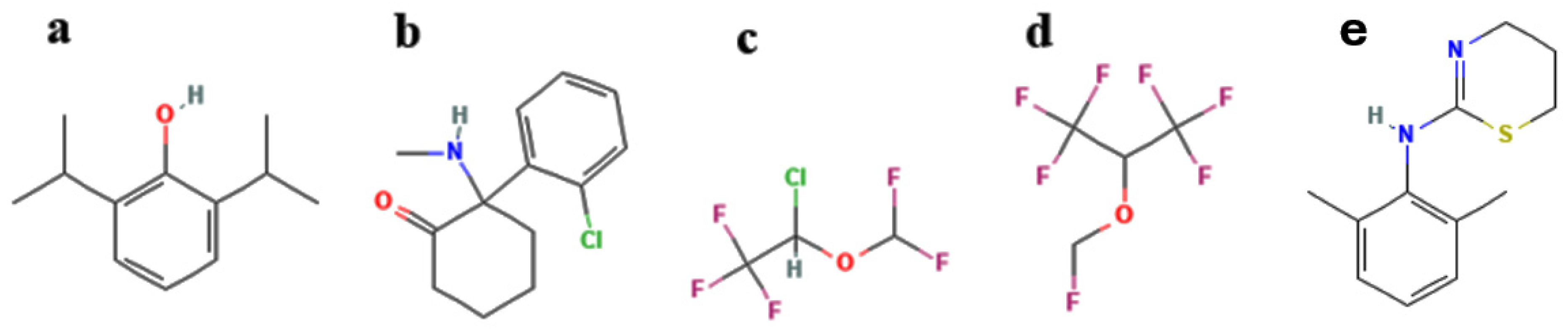
A Comparative Study of Common Anesthetics Propofol, Sevoflurane, Isoflurane and Ketamine on Lipid Membrane Fluidity
Abstract
1. Introduction
2. Results and Discussion
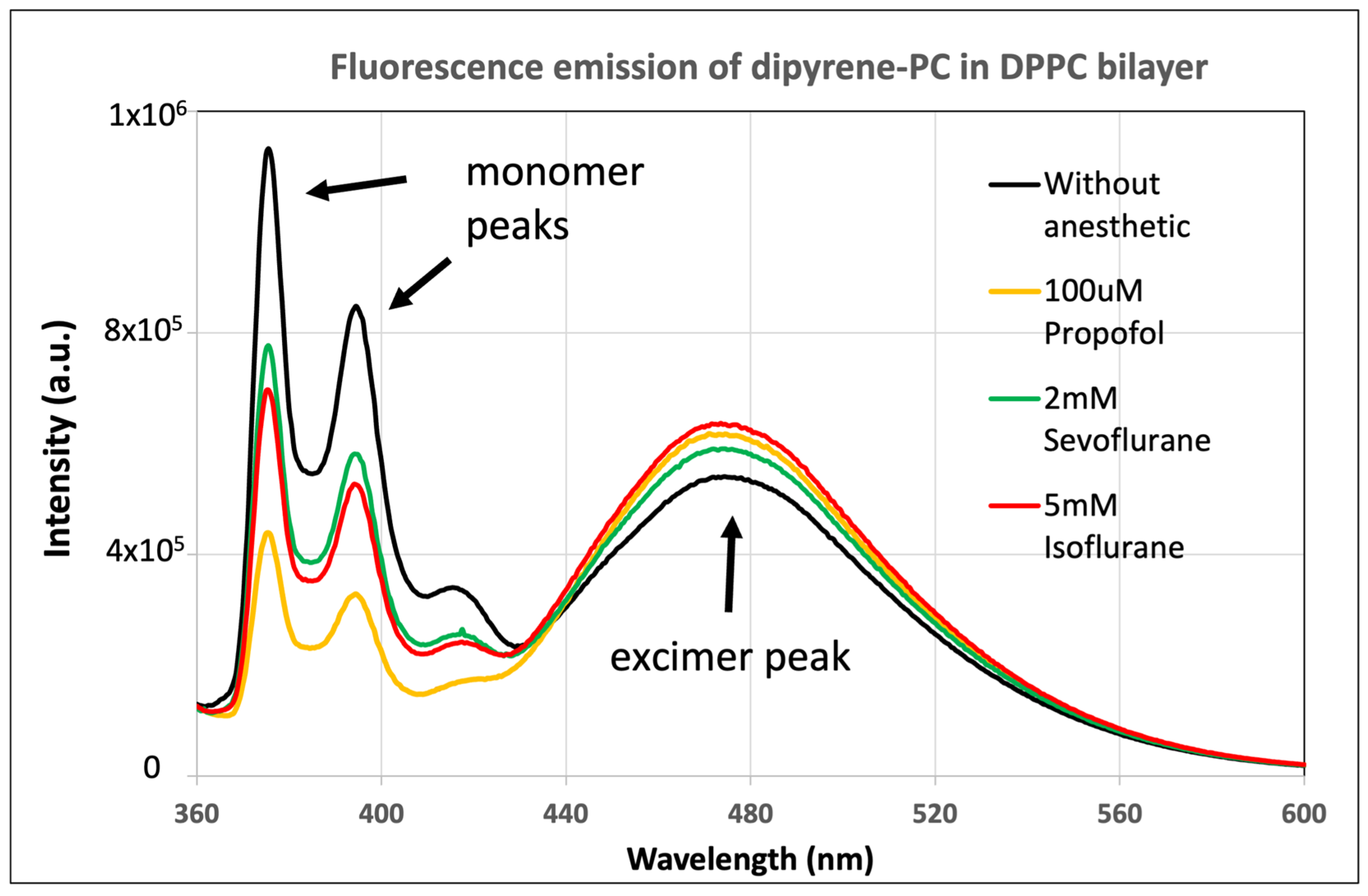
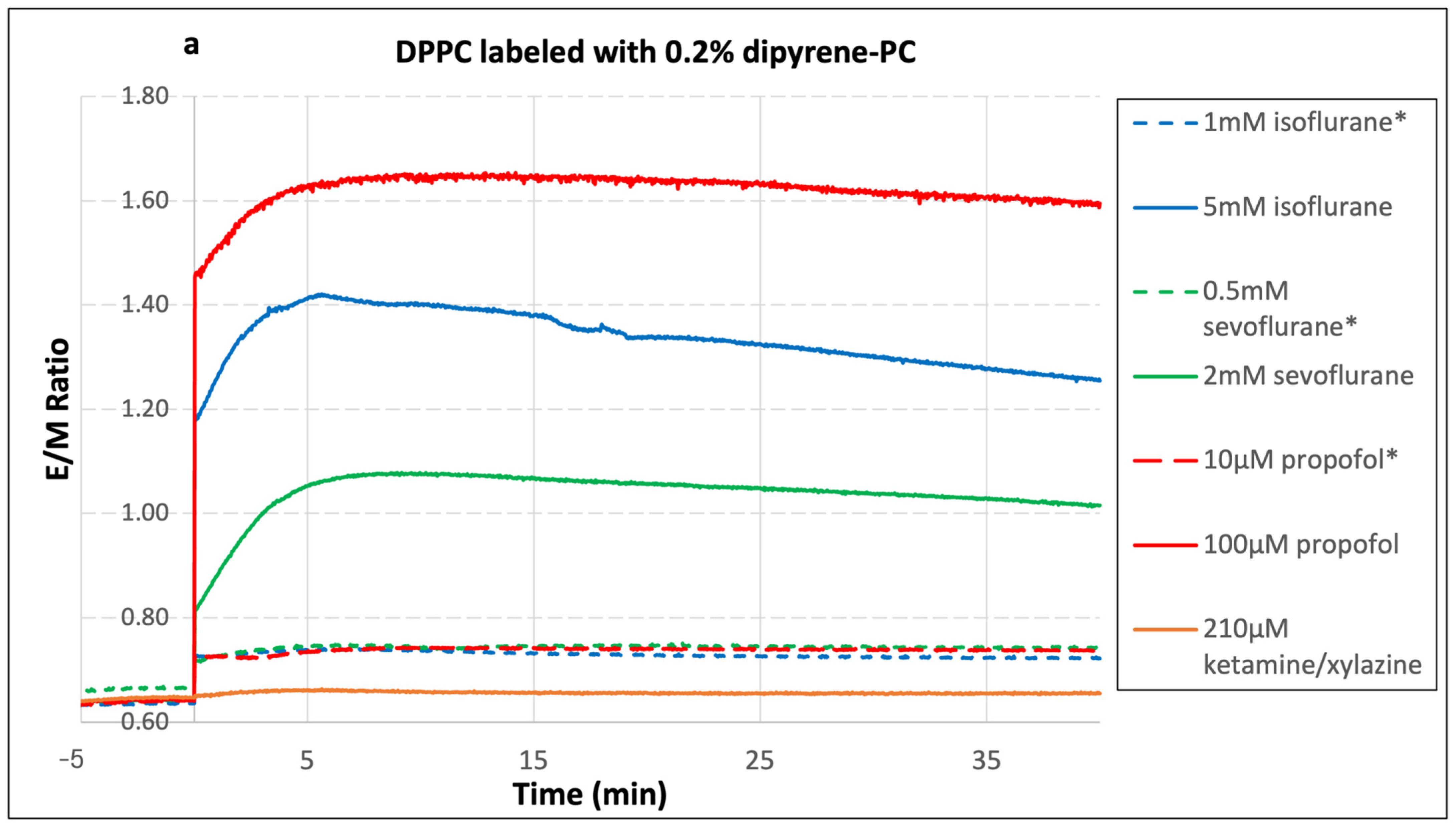
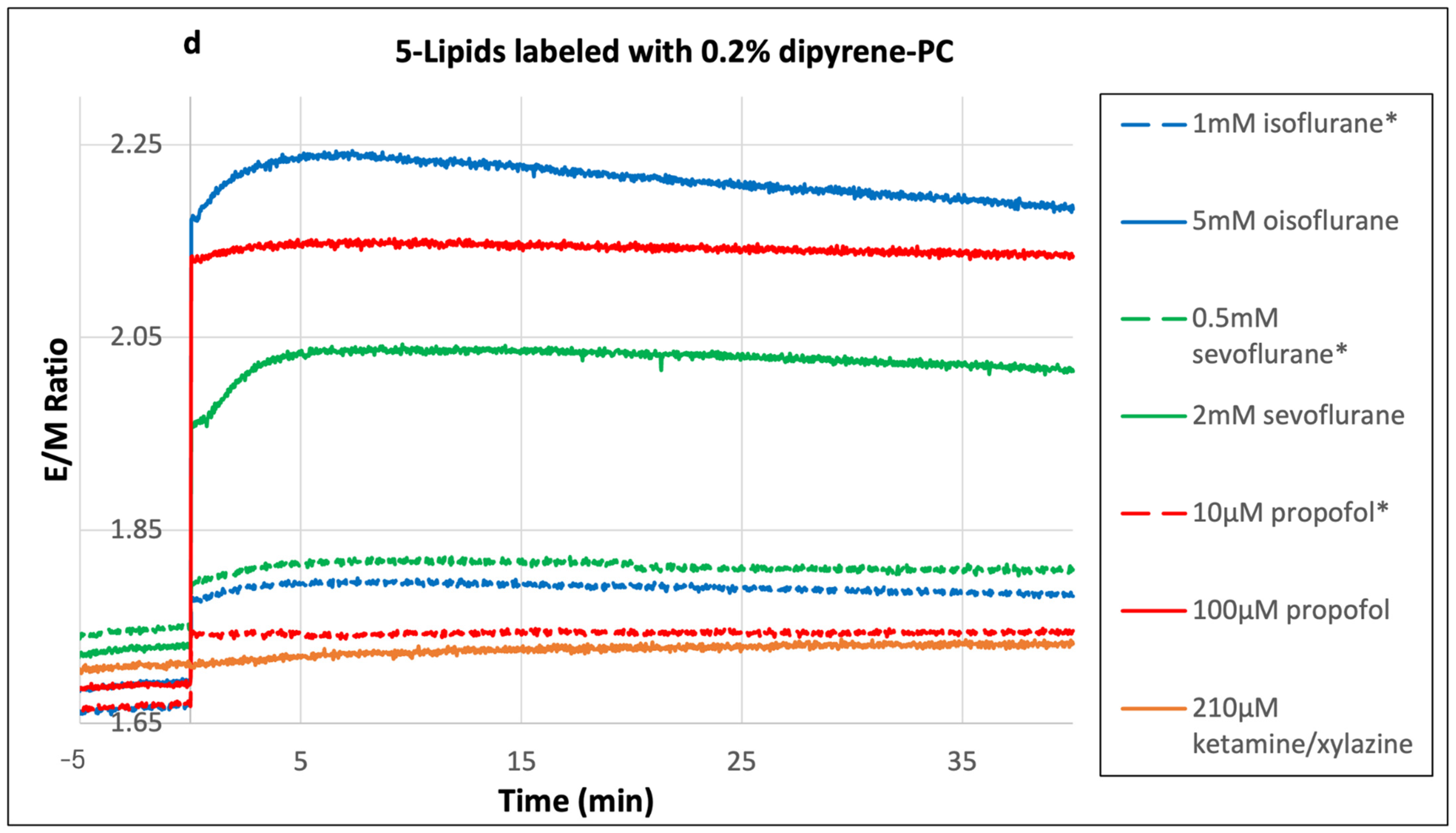
2.1. Dipyrene-PC E/M Ratio
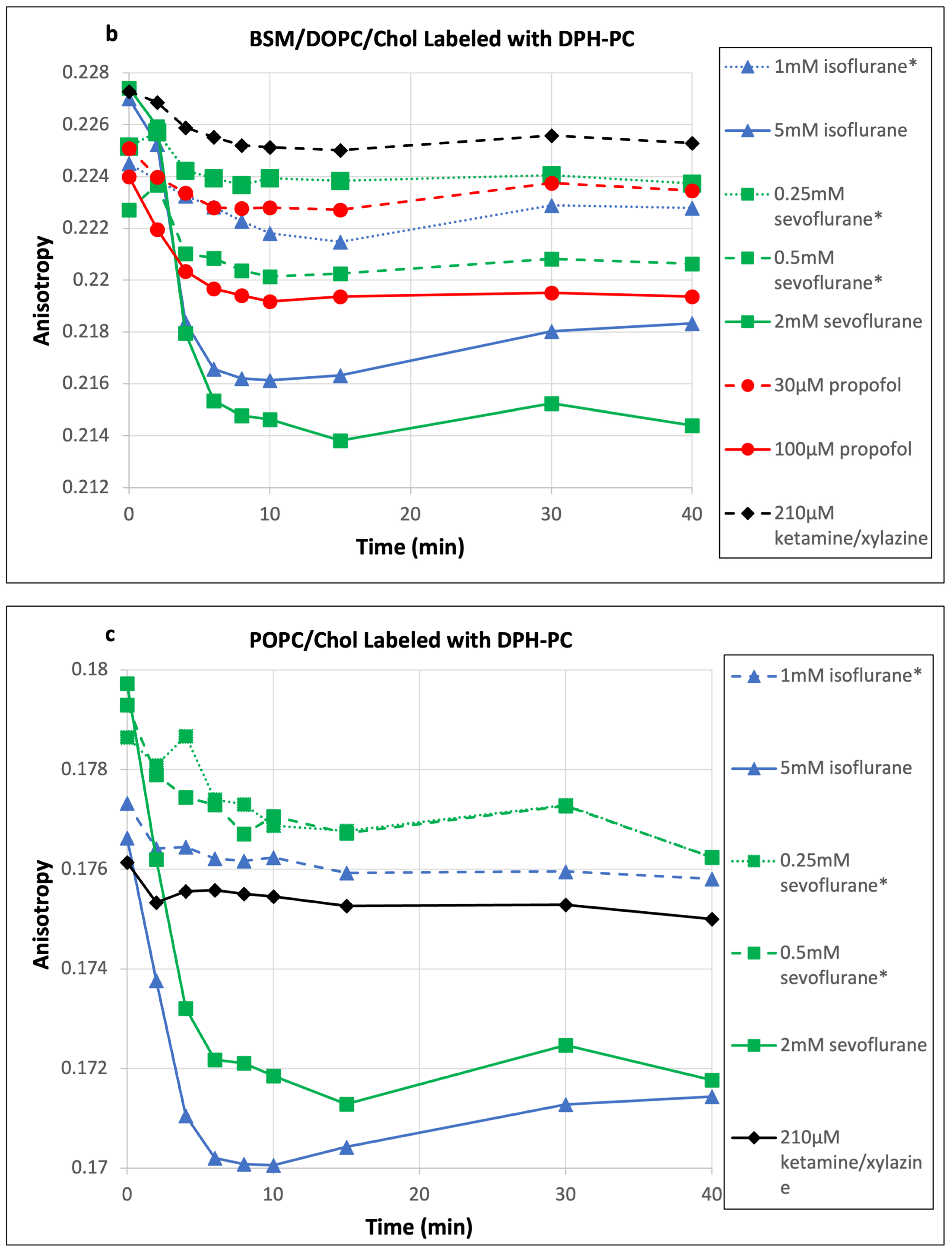
2.2. DPH-PC Anisotropy
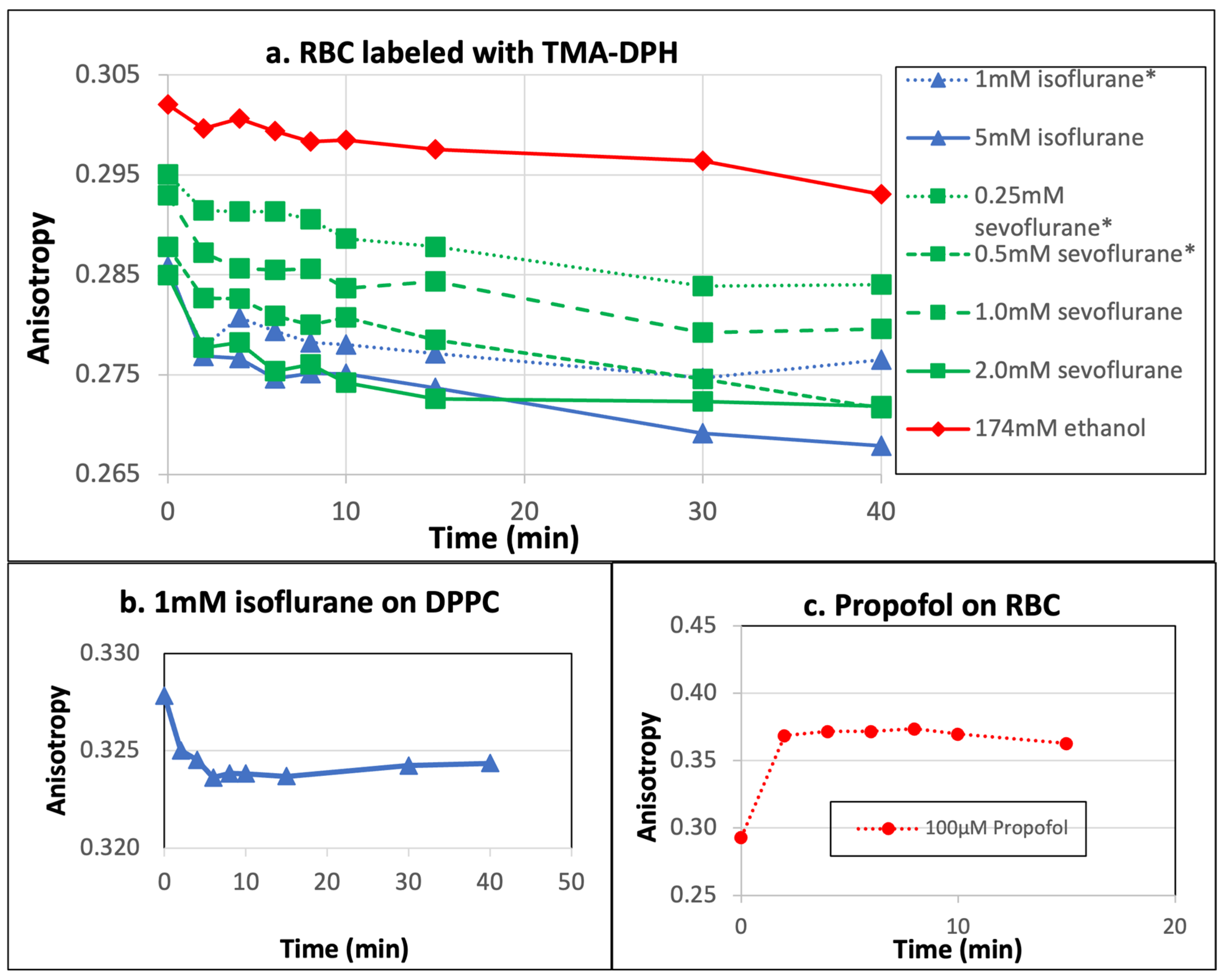
2.3. Fluorescence Anisotropy of Red Blood Cells
2.4. Sevoflurane and Isoflurane
2.5. Propofol
2.6. Ketamine
3. Materials and Methods
3.1. Preparation and Labeling of Liposomes
3.2. Excimer/Monomer (E/M) Ratio Measurements
3.3. Fluorescence Anisotropy Measurements
3.4. Washing and Labeling of Red Blood Cells (RBCs)
3.5. Measurement Protocol
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lenaz, G.; Curatola, G.; Mazzanti, L.; Parenti-Castelli, G.; Landi, L.; Sechi, A.M. A conformational model of the action of general anesthetics at the membrane level. III. Anesthetics and the properties of membrane-bound enzymes: Mitochondrial ATPase. Ital. J. Biochem. 1978, 27, 431–449. [Google Scholar]
- Mazzanti, L.; Curatola, G.; Zolese, G.; Bertoli, E.; Lenaz, G. Lipid protein interactions in mitochondria. VIII. Effect of general anesthetics on the mobility of spin labels in lipid vesicles and mitochondrial membranes. J. Bioenerg. Biomembr. 1979, 11, 17–32. [Google Scholar] [CrossRef]
- Trudell, J.R.; Payan, D.G.; Chin, J.H.; Cohen, E.N. The antagonistic effect of an inhalation anesthetic and high pressure on the phase diagram of mixed dipalmitoyl-dimyristoylphosphatidylcholine bilayers. Proc. Natl. Acad. Sci. USA 1975, 72, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, H. Structure-specific membrane-fluidizing effect of propofol. Clin. Exp. Pharmacol. Physiol. 2001, 28, 292–299. [Google Scholar] [CrossRef]
- Turkyilmaz, S.; Almeida, P.F.; Regen, S.L. Effects of isoflurane, halothane, and chloroform on the interactions and lateral organization of lipids in the liquid-ordered phase. Langmuir 2011, 27, 14380–14385. [Google Scholar] [CrossRef] [PubMed]
- Weinrich, M.; Worcester, D.L. Xenon and other volatile anesthetics change domain structure in model lipid raft membranes. J. Phys. Chem. B 2013, 117, 16141–16147. [Google Scholar] [CrossRef]
- Herold, K.F.; Sanford, R.L.; Lee, W.; Andersen, O.S.; Hemmings, H.C., Jr. Clinical concentrations of chemically diverse general anesthetics minimally affect lipid bilayer properties. Proc. Natl. Acad. Sci. USA 2017, 114, 3109–3114. [Google Scholar] [CrossRef]
