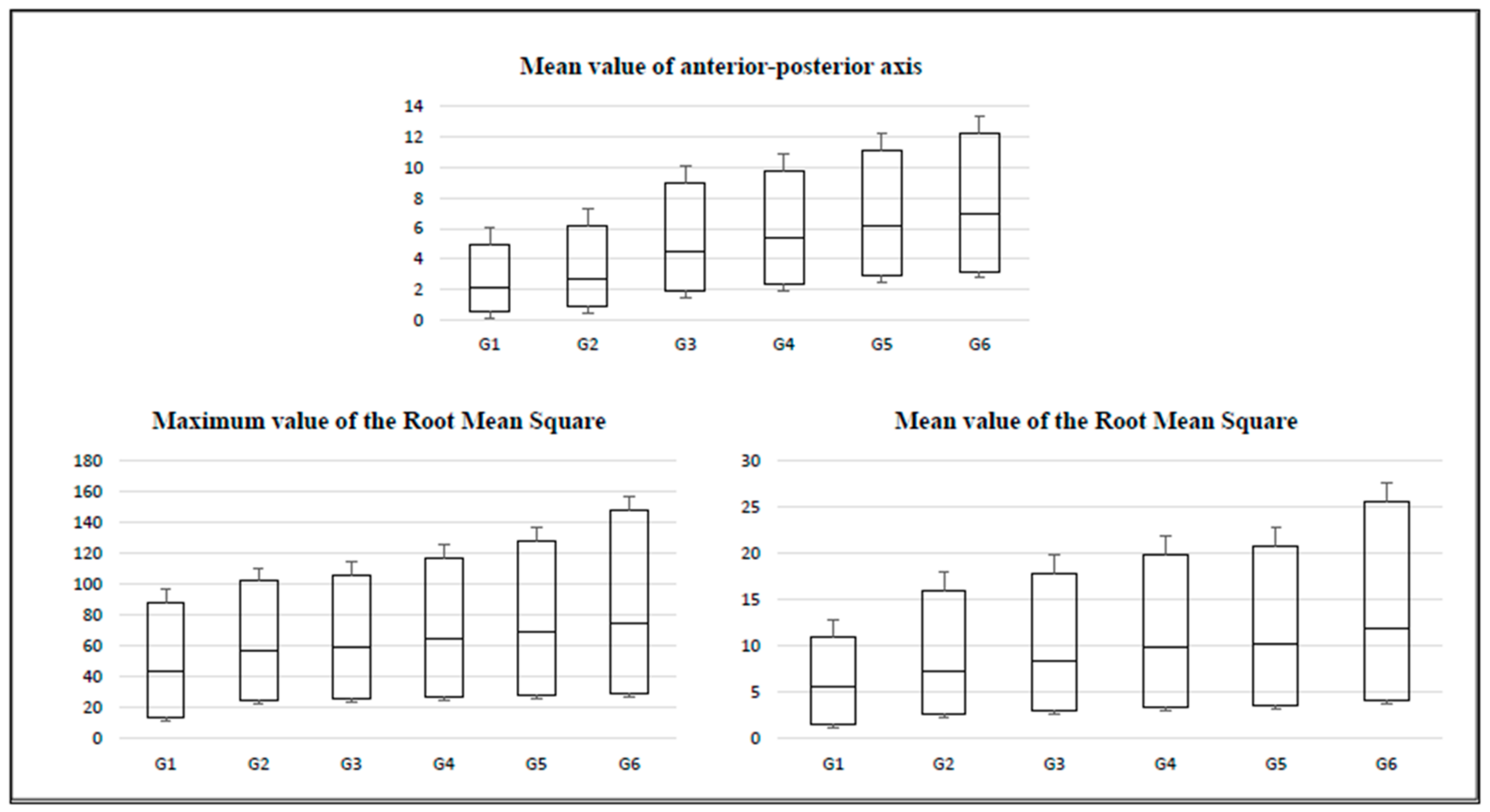
| Variable | G1 (n = 87) | G2 (n = 72) | G3 (n = 85) | G4 (n = 92) | G5 (n = 87) | G6 (n = 73) |
|---|---|---|---|---|---|---|
| Mean value of anterior-posterior axis | ||||||
| Mean ± standard deviation | 2.2 ± 2.5 | 2.6 ± 1.8 | 2.8 ± 1.4 | 2.9 ± 3.3 | 3.2 ± 2 | 4.4 ± 4 |
| Kurtosis | 10 | 5.1 | 3 | 2.9 | 4.5 | 2.5 |
| Percentile 25 | 0.6 | 0.9 | 1.9 | 2.4 | 2.9 | 3.2 |
| Percentile 50 (median) | 1.5 | 1.8 | 2.6 | 3 | 3.3 | 3.8 |
| Percentile 75 | 2.8 | 3.5 | 4.5 | 4.4 | 4.9 | 5.2 |
| Interquartile range | 2.2 | 2.6 | 2.6 | 2 | 2 | 2 |
| Maximum value of the Root Mean Square of accelerations | ||||||
| Mean ± standard deviation | 30.7 ± 18.9 | 36.7 ± 14.3 | 38.2 ± 23.2 | 38.7 ± 21.3 | 41.7 ± 17.8 | 52.6 ± 30 |
| Kurtosis | 1.8 | 2.9 | 2.7 | 5.2 | 2.4 | 2.1 |
| Percentile 25 | 14 | 24.8 | 25.7 | 26.7 | 27.7 | 29.5 |
| Percentile 50 (median) | 30.1 | 32.5 | 33.9 | 37.6 | 41 | 45.3 |
| Percentile 75 | 43.8 | 44.6 | 46.1 | 52.5 | 59 | 72.7 |
| Interquartile range | 29.8 | 19.8 | 20.4 | 25.8 | 31.3 | 43.2 |
| Mean value of the Root Mean Square of accelerations | ||||||
