Therapeutic Potential of Latin American Medicinal Plants in Oral Diseases: From Dental Pain to Periodontal Inflammation—A Systematic Review
Abstract
1. Introduction
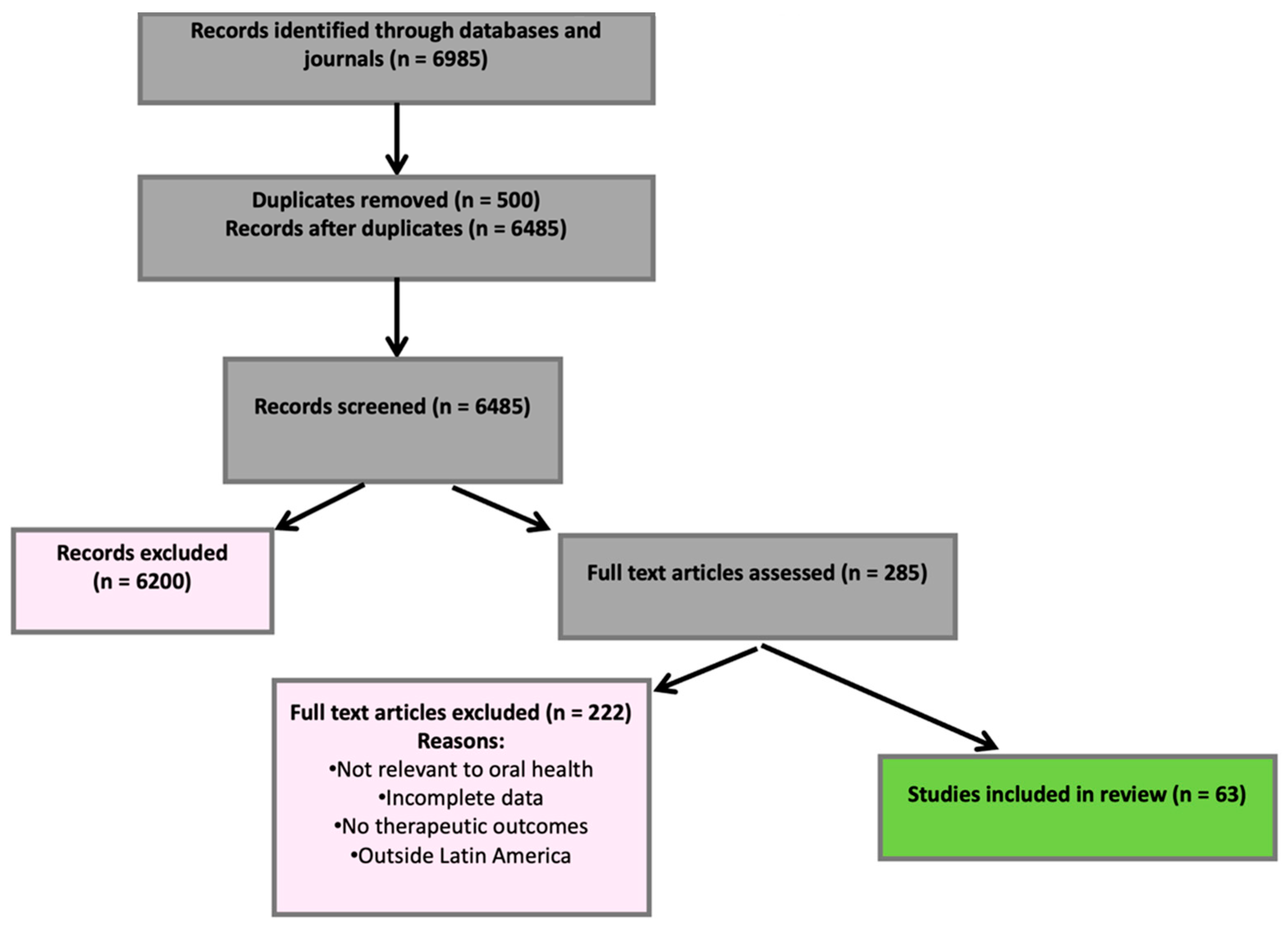
2. Materials and Methods
- Propolis (resinous product of Apis mellifera L., Apidae): Antimicrobial and anti-inflammatory activity, effective against gingivitis and periodontitis.