- Daniell, L.C.; Harris, R.A. Neuronal intracellular calcium concentrations are altered by anesthetics: Relationship to membrane fluidization. J. Pharmacol. Exp. Ther. 1988, 245, 1–7. [Google Scholar] [CrossRef]
- Franks, N.P.; Lieb, W.R. Selective actions of volatile general anaesthetics at molecular and cellular levels. Br. J. Anaesth. 1993, 71, 65–76. [Google Scholar] [CrossRef]
- Harris, R.A.; Bruno, P. Membrane disordering by anesthetic drugs: Relationship to synaptosomal sodium and calcium fluxes. J. Neurochem. 1985, 44, 1274–1281. [Google Scholar] [CrossRef] [PubMed]
- Kopp Lugli, A.; Yost, C.S.; Kindler, C.H. Anaesthetic mechanisms: Update on the challenge of unravelling the mystery of anaesthesia. Eur. J. Anaesthesiol. 2009, 26, 807–820. [Google Scholar] [CrossRef]
- Richardson, C.A.; Flecknell, P.A. Anaesthesia and post-operative analgesia following experimental surgery in laboratory rodents: Are we making progress? Altern. Lab. Anim. 2005, 33, 119–127. [Google Scholar] [CrossRef]
- Lamont, L.A.; Tranquilli, W.J.; Grimm, K.A. Physiology of pain. Vet. Clin. N. Am. Small Anim. Pract. 2000, 30, 703–728. [Google Scholar] [CrossRef] [PubMed]
- Sebel, P.S.; Lowdon, J.D. Propofol: A new intravenous anesthetic. Anesthesiology 1989, 71, 260–277. [Google Scholar] [CrossRef] [PubMed]
- Franks, N.P.; Lieb, W.R. Molecular and cellular mechanisms of general anaesthesia. Nature 1994, 367, 607–614. [Google Scholar] [CrossRef]
- Krasowski, M.D.; Koltchine, V.V.; Rick, C.E.; Ye, Q.; Finn, S.E.; Harrison, N.L. Propofol and other intravenous anesthetics have sites of action on the gamma-aminobutyric acid type A receptor distinct from that for isoflurane. Mol. Pharmacol. 1998, 53, 530–538. [Google Scholar] [CrossRef]
- Patel, J.; Chowdhury, E.A.; Noorani, B.; Bickel, U.; Huang, J. Isoflurane increases cell membrane fluidity significantly at clinical concentrations. Biochim. Biophys. Acta Biomembr. 2020, 1862, 183140. [Google Scholar] [CrossRef]
- Noorani, B.; Chowdhury, E.A.; Alqahtani, F.; Ahn, Y.; Nozohouri, E.; Zoubi, S.; Patel, D.; Wood, L.; Huang, J.; Siddique, M.B.; et al. Effects of Volatile Anesthetics versus Ketamine on Blood-Brain Barrier Permeability via Lipid-Mediated Alterations of Endothelial Cell Membranes. J. Pharmacol. Exp. Ther. 2023, 385, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Nozohouri, E.; Ahn, Y.; Zoubi, S.; Patel, D.; Archile, S.R.; Akter, K.A.; Siddique, M.B.; Huang, J.; Abbruscato, T.J.; Bickel, U. The Acute Impact of Propofol on Blood-Brain Barrier Integrity in Mice. Pharm. Res. 2024, 41, 1599–1611. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.M.; Neese, O.R.; Bieber, D.D.; Lewis, K.A.; Ahmadi, L.M.; Parsons, D.W.; Canfield, S.G. The Effects of Propofol on a Human in vitro Blood-Brain Barrier Model. Front. Cell Neurosci. 2022, 16, 835649. [Google Scholar] [CrossRef]
- Vanousova, K.; Beranova, J.; Fiser, R.; Jemiola-Rzeminska, M.; Matyska Liskova, P.; Cybulski, L.; Strzalka, K.; Konopasek, I. Membrane fluidization by alcohols inhibits DesK-DesR signalling in Bacillus subtilis. Biochim. Biophys. Acta Biomembr. 2018, 1860, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Feigenson, G.W.; Buboltz, J.T. Ternary phase diagram of dipalmitoyl-PC/dilauroyl-PC/cholesterol: Nanoscopic domain formation driven by cholesterol. Biophys. J. 2001, 80, 2775–2788. [Google Scholar] [CrossRef] [PubMed]
- Konyakhina, T.M.; Feigenson, G.W. Phase diagram of a polyunsaturated lipid mixture: Brain sphingomyelin/1-stearoyl-2-docosahexaenoyl-sn-glycero-3-phosphocholine/cholesterol. Biochim. Biophys. Acta 2016, 1858, 153–161. [Google Scholar] [CrossRef]
- Nelson, S.C.; Neeley, S.K.; Melonakos, E.D.; Bell, J.D.; Busath, D.D. Fluorescence anisotropy of diphenylhexatriene and its cationic Trimethylamino derivative in liquid dipalmitoylphosphatidylcholine liposomes: Opposing responses to isoflurane. BMC Biophys. 2012, 5, 5. [Google Scholar] [CrossRef]
- Kalb, E.; Paltauf, F.; Hermetter, A. Fluorescence lifetime distributions of diphenylhexatriene-labeled phosphatidylcholine as a tool for the study of phospholipid-cholesterol interactions. Biophys. J. 1989, 56, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Barrow, D.A.; Lentz, B.R. Membrane structural domains. Resolution limits using diphenylhexatriene fluorescence decay. Biophys. J. 1985, 48, 221–234. [Google Scholar] [CrossRef]
- Somerharju, P. Pyrene-labeled lipids as tools in membrane biophysics and cell biology. Chem. Phys. Lipids 2002, 116, 57–74. [Google Scholar] [CrossRef]
- Mazoit, J.X.; Samii, K. Binding of propofol to blood components: Implications for pharmacokinetics and for pharmacodynamics. Br. J. Clin. Pharmacol. 1999, 47, 35–42. [Google Scholar] [CrossRef]
- Servin, F.; Desmonts, J.M.; Haberer, J.P.; Cockshott, I.D.; Plummer, G.F.; Farinotti, R. Pharmacokinetics and protein binding of propofol in patients with cirrhosis. Anesthesiology 1988, 69, 887–891. [Google Scholar] [CrossRef]