| Mean ± standard deviation | 4.5 ± 3.8 | 6.3 ± 4 | 6.4 ± 6.3 | 7.2 ± 4.6 | 7.4 ± 3.7 | 10.6 ± 12.1 |
| Kurtosis | 6.1 | 3.6 | 3 | 3 | 10.2 | 2 |
| Percentile 25 | 1.5 | 2.6 | 3.1 | 3.4 | 3.6 | 4.1 |
| Percentile 50 (median) | 4.1 | 4.7 | 5.3 | 6.5 | 6.7 | 7.8 |
| Percentile 75 | 5.3 | 8.7 | 9.4 | 10 | 10.4 | 13.6 |
| Interquartile range | 3.8 | 6.1 | 6.3 | 6.6 | 6.8 | 9.5 |
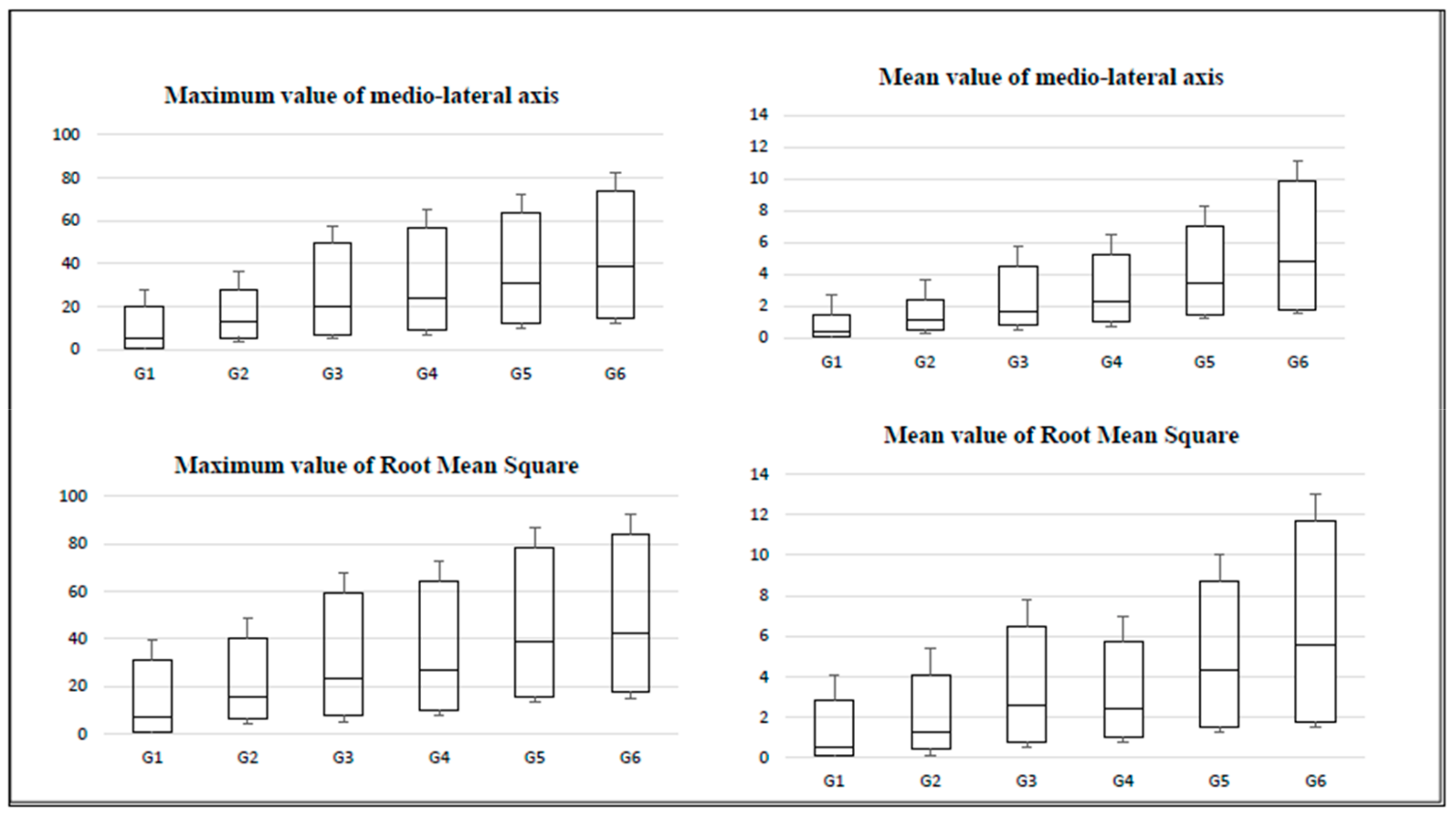
| Variable | G1 (n = 87) | G2 (n = 72) | G3 (n = 85) | G4 (n = 92) | G5 (n = 87) | G6 (n = 73) |
|---|---|---|---|---|---|---|
| Maximum value of medio-lateral axis | ||||||
| Mean ± standard deviation | 9.5 ± 11.6 | 12.6 ± 13.6 | 18 ± 16.4 | 18.2 ± 16.5 | 22.5 ± 15.7 | 22.6 ± 14.1 |
| Kurtosis | 3 | 3.3 | 5.3 | 2.5 | 6.2 | 1.8 |
| Percentile 25 | 0.4 | 5.7 | 7 | 9 | 12.2 | 14.3 |
| Percentile 50 (median) | 5 | 7 | 13 | 15 | 19 | 24.7 |
| Percentile 75 | 14.3 | 15.3 | 29.3 | 33 | 32.7 | 34.7 |
| Interquartile range | 13.9 | 9.6 | 22.3 | 24 | 20.5 | 20.4 |
| Mean value of medio-lateral axis | ||||||
| Mean ± standard deviation | 0.9 ± 1.3 | 1.2 ± 1.4 | 2 ± 2.4 | 2 ± 2.7 | 3 ± 3.8 | 2.9 ± 2.1 |