- Salvia rosmarinus Spenn. (Lamiaceae): Used for pain relief and wound healing in the oral cavity.
- Moringa (Moringa oleifera): Anti-inflammatory effects beneficial to oral tissues.
- Aloe vera (L.) Burm.f. (Asphodelaceae) and Ocimum basilicum L. (Lamiaceae): Known for healing and antibacterial properties relevant to disease prevention and oral care.
3. Pain and Its Relationship with Dentistry
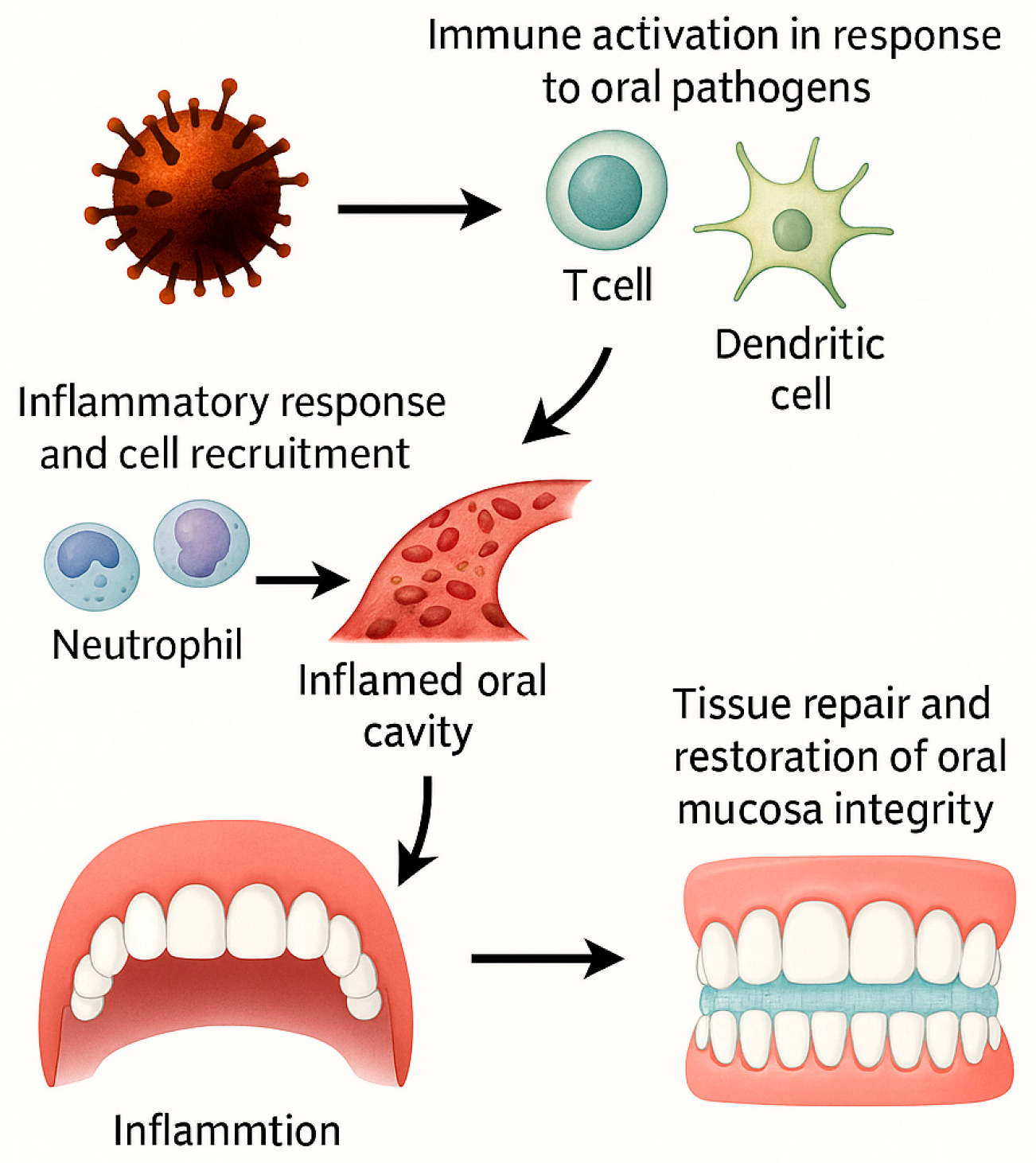
4. Causes of Dental Pain
5. Conventional Pharmacology for Pain Management
6. Use of Medicinal Plants for Reducing Oral Pain
7. Dental Products
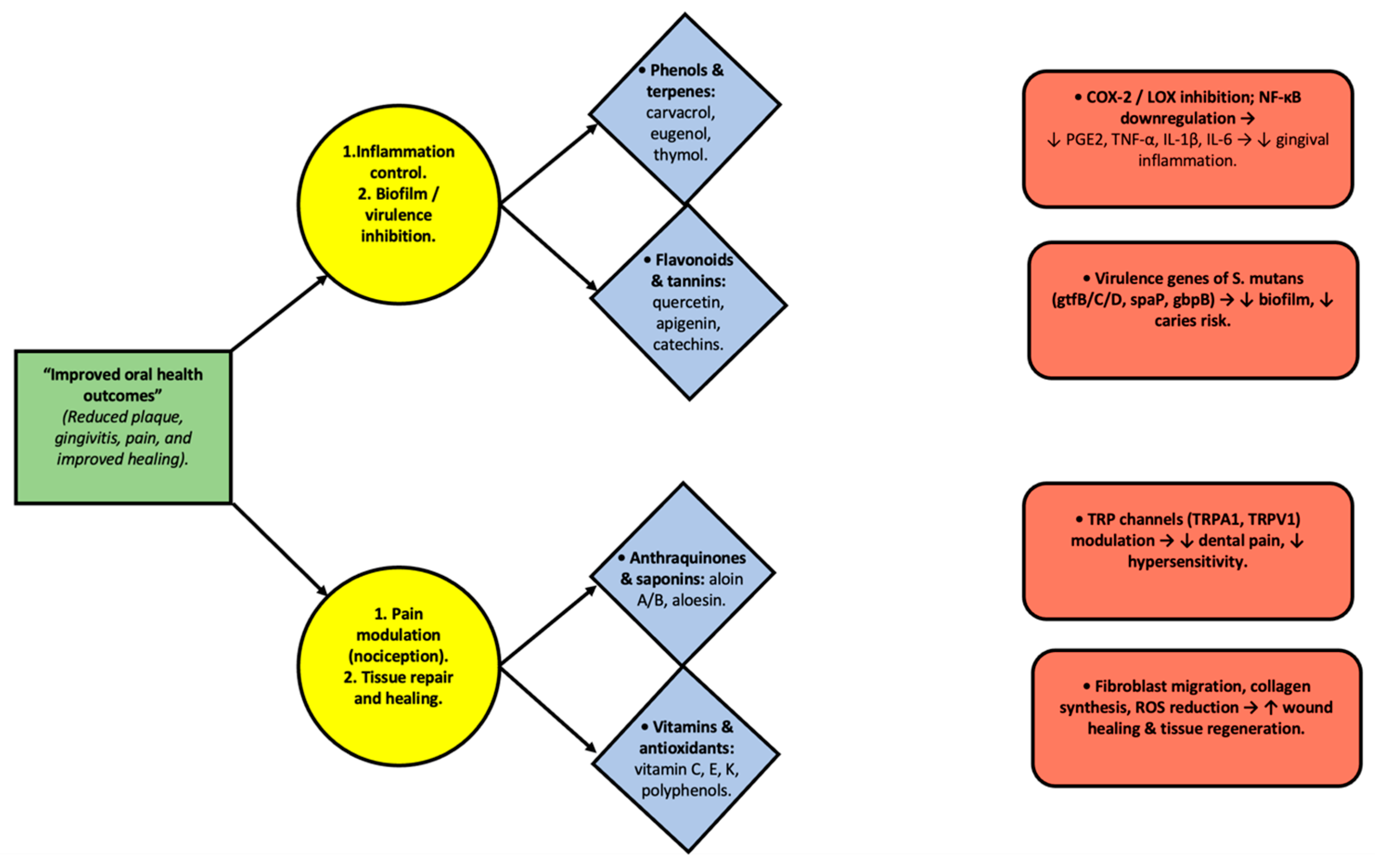
8. Mechanism of Action of Plants in Inflammation
Mechanisms of Action of Selected Plant Metabolites in Oral Inflammation
9. Internal Inflammatory Process
10. Properties of Medicinal Plants
11. Biodiversity of Medicinal Plants in Latin America
12. Regulation of Medicinal Plants in Colombia
13. Medicinal Plants for Inflammation and Gingival Problems
14. Medicinal Plants for Periodontal Problems
15. Results and Discussion
16. Conclusions and Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Oral Health. Available online: https://www.who.int/es/news-room/fact-sheets/detail/oral-health (accessed on 7 September 2025).
