Device Development for Detecting Thumb Opposition Impairment Using Carbon Nanotube-Based Strain Sensors
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Physical Examination and NCV Testing
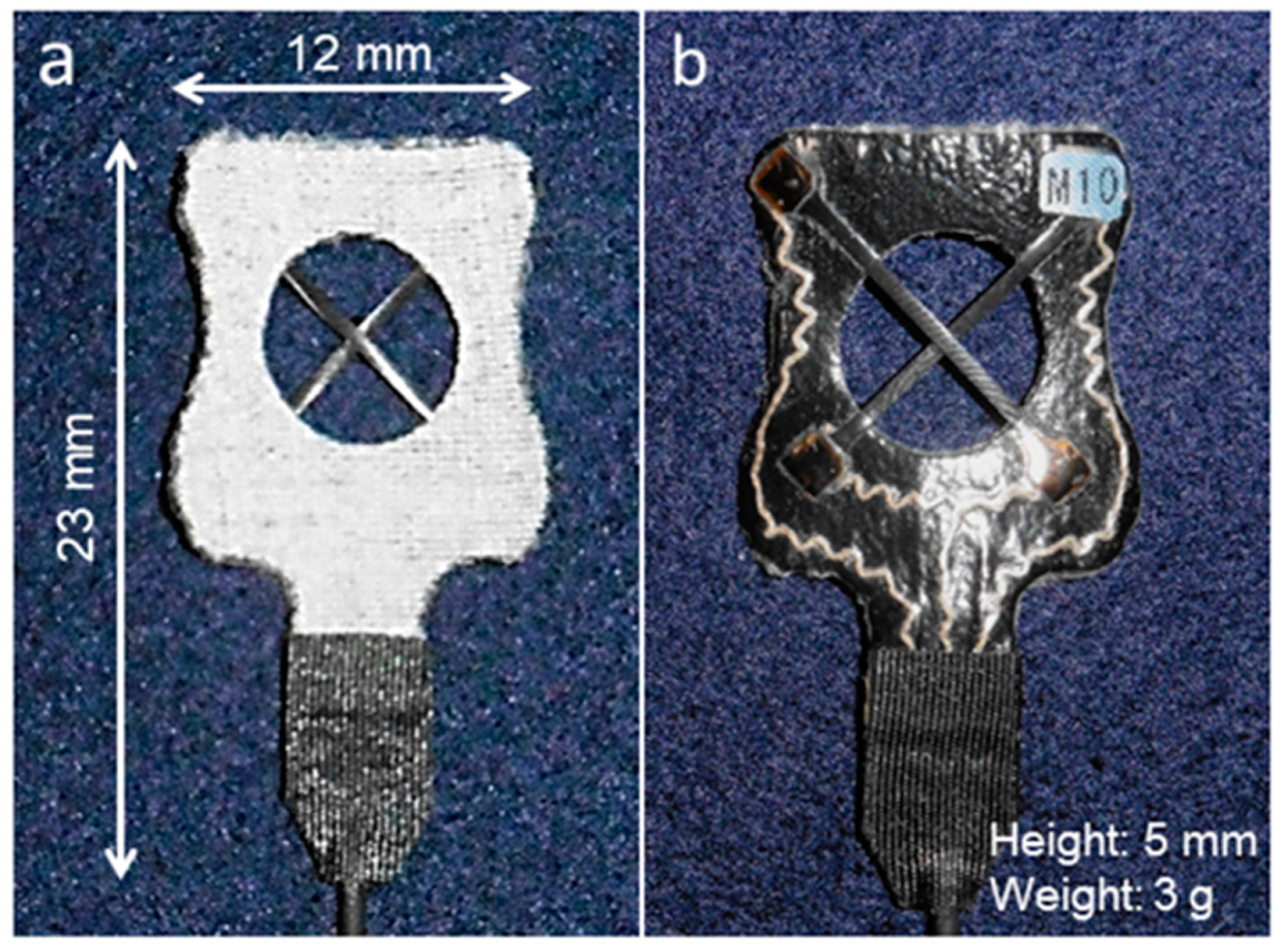
2.3. Apparatus
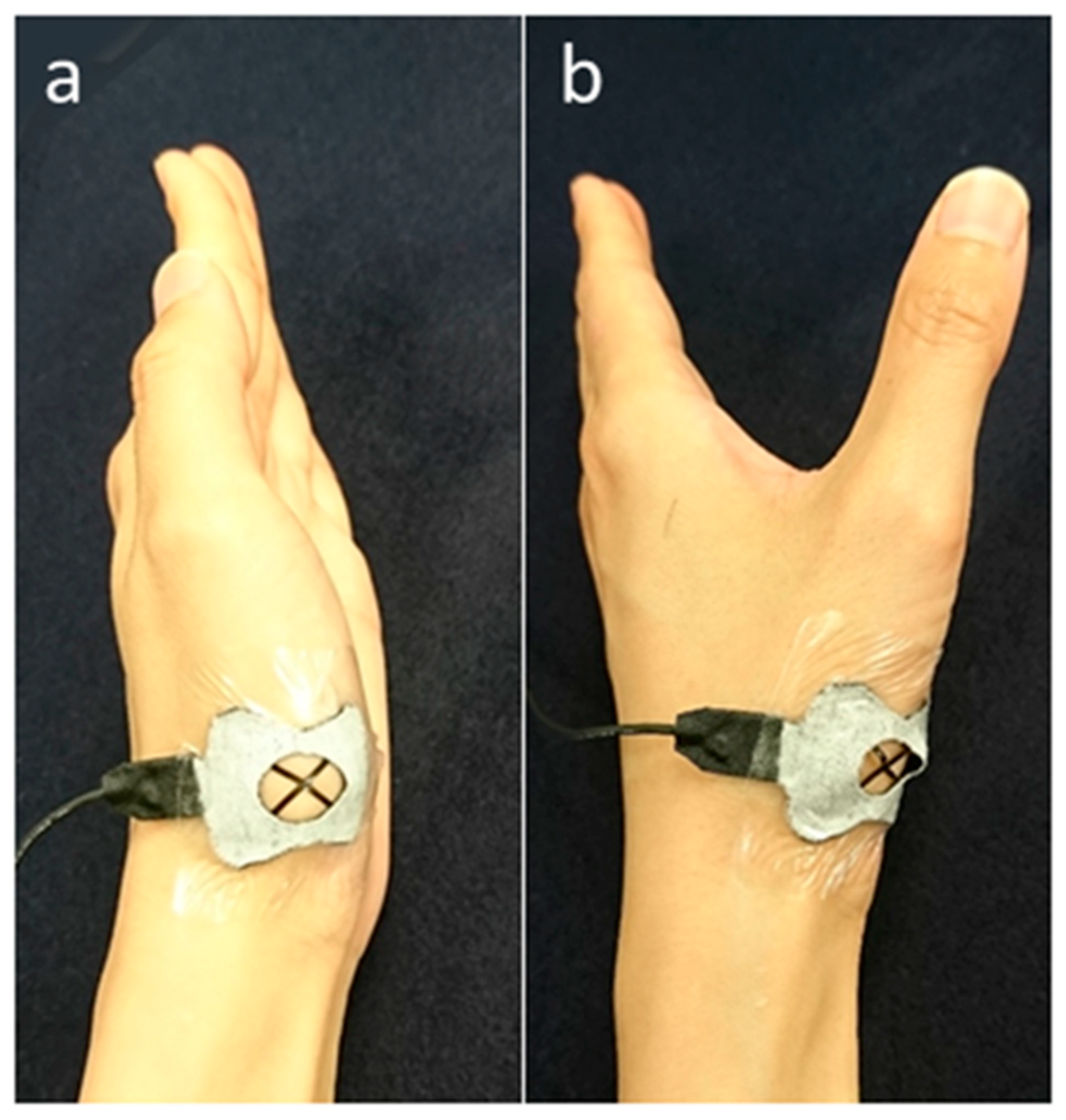
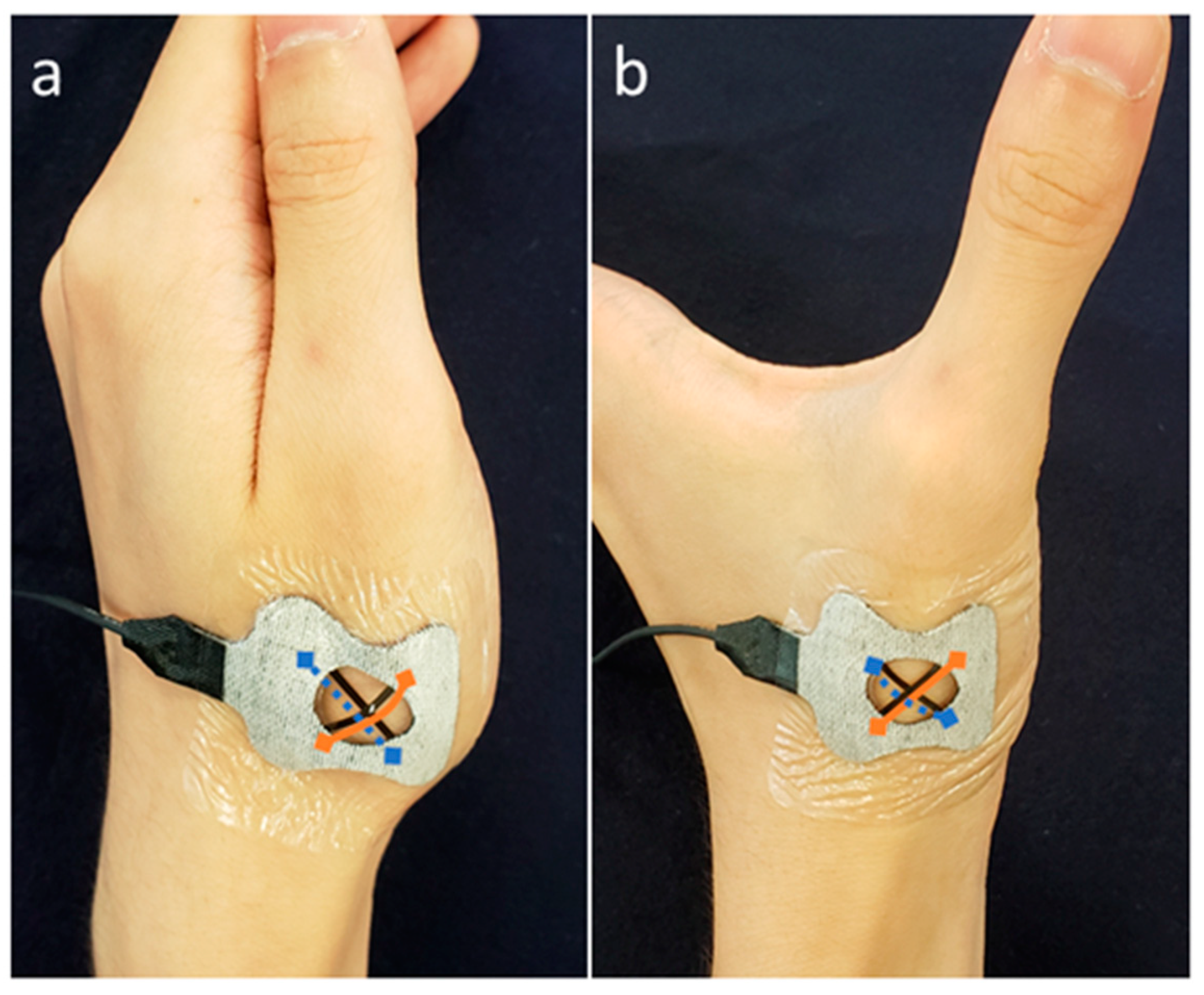
2.4. Measurements
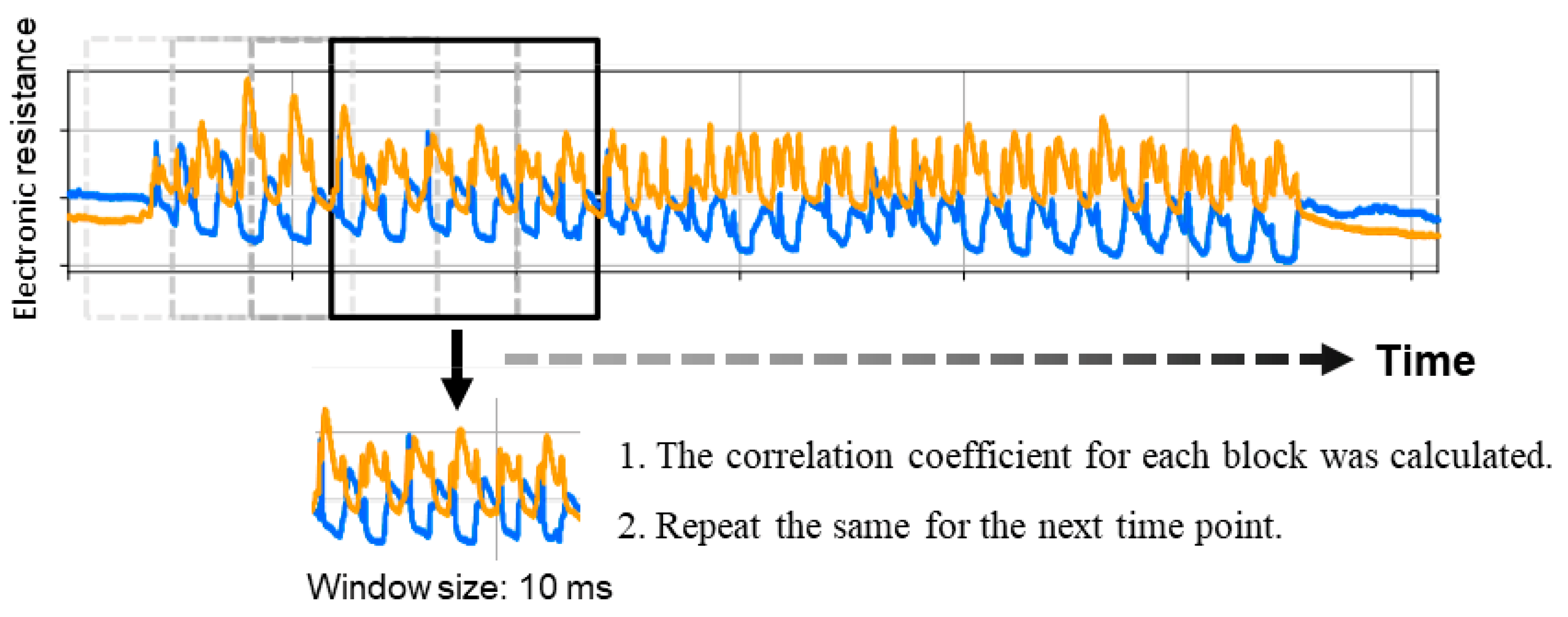
2.5. Analysis
3. Results
3.1. Patient Characteristics
3.2. Measurement Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cifrek, M.; Medved, V.; Tonkovic, S.; Ostojic, S. Surface EMG based muscle fatigue evaluation in biomechanics. Clin. Biomech. 2009, 24, 327–340. [Google Scholar] [CrossRef]
- Jarque-Bou, N.J.; Scano, A.; Atzori, M.; Muller, H. Kinematic synergies of hand grasps: A comprehensive study on a large publicly available dataset. J. Neuroeng. Rehabil. 2019, 16, 63. [Google Scholar] [CrossRef]
- Eschmann, H.; Heroux, M.E.; Cheetham, J.H.; Potts, S.; Diong, J. Thumb and finger movement is reduced after stroke: An observational study. PLoS ONE 2019, 14, e0217969. [Google Scholar] [CrossRef]
- Barlow, S.; Custead, R.; Lee, J.; Hozan, M.; Greenwood, J. Wireless Sensing of Lower Lip and Thumb-Index Finger ‘Ramp-and-Hold’ Isometric Force Dynamics in a Small Cohort of Unilateral MCA Stroke: Discussion of Preliminary Findings. Sensors 2020, 20, 1221. [Google Scholar] [CrossRef]
- Lin, B.; Hsiao, P.; Yang, S.; Su, C.; Lee, I. Data Glove System Embedded With Inertial Measurement Units for Hand Function Evaluation in Stroke Patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 2204–2213. [Google Scholar] [CrossRef]