- Shityakov, S.; Fischer, A.; Su, K.P.; Hussein, A.A.; Dandekar, T.; Broscheit, J. Novel Approach for Characterizing Propofol Binding Affinities to Serum Albumins from Different Species. ACS Omega 2020, 5, 25543–25551. [Google Scholar] [CrossRef] [PubMed]
- Shafer, A.; Doze, V.A.; Shafer, S.L.; White, P.F. Pharmacokinetics and pharmacodynamics of propofol infusions during general anesthesia. Anesthesiology 1988, 69, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Engdahl, O.; Abrahams, M.; Bjornsson, A.; Vegfors, M.; Norlander, B.; Ahlner, J.; Eintrei, C. Cerebrospinal fluid concentrations of propofol during anaesthesia in humans. Br. J. Anaesth. 1998, 81, 957–959. [Google Scholar] [CrossRef]
- Davies, M.; Thuynsma, R.P.; Dunn, S.M. Effects of propofol and pentobarbital on ligand binding to GABAA receptors suggest a similar mechanism of action. Can. J. Physiol. Pharmacol. 1998, 76, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Fukami, S.; Uchida, I.; Takenoshita, M.; Mashimo, T.; Yoshiya, I. The effects of a point mutation of the beta2 subunit of GABA(A) receptor on direct and modulatory actions of general anesthetics. Eur. J. Pharmacol. 1999, 368, 269–276. [Google Scholar] [CrossRef]
- Inoue, Y.; Shibuya, I.; Kabashima, N.; Noguchi, J.; Harayama, N.; Ueta, Y.; Sata, T.; Shigematsu, A.; Yamashita, H. The mechanism of inhibitory actions of propofol on rat supraoptic neurons. Anesthesiology 1999, 91, 167–178. [Google Scholar] [CrossRef]
- Altmayer, P.; Buch, U.; Buch, H.P. Propofol binding to human blood proteins. Arzneimittelforschung 1995, 45, 1053–1056. [Google Scholar]
- Riu, P.L.; Riu, G.; Testa, C.; Mulas, M.; Caria, M.A.; Mameli, S.; Mameli, O. Disposition of propofol between red blood cells, plasma, brain and cerebrospinal fluid in rabbits. Eur. J. Anaesthesiol. 2000, 17, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Li, S.; Xue, H.; Sun, L.; Kim, D.H.; Liu, Y. Effects of Propofol Treatment in Neural Progenitors Derived from Human-Induced Pluripotent Stem Cells. Neural. Plast. 2017, 2017, 9182748. [Google Scholar] [CrossRef] [PubMed]
- Sall, J.W.; Stratmann, G.; Leong, J.; Woodward, E.; Bickler, P.E. Propofol at clinically relevant concentrations increases neuronal differentiation but is not toxic to hippocampal neural precursor cells in vitro. Anesthesiology 2012, 117, 1080–1090. [Google Scholar] [CrossRef]
