Maximal Walking Distance in Persons with a Lower Limb Amputation
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Accelerometers
2.3. Protocol
2.4. Data Analysis and Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Participants
3.2. Maximal Number of Consecutive Steps and 10 MWT
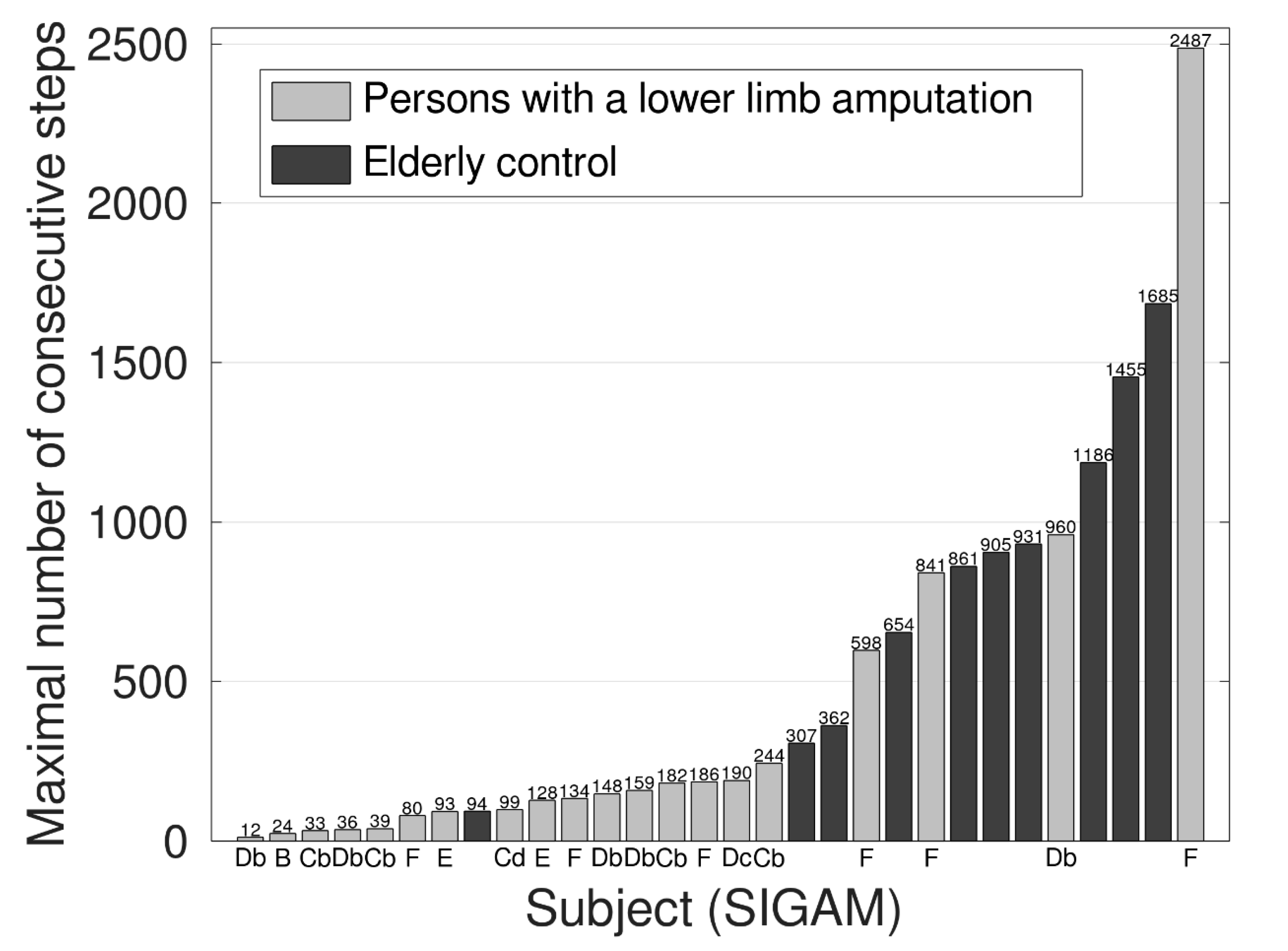
Maximal Number of Consecutive Steps per Individual
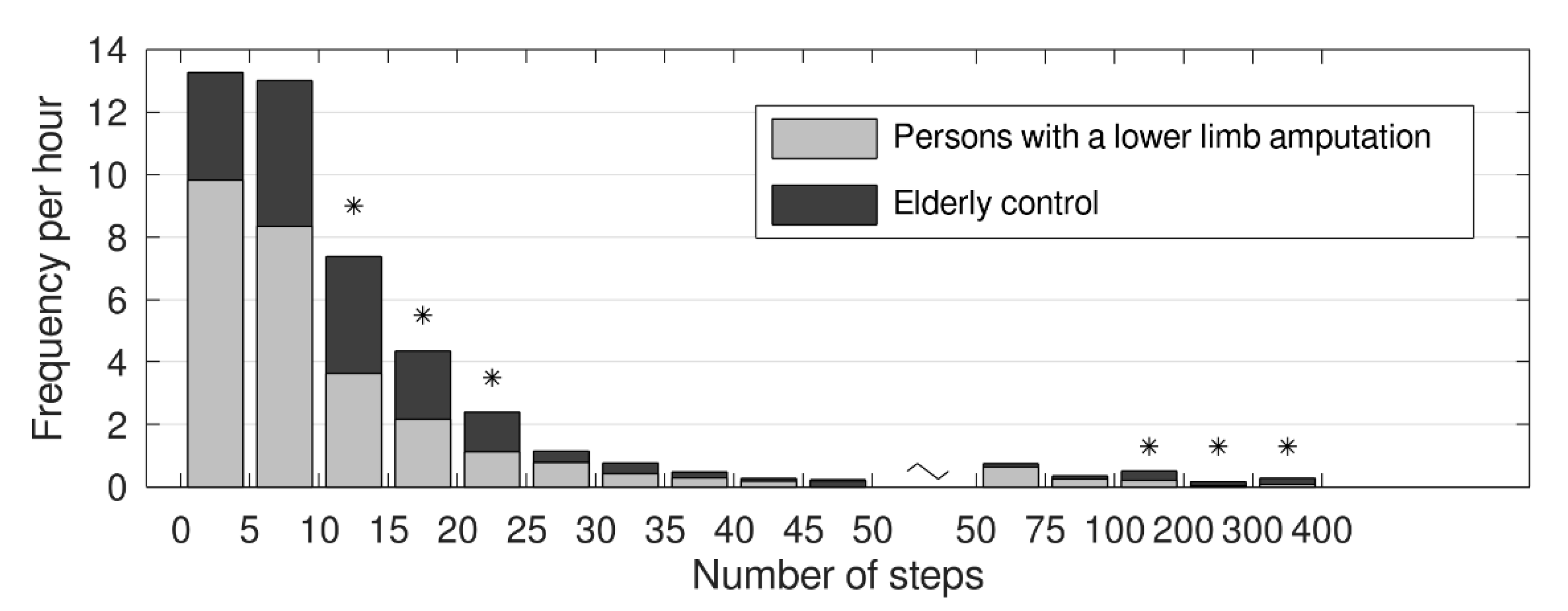
3.3. Frequency of Number of Steps per Hour
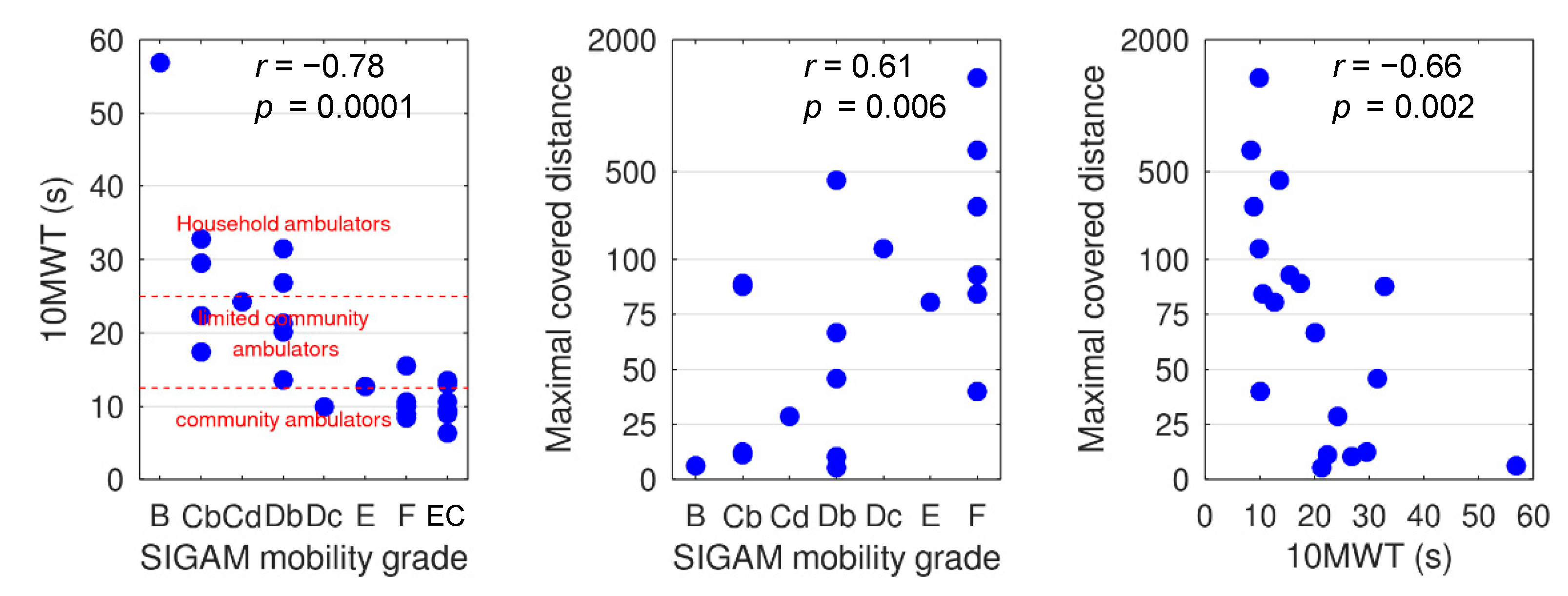
3.4. 10 MWT and Maximal Covered Walking Distance
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Legro, M.W.; Reiber, G.; del Aguila, M.; Ajax, M.J.; Boone, D.A.; Larsen, J.A.; Smith, D.G.; Sangeorzan, B. Issues of importance reported by persons with lower limb amputations and prostheses. J. Rehabil. Res. Dev. 1999, 36, 155–163. [Google Scholar]
- Christensen, B.; Ellegaard, B.; Bretler, U.; Ostrup, E.L. The effect of prosthetic rehabilitation in lower limb amputees. Prosthet. Orthot. Int. 1995, 19, 46–52. [Google Scholar] [CrossRef]
- Pell, J.P.; Donnan, P.T.; Fowkes, F.G.; Ruckley, C.V. Quality of life following lower limb amputation for peripheral arterial disease. Eur. J. Vasc. Surg. 1993, 7, 448–451. [Google Scholar] [CrossRef]
- Ryall, N.H.; Eyres, S.B.; Neumann, V.C.; Bhakta, B.B.; Tennant, A. The SIGAM mobility grades: A new population-specific measure for lower limb amputees. Disabil. Rehabil. 2003, 25, 833–844. [Google Scholar] [CrossRef]
- Pohjolainen, T.; Alaranta, H.W. Primary survival and prosthetic fitting of lower limb amputees. J. Prosthet. Orthot. Int. 1989, 13, 63–69. [Google Scholar] [CrossRef]
- Inderbitzi, R.; Buettiker, M.; Enzler, M. The long-term mobility and mortality of patients with peripheral arterial disease following bilateral amputation. Eur. J. Vasc. Endovasc. Surg. 2003, 26, 59–64. [Google Scholar] [CrossRef]
- Klesges, R.C.; Eck, L.H.; Mellon, M.W.; Fulliton, W.; Somes, G.W.; Hanson, C.L. The accuracy of self-reports of physical activity. Med. Sci. Sports Exerc. 1990, 22, 690–697. [Google Scholar] [CrossRef]