- Wirth, M.A.; Fischer, G.; Verdu, J.; Reissner, L.; Balocco, S.; Calcagni, M. Comparison of a New Inertial Sensor Based System with an Optoelectronic Motion Capture System for Motion Analysis of Healthy Human Wrist Joints. Sensors 2019, 19, 5297. [Google Scholar] [CrossRef]
- Kumar, P.; Verma, J.; Prasad, S. Hand data glove: A wearable real-time device for human-computer interaction. Int. J. Adv. Sci. Technol. 2012, 43, 15–26. [Google Scholar]
- Williams, N.W.; Penrose, J.M.; Caddy, C.M.; Barnes, E.; Hose, D.R.; Harley, P. A goniometric glove for clinical hand assessment. Construction, calibration and validation. J. Hand Surg. 2000, 25, 200–207. [Google Scholar] [CrossRef]
- Berger, A.J.; Meals, R.A. Management of osteoarthrosis of the thumb joints. J. Hand Surg. Am. 2015, 40, 843–850. [Google Scholar] [CrossRef]
- Edmunds, J.O. Current concepts of the anatomy of the thumb trapeziometacarpal joint. J. Hand Surg. Am. 2011, 36, 170–182. [Google Scholar] [CrossRef]
- Kurtzman, L.C.; Stern, P.J.; Yakuboff, K.P. Reconstruction of the burned thumb. Hand Clin. 1992, 8, 107–119. [Google Scholar]
- Bunnell, S. Opposition of the thumb. JBJS 1938, 20, 269–284. [Google Scholar]
- Cooney, W.P.; Linscheid, R.L.; An, K.N. Opposition of the thumb: An anatomic and biomechanical study of tendon transfers. J. Hand Surg. Am. 1984, 9, 777–786. [Google Scholar] [CrossRef]
