Organ Contouring for Lung Cancer Patients with a Seed Generation Scheme and Random Walks
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
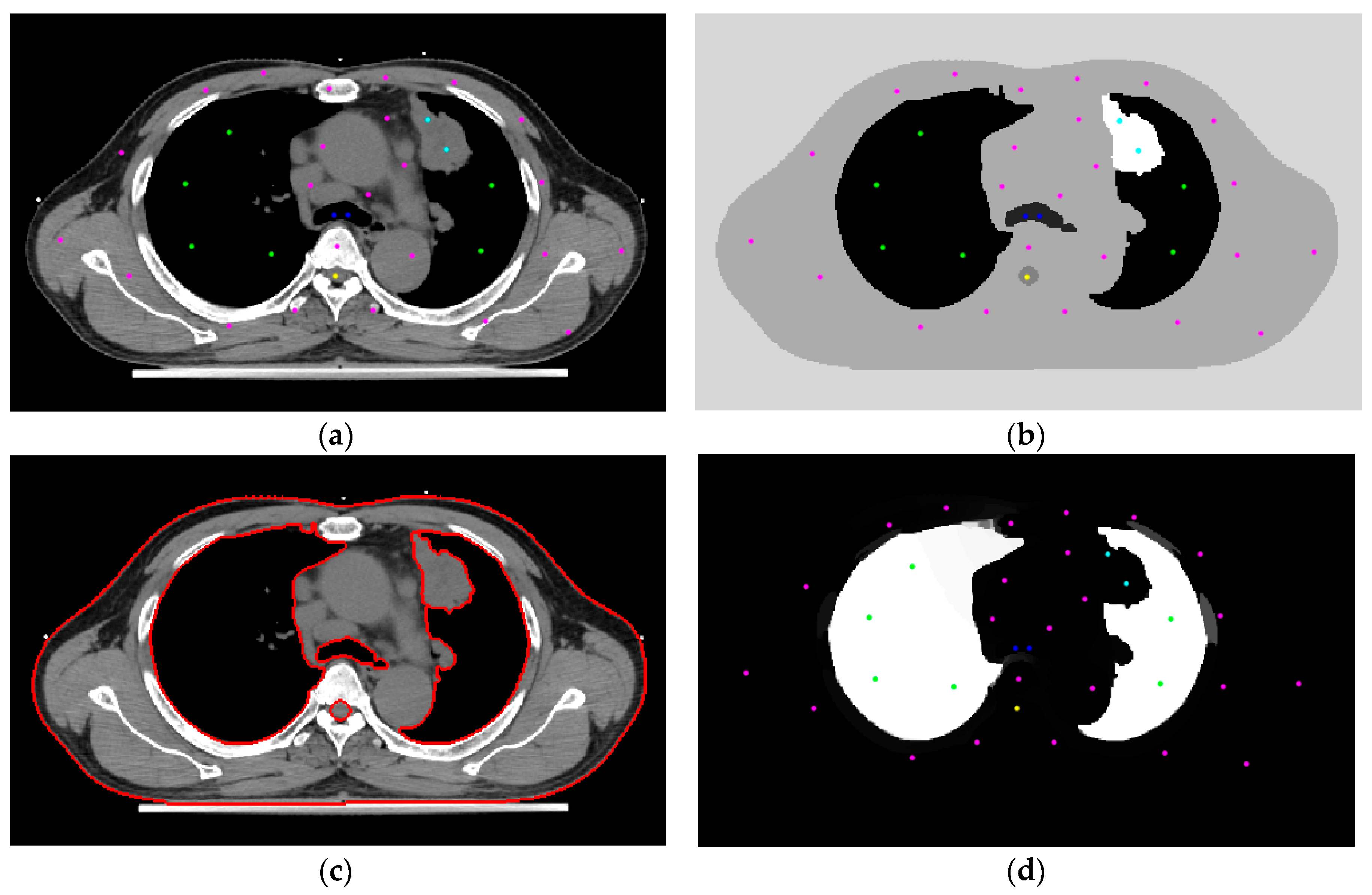
2.2. Initial Settings
2.3. Random Walks Algorithm
2.4. Boundary Erosion
2.5. Use of the Skeleton Technique to Produce Seeds
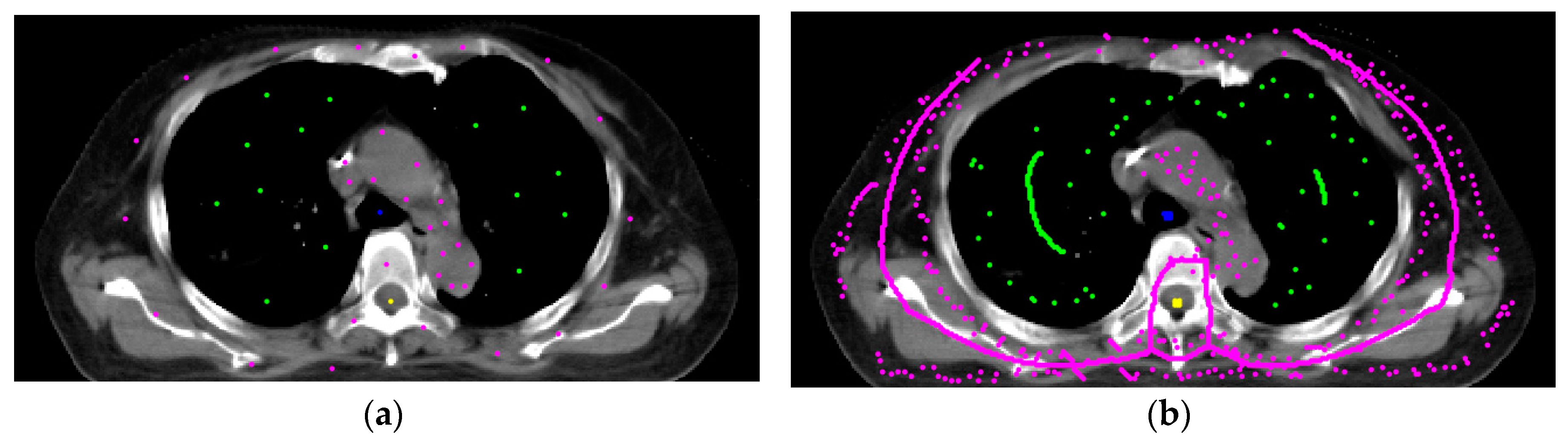
2.6. Modification of the Spinal Cord Boundary
2.7. System Accuracy
3. Results
3.1. Initial Settings
3.2. Automated Segmentation
3.3. Free Parameter β
3.4. System Validity
3.5. System Comparison
3.6. Radiotherapy Plan
4. Discussion
- (1)
- Every patient has different disease conditions. Their tumors, bodies, organs, and so forth are variable. An oncologist manages many patients and has to finish many RTTPs per day. Some patients are easy, and some are very challenging to handle.
- (2)
- In some critical cases, one oncologist might need help from other more experienced oncologists. In such a situation, the time needed is increased.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Postmus, P.E.; Kerr, K.M.; Oudkerk, M.; Senan, S.; Waller, D.A.; Vansteenkiste, J.; Escriu, C.; Peters, S. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Thariat, J.; Hannoun-Levi, J.M.; Myint, A.S.; Vuong, T.; Gérard, J.P. Past, present, and future of radiotherapy for the benefit of patients. Nat. Rev. Clin. Oncol. 2013, 10, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Kang, W.; Hu, H.; Wang, B. HOSVD-Based 3D Active Appearance Model: Segmentation of Lung Fields in CT Images. J. Med. Syst. 2016, 40, 176. [Google Scholar] [CrossRef] [PubMed]