- Lagerros, Y.T.; Lagiou, P. Assessment of physical activity and energy expenditure in epidemiological research of chronic diseases. Eur. J. Epidemiol. 2007, 22, 353–362. [Google Scholar] [CrossRef]
- Cuperus, N.; Hoogeboom, T.J.; Neijland, Y.; van den Ende, C.H.; Keijsers, N.L. Are people with rheumatoid arthritis who undertake activity pacing at risk of being too physically inactive? Clin. Rehabil. 2012, 26, 1048–1052. [Google Scholar] [CrossRef]
- Orendurff, M.S.; Kobayashi, T.; Villarosa, C.Q.; Coleman, K.L.; Boone, D.A. Comparison of a computerized algorithm and prosthetists’ judgment in rating functional levels based on daily step activity in transtibial amputees. J. Rehabil. Assist. Technol. Eng. 2016, 3. [Google Scholar] [CrossRef]
- Burger, H.; Marincek, C.; Isakov, E. Mobility of persons after traumatic lower limb amputation. Disabil. Rehabil. 1997, 19, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Legro, M.W.; Reiber, G.D.; Smith, D.G.; del Aguila, M.; Larsen, J.; Boone, D. Prosthesis evaluation questionnaire for persons with lower limb amputations: Assessing prosthesis-related quality of life. Arch. Phys. Med. Rehabil. 1998, 79, 931–938. [Google Scholar] [CrossRef]
- Miller, W.C.; Deathe, A.B.; Speechley, M. Lower extremity prosthetic mobility: A comparison of 3 self-report scales. Arch. Phys. Med. Rehabil. 2001, 82, 1432–1440. [Google Scholar] [CrossRef]
- Hagberg, B.R.; Hägg, O. Questionnaire for Persons with a Transfemoral Amputation (Q-TFA): Initial validity and reliability of a new outcome measure. J. Rehabil. Res. Dev. 2004, 41, 695–706. [Google Scholar] [CrossRef]
- Raschke, S.U.; Orendurff, M.S.; Mattie, J.L.; Kenyon, D.E.; Jones, O.Y.; Moe, D.; Winder, L.; Wong, A.S.; Moreno-Hernández, A.; Highsmith, M.J.; et al. Biomechanical characteristics, patient preference and activity level with different prosthetic feet: A randomized double blind trial with laboratory and community testing. J. Biomech. 2015, 48, 146–152. [Google Scholar] [CrossRef]