- Geere, J.; Chester, R.; Kale, S.; Jerosch-Herold, C. Power grip, pinch grip, manual muscle testing or thenar atrophy—Which should be assessed as a motor outcome after carpal tunnel decompression? A systematic review. BMC Musculoskelet. Disord. 2007, 8, 114. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Xia, H.; Guo, C. A Model-Based System for Real-Time Articulated Hand Tracking Using a Simple Data Glove and a Depth Camera. Sensors 2019, 19, 4680. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Bae, J. A Three-dimensional Finger Motion Measurement System of a Thumb and an Index Finger Without a Calibration Process. Sensors 2020, 20, 756. [Google Scholar] [CrossRef]
- Wang, K.K.; Zhang, X.; McCombe, D.; Ackland, D.C.; Ek, E.T.; Tham, S.K. Quantitative analysis of in-vivo thumb carpometacarpal joint kinematics using four-dimensional computed tomography. J. Hand Surg. Eur. Vol. 2018, 43, 1088–1097. [Google Scholar] [CrossRef]
- Kapandji, A. Clinical test of apposition and counter-apposition of the thumb. Ann Chir Main. 1986, 5, 67–73. [Google Scholar] [CrossRef]
- Bakhach, J.; Chaya, B.; Papazian, N. Omega “Omega” Pulley Plasty for Surgical Management of DeQuervain’s Disease. J. Hand Surg. Asian Pac. Vol. 2018, 23, 170–175. [Google Scholar] [CrossRef]
- Dehl, M.; Chelli, M.; Lippmann, S.; Benaissa, S.; Rotari, V.; Moughabghab, M. Results of 115 Rubis II reverse thumb carpometacarpal joint prostheses with a mean follow-up of 10 years. J. Hand Surg. Eur. Vol. 2017, 42, 592–598. [Google Scholar] [CrossRef]
- Smeraglia, F.; Soldati, A.; Orabona, G.; Ivone, A.; Balato, G.; Pacelli, M. Trapeziometacarpal arthrodesis: Is bone union necessary for a good outcome? J. Hand Surg. Eur. Vol. 2015, 40, 356–361. [Google Scholar] [CrossRef]