- Secretaría de Salud de Medellín. Profundización del Análisis de la Situación S. Medellín 2005–2020; Secretaría de Salud: Medellín, Colombia, 2021; pp. 1–50.
- Valdéz Grefa, L.K.; Palacios Paredes, E.W. Prácticas etnobotánicas odontológicas de la comunidad Kichwa Playas de Oro, parroquia Santa Cecilia, cantón Lago Agrio, provincia de Sucumbíos. Recimundo 2022, 6 (Suppl. S1), 242–252. [Google Scholar] [CrossRef]
- Fuentes, F.; Faúndez, F.; Roa, I. Fitoterapias en lesiones de mucosa oral: Propiedades reparativas y aplicación clínica. Revisión sistemática de la literatura. Int. J. Odontostomatol. 2016, 10, 539–545. [Google Scholar] [CrossRef]
- Vara-Delgado, A.; Sosa-González, R.; Alayón-Recio, C.S.; Ayala-Sotolongo, N.; Moreno-Capote, G.; Alayón-Recio, V.C. Uso de la manzanilla en el tratamiento de las enfermedades periodontales. Rev. Arch. Med. Camagüey 2019, 23, 403–409. [Google Scholar]
- Vicente-Herrero, M.T.; Delgado-Bueno, S.; Bandrés-Moyá, F.; Ramírez-Íñiguez-de-la-Torre, M.V.; Capdevilla-García, L. Valoración del dolor. Revisión comparativa de escalas y cuestionarios. Rev. Soc. Esp. Dolor 2018, 25, 228–236. [Google Scholar] [CrossRef]
- Ministerio de la Protección Social. Vademécum Colombiano de Plantas Medicinales; Ministerio de la Protección Social: Bogotá, Colombia, 2008.
- Miguélez-Medrán, B.C.; Goicoechea García, C.; López Sánchez, A.; Martínez García, M.A. Dolor orofacial en la clínica odontológica. Rev. Soc. Esp. Dolor 2019, 26, 233–242. [Google Scholar] [CrossRef]
- Rodríguez Reyes, O.; García Cabrera, L.; Bosch Núñez, A.I.; Inclán Acosta, A. Fisiopatología del dolor bucodental: Una visión actualizada del tema. Medisan 2013, 17, 5080–5090. [Google Scholar]
- Latorre, G.; González-García, N.; García-Ull, J.; González-Oria, C.; Porta-Etessam, J.; Molina, F.J.; Guerrero-Peral, A.L.; Belvís, R.; Rodríguez, R.; Bescós, A.; et al. Diagnóstico y tratamiento de la neuralgia del trigémino: Documento de consenso del Grupo de Estudio de Cefaleas de la Sociedad Española de Neurología. Neurología 2023, 38 (Suppl. S1), S37–S52. [Google Scholar] [CrossRef] [PubMed]
- Ríos Erazo, M.; Herrera Ronda, A.; Rojas Alcayaga, S. Ansiedad dental: Evaluación y tratamiento. Av. Odontoestomatol. 2014, 30, 39–46. [Google Scholar] [CrossRef]
- López Sánchez, A.F.; González Romero, E.A. Dolor dental. Med. Integr. 2001, 37, 242–249. [Google Scholar]
- Servicio Canario de la Salud. Dirección General de Salud Pública. ¿Qué es el Dolor Dental? Programa de Salud Oral. Servicio de Promoción de la Salud, Gobierno de Canarias; 2025. Available online: https://www3.gobiernodecanarias.org/sanidad/scs/content/4b1164e9-e63b-11e0-bf4e-bd28dc0dbd05/que_es_el_dolor_dental.pdf (accessed on 19 May 2025).
