Ubiquitous Emergency Medical Service System Based on Wireless Biosensors, Traffic Information, and Wireless Communication Technologies: Development and Evaluation
Abstract
:1. Introduction
- Management of wires in the ambulance: in the delivery of first-aid to patients, sensor wires may cause inconvenience for patients and healthcare providers.
- Ubiquitous accessibility of the patient’s biosignals in remote areas where the ambulance cannot arrive: this would delay the first-aid.
- Availability of real-time traffic information: Without real-time traffic information, the ambulance cannot reach the accident site in the shortest time.
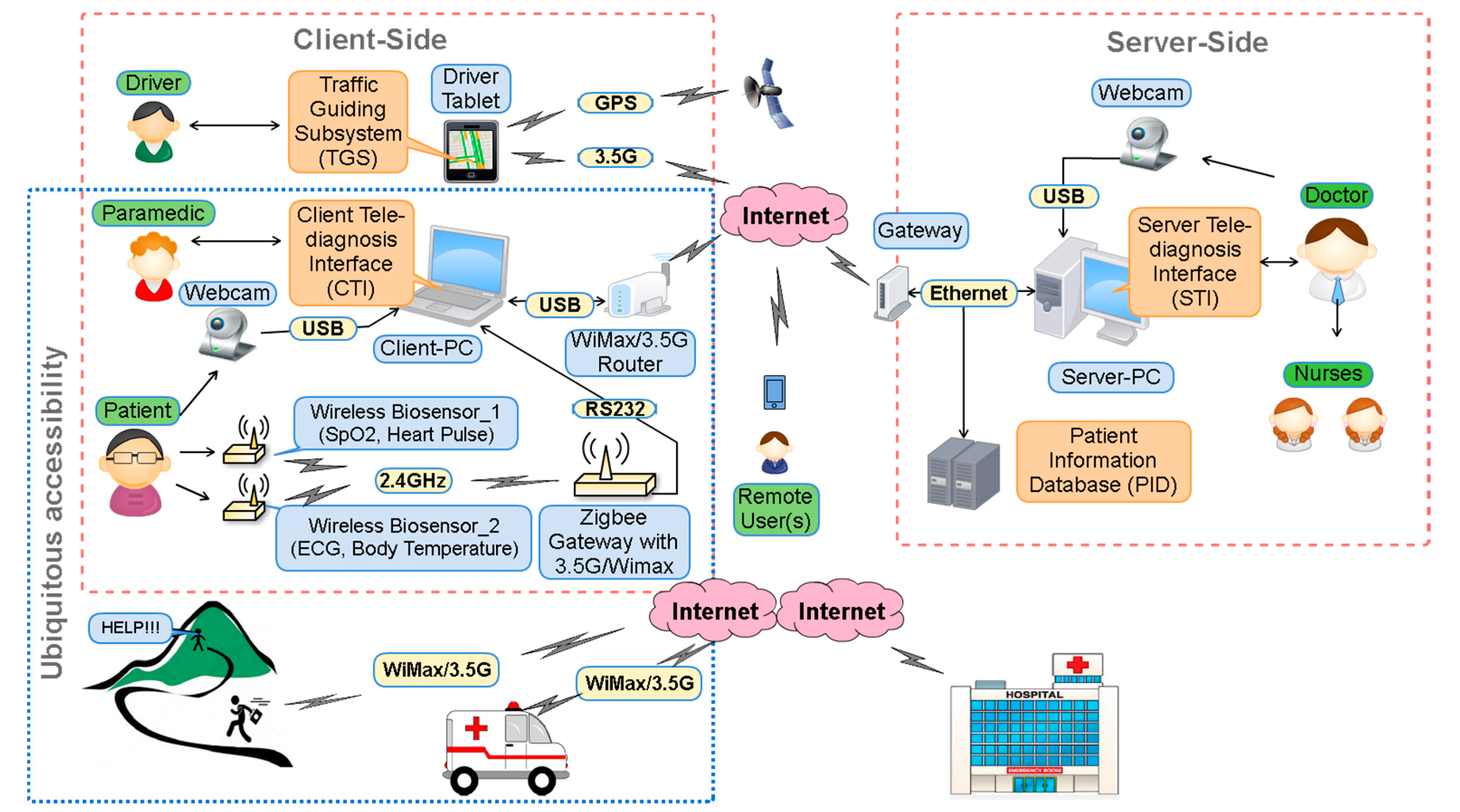
2. Materials and Methods
2.1. Wireless Sensors and Remote Accessibility
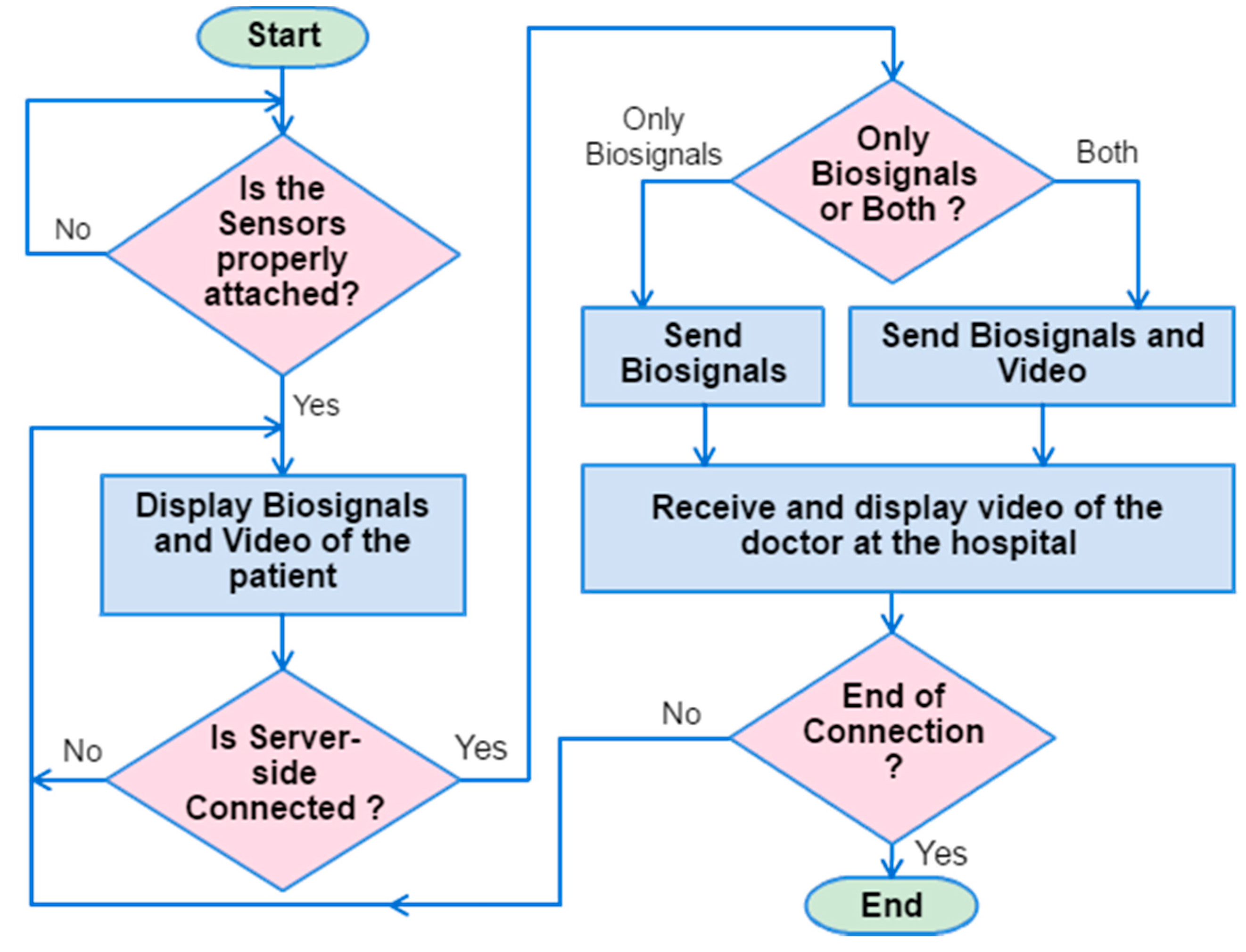
2.2. Client Tele-Diagnosis Interface
2.3. Server Tele-Diagnosis Interface
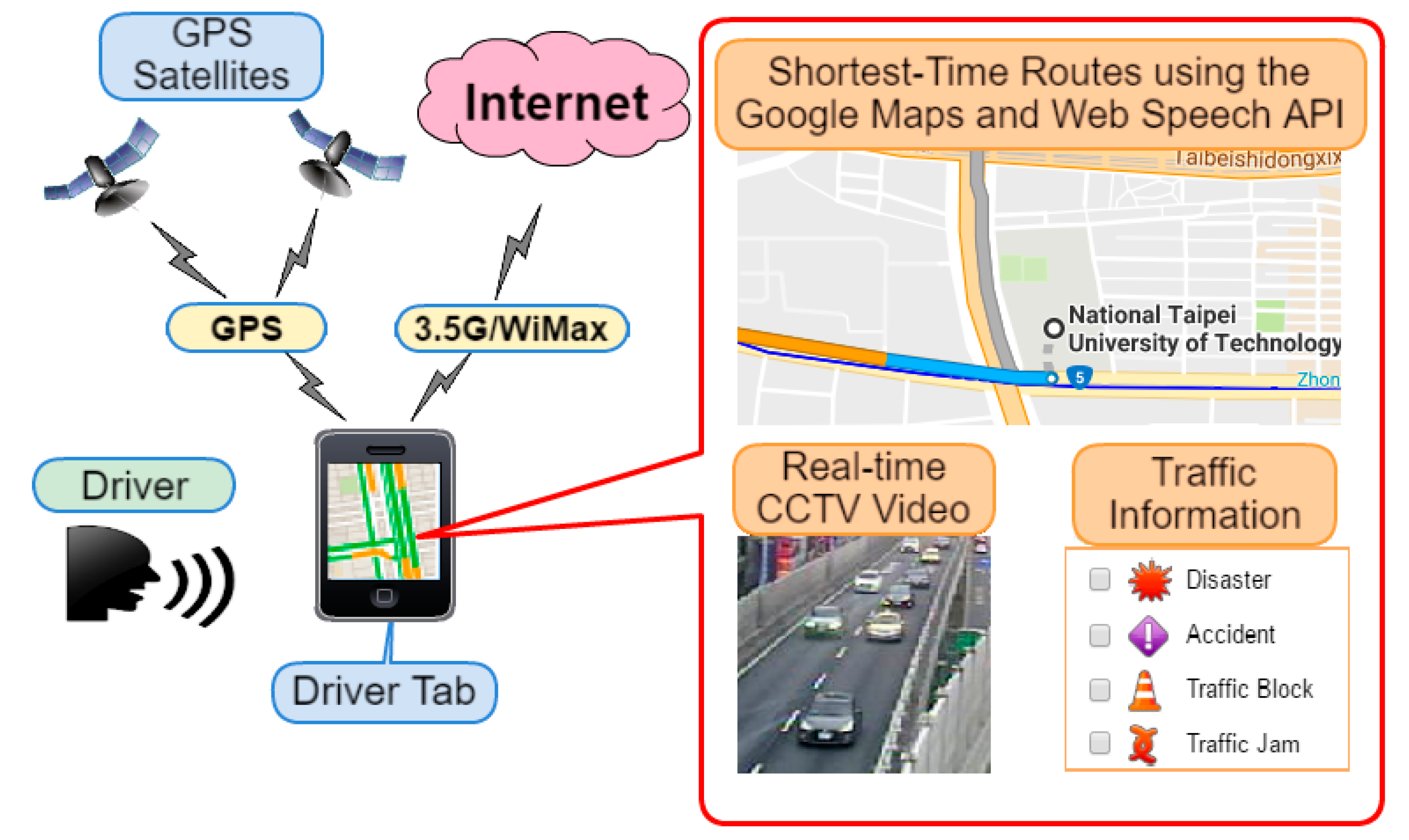
2.4. Traffic Guiding Subsystem
3. Results