- Barakat, M.J.; Field, J.; Taylor, J. The range of movement of the thumb. Hand 2013, 8, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Dilokhuttakarn, T.; Naito, K.; Kinoshita, M.; Sugiyama, Y.; Goto, K.; Iwase, Y.; Kaneko, K. Evaluation of thenar muscles by MRI in carpal tunnel syndrome. Exp. Ther. Med. 2017, 14, 2025–2030. [Google Scholar] [CrossRef] [PubMed]
- Kuroiwa, T.; Nimura, A.; Suzuki, S.; Sasaki, T.; Okawa, A.; Fujita, K. Measurement of thumb pronation and palmar abduction angles with a small motion sensor: A comparison with Kapandji scores. J. Hand Surg. Eur. Vol. 2019, 44, 728–733. [Google Scholar] [CrossRef]
- Kawanishi, Y.; Oka, K.; Tanaka, H.; Okada, K.; Sugamoto, K.; Murase, T. In Vivo 3-Dimensional Kinematics of Thumb Carpometacarpal Joint During Thumb Opposition. J. Hand Surg. Am. 2018, 43, 182.e1–182.e7. [Google Scholar] [CrossRef]
- Marquardt, T.L.; Nataraj, R.; Evans, P.J.; Seitz, W.H., Jr.; Li, Z.M. Carpal tunnel syndrome impairs thumb opposition and circumduction motion. Clin. Orthop. Relat. Res. 2014, 472, 2526–2533. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuroiwa, T.; Fujita, K.; Nimura, A.; Miyamoto, T.; Sasaki, T.; Okawa, A. A new method of measuring the thumb pronation and palmar abduction angles during opposition movement using a three-axis gyroscope. J. Orthop. Surg. Res. 2018, 13, 288. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Hayamizu, Y.; Yamamoto, Y.; Yomogida, Y.; Izadi-Najafabadi, A.; Futaba, D.N.; Hata, K. A stretchable carbon nanotube strain sensor for human-motion detection. Nat. Nanotechnol. 2011, 6, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Lu, N.; Ma, R.; Kim, Y.S.; Kim, R.H.; Wang, S.; Wu, J.; Won, S.M.; Tao, H.; Islam, A.; et al. Epidermal electronics. Science 2011, 333, 838–843. [Google Scholar] [CrossRef]