- Anastasiades, P.; Johnston, D.W. A simple activity measure for use with ambulatory subjects. Psychophysiology 1990, 27, 87–93. [Google Scholar] [CrossRef]
- Bussmann, J.B.; Grootscholten, E.A.; Stam, H.J. Daily physical activity and heart rate response in people with a unilateral transtibial amputation for vascular disease. Arch. Phys. Med. Rehabil. 2004, 85, 240–244. [Google Scholar] [CrossRef]
- Bussmann, J.B.; Schrauwen, H.J.; Stam, H.J. Daily physical activity and heart rate response in people with a unilateral traumatic transtibial amputation. Arch. Phys. Med. Rehabil. 2008, 89, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Selles, R.W.; Janssens, P.J.; Jongenengel, C.D.; Bussmann, J.B. A randomized controlled trial comparing functional outcome and cost efficiency of a total surface-bearing socket versus a conventional patellar tendon-bearing socket in transtibial amputees. Arch. Phys. Med. Rehabil. 2005, 86, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Houdijk, H.; Appelman, F.M.; Van Velzen, J.M.; Van der Woude, L.H.; Van Bennekom, C.A. Validity of DynaPort GaitMonitor for assessment of spatiotemporal parameters in amputee gait. J. Rehabil. Res. Dev. 2008, 45, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Theeven, P.J.; Hemmen, B.; Geers, R.P.; Smeets, R.J.; Brink, P.R.; Seelen, H.A. Influence of advanced prosthetic knee joints on perceived performance and everyday life activity level of low-functional persons with a transfemoral amputation or knee disarticulation. J. Rehabil. Med. 2012, 44, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Redfield, M.T.; Cagle, J.C.; Hafner, B.J.; Sanders, J.E. Classifying prosthetic use via accelerometry in persons with transtibial amputations. J. Rehabil. Res. Dev. 2013, 50, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Samuelsen, B.T.; Andrews, K.L.; Houdek, M.T.; Terry, M.; Shives, T.C.; Sim, F.H. The Impact of the Immediate Postoperative Prosthesis on Patient Mobility and Quality of Life after Transtibial Amputation. Am. J. Phys. Med. Rehabil. 2017, 96, 116–119. [Google Scholar] [CrossRef]