3.1. Initialization Time
3.2. Data Rate
3.3. End-to-End Delay
3.4. Response and Delivery Time
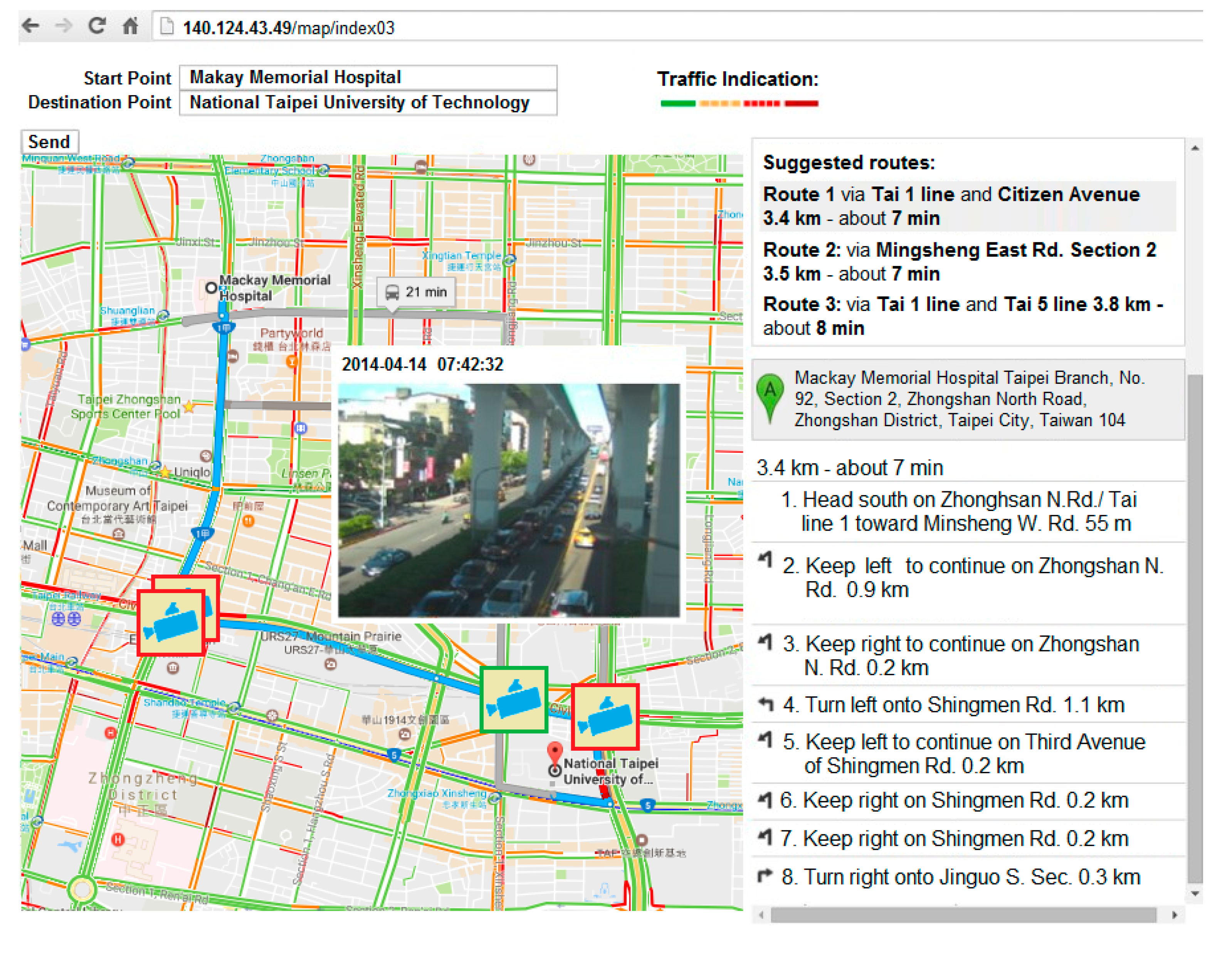
3.4.1. Experimental Setup
- 1
- Locations: The patient and hospital sites are determined a priori as, respectively, National Taipei University of Technology and Mackay Memorial Hospital.