- Amjadi, M.; Kyung, K.-U.; Park, I.; Sitti, M. Stretchable, Skin-Mountable, and Wearable Strain Sensors and Their Potential Applications: A Review. Adv. Funct. Mater. 2016, 26, 1678–1698. [Google Scholar] [CrossRef]
- Hwang, E.; Seo, J.; Kim, Y. A Polymer-Based Flexible Tactile Sensor for Both Normal and Shear Load Detections and Its Application for Robotics. J. Microelectromechanical Syst. 2007, 16, 556–563. [Google Scholar] [CrossRef]
- Lipomi, D.J.; Vosgueritchian, M.; Tee, B.C.; Hellstrom, S.L.; Lee, J.A.; Fox, C.H.; Bao, Z. Skin-like pressure and strain sensors based on transparent elastic films of carbon nanotubes. Nat. Nanotechnol. 2011, 6, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.; Lee, P.; Chou, J.B.; Xu, R.; Zhao, R.; Hart, A.J.; Kim, S.G. Extremely Elastic Wearable Carbon Nanotube Fiber Strain Sensor for Monitoring of Human Motion. ACS Nano 2015, 9, 5929–5936. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, A.; Nakamoto, H.; Yamaji, T.; Ootaka, H.; Bessho, Y.; Nakamura, R.; Ono, R. Method for measuring tri-axial lumbar motion angles using wearable sheet stretch sensors. PLoS ONE 2017, 12, e0183651. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Li, M.; Mei, T.; McCoul, D.; Qin, S.; Zhao, Z.; Zhao, J. Wearable Stretch Sensors for Motion Measurement of the Wrist Joint Based on Dielectric Elastomers. Sensors 2017, 17, 2708. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Padua, L.; Lo Monaco, M.; Padua, R.; Gregori, B.; Tonali, P. Neurophysiological classification of carpal tunnel syndrome: Assessment of 600 symptomatic hands. Ital. J. Neurol. Sci. 1997, 18, 145–150. [Google Scholar] [CrossRef]