- Svennerholm, L.; Bostrom, K.; Jungbjer, B.; Olsson, L. Membrane lipids of adult human brain: Lipid composition of frontal and temporal lobe in subjects of age 20 to 100 years. J. Neurochem. 1994, 63, 1802–1811. [Google Scholar] [CrossRef]
- Veilleux-Lemieux, D.; Castel, A.; Carrier, D.; Beaudry, F.; Vachon, P. Pharmacokinetics of ketamine and xylazine in young and old Sprague-Dawley rats. J. Am. Assoc. Lab. Anim. Sci. 2013, 52, 567–570. [Google Scholar] [PubMed]
- Mazzanti, L.; Pastuszko, A.; Lenaz, G. Effects of ketamine anesthesia on rat-brain membranes: Fluidity changes and kinetics of acetylcholinesterase. Biochim. Biophys. Acta 1986, 861, 105–110. [Google Scholar] [CrossRef]
- Jerabek, H.; Pabst, G.; Rappolt, M.; Stockner, T. Membrane-mediated effect on ion channels induced by the anesthetic drug ketamine. J. Am. Chem. Soc. 2010, 132, 7990–7997. [Google Scholar] [CrossRef] [PubMed]
- Kingsley, P.B.; Feigenson, G.W. The synthesis of a perdeuterated phospholipid: 1,2-dimyristoyl-sn-glycero-3-phosphocholine-d72. Chem. Phys. Lipids 1979, 24, 135–147. [Google Scholar] [CrossRef]
- Tewes, B.J.; Galla, H.J. Lipid polarity in brain capillary endothelial cells. Endothelium 2001, 8, 207–220. [Google Scholar] [CrossRef] [PubMed]
- Buboltz, J.T. A more efficient device for preparing model-membrane liposomes by the rapid solvent exchange method. Rev. Sci. Instrum. 2009, 80, 124301. [Google Scholar] [CrossRef]
- Mukherjee, S.; Xu, W.; Hsu, F.F.; Patel, J.; Huang, J.; Zhang, K. Sterol methyltransferase is required for optimal mitochondrial function and virulence in Leishmania major. Mol. Microbiol. 2019, 111, 65–81. [Google Scholar] [CrossRef]
- Ahn, Y.; Patil, C.D.; Nozohouri, E.; Zoubi, S.; Patel, D.; Bickel, U. Higher Brain Uptake of Gentamicin and Ceftazidime under Isoflurane Anesthesia Compared to Ketamine/Xylazine. Pharmaceutics 2024, 16, 135. [Google Scholar] [CrossRef]



| Membranes | Drug Concentrations | Before Adding Drug | Averages Between 8 and 15 min After Adding Anesthetic | Percentage Change | |
|---|---|---|---|---|---|
| DPPC | Sevoflurane | 0.25 mM * | 0.665 ± 0.004 | 0.710 ± 0.007 | 6.77% |
| 0.50 mM * | 0.664 ± 0.028 | 0.744 ± 0.022 | 12.05% | ||
| 1.0 mM | 0.659 ± 0.030 | 0.820 ± 0.042 | 24.43% | ||
| 2.0 mM | 0.642 ± 0.001 | 1.073 ± 0.029 | 67.13% | ||
| Isoflurane | 1 mM * | 0.636 ± 0.009 | 0.736 ± 0.036 | 15.72% | |
| 5 mM | 0.643 ± 0.004 | 1.394 ± 0.049 | 116.8% | ||
| Propofol | 1 µM * | 0.662 ± 0.003 | 0.681 ± 0.008 | 2.87% | |
| 5 µM * | 0.669 ± 0.004 | 0.711 ± 0.006 | 6.28% | ||
| 10 µM * | 0.639 ± 0.017 | 0.742 ± 0.004 | 16.12% | ||