- 2
- Dates of experiments: 14, 16 and 18 April 2014 (Monday, Wednesday, and Friday). The experimental period consists of three shorter periods: morning rush hour (7:30–8:30 a.m.), noon off-peak hour (12:00 p.m.–1:00 p.m.) and afternoon rush hour (5:30–6:30 p.m.). Traffic conditions are based on the travelling speed: above 60 km/h is specified as clear; 40–60 km/h is specified as semi-congested, and less than 40 km/h is specified as congested.
- 3
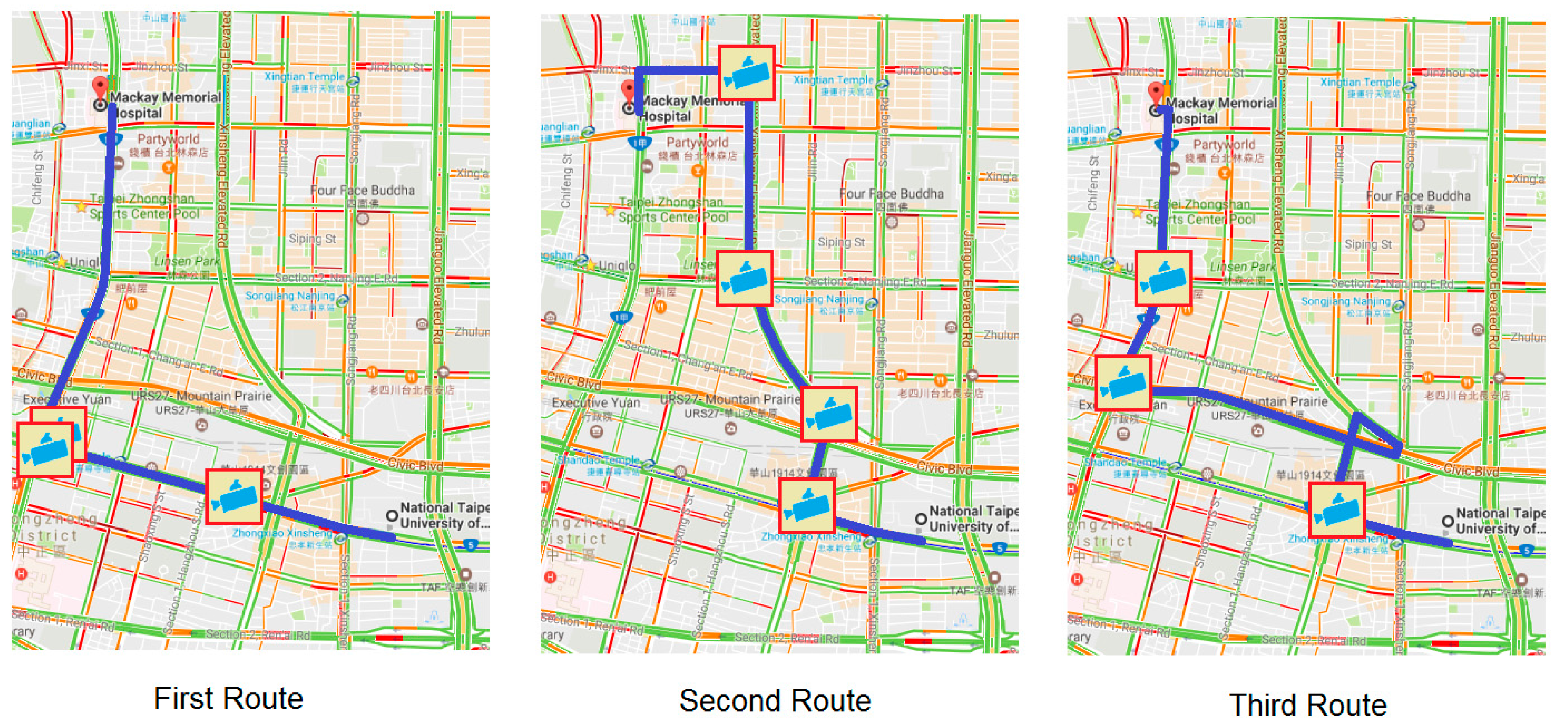
- Experimental methods: Two ambulances are involved on different routes (Route 1, Route 2). Route 1 is the first route among the three suggested routes by GMs; Route 2 is a chosen route by the driver after his inspection of the traffic condition. Thus, Route 2 can be the same as Route 1 if the traffic condition of Route 1 is good. Three different routes are suggested by GMs for the response (see Figure 8) and for the delivery (see Figure 9) routes. Both ambulances simultaneously departed from the same location and a stopwatch was used to record their time.