- Hegazy, G.; Mansour, T.; Alshal, E.; Abdelaziz, M.; Alnahas, M.; El-Sebaey, I. Madelung’s deformity: Capitate-related versus ulna-related measurement methods. J. Hand Surg. Eur. Vol. 2019, 44, 524–531. [Google Scholar] [CrossRef]
- Marei, A.; Doi, K.; Hattori, Y.; Sakamot, S. Quantitative assessment of elbow flexion by handheld dynamometry in brachial plexus palsy. J. Hand Surg. Eur. Vol. 2019, 44, 256–262. [Google Scholar] [CrossRef]
- Sun, G.T.W.; MacLean, S.B.M.; Alexander, J.J.; Woodman, R.; Bain, G.I. Association of scapholunate dissociation and two-part articular fractures of the distal radius. J. Hand Surg. Eur. Vol. 2019, 44, 468–474. [Google Scholar] [CrossRef]
- Gelberman, R.H.; Pfeffer, G.B.; Galbraith, R.T.; Szabo, R.M.; Rydevik, B.; Dimick, M. Results of treatment of severe carpal-tunnel syndrome without internal neurolysis of the median nerve. J. Bone Jt. Surg. Am. Vol. 1987, 69, 896–903. [Google Scholar] [CrossRef]
- Suzuki, K.; Yataka, K.; Okumiya, Y.; Sakakibara, S.; Sako, K.; Mimura, H.; Inoue, Y. Rapid-Response, Widely Stretchable Sensor of Aligned MWCNT/Elastomer Composites for Human Motion Detection. ACS Sens. 2016, 1, 817–825. [Google Scholar] [CrossRef]
- Garg, B.; Manhas, V.; Vardhan, A.; Srivastava, D.N.; Das, C.J.; Vibha, D.; Gupta, V.; Malhotra, R.; Kotwal, P. Thumb Opposition Recovery Following Surgery for Severe Carpal Tunnel Syndrome: A Clinical, Radiological, and Electrophysiological Pilot Study. J. Hand Surg. Am. 2019, 44, 157.e1–157.e5. [Google Scholar] [CrossRef] [PubMed]