- Cheng, D.C.; Wu, J.F.; Kao, Y.H.; Su, C.H.; Liu, S.-H. Accurate Measurement of Cross-Sectional Area of Femoral Artery on MRI Sequences of Transcontinental Ultramarathon Runners Using Optimal Parameters Selection. J. Med. Syst. 2016, 40, 260. [Google Scholar] [CrossRef]
- Cheng, D.C.; Chen, L.W.; Shen, Y.W.; Fuh, L.J. Computer-assisted system on mandibular canal detection. Biomed. Eng. Biomed. Tech. 2019, 62, 575–580. [Google Scholar] [CrossRef]
- Thomas, H.M.T.; Devakumar, D.; Sasidharan, B.; Heck, D.K.; Bowen, S.R.; Samuel, E.J.J. Hybrid positron emission tomography segmentation of heterogeneous lung tumors using 3D Slicer: Improved GrowCut algorithm with threshold initialization. J. Med. Imaging 2017, 4, 011009. [Google Scholar] [CrossRef]
- Uberti, M.G.; Boska, M.D.; Liu, Y. A semi-automatic image segmentation method for extraction of brain volume from in vivo mouse head magnetic resonance imaging using constraint level sets. J. Neurosci. Methods 2009, 179, 338–344. [Google Scholar] [CrossRef][Green Version]
- Grady, L. Random walks for image segmentation. IEEE Trans. Pattern Anal. Mach. Intell. 2006, 28, 1768–1783. [Google Scholar] [CrossRef]
- Mathworks. Available online: https://www.mathworks.com/ (accessed on 1 August 2020).