- Mata Sánchez, N.; Jiménez Méndez, C.; Sánchez Mendieta, K.P. Recesión gingival y su efecto en la hipersensibilidad dentinaria. Rev. ADM 2018, 75, 326–333. [Google Scholar]
- Jwa, S.K. Eficacia de los extractos de hoja de Moringa oleifera contra la biopelícula cariogénica. Prev. Nutr. Food Sci. 2019, 24, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Canakci, C.F.; Canakci, V. Dental pain experienced by patients undergoing different periodontal therapies. J. Am. Dent. Assoc. 2007, 138, 1563–1573. [Google Scholar] [CrossRef]
- Catalá Pizarro, M.; Cortés Lillo, O. La caries dental: Una enfermedad que se puede prevenir. An. Pediatría Contin. 2014, 12, 147–151. [Google Scholar] [CrossRef]
- González-Gallego, J.; Sánchez-Campos, S.; Tuñón, M.J. Anti-inflammatory properties of dietary flavonoids. Nutr. Hosp. 2007, 22, 287–293. [Google Scholar]
- López Silva, M.C.; Diz-Iglesias, P.; Seoane-Romero, J.M.; Quintas, V.; Méndez-Brea, F.; Varela-Centelles, P. Actualización en medicina de familia: Patología periodontal. Med. Fam. (Semer.) 2017, 43, 141–148. [Google Scholar] [CrossRef]
- Ziegler, A. Los analgésicos en odontología. Quintessence 2012, 25, 8–18. [Google Scholar]
- Casariego, Z.J. Mecanismo de acción de plantas medicinales aplicadas en lesiones estomatológicas: Revisión. Av. Odontoestomatol. 2016, 32, 35–44. [Google Scholar] [CrossRef]
- Perazzo, F.; Souza, R.; Carvalho, J.C.; Groppo, F. Utilización de sustancias naturales en odontología. J. Bras. Fitomed. 2004, 2, 9–16. [Google Scholar]
- Lameda Albornoz, M.A.; Paredes Rivas, M.F.; Sánchez Díaz, J.T.; Sayago Lameda, M.J.; Yáñez Guerrero, P.A. Uso de las plantas medicinales para el tratamiento de la enfermedad periodontal: Una revisión sistemática. Rev. Venez. Investig. Odontol. 2019, 7, 85–96. [Google Scholar]
- Lopes-Martins, R.A.; Pegoraro, D.H.; Woisky, R.; Penna, S.C.; Sertié, J.A. The anti-inflammatory and analgesic effects of a crude extract of Petiveria alliacea L. (Phytolaccaceae). Phytomedicine 2002, 9, 245–248. [Google Scholar] [CrossRef]
- Santos Filho, E.X.D.; Arantes, D.A.C.; Oton Leite, A.F.; Batista, A.C.; Mendonça, E.F.; Marreto, R.N.; Naves, L.N.; Lima, E.M.; Valadares, M.C. Randomized clinical trial of a muco-adhesive formulation containing curcuminoids (Zingiberaceae) and Bidens pilosa Linn (Asteraceae) extract (FITOPROT) for the prevention and treatment of oral mucositis–phase I study. Chem. Biol. Interact. 2018, 291, 228–236. [Google Scholar] [CrossRef]
- Criollo Jiménez, M.E. Efecto Antiinflamatorio de Zingiber officinale Roscoe (Jengibre) Sobre los Tejidos Blandos en Estudiantes de Octavo, Noveno y Décimo Año de Educación Básica del Colegio Fis-Comisional “La Dolorosa” que Presentan Gingivitis, en el Período Junio–Diciembre 2011. Bachelor’s Thesis, Universidad Nacional de Loja, Loja, Ecuador, 2012. Available online: https://dspace.unl.edu.ec/server/api/core/bitstreams/aedc9d50-b461-43a1-9cc5-517489c753e1/content (accessed on 7 September 2025).
- Rodríguez, M.; Aguilar, D.; León, J. Actividad antiinflamatoria de plantas medicinales: Anti-inflammatory activity of medicinal plants (Review). Rev. Colomb. Cienc. Hortic. 2020, 14, e11847. [Google Scholar] [CrossRef]
- Barraza, M.A.; Calabró, L.R.; Delgado, E.M.; Peñaloza Azcurra, L.; Suárez Medina, A.L. Usos y Conocimientos de Plantas Medicinales. Bachelor’s Thesis, Universidad Nacional de San Martín, Buenos Aires, Argentina, 2020. Available online: https://ri.unsam.edu.ar/handle/123456789/1316 (accessed on 7 September 2025).