- Orendurff, M.S.; Raschke, S.U.; Winder, L.; Moe, D.; Boone, D.A.; Kobayashi, T. Functional level assessment of individuals with transtibial limb loss: Evaluation in the clinical setting versus objective community ambulatory activity. J. Rehabil. Assist. Technol. Eng. 2016, 3. [Google Scholar] [CrossRef] [PubMed]
- Van Dam, M.S.; Kok, G.J.; Munneke, M.; Vogelaar, F.J.; Vliet Vlieland, T.P.; Taminiau, A.H. Measuring physical activity in patients after surgery for a malignant tumour in the leg. The reliability and validity of a continuous ambulatory activity monitor. J. Bone Joint Surg. Br. 2001, 83, 1015–1019. [Google Scholar] [CrossRef] [PubMed]
- Bussmann, J.B.; Damen, L.; Stam, H.J. Analysis and decomposition of signals obtained by thigh-fixed accelerometry during walking. Med. Biol. Eng. Comput. 2000, 38, 632–638. [Google Scholar] [CrossRef]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef]
- Keijsers, N.L.; Horstink, M.W.; Gielen, S.C. Ambulatory motor assessment in Parkinson’s disease. Mov. Disord. 2006, 21, 34–44. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Patla, A.E.; Stewart, A.; Ferrucci, L.; Ciol, M.A.; Guralnik, J.M. Environmental demands associated with community mobility in older adults with and without mobility disabilities. Phys. Ther. 2002, 82, 670–681. [Google Scholar] [CrossRef]
- Robinett, C.S.; Vondran, M.A. Functional ambulation velocity and distance requirements in rural and urban communities. A clinical report. Phys. Ther. 1988, 68, 1371–1373. [Google Scholar] [CrossRef]