| 30 µM | 0.656 ± 0.015 | 0.917 ± 0.014 | 39.79% | ||
| 100 µM | 0.643 ± 0.027 | 1.646 ± 0.090 | 155.99% | ||
| 200 µM | 0.647 ± 0.018 | 2.184 ± 0.023 | 237.56% | ||
| Ketamine/ xylazine | 42 µM * | No change | |||
| 210 µM | 0.646 ± 0.007 | 0.658 ± 0.002 | 1.86% | ||
| BSM/DOPC/Chol | Sevoflurane | 0.25 mM * | 0.770 ± 0.014 | 0.811 ± 0.008 | 5.32% |
| 0.50 mM * | 0.771 ± 0.024 | 0.835 ± 0.027 | 8.30% | ||
| 1.0 mM | 0.794 ± 0.009 | 0.877 ± 0.009 | 10.45% | ||
| 2.0 mM | 0.789 ± 0.016 | 0.960 ± 0.024 | 21.67% | ||
| Isoflurane | 1 mM * | 0.763 ± 0.040 | 0.839 ± 0.033 | 9.96% | |
| 5 mM | 0.793 ± 0.029 | 1.155 ± 0.034 | 45.65% | ||
| Propofol | 1 µM * | 0.728 ± 0.011 | 0.796 ± 0.011 | 9.34% | |
| 5 µM * | 0.780 ± 0.012 | 0.810 ± 0.007 | 3.85% | ||
| 10 µM * | 0.780 ± 0.008 | 0.851 ± 0.013 | 9.10% | ||
| 30 µM | 0.767 ± 0.033 | 0.944 ± 0.018 | 23.08% | ||
| 100 µM | 0.773 ± 0.004 | 1.235 ± 0.013 | 59.77% | ||
| 200 µM | 0.779 ± 0.007 | 1.499 ± 0.042 | 92.43% | ||
| Ketamine/ xylazine | 42 µM * | No change | |||
| 210 µM | 0.773 ± 0.305 | 0.809 ± 0.036 | 4.66% | ||
| POPC/Chol | Sevoflurane | 0.25 mM * | 1.596 ± 0.016 | 1.651 ± 0.017 | 3.45% |
| 0.50 mM * | 1.588 ± 0.008 | 1.686 ± 0.007 | 6.17% | ||
| 1.0 mM | 1.586 ± 0.014 | 1.765 ± 0.008 | 11.29% | ||
| 2.0 mM | 1.601 ± 0.011 | 1.939 ± 0.034 | 21.11% | ||
| Isoflurane | 1 mM * | 1.569 ± 0.010 | 1.704 ± 0.009 | 8.60% | |
| 5 mM | 1.555 ± 0.019 | 2.139 ± 0.056 | 37.56% | ||
| Propofol | 1 µM * | 1.596 ± 0.003 | 1.623 ± 0.004 | 1.69% | |
| 5 µM * | 1.576 ± 0.004 | 1.609 ± 0.007 | 2.09% | ||
| 10 µM * | 1.550 ± 0.007 | 1.615 ± 0.013 | 4.19% | ||
| 30 µM | 1.580 ± 0.005 | 1.763 ± 0.019 | 11.58% | ||
| 100 µM | 1.563 ± 0.023 | 1.995 ± 0.032 | 27.64% | ||
| 200 µM | 1.554 ± 0.010 | 2.128 ± 0.044 | 36.94% | ||
| Ketamine/ xylazine | 42 µM * | No change | |||
| 210 µM | 1.562 ± 0.008 | 1.573 ± 0.002 | 0.70% | ||
| 5-Lipids | Sevoflurane | 0.25 mM * | 1.741 ± 0.012 | 1.787 ± 0.009 | 2.64% |
| 0.50 mM * | 1.746 ± 0.022 | 1.818 ± 0.024 | 4.12% | ||
| 1.0 mM | 1.713 ± 0.012 | 1.844 ± 0.013 | 7.65% | ||
| 2.0 mM | 1.727 ± 0.006 | 2.037 ± 0.023 | 17.95% | ||
| Isoflurane | 1 mM * | 1.666 ± 0.053 | 1.795 ± 0.049 | 7.74% | |
| 5 mM | 1.690 ± 0.010 | 2.232 ± 0.018 | 32.07% | ||
| Propofol | 1 µM * | 1.708 ± 0.017 | 1.728 ± 0.009 | 1.17% | |
| 5 µM * | 1.708 ± 0.003 | 1.734 ± 0.005 | 1.52% | ||
| 10 µM * | 1.668 ± 0.012 | 1.743 ± 0.012 | 4.49% | ||
| 30 µM | 1.674 ± 0.013 | 1.859 ± 0.030 | 11.05% | ||
| 100 µM | 1.689 ± 0.018 | 2.147 ± 0.018 | 27.12% | ||
