Quantification of Triple Single-Leg Hop Test Temporospatial Parameters: A Validated Method Using Body-Worn Sensors for Functional Evaluation after Knee Injury
Abstract
1. Introduction
2. Materials and Methods
2.1. Wearable Measurement System
2.2. The Reference System
2.3. Experimental Protocol
2.3.1. Criterion-Related Validation Experiments
2.3.2. Construct Validation Experiments
2.4. Temporal Events Detection
2.4.1. Reference Temporal Events
2.4.2. IMU-based Temporal Events
2.5. Forward Progression Estimation
2.5.1. Reference Forward Progression
2.5.2. IMU-based Forward Progression
2.6. Data Analysis and Statistical Tests
3. Results
3.1. Estimations of Temporospatial Parameters: IMU Versus Reference Systems
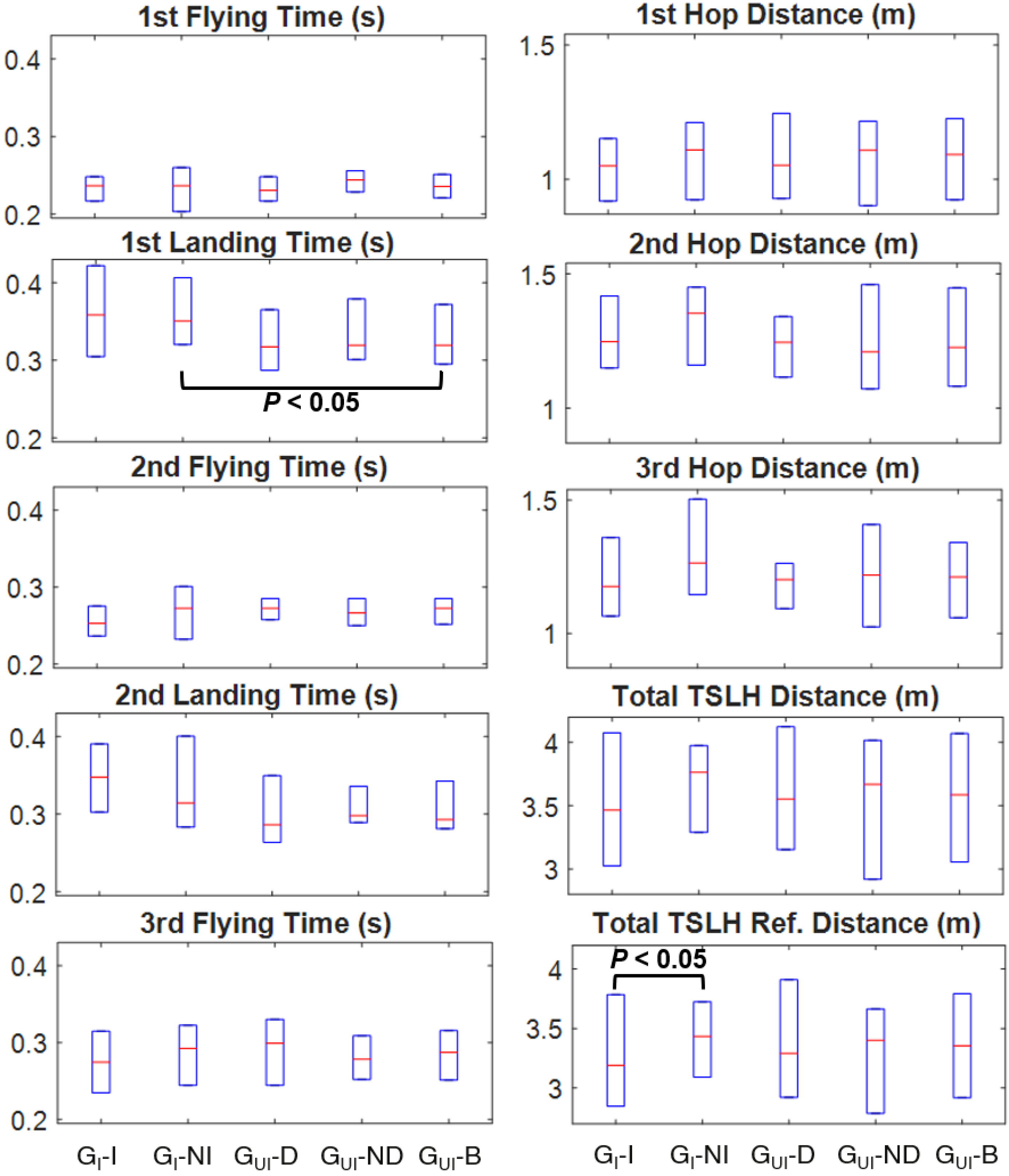
3.2. Comparison of Temporospatial Results among Injured and Uninjured Youth
3.3. Correlations between the KOOS and Temporospatial Parameters in Injured Youth
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef]
- Andriacchi, T.P.; Mündermann, A.; Smith, R.L.; Alexander, E.J.; Dyrby, C.O.; Koo, S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann. Biomed. Eng. 2004, 32, 447–457. [Google Scholar] [CrossRef]
- Schmitt, L.C.; Paterno, M.V.; Hewett, T.E. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 2012, 42, 750–759. [Google Scholar] [CrossRef]
- Van Melick, N.E.; Van Cingel, R.E.H.; Tienen, T.G. Van Functional performance 2–9 years after ACL reconstruction: Cross-sectional comparison between athletes with bone-patellar tendon-bone, semitendinosus/gracilis and healthy controls. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Xergia, S.A.; Pappas, E.; Zampeli, F.; Georgiou, S.; Georgoulis, A.D. Asymmetries in Functional Hop Tests, Lower Extremity Kinematics, and Isokinetic Strength Persist 6 to 9 Months Following Anterior Cruciate Ligament Reconstruction. J. Orthop. Sports Phys. Ther. 2013, 43, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Xergia, S.A.; Pappas, E.; Georgoulis, A.D. Association of the single-limb hop test with isokinetic, kinematic, and kinetic asymmetries in patients after anterior cruciate ligament reconstruction. Sports Health 2014, 7, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Wellsandt, E.; Gardinier, E.S.; Manal, K.; Axe, M.J.; Buchanan, T.S.; Snyder-Mackler, L. Decreased knee joint loading associated with early knee osteoarthritis after anterior cruciate ligament injury. Am. J. Sports Med. 2016, 44, 143–151. [Google Scholar] [CrossRef]
- Tyler Hamilton, R.; Shultz, S.J.; Schmitz, R.J.; Perrin, D.H. Triple-hop distance as a valid predictor of lower limb strength and power. J. Athl. Train. 2008, 43, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Logerstedt, D.; Grindem, H.; Lynch, A.; Eitzen, I.; Engebretsen, L.; Risberg, M.A.; Axe, M.J.; Snyder-mackler, L. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2012, 40, 2348–2356. [Google Scholar] [CrossRef]