- Zdarilová, A.; Svobodová, A.; Šimánek, V.; Ulrichová, J. Extract of Prunella vulgaris and rosmarinic acid suppresses lipopolysaccharide-induced alteration in human gingival fibroblasts. Toxicol. In Vitro 2009, 23, 386–392. [Google Scholar] [CrossRef]
- Chen, C.-P.; Lin, Y.-C.; Peng, Y.-H.; Chen, H.-M.; Lin, J.-T.; Kao, S.-H. Rosmarinic acid attenuates lipopolysaccharide-induced inflammatory response in vascular smooth muscle cells by inhibiting MAPK/NF-κB pathway. Pharmaceuticals 2022, 15, 437. [Google Scholar] [CrossRef]
- Sugiharto, S.; Ramadany, S.; Handayani, H.; Achmad, H.; Gani, A.; Tanumihardja, M.; Sesiorina, A.; Harmawaty. Ethanolic extract of Moringa oleifera leaves influences NF-κB signaling pathway for periodontal tissue regeneration in rats. J. Popul. Ther. Clin. Pharmacol. 2023, 30, e324–e332. [Google Scholar] [CrossRef]
- Kandikur, S.; Guttiganur, N.; Aspalli, S.; Bhavana. Comparing the anti-plaque and anti-gingivitis efficacy of Moringa oleifera mouthwash to chlorhexidine and saltwater concentration in treating gingivitis: A randomized controlled clinical trial. IOSR J. Dent. Med. Sci. 2025, 24, 49–57. [Google Scholar]
- Thuwajit, P.; Ruangpornvisuti, V.; Kengkwasing, P.; Chokboribal, J.; Sangvanich, P. Acemannan increases NF-κB/DNA binding and IL-6/-8 expression by selectively binding Toll-like receptor-5 in human gingival fibroblasts. Carbohydr. Polym. 2017, 161, 149–157. [Google Scholar] [CrossRef]
- Sánchez, M.; González-Burgos, E.; Iglesias, I.; Gómez-Serranillos, M.P. Pharmacological update properties of Aloe vera and its major active constituents. Molecules 2020, 25, 1324. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.P.; Carvalho-Filho, P.C.; Sampaio, G.P.; Silva, R.R.; Falcão, M.M.; Pimentel, A.C.M.; Oliveira, Y.A.; Miranda, P.M.; Santos, E.K.N.; Meyer, R.; et al. In vitro immunomodulatory effect of linalool on P. gingivalis infection. Glob. J. Med. Res. F Dis. 2019, 20, 7–16. [Google Scholar] [CrossRef]
- Lozoya Legorreta, X. ¿Una Nueva Farmacéutica Para el Siglo XXI? La Aportación de América Latina al Estudio de las Plantas Medicinales; Editorial CENIC: La Habana, Cuba, 2022. [Google Scholar]
- Soria, N. Medicinal plants and their application in public health. Rev. Salud Pública Parag. 2018, 8, 7–8. [Google Scholar] [CrossRef]
- Congreso de Colombia. Ley 1164 de 2007, por la Cual se Dictan Disposiciones en Materia del Talento Humano en Salud; Diario Oficial No. 46.786, Bogotá, Colombia. 2007. Available online: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=27528 (accessed on 7 September 2025).
- Ministerio de Salud y Protección Social. Lineamientos Técnicos para la Articulación de las Medicinas y las Terapias Alternativas y Complementarias, en el Marco del Sistema General de Seguridad Social en Salud; Ministerio de Salud: Bogotá, Colombia, 2018.
- Cervantes Pérez, A. Medicina Alternativa: Fitoterapia Como Coadyuvante en el Tratamiento de la Enfermedad Periodontal 2016. Bachelor’s Thesis, Universidad Nacional Autónoma de México, Mexico City, Mexico, 2017. Available online: https://repositorio.unam.mx/contenidos/393452 (accessed on 7 September 2025).
- Menon, P.; Pevali, J.; Fenol, A.; Peter, M.R.; Lakshmi, P.; Suresh, R. Effectiveness of ginger on pain following periodontal surgery: A randomized crossover clinical trial. J. Ayurveda Integr. Med. 2020, 12, 65–69. [Google Scholar] [CrossRef]
- Maragliano, P.; Viola, T. How Ginger Supplements Can Affect Dental Care. DentistryIQ. 8 May 2024. Available online: https://www.dentistryiq.com/dentistry/pharmacology/video/55038367/how-ginger-supplements-can-affect-dental-care (accessed on 7 September 2025).