| 200 µM | 1.717 ± 0.021 | 2.372 ± 0.021 | 38.15% | ||
| Ketamine/ xylazine | 42 µM * | No change | |||
| 210 µM | 1.709 ± 0.0113 | 1.725 ± 0.003 | 0.94% | ||
| Membranes | Drug Concentrations | Before Adding Anesthetic | Averages Between 8 to 15 min After Adding Anesthetic | Percentage Change | |
|---|---|---|---|---|---|
| DPPC | Sevoflurane | 0.25 mM * | 0.3109 ± 0.0004 | 0.3091 ± 0.0002 | −0.58% |
| 0.50 mM * | 0.3084 ± 0.0010 | 0.3052 ± 0.0012 | −1.04% | ||
| 1.0 mM | 0.3081 ± 0.0009 | 0.3017 ± 0.0019 | −2.08% | ||
| 2.0 mM | 0.3085 ± 0.0005 | 0.2948 ± 0.0005 | −4.44% | ||
| Isoflurane | 1 mM * | 0.3044 ± 0.0013 | 0.2985 ± 0.0027 | −1.94% | |
| 5 mM | 0.3062 ± 0.0020 | 0.2746 ± 0.0034 | −10.32% | ||
| Propofol | 1 µM * | No change | |||
| 5 µM * | 0.3077 ± 0.0006 | 0.3052 ± 0.0008 | −0.81% | ||
| 10 µM * | 0.3072 ± 0.0018 | 0.3034 ± 0.0029 | −1.24% | ||
| 30 µM | 0.3072 ± 0.0021 | 0.2940 ± 0.0034 | −4.30% | ||
| 100 µM | 0.3056 ± 0.0001 | 0.2858 ± 0.0014 | −6.48% | ||
| 200 µM | 0.3096 ± 0.0012 | 0.2325 ± 0.0030 | −24.90% | ||
| Ketamine/ xylazine | 42 µM * | 0.3052 ± 0.0029 | 0.3030 ± 0.0028 | −0.72% | |
| 210 µM | 0.3077 ± 0.0003 | 0.3046 ± 0.0018 | −1.01% | ||
| BSM/DOPC/Chol | Sevoflurane | 0.25 mM * | 0.2251 ± 0.0017 | 0.2238 ± 0.0020 | −0.58% |
| 0.50 mM * | 0.2227 ± 0.0012 | 0.2202 ± 0.0016 | −1.12% | ||
| 1.0 mM | 0.2252 ± 0.0017 | 0.2191 ± 0.0005 | −2.71% | ||
| 2.0 mM | 0.2274 ± 0.0014 | 0.2144 ± 0.0009 | −5.72% | ||
| Isoflurane | 1 mM * | 0.2245 ± 0.0003 | 0.2218 ± 0.0005 | −1.20% | |
| 5 mM | 0.2270 ± 0.0005 | 0.2162 ± 0.0006 | −4.76% | ||
| Propofol | 1 µM *–10 µM * | No change | |||
| 30 µM | 0.2251 ± 0.0009 | 0.2228 ± 0.0007 | −1.02% | ||
| 100 µM | 0.2240 ± 0.0006 | 0.2193 ± 0.0003 | −2.10% | ||
| 200 µM | 0.2279 ± 0.0025 | 0.2200 ± 0.0024 | −3.47% | ||
| Ketamine/ xylazine | 42 µM * | No change | |||
| 210 µM | 0.2273 ± 0.0011 | 0.2251 ± 0.0017 | −0.97% | ||
| POPC/Chol | Sevoflurane | 0.25 mM * | 0.1787 ± 0.0002 | 0.1770 ± 0.0005 | −0.95% |
| 0.50 mM * | 0.1793 ± 0.0002 | 0.1768 ± 0.0004 | −1.39% | ||
| 1.0 mM | 0.1785 ± 0.0003 | 0.1747 ± 0.0002 | −2.13% | ||
| 2.0 mM | 0.1797 ± 0.0002 | 0.1718 ± 0.0005 | −4.40% | ||
| Isoflurane | 1 mM * | 0.1773 ± 0.0006 | 0.1761 ± 0.0006 | −0.68% | |
| 5 mM | 0.1766 ± 0.0001 | 0.1702 ± 0.0005 | −3.62% | ||
| Propofol | 1 µM *–200 µM | No change | |||
| Ketamine/ xylazine | 42 µM * | 0.1770 ± 0.0007 | 0.1769 ± 0.0008 | −0.06% | |
| 210 µM | 0.1761 ± 0.0018 | 0.1754 ± 0.0019 | −0.39% | ||