- Nolan, W.B., III; Alkaitis, D.; Glickel, S.Z.; Snow, S. Results of treatment of severe carpal tunnel syndrome. J. Hand Surg. Am. 1992, 17, 1020–1023. [Google Scholar] [CrossRef]
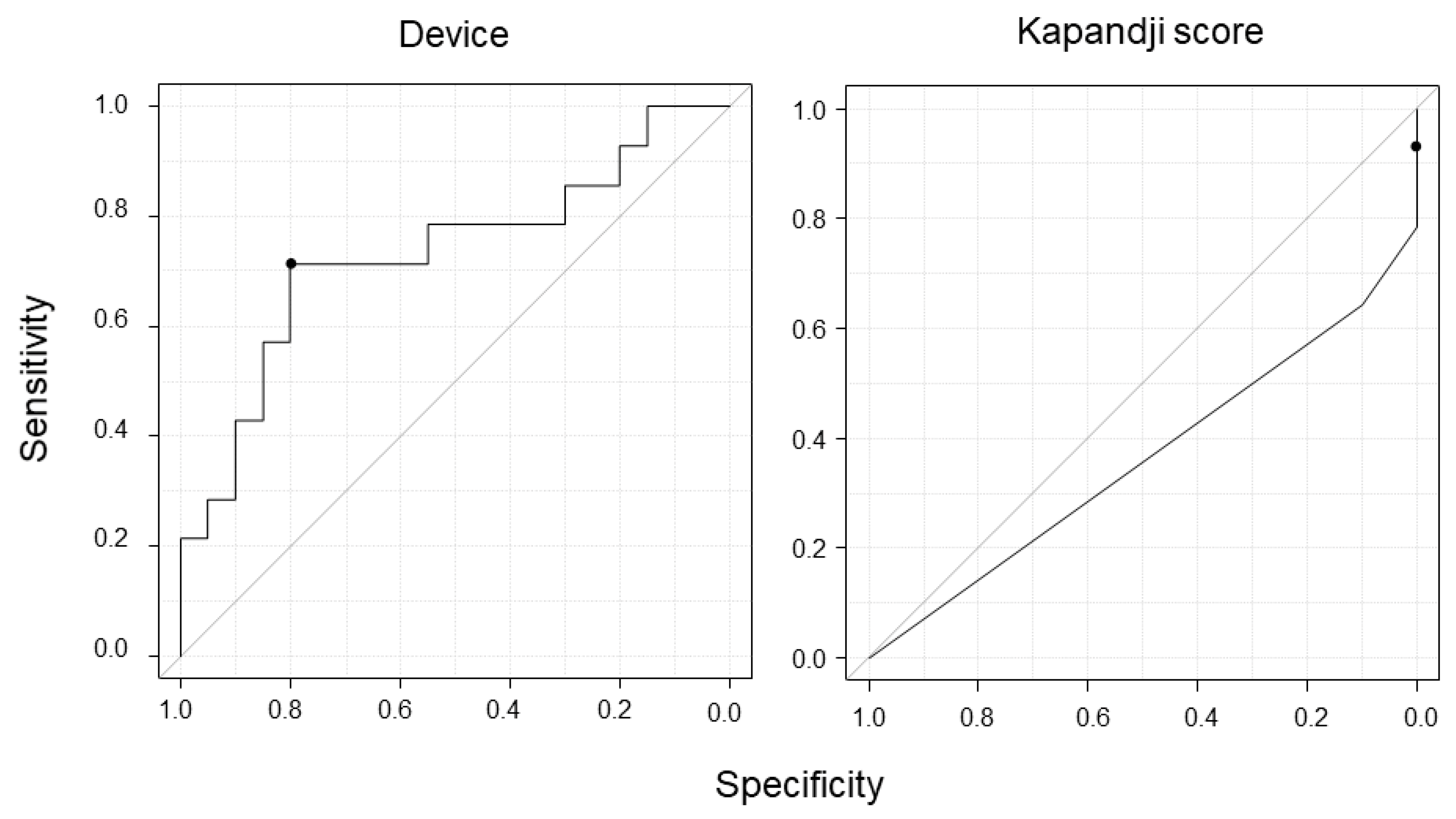
- Greiner, M.; Pfeiffer, D.; Smith, R.D. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev. Vet. Med. 2000, 45, 23–41. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef]
- Kuhlman, K.A.; Hennessey, W.J. Sensitivity and specificity of carpal tunnel syndrome signs. Am. J. Phys. Med. Rehabil. 1997, 76, 451–457. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Danjo, J.; Sawada, H.; Uchida, K.; Danjo, S.; Nakamura, Y. Efficacy of a new microvibration sensation measurement device at detecting diabetic peripheral neuropathy using a newly devised finger method. J. Gen. Fam. Med. 2017, 18, 155–161. [Google Scholar] [CrossRef]
- Fujita, K.; Watanabe, T.; Kuroiwa, T.; Sasaki, T.; Nimura, A.; Sugiura, Y. A Tablet-Based App for Carpal Tunnel Syndrome Screening: Diagnostic Case-Control Study. JMIR Mhealth Uhealth 2019, 7, e14172. [Google Scholar] [CrossRef]
- Wainner, R.S.; Fritz, J.M.; Irrgang, J.J.; Delitto, A.; Allison, S.; Boninger, M.L. Development of a clinical prediction rule for the diagnosis of carpal tunnel syndrome. Arch. Phys. Med. Rehabil. 2005, 86, 609–618. [Google Scholar] [CrossRef] [PubMed]


| Control (n = 11) | CTS (n = 13) | p-Value | |
|---|---|---|---|
| Age (years) | 64 [58–68] | 59 [55–67] | 0.56 |
| Sex (female) | 10 | 12 | |
| Number of hands | 20 | 14 | |