- Ju, W.; Xiang, D.; Zhang, B.; Wang, L.; Kopriva, I.; Chen, X. Random Walk and Graph Cut for Co-Segmentation of Lung Tumor on PET-CT Images. IEEE Trans. Image Process. 2015, 24, 5854–5867. [Google Scholar] [CrossRef]
- Dakua, S.P.; Sahambi, J.S. Modified active contour model and Random Walk approach for left ventricular cardiac MR image segmentation. Int. J. Numer. Methods Biomed. Eng. 2011, 27, 1350–1361. [Google Scholar] [CrossRef]
- Karamalis, A.; Wein, W.; Klein, T.; Navab, N. Ultrasound confidence maps using random walks. Med. Image Anal. 2012, 16, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Stefano, A.; Vitabile, S.; Russo, G.; Ippolito, M.; Sabini, M.G.; Sardina, D. An enhanced random walk algorithm for delineation of head and neck cancers in PET studies. Med. Biol. Eng. Comput. 2017, 55, 897–908. [Google Scholar] [CrossRef] [PubMed]
- González, R.C.; Woods, R.E. Digital Image Processing, 3rd ed.; Person Prentice Hall: Upper Saddle River, NJ, USA, 2008. [Google Scholar]
- Kong, T.Y.; Rosenfeld, A. Topological Algorithms for Digital Image Processing; Elsevier: Amsterdam, The Netherlands, 1996. [Google Scholar]
- Dice, L.R. Measures of the Amount of Ecologic Association between Species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- Sørensen, T.A. A method of establishing groups of equal amplitude in plant sociology based on similarity of species content and its application to analyses of the vegetation on Danish commons. Biol. Skar. 1948, 5, 1–34. [Google Scholar]
- Krizhevsky, A. CIFAR-10 and CIFAR-100 Datasets. Available online: https://www.cs.toronto.edu/~kriz/cifar.html (accessed on 1 August 2020).
- The Coco Dataset. Available online: https://cocodataset.org/#home (accessed on 1 August 2020).
- Emmert-Streib, F.; Yang, Z.; Feng, H.; Tripathi, S.; Dehmer, M. An introductory review of deep learning for prediction models with big data. Front. Artif. Intell. 2020. [Google Scholar] [CrossRef]
- Shrestha, A.; Mahmood, A. Review of deep learning algorithms and architectures. IEEE Access 2020, 7, 53040–53065. [Google Scholar] [CrossRef]
- LeCun, Y.; Cortes, C.; Burges, C. The MNIST Database of Handwritten Digits. Available online: http://yann.lecun.com/exdb/mnist/ (accessed on 1 August 2020).
- Vendt, B. LIDC-IDRI Dataset. Available online: https://wiki.cancerimagingarchive.net/display/Public/LIDC-IDRI (accessed on 1 August 2020).
- Ahlawat, S.; Choudhary, A.; Nayyar, A.; Singh, S.; Yoon, B. Improved handwritten digit recognition using convolutional neural networks (CNN). Sensors 2020, 20, 3344. [Google Scholar] [CrossRef]
- Chi, J.; Zhang, S.; Yu, X.; Wu, C.; Jiang, Y. A novel pulmonary nodule detection model based on multi-step cascaded networks. Sensors 2020, 20, 4301. [Google Scholar] [CrossRef]
- Lee, S.; Stewart, J.; Lee, Y.; Myrehaug, S.; Sahgal, A.; Ruschin, M.; Tseng, C.L. Improved dosimetric accuracy with semi-automatic contour propagation of organ-at-risk in glioblastoma patients. J. Appl. Clin. Med. Phys. 2019, 20, 45–53. [Google Scholar] [CrossRef]
- Su, H.-H.; Pan, H.-W.; Lu, C.-P.; Chuang, J.-J.; Yang, T. Automatic detection method for cancer cell nucleus image based on deep-learning analysis and color layer signature analysis algorithm. Sensors 2020, 20, 4409. [Google Scholar] [CrossRef]
- Rote, G. Computing the minimum Hausdorff distance between two point sets on a line under translation. Inf. Process. Lett. 1991, 38, 123–127. [Google Scholar] [CrossRef]