3.4.2. Case I
3.4.3. Case II
3.4.4. Case III
3.5. Speech Recognition
4. Discussion
5. Conclusions and Future Work
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Castrén, M.; Karlsten, R.; Lippert, F.; Christensen, E.F.; Bovim, E.; Kvam, A.M.; Robertson-Steel, I.; Overton, J.; Kraft, T.; Engerstrom, L.; et al. Recommended guidelines for reporting on emergency medical dispatch when conducting research in emergency medicine: The Utstein style. Resuscitation 2008, 79, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Pons, P.T.; Markovchick, V.J. Eight minutes or less: Does the ambulance response time guideline impact trauma patient outcome? J. Emerg. Med. 2002, 23, 43–48. [Google Scholar] [CrossRef]
- Marsden, A.K. Getting the right ambulance to the right patient at the right time. Accid. Emerg. Nurs. 1995, 3, 177–183. [Google Scholar] [CrossRef]
- O’Keeffe, C.; Nicholl, J.; Turner, J.; Goodacre, S. Role of ambulance response times in the survival of patients with out-of-hospital cardiac arrest. Emerg. Med. J. 2011, 28, 703–706. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Mangas, R.; García-Ferrrer, A.; De Juan, A.; Arroyo, A.M. The probability of death in road traffic accidents. How important is a quick medical response? Accid. Anal. Prev. 2010, 42, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, R.P.; Cummings, G.R.; Phelan, H.A.; Mulekar, M.S.; Rodning, C.B. Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis. Am. J. Surg. 2009, 197, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Vukmir, R.B. Survival from prehospital cardiac arrest is critically dependent upon response time. Resuscitation 2006, 69, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Kyriacou, E.; Pavlopoulos, S.; Berler, A.; Neophytou, M.; Bourka, A.; Georgoulas, A.; Anagnostaki, A.; Karayiannis, D.; Schizas, C.; Pattichis, C.; et al. Multi-purpose HealthCare Telemedicine Systems with mobile communication link support. Biomed. Eng. Online 2003, 2, 7. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.; Ganz, A. A mobile teletrauma system using 3G networks. IEEE Trans. Inf. Technol. Biomed. 2004, 8, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Mandellos, G.J.; Lymperopoulos, D.K.; Koukias, M.N.; Tzes, A.; Lazarou, N.; Vagianos, C. A novel mobile telemedicine system for ambulance transport. Design and evaluation. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; pp. 3080–3083.
- Thelen, S.; Czaplik, M.; Meisen, P.; Schilberg, D.; Jeschke, S. Using off-the-shelf medical devices for biomedical signal monitoring in a telemedicine system for emergency medical services. IEEE J. Biomed. Heal. Inform. 2015, 19, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Alesanco, Á.; García, J. Clinical assessment of wireless ECG transmission in real-time cardiac telemonitoring. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 1144–1152. [Google Scholar] [CrossRef] [PubMed]
- Su, M.J.; Huei-Ming, M.; Ko, C.I.; Chiang, W.C.; Yang, C.W.; Chen, S.J.; Chen, R.; Chen, H.S. Application of tele-ultrasound in medical emergency services. In Proceedings of the IEEE 10th International Conference on HealthCom, Singapore, 7–9 July 2008; pp. 66–67.
- Kang, J.; Shin, I.H.; Koo, Y.; Jung, M.Y.; Suh, G.J.; Kim, H.C. HSDPA (3.5G)-based ubiquitous integrated biotelemetry system for emergency care. In Proceeedings of 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 3665–3670.