- Lapointe, R.; Lajoie, Y.; Serresse, O.; Barbeau, H. Functional community ambulation requirements in incomplete spinal cord injured subjects. Spinal Cord 2001, 39, 327–335. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wong, D.W.C.; Lam, W.K.; Yeung, L.F.; Lee, W.C. Does long-distance walking improve or deteriorate walking stability of transtibial amputees? Clin. Biomech. 2015, 30, 867–873. [Google Scholar] [CrossRef]
- Yeung, L.F.; Leung, A.K.; Zhang, M.; Lee, W.C. Effects of long-distance walking on socket-limb interface pressure, tactile sensitivity and subjective perceptions of trans-tibial amputees. Disabil. Rehabil. 2013, 35, 888–893. [Google Scholar] [CrossRef] [PubMed]
- Bootsma-van der Wiel, A.; Gussekloo, J.; de Craen, A.J.; van Exel, E.; Knook, D.L.; Lagaay, A.M.; Westendorp, R.G. Disability in the oldest old: “can do” or “do do”? J. Am. Geriatr. Soc. 2001, 49, 909–914. [Google Scholar] [CrossRef] [PubMed]
- Albert, M.V.; McCarthy, C.; Valentin, J.; Herrmann, M.; Kording, K.; Jayaraman, A. Monitoring functional capability of individuals with lower limb amputations using mobile phones. PLoS ONE 2013, 8, e65340. [Google Scholar] [CrossRef]
- Washabaugh, E.P.; Kalyanaraman, T.; Adamczyk, P.G.; Claflin, E.S.; Krishnan, C. Validity and repeatability of inertial measurement units for measuring gait parameters. Gait Posture 2017, 55, 87–93. [Google Scholar] [CrossRef]
- Hung, T.N.; Suh, Y.S. Inertial Sensor-Based Two Feet Motion Tracking for Gait Analysis. Sensors 2013, 13, 5614–5629. [Google Scholar] [CrossRef]
- Bort-Roig, J.; Gilson, N.D.; Puig-Ribera, A.; Contreras, R.S.; Trost, S.G. Measuring and influencing physical activity with smartphone technology: A systematic review. Sports Med. 2014, 44, 671–686. [Google Scholar] [CrossRef]
- Gonze, B.B.; Padovani, R.D.C.; Simoes, M.D.S.; Lauria, V.; Proença, N.L.; Sperandio, E.F.; Ostolin, T.L.V.D.P.; Gomes, G.A.O.; Castro, P.C.; Romiti, M.; et al. Use of a Smartphone App to Increase Physical Activity Levels in Insufficiently Active Adults: Feasibility Sequential Multiple Assignment Randomized Trial (SMART). JMIR Res. Protoc. 2020, 9. [Google Scholar] [CrossRef]