| Kurtosis | 4.1 | 3.5 | 5.9 | 6.3 | 12.5 | 1.6 |
| Percentile 25 | 0.1 | 0.5 | 0.8 | 1 | 1.5 | 1.8 |
| Percentile 50 (median) | 0.3 | 0.6 | 0.9 | 1.3 | 1.9 | 3 |
| Percentile 75 | 1 | 1.3 | 2.8 | 2.9 | 3.6 | 5.1 |
| Interquartile range | 0.9 | 0.8 | 2 | 1.9 | 2.1 | 3.3 |
| Maximum value of the Root Mean Square of accelerations | ||||||
| Mean ± standard deviation | 14.4 ± 15.7 | 16.9 ± 16.3 | 22.5 ± 19.7 | 22 ± 18.2 | 26.3 ± 16.3 | 29.2 ± 23.2 |
| Kurtosis | 1.9 | 2.6 | 4.7 | 2.5 | 9.6 | 2.1 |
| Percentile 25 | 0.4 | 6.4 | 7.7 | 10 | 15.7 | 17.4 |
| Percentile 50 (median) | 6.4 | 9.3 | 15.8 | 17 | 23.1 | 25.2 |
| Percentile 75 | 23.8 | 24.8 | 35.8 | 37.4 | 39.5 | 41.6 |
| Interquartile range | 23.4 | 18.4 | 28.1 | 27.4 | 23.8 | 24.2 |
| Mean value of the Root Mean Square of accelerations | ||||||
| Mean ± standard deviation | 1.4 ± 1.7 | 1.7 ± 1.8 | 2.8 ± 3 | 2.8 ± 3.5 | 3.8 ± 2.5 | 4.4 ± 6 |
| Kurtosis | 2.5 | 3.2 | 5 | 6.1 | 15.5 | 1.8 |
| Percentile 25 | 0.02 | 0.4 | 0.8 | 1 | 1.5 | 1.8 |
| Percentile 50 (median) | 0.4 | 0.9 | 1.8 | 1.4 | 2.8 | 3.8 |
| Percentile 75 | 2.3 | 2.8 | 3.9 | 3.3 | 4.4 | 6.1 |