- Niyato, D.; Hossain, E.; Diamond, J. IEEE 802.16/WiMAX-Based Broadband Wireless Access and its Application for Telemedicine/E-Health Services. IEEE Trans. Wirel. Commun. 2007, 14, 72–83. [Google Scholar] [CrossRef]
- Walter, S.; Kostopoulos, P.; Haass, A.; Keller, I.; Lesmeister, M.; Schlechtriemen, T.; Roth, C.; Papanagiotou, P.; Grunwald, I.; Schumacher, H.; et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: A randomised controlled trial. Lancet Neurol. 2012, 11, 397–404. [Google Scholar] [CrossRef]
- Felzen, M.; Brokmann, J.C.; Beckers, S.K.; Czaplik, M.; Hirsch, F.; Tamm, M.; Rossaint, R.; Bergrath, S. Improved technical performance of a multifunctional prehospital telemedicine system between the research phase and the routine use phase—An observational study. J. Telemed. Telecare 2016. [Google Scholar] [CrossRef] [PubMed]
- Tokuda, K.; Ohmori, S. Demonstration experiments of SAFER (Speedy Ambulance First-aid, Emergency, Rescue Operations Supporting) system. In Proceedings of the 14th International Symposium on Wireless Personal Multimedia Communications, Brest, France, 3–7 October 2011.
- Chen, C.Y.; Chen, P.Y.; Chen, W.T. A Novel Emergency Vehicle Dispatching System. In Proceedings of the 16th International Symposium on Wireless Personal Multimedia Communications, Atlantic City, NJ, USA, 24–27 June 2013.
- Lim, C.S.; Mamat, R.; Braunl, T. Impact of ambulance dispatch policies on performance of emergency medical services. IEEE Trans. Intell. Transp. Syst. 2011, 12, 624–632. [Google Scholar] [CrossRef]
- Buchenscheit, A.; Schaub, F.; Kargl, F.; Weber, M. A VANET-based emergency vehicle warning system. In Proceedings of the 2009 IEEE Vehicular Networking Conference, Tokyo, Japan, 28–30 October 2009.
- Chang, C.-S.; Tan, T.-H.; Chen, Y.-F.; Huang, Y.-F.; Lee, M.-H.; Hsu, J.-C.; Chen, H.-C. Development of a ubiquitous emergency medical service system based on zigbee and 3.5 G wireless communication technologies. In Proceedings of the Second International Conference, Hong Kong, China, 28–30 June 2010.
- Windows Sockets (Winsock). Available online: https://www.techopedia.com/definition/5030/windows-sockets-winsock (accessed on 25 September 2016).
- Web Speech API Specification. Available online: https://dvcs.w3.org/hg/speech-api/raw-file/tip/speechapi.html# speechreco-section (accessed on 25 September 2016).
- Google Traffic. Available online: https://en.wikipedia.org/wiki/Google_Traffic (accessed on 25 September 2016).
- Traffic Control Center in Taipei. Available online: http://tms.bote.taipei.gov.tw/ (accessed on 25 September 2016).
- NetLimiter Homepage. Available online: http://www.netlimiter.com/ (accessed on 25 September 2016).
- Molisch, A.F. Wireless Communications, 2nd ed.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2010. [Google Scholar]
- Hu, J.J. Development of an Emergency Medical Service (EMS) System Based on Real-Time Traffic Information. Master’s Thesis, Department of Electrical Engineering, National Taipei University of Technology, Taipei, Taiwan, 2011. [Google Scholar]
- Aguirre, E.; Iturri, P.L.; Azpilicueta, L.; de Miguel-Bilbao, S.; Ramos, V.; Gárate, U.; Falcone, F. Analysis of estimation of electromagnetic dosimetric values from non-ionizing radiofrequency fields in conventional road vehicle environments. Electromagn. Biol. Med. 2015, 34, 19–28. [Google Scholar] [CrossRef] [PubMed]
- DIGI XBee/XBee-PRO DigiMesh 2.4 Radio Frequency (RF) Module User Guide. Available online: http://www.digi.com/resources/documentation/digidocs/pdfs/90000991.pdf (accessed on 18 January 2017).