- Button, K.; Roos, P.E.; Van Deursen, R.W.M. Activity progression for anterior cruciate ligament injured individuals. Clin. Biomech. 2014, 29, 206–212. [Google Scholar] [CrossRef][Green Version]
- van der Harst, J.J.; Gokeler, A.; Hof, A.L. Leg kinematics and kinetics in landing from a single-leg hop for distance. A comparison between dominant and non-dominant leg. Clin. Biomech. 2007, 22, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Gokeler, A.; Hof, A.L.; Arnold, M.P.; Dijkstra, P.U.; Postema, K.; Otten, E. Abnormal landing strategies after ACL reconstruction. Scand. J. Med. Sci. Sport 2010, 20, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, G.K.; Lephart, S.M.; Hwang, J.H.; Wainner, M.R.S. Hop Tests as Predictors of Dynamic Knee Stability. J. Orthop. Sports Phys. Ther. 2001, 31, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Orishimo, K.F.; Kremenic, I.J. Effect of fatigue on single-leg hop landing biomechanics. J. Appl. Biomech. 2006, 22, 245–254. [Google Scholar] [CrossRef]
- Kotsifaki, A.; Korakakis, V.; Whiteley, R.; Van Rossom, S.; Jonkers, I. Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 1–16. [Google Scholar] [CrossRef]
- Petschnig, R.; Baron, R.; Albrecht, M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 1998, 28, 23–31. [Google Scholar] [CrossRef]
- Wren, T.A.L.; Mueske, N.M.; Brophy, C.H.; Pace, J.L.; Katzel, M.J.; Edison, B.R.; VandenBerg, C.D.; Zaslow, T.L. Hop distance symmetry does not indicate normal landing biomechanics in adolescent athletes with recent anterior cruciate ligament reconstruction. J. Orthop. Sports Phys. Ther. 2018, 1–23. [Google Scholar] [CrossRef]
- Sabatini, A.M. Quaternion-based strap-down integration method for applications of inertial sensing to gait analysis. Med. Biol. Eng. Comput. 2005, 43, 94–101. [Google Scholar] [CrossRef]
- Mariani, B.; Hoskovec, C.; Rochat, S.; Büla, C.; Penders, J.; Aminian, K. 3D gait assessment in young and elderly subjects using foot-worn inertial sensors. J. Biomech. 2010, 43, 2999–3006. [Google Scholar] [CrossRef]
- Peruzzi, A.; Croce, U.D.; Cereatti, A. Estimation of stride length in level walking using an inertial measurement unit attached to the foot: A validation of the zero velocity assumption during stance. J. Biomech. 2011, 44, 1991–1994. [Google Scholar] [CrossRef]
- Aminian, K.; Najafi, B.; Büla, C.; Leyvraz, P.-F.; Robert, P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J. Biomech. 2002, 35, 689–699. [Google Scholar] [CrossRef]