- Silsupadol, P.; Teja, K.; Lugade, V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture 2017, 58, 516–522. [Google Scholar] [CrossRef]
- Kang, X.; Huang, B.; Qi, G. A Novel Walking Detection and Step Counting Algorithm Using Unconstrained Smartphones. Sensors 2018, 18, 297. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Persons with A Lower Limb Amputation | Elderly Control Group | p-Value |
|---|---|---|---|
| Gender (M:F) | 13:7 | 5:5 | |
| Age (years) | 68 (60–74) | 76 (69–81) | 0.43 |
| Height (cm) | 171 (165–179) | 172 (168–175) | 0.93 |
| Weight (kg) | 77 (67–85) * | 78 (75–78) | 0.83 |
| Amputation level | TT n = 9 KE n = 4 TF n = 7 | n.a. | |
| Reason for amputation | Traumatic n = 6 Vascular n = 10 Oncological n = 2 VOther n = 2 | n.a. | |
| SIGAM mobility grade | B n = 1 C n = 5 D n = 6 E n = 2 F n = 6 | n.a. |
| Variable | Persons with A Lower Limb Amputation n = 20 | Elderly Control Group n = 10 | p-Value |
|---|---|---|---|
| Maximal consecutive steps | 141 (60–217) | 883 (362–1168) | <0.001 |
| 10 MWT (s) | 17.4 (10.3–25.5) | 9.4 (9.1–10.6) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hofstad, C.J.; Bongers, K.T.J.; Didden, M.; van Ee, R.F.; Keijsers, N.L.W. Maximal Walking Distance in Persons with a Lower Limb Amputation. Sensors 2020, 20, 6770. https://doi.org/10.3390/s20236770
Hofstad CJ, Bongers KTJ, Didden M, van Ee RF, Keijsers NLW. Maximal Walking Distance in Persons with a Lower Limb Amputation. Sensors. 2020; 20(23):6770. https://doi.org/10.3390/s20236770
Chicago/Turabian StyleHofstad, Cheriel J., Kim T.J. Bongers, Mark Didden, René F. van Ee, and Noël L.W. Keijsers. 2020. "Maximal Walking Distance in Persons with a Lower Limb Amputation" Sensors 20, no. 23: 6770. https://doi.org/10.3390/s20236770
APA StyleHofstad, C. J., Bongers, K. T. J., Didden, M., van Ee, R. F., & Keijsers, N. L. W. (2020). Maximal Walking Distance in Persons with a Lower Limb Amputation. Sensors, 20(23), 6770. https://doi.org/10.3390/s20236770