| Interquartile range | 2.28 | 2.4 | 3.1 | 2.3 | 2.9 | 4.3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leirós-Rodríguez, R.; Romo-Pérez, V.; García-Soidán, J.L.; García-Liñeira, J. Percentiles and Reference Values for the Accelerometric Assessment of Static Balance in Women Aged 50–80 Years. Sensors 2020, 20, 940. https://doi.org/10.3390/s20030940
Leirós-Rodríguez R, Romo-Pérez V, García-Soidán JL, García-Liñeira J. Percentiles and Reference Values for the Accelerometric Assessment of Static Balance in Women Aged 50–80 Years. Sensors. 2020; 20(3):940. https://doi.org/10.3390/s20030940
Chicago/Turabian StyleLeirós-Rodríguez, Raquel, Vicente Romo-Pérez, Jose Luis García-Soidán, and Jesús García-Liñeira. 2020. "Percentiles and Reference Values for the Accelerometric Assessment of Static Balance in Women Aged 50–80 Years" Sensors 20, no. 3: 940. https://doi.org/10.3390/s20030940
APA StyleLeirós-Rodríguez, R., Romo-Pérez, V., García-Soidán, J. L., & García-Liñeira, J. (2020). Percentiles and Reference Values for the Accelerometric Assessment of Static Balance in Women Aged 50–80 Years. Sensors, 20(3), 940. https://doi.org/10.3390/s20030940