| Number of hands with cane | 2 | 2 |
| Thenar Atrophy | |
|---|---|
| Absent | 6 |
| Mild | 1 |
| Moderate | 3 |
| Severe | 4 |
| Padua’s classification | |
| Normal | 0 |
| Minimal | 0 |
| Mild | 0 |
| Moderate | 7 |
| Severe | 2 |
| Extreme | 5 |
| Kapandji Score | Control (n = 20) | CTS (n = 14) |
|---|---|---|
| 1 | 0 | 0 |
| 2 | 0 | 0 |
| 3 | 0 | 0 |
| 4 | 0 | 0 |
| 5 | 0 | 1 (7) |
| 6 | 0 | 0 |
| 7 | 0 | 0 |
| 8 | 0 | 2 (14) |
| 9 | 2 (10) | 2 (14) |
| 10 | 18 (90) | 9 (65) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuroiwa, T.; Nimura, A.; Takahashi, Y.; Sasaki, T.; Koyama, T.; Okawa, A.; Fujita, K. Device Development for Detecting Thumb Opposition Impairment Using Carbon Nanotube-Based Strain Sensors. Sensors 2020, 20, 3998. https://doi.org/10.3390/s20143998
Kuroiwa T, Nimura A, Takahashi Y, Sasaki T, Koyama T, Okawa A, Fujita K. Device Development for Detecting Thumb Opposition Impairment Using Carbon Nanotube-Based Strain Sensors. Sensors. 2020; 20(14):3998. https://doi.org/10.3390/s20143998
Chicago/Turabian StyleKuroiwa, Tomoyuki, Akimoto Nimura, Yu Takahashi, Toru Sasaki, Takafumi Koyama, Atsushi Okawa, and Koji Fujita. 2020. "Device Development for Detecting Thumb Opposition Impairment Using Carbon Nanotube-Based Strain Sensors" Sensors 20, no. 14: 3998. https://doi.org/10.3390/s20143998
APA StyleKuroiwa, T., Nimura, A., Takahashi, Y., Sasaki, T., Koyama, T., Okawa, A., & Fujita, K. (2020). Device Development for Detecting Thumb Opposition Impairment Using Carbon Nanotube-Based Strain Sensors. Sensors, 20(14), 3998. https://doi.org/10.3390/s20143998