- Ghaffari, M.; Sanchez, L.; Xu, G.; Alaraj, A.; Zhou, X.J.; Charbel, F.T.; Linninger, A.A. Validation of parametric mesh generation for subject-specific cerebroarterial trees using modified Hausdorff distance metrics. Comput. Biol. Med. 2018, 100, 209–220. [Google Scholar] [CrossRef] [PubMed]






| Hounsfield Units | Tissue |
|---|---|
| 20 to 40 | Muscle, vessel, soft tissue |
| 0 | Water |
| −30 to −70 | Fat |
| −400 to −600 | Lung |
| −1000 | Air |
| Case No. | Lungs | Airway | Heart | Spinal Cord | Body | GTV | Computation Time (s) |
|---|---|---|---|---|---|---|---|
| 1 | 0.938 | 0.779 | 0.872 | 0.770 | 0.851 | 0.514 | 83 |
| 2 | 0.923 | --- 1 | 0.850 | 0.692 | 0.795 | 0.403 | 87 |
| 3 | 0.962 | 0.948 | 0.849 | 0.853 | 0.852 | --- 2 | 151 |
| 4 | 0.921 | 0.906 | 0.866 | 0.767 | 0.914 | 0.514 | 195 |
| 5 | 0.934 | 0.686 | 0.945 | 0.835 | 0.842 | 0.284 | 85 |
| 6 | 0.947 | 0.918 | 0.880 | 0.748 | 0.859 | 0.719 | 115 |
| 7 | 0.942 | --- 1 | --- 1 | 0.715 | 0.901 | 0.754 | 139 |
| 8 | 0.953 | 0.905 | --- 1 | 0.760 | 0.774 | 0.889 | 119 |
| 9 | 0.870 | 0.823 | --- 1 | 0.605 | 0.899 | 0.759 | 213 |
| 10 | 0.943 | 0.893 | 0.849 | 0.718 | 0.799 | 0.520 | 186 |
| 11 | 0.946 | 0.908 | 0.932 | 0.770 | 0.855 | 0.381 | 149 |
| 12 | 0.976 | 0.855 | 0.915 | 0.840 | 0.819 | 0.204 | 119 |
| 13 | 0.950 | 0.948 | 0.912 | 0.812 | 0.776 | 0.406 | 88 |
| 14 | 0.935 | 0.837 | --- 1 | 0.587 | 0.898 | 0.598 | 231 |
| 15 | 0.926 | 0.782 | 0.823 | 0.596 | 0.873 | 0.891 | 152 |
| Mean | 0.94 | 0.86 | 0.88 | 0.74 | 0.85 | 0.57 | 141 |
| Std. | 0.02 | 0.07 | 0.04 | 0.09 | 0.04 | 0.21 | 48 |
| Dice Coefficient | FPR | FNR | ||
|---|---|---|---|---|
| Lung | Eclipse | 0.995 | 0.007 | 0.001 |
| Our system | 0.938 | 0.080 | 0.007 | |
| Spinal cord | Eclipse | 0.792 | 0.508 | 0.038 |
| Our system | 0.770 | 0.551 | 0.097 |
| Case No. | Lungs | Airway | Heart | Spinal Cord | Body | GTV |
|---|---|---|---|---|---|---|
| 1 | 0.899 | 0.865 | 0.919 | 0.695 | 0.807 | 0.814 |
| 2 | 0.892 | 0.785 | 0.876 | 0.728 | 0.853 | 0.868 |
| 3 | 0.865 | 0.745 | 0.896 | 0.799 | 0.850 | 0.829 |
| 4 | 0.926 | 0.850 | 0.816 | 0.689 | 0.863 | 0.822 |
| 5 | 0.890 | 0.817 | 0.858 | 0.649 | 0.824 | 0.915 |
| 6 | 0.899 | 0.819 | 0.000 | 0.725 | 0.815 | 0.851 |
| 7 | 0.903 | 0.907 | 0.886 | 0.634 | 0.846 | 0.686 |
| 8 | 0.906 | 0.757 | 0.895 | 0.756 | 0.831 | 0.682 |
| 9 | 0.895 | 0.810 | 0.826 | 0.737 | 0.847 | 0.695 |
| 10 | 0.904 | 0.767 | 0.854 | 0.687 | 0.852 | 0.639 |
| Mean | 0.90 | 0.81 | 0.78 | 0.71 | 0.84 | 0.78 |
| Std. | 0.02 | 0.05 | 0.26 | 0.05 | 0.02 | 0.09 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, D.-C.; Chi, J.-H.; Yang, S.-N.; Liu, S.-H. Organ Contouring for Lung Cancer Patients with a Seed Generation Scheme and Random Walks. Sensors 2020, 20, 4823. https://doi.org/10.3390/s20174823
Cheng D-C, Chi J-H, Yang S-N, Liu S-H. Organ Contouring for Lung Cancer Patients with a Seed Generation Scheme and Random Walks. Sensors. 2020; 20(17):4823. https://doi.org/10.3390/s20174823
Chicago/Turabian StyleCheng, Da-Chuan, Jen-Hong Chi, Shih-Neng Yang, and Shing-Hong Liu. 2020. "Organ Contouring for Lung Cancer Patients with a Seed Generation Scheme and Random Walks" Sensors 20, no. 17: 4823. https://doi.org/10.3390/s20174823
APA StyleCheng, D.-C., Chi, J.-H., Yang, S.-N., & Liu, S.-H. (2020). Organ Contouring for Lung Cancer Patients with a Seed Generation Scheme and Random Walks. Sensors, 20(17), 4823. https://doi.org/10.3390/s20174823