- Salarian, A.; Russmann, H.; Vingerhoets, F.J.G.; Dehollain, C.; Blanc, Y.; Burkhard, P.R.; Aminian, K. Gait assessment in Parkinson’s disease: Toward an ambulatory system for long-term monitoring. IEEE Trans. Biomed. Eng. 2004, 51, 1434–1443. [Google Scholar] [CrossRef] [PubMed]
- Mariani, B.; Rouhani, H.; Crevoisier, X.; Aminian, K. Quantitative estimation of foot-flat and stance phase of gait using foot-worn inertial sensors. Gait Posture 2013, 37, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Boutaayamou, M.; Schwartz, C.; Stamatakis, J.; Denoël, V.; Maquet, D.; Forthomme, B.; Croisier, J.; Macq, B.; Verly, J.G.; Garraux, G.; et al. Development and validation of an accelerometer-based method for quantifying gait events. Med. Eng. Phys. J. 2015, 37, 226–232. [Google Scholar] [CrossRef]
- Dowling, A.V.; Favre, J.; Andriacchi, T.P. A wearable system to assess risk for anterior cruciate ligament injury during jump landing: Measurements of temporal events, jump height, and sagittal plane kinematics. J. Biomech. Eng. 2011, 133, 071008. [Google Scholar] [CrossRef]
- Setuain, I.; González-Izal, M.; Alfaro, J.; Gorostiaga, E.; Izquierdo, M. Acceleration and orientation jumping performance differences among elite professional male handball players with or without previous ACL reconstruction: An inertial sensor unit-based study. PM R 2015, 7, 1243–1253. [Google Scholar] [CrossRef]
- Quagliarella, L.; Sasanelli, N.; Belgiovine, G.; Moretti, L. Evaluation of standing vertical jump by ankles acceleration measurement. J. Strength Cond. Res. 2010, 24, 23–27. [Google Scholar] [CrossRef]
- Cappozzo, A.; Catani, F.; Della Croce, U.; Leardini, A. Position and orietnation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Roos, E.M.; Lohmander, L.S. The Knee Injury and Osteoarthritis Outcome Score (KOOS): From Joint Injury to Osteoarthritis. Health Qual. Life Outcomes 2003, 1, 64. [Google Scholar] [CrossRef]
- Cappozzo, A.; Della Croce, U.; Leardini, A.; Chiari, L. Human movement analysis using stereophotogrammetry. Part 1: Theoretical background. Gait Posture 2005, 21, 186–196. [Google Scholar] [CrossRef]
- Alton, F.; Baldey, L.; Caplan, S.; Morrissey, M.C. A kinematic comparison of overground and treadmill walking. Clin. Biomech. 1998, 13, 434–440. [Google Scholar] [CrossRef]
- Fellin, R.E.; Rose, W.C.; Royer, T.D.; Davis, I.S. Comparison of methods for kinematic identification of footstrike and toe-off during overground and treadmill running. J. Sci. Med. Sport 2010, 13, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Preece, S.; Mason, D.; Bramah, C. A comparison of kinematic algorithms to estimate gait events during overground running. Gait Posture 2015, 41, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Noamani, A.; Nazarahari, M.; Lewicke, J.; Vette, A.H.; Rouhani, H. Validity of using wearable inertial sensors for assessing the dynamics of standing balance. Med. Eng. Phys. 2020, 77, 53–59. [Google Scholar] [CrossRef]