| Ambulance Driving Speed (km/h) | WiMAX (Mbits/s) | 3.5 G (Mbits/s) | Ratio RateWiMAX/Rate3.5G |
|---|---|---|---|
| 0 | 4.98 | 1.97 | 2.52 |
| 40–59 | 4.71 | 1.71 | 2.75 |
| 60–79 | 2.71 | 1.67 | 1.62 |
| 80–100 | 2.02 | 0.91 | 2.21 |
| Ambulance Driving Speed (km/h) | WiMAX (s) | 3.5 G (s) | Difference Time3.5G–TimeWiMax (s) |
|---|---|---|---|
| 0 | 0.100 | 0.254 | 0.154 |
| 40–59 | 0.106 | 0.292 | 0.186 |
| 60–79 | 0.185 | 0.299 | 0.114 |
| 80–100 | 0.248 | 0.549 | 0.301 |
| Execution Period | Response Time | Delivery Time | ||||
|---|---|---|---|---|---|---|
| Route 1 | Route 2 | Difference | Route 1 | Route 2 | Difference | |
| 7:30–8:30 a.m. | 694 s | 458 s | 236 s | 452 s | 349 s | 91 s |
| 12:00–1:00 p.m. | 402 s | 408 s | –6 s | 327 s | 333 s | –6 s |
| 5:30–6:30 p.m. | 756 s | 506 s | 250 s | 588 s | 432 s | 144 s |
| No. | Name (Address) in English |
|---|---|
| 1 | Taipei Fine Arts Museum (No. 181, Section 3, Zhongshan N. Road, Zhongshan Dist., Taipei City) |
| 2 | No. 181, Section 3, Zhongshan N. Road, Zhongshan Dist., Taipei City |
| 3 | National Taiwan University Hospital (No. 7, Chung Shan S. Road (Zhongshan S. Road, Zhongzheng Dist., Taipei City) |
| 4 | No. 7, Chung Shan S. Road (Zhongshan S. Rd, Zhongzheng Dist., Taipei City) |
| 5 | Taipei Zoo (No. 30, Section 2, Xinguang Road, Wenshan Dist., Taipei City) |
| 6 | No. 30, Section 2, Xinguang Road, Wenshan Dist., Taipei City |
| 7 | National Palace Museum (No. 221, Section 2, Zhishan Road, Shilin Dist., Taipei City) |
| 8 | No. 221, Section 2, Zhishan Road, Shilin Dist., Taipei City |
| 9 | Taipei 101 (No. 7, Section 5, Xinyi Road, Xinyi Dist., Taipei City) |
| 10 | No. 7, Section 5, Xinyi Road, Xinyi Dist., Taipei City |
© 2017 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, T.-H.; Gochoo, M.; Chen, Y.-F.; Hu, J.-J.; Chiang, J.Y.; Chang, C.-S.; Lee, M.-H.; Hsu, Y.-N.; Hsu, J.-C. Ubiquitous Emergency Medical Service System Based on Wireless Biosensors, Traffic Information, and Wireless Communication Technologies: Development and Evaluation. Sensors 2017, 17, 202. https://doi.org/10.3390/s17010202
Tan T-H, Gochoo M, Chen Y-F, Hu J-J, Chiang JY, Chang C-S, Lee M-H, Hsu Y-N, Hsu J-C. Ubiquitous Emergency Medical Service System Based on Wireless Biosensors, Traffic Information, and Wireless Communication Technologies: Development and Evaluation. Sensors. 2017; 17(1):202. https://doi.org/10.3390/s17010202
Chicago/Turabian StyleTan, Tan-Hsu, Munkhjargal Gochoo, Yung-Fu Chen, Jin-Jia Hu, John Y. Chiang, Ching-Su Chang, Ming-Huei Lee, Yung-Nian Hsu, and Jiin-Chyr Hsu. 2017. "Ubiquitous Emergency Medical Service System Based on Wireless Biosensors, Traffic Information, and Wireless Communication Technologies: Development and Evaluation" Sensors 17, no. 1: 202. https://doi.org/10.3390/s17010202
APA StyleTan, T.-H., Gochoo, M., Chen, Y.-F., Hu, J.-J., Chiang, J. Y., Chang, C.-S., Lee, M.-H., Hsu, Y.-N., & Hsu, J.-C. (2017). Ubiquitous Emergency Medical Service System Based on Wireless Biosensors, Traffic Information, and Wireless Communication Technologies: Development and Evaluation. Sensors, 17(1), 202. https://doi.org/10.3390/s17010202