| 5-Lipids | Sevoflurane | 0.25 mM * | 0.1746 ± 0.0002 | 0.1735 ± 0.0006 | −0.63% |
| 0.50 mM * | 0.1750 ± 0.0009 | 0.1731 ± 0.0003 | −1.08% | ||
| 1.0 mM | 0.1744 ± 0.0005 | 0.1709 ± 0.0007 | −2.01% | ||
| 2.0 mM | 0.1760 ± 0.0006 | 0.1687 ± 0.0003 | −4.15% | ||
| Isoflurane | 1 mM * | 0.1749 ± 0.0008 | 0.1732 ± 0.0002 | −0.97% | |
| 5 mM | 0.1748 ± 0.0008 | 0.1677 ± 0.0010 | −4.06% | ||
| Propofol | 1 µM *–30 µM | No change | |||
| 100 µM | 0.1757 ± 0.0010 | 0.1743 ± 0.0010 | −0.80% | ||
| 200 µM | 0.1757 ± 0.0006 | 0.1730 ± 0.0008 | −1.54% | ||
| Ketamine/ xylazine | 42 µM * | No change | |||
| 210 µM | 0.1750 ± 0.0004 | 0.1744 ± 0.0004 | −0.34% | ||
| Drug Concentration | Before Adding Anesthetic | After Adding Anesthetic | Percentage Change |
|---|---|---|---|
| 1 mM Isoflurane * | 0.285177 ± 0.0011 | 0.2778 ± 0.0024 | −2.59% |
| 5 mM Isoflurane | 0.285858 ± 0.0040 | 0.2746 ± 0.0052 | −3.92% |
| 0.25 mM Sevoflurane * | 0.295056 ± 0.0029 | 0.2890 ± 0.0032 | −2.03% |
| 0.5 mM Sevoflurane * | 0.287785 ± 0.0040 | 0.2798 ± 0.0035 | −2.78% |
| 1.0 mM Sevoflurane | 0.292957 ± 0.0034 | 0.2845 ± 0.0036 | −2.90% |
| 2.0 mM Sevoflurane | 0.284942 ± 0.0083 | 0.2743 ± 0.0090 | −3.72% |
| 174 mM Ethanol | 0.302055 ± 0.0130 | 0.2981 ± 0.0124 | −1.29% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siddique, M.B.; Nozohouri, E.; Ahn, Y.; Zoubi, S.; Bickel, U.; Huang, J. A Comparative Study of Common Anesthetics Propofol, Sevoflurane, Isoflurane and Ketamine on Lipid Membrane Fluidity. Int. J. Mol. Sci. 2025, 26, 1337. https://doi.org/10.3390/ijms26031337
Siddique MB, Nozohouri E, Ahn Y, Zoubi S, Bickel U, Huang J. A Comparative Study of Common Anesthetics Propofol, Sevoflurane, Isoflurane and Ketamine on Lipid Membrane Fluidity. International Journal of Molecular Sciences. 2025; 26(3):1337. https://doi.org/10.3390/ijms26031337
Chicago/Turabian StyleSiddique, Muhammad Bilal, Ehsan Nozohouri, Yeseul Ahn, Sumaih Zoubi, Ulrich Bickel, and Juyang Huang. 2025. "A Comparative Study of Common Anesthetics Propofol, Sevoflurane, Isoflurane and Ketamine on Lipid Membrane Fluidity" International Journal of Molecular Sciences 26, no. 3: 1337. https://doi.org/10.3390/ijms26031337
APA StyleSiddique, M. B., Nozohouri, E., Ahn, Y., Zoubi, S., Bickel, U., & Huang, J. (2025). A Comparative Study of Common Anesthetics Propofol, Sevoflurane, Isoflurane and Ketamine on Lipid Membrane Fluidity. International Journal of Molecular Sciences, 26(3), 1337. https://doi.org/10.3390/ijms26031337