- Rouhani, H.; Favre, J.; Crevoisier, X.; Aminian, K. Measurement of multi-segment foot joint angles during gait using a wearable system. J. Biomech. Eng. 2012, 134, 061006. [Google Scholar] [CrossRef]
- Swinscow, T.D.V. Statistics at Square One, 11th ed.; Campbell, M.J., Ed.; BMJ Publishing Group: London, UK, 2009. [Google Scholar]
- Fasel, B.; Spörri, J.; Schütz, P.; Lorenzetti, S.; Aminian, K. Validation of functional calibration and strap-down joint drift correction for computing 3D joint angles of knee, hip, and trunk in alpine skiing. PLoS ONE 2017, 12, e0181446. [Google Scholar] [CrossRef]
- Collins, N.J.; Prinsen, C.A.C.; Christensen, R.; Bartels, E.M.; Terwee, C.B.; Roos, E.M. Knee Injury and Osteoarthritis Outcome Score ( KOOS ): Systematic review and meta-analysis of measurement properties. Osteoarthr. Cartil. 2016, 24, 1317–1329. [Google Scholar] [CrossRef]
- Whittaker, J.L.; Woodhouse, L.J.; Nettel-aguirre, A.; Emery, C.A. Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3–10 years following knee joint injury in youth sport. Osteoarthr. Cartil. 2015, 23, 1122–1129. [Google Scholar] [CrossRef]



| Characteristics | Criterion-Related Validation (n = 10) | Construct Validation (n = 32) | ||
|---|---|---|---|---|
| Injured (n = 0) | Uninjured (n = 10) | Injured 1 (n = 22) | Uninjured 1 (n = 10) | |
| Sex (W/M) | - | 0W/10M | 17W/5M | 9W/1M |
| Age 2 (years) | - | 23 ± 3 | 16 ± 1 | 17 ± 2 |
| Height 2 (cm) | - | 177 ± 10 | 167 ± 12 | 171 ± 9 |
| Body Mass 2 (kg) | - | 68 ± 8 | 60 ± 14 | 65 ± 10 |
| Dominant Leg (R/L) | - | 10R/0L | 19R/3L | 10R/0L |
| Injured Leg (R/L) | - | - | 12R/10L | - |
| KOOS Symptom 2 | - | - | 84 ± 16 | 95 ± 6 |
| KOOS ADL 2 | - | - | 99 ± 4 | 100 ± 0 |
| KOOS Pain 2 | - | - | 90 ± 14 | 100 ± 0 |
| KOOS Sport/Rec 2 | - | - | 85 ± 20 | 100 ± 0 |
| KOOS QoL 2 | - | - | 50 ± 30 | 100 ± 5 |
| Validated Parameter | Error 1 | |||||
|---|---|---|---|---|---|---|
| (25% | 50% | 75%) | (25% | 50% | 75%) | |
| Temporal Parameters | Error 1 (ms and sample) | Absolute Error 1 (ms and sample) | ||||
| Initial Contact Instants | [−10(−1) | 2(0) | 12(1)] | [4(0) | 12(1) | 20(2)] |
| Terminal Contact Instants | [−8(−1) | 12(1) | 16(2)] | [10(1) | 14(1) | 20(2)] |
| Flying Times | [−12(−1) | −4(0) | 6(1)] | [6(1) | 10(1) | 18(2)] |
| Landing Times | [−4(0) | 6(1) | 14(1)] | [4(0) | 10(1) | 20(2)] |
| Forward Progression Distances | Relative Error (%) 1 | Absolute Error (cm) 1 | ||||
| First Hops | [3.62 | 5.50 | 6.31] | [4.46 | 6.11 | 7.17] |
| Second Hops | [1.71 | 3.05 | 6.52] | [1.90 | 3.82 | 7.54] |
| Third Hops | [2.15 | 5.64 | 8.65] | [2.39 | 7.39 | 10.78] |
| All Individual Hops 2 | [2.08 | 4.44 | 7.69] | [2.42 | 5.41 | 9.77] |
| Total TSLH Progression 2 | [1.03 | 2.40 | 4.01] | [3.83 | 9.35 | 14.12] |
| KOOS Subscale | Time | Time Asymmetry 1 | ||||||||
| Fly 1 | Land 1 | Fly 2 | Land 2 | Fly 3 | Fly 1 | Land 1 | Fly 2 | Land 2 | Fly 3 | |
| Symptom | 0.166 | 0.003 | 0.660 | 0.055 | 0.381 | −0.117 | 0.049 | −0.536 | 0.245 | 0.016 |
| ADL | 0.390 | −0.027 | 0.448 | 0.085 | 0.157 | −0.225 | 0.254 | −0.366 | 0.291 | 0.044 |
| Pain | 0.126 | 0.052 | 0.253 | 0.095 | −0.056 | −0.054 | −0.014 | −0.148 | 0.082 | 0.317 |
| Sport/Rec | 0.117 | −0.035 | 0.401 | −0.075 | 0.067 | −0.070 | 0.109 | −0.363 | 0.357 | 0.108 |
| QoL | 0.001 | −0.150 | −0.062 | −0.005 | −0.158 | −0.249 | 0.338 | −0.137 | 0.328 | −0.121 |
| KOOS Subscale | Distance | Distance Asymmetry 2 | ||||||||
| Hop 1 | Hop 2 | Hop 3 | TSLH Total | TSLH Total (Ref.) 3 | Hop 1 | Hop 2 | Hop 3 | TSLH Total | TSLH Total (Ref.) 3 | |
| Symptom | 0.403 | 0.485 | 0.502 | 0.494 | 0.502 | 0.259 | −0.201 | 0.312 | 0.177 | 0.414 |
| ADL | 0.429 | 0.414 | 0.327 | 0.407 | 0.422 | 0.178 | −0.407 | 0.181 | 0.024 | 0.324 |
| Pain | 0.245 | 0.175 | 0.206 | 0.222 | 0.253 | 0.115 | −0.402 | 0.137 | −0.044 | 0.170 |
| Sport/Rec | 0.308 | 0.259 | 0.157 | 0.273 | 0.263 | 0.168 | −0.363 | 0.087 | −0.039 | 0.231 |
| QoL | 0.119 | 0.203 | 0.222 | 0.151 | 0.239 | −0.041 | −0.545 | 0.071 | −0.156 | 0.059 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmadian, N.; Nazarahari, M.; Whittaker, J.L.; Rouhani, H. Quantification of Triple Single-Leg Hop Test Temporospatial Parameters: A Validated Method Using Body-Worn Sensors for Functional Evaluation after Knee Injury. Sensors 2020, 20, 3464. https://doi.org/10.3390/s20123464
Ahmadian N, Nazarahari M, Whittaker JL, Rouhani H. Quantification of Triple Single-Leg Hop Test Temporospatial Parameters: A Validated Method Using Body-Worn Sensors for Functional Evaluation after Knee Injury. Sensors. 2020; 20(12):3464. https://doi.org/10.3390/s20123464
Chicago/Turabian StyleAhmadian, Niloufar, Milad Nazarahari, Jackie L. Whittaker, and Hossein Rouhani. 2020. "Quantification of Triple Single-Leg Hop Test Temporospatial Parameters: A Validated Method Using Body-Worn Sensors for Functional Evaluation after Knee Injury" Sensors 20, no. 12: 3464. https://doi.org/10.3390/s20123464
APA StyleAhmadian, N., Nazarahari, M., Whittaker, J. L., & Rouhani, H. (2020). Quantification of Triple Single-Leg Hop Test Temporospatial Parameters: A Validated Method Using Body-Worn Sensors for Functional Evaluation after Knee Injury. Sensors, 20(12), 3464. https://doi.org/10.3390/s20123464