- Gutiérrez, R.; Albarrán, R. Uso de plantas medicinales como terapia coadyuvante en el tratamiento periodontal: Revisión de la literatura. Rev. Odontol. Los Andes 2020, 15, 45–56. [Google Scholar]
- Mohammed, S.A.; Akram, H.M. Evaluating the efficacy of resveratrol-containing mouthwash as an adjunct treatment for periodontitis: A randomized clinical trial. Eur. J. Dent. 2025, 19, 354–365. [Google Scholar] [CrossRef]
- Ragul, P.; Dhanraj, M.; Jain, A.R. Efficacy of eucalyptus oil over chlorhexidine mouthwash in dental practice. Drug Invent. Today 2018, 10, 638–641. [Google Scholar]
- Waizel-Bucay, J.; Martín Martínez Rico, I. Plantas empleadas en odontalgias I. Rev. ADM 2007, 64, 173–186. [Google Scholar]
- Khairnar, M.S.; Pawar, B.; Marawar, P.P.; Mani, A. Evaluation of Calendula officinalis as an anti-plaque and anti-gingivitis agent. J. Indian Soc. Periodontol. 2013, 17, 741–747. [Google Scholar] [CrossRef]
- Nayak, N.; Varghese, J.; Shetty, S.; Bhat, V.; Durekhar, T.; Lobo, R.; Nayak, U.Y.; Vishwanath, U. Evaluation of a mouthrinse containing guava leaf extract as part of comprehensive oral care regimen: A randomized placebo-controlled clinical trial. BMC Complement. Altern. Med. 2019, 19, 327. [Google Scholar] [CrossRef] [PubMed]
- Moya Jiménez, L.E. Uso de Plantas Medicinales Como Analgésico-Antiinflamatorio en la Parroquia Marcos Espinel del Cantón Santiago de Pillaro. Bachelor’s Thesis, Universidad Técnica de Ambato, Ambato, Ecuador, 2018. Available online: https://repositorio.uta.edu.ec/items/cd0c16b7-350b-4270-aa4b-f4983015952f (accessed on 7 September 2025).
- Ali, M.S.M.; Mohammed, A.N. Efficacy of oregano essential oil mouthwash in reducing oral halitosis: A randomized, double-blind clinical trial. J. Res. Med. Dent. Sci. 2021, 9, 285–290. [Google Scholar]
- National Institute of Diabetes and Digestive and Kidney Diseases. Oregano. In LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]; National Library of Medicine (US): Bethesda, MD, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK591556/ (accessed on 7 September 2025).
- Yuan, Y.; Sun, J.; Song, Y.; Raka, R.N.; Xiang, J.; Wu, H.; Xiao, J.; Jin, J.; Hui, X. Antibacterial activity of oregano essential oils against Streptococcus mutans in vitro and analysis of active components. BMC Complement. Med. Ther. 2023, 23, 61. [Google Scholar] [CrossRef]
- Gupta, R.; Gupta, D.; Bhaskar, D.J.; Yadav, A.; Obaid, K.; Mishra, S. Preliminary antiplague efficacy of Aloe vera mouthwash in a 4-day plaque regrowth model: A randomized control trial. J. Indian Soc. Periodontol. 2014, 24, 139–144. [Google Scholar] [CrossRef]
- El Hajj, M.; Holst, L. Herbal medicine use during pregnancy: A review of the literature with a special focus on Sub-Saharan Africa. Front. Pharmacol. 2020, 11, 866. [Google Scholar] [CrossRef]
- Kamath, D.G.; Nadimpalli, H.; Nayak, S.U.; Rajendran, V.; Natarajan, S. Comparison of anti-plaque and anti-gingivitis effects of Aloe vera mouthwash with chlorhexidine in fixed orthodontic patients: A randomized controlled trial. Int. J. Dent. Hyg. 2023, 21, 211–218. [Google Scholar] [CrossRef]
- Vairabhava, L.O.; Korsuwannawong, S.; Ruangsawasdi, N.; Phruksaniyom, C.; Srichan, R. The efficiency of natural wound healing and bacterial biofilm inhibition of Aloe vera and sodium chloride toothpaste preparation. BMC Complement. Med. Ther. 2022, 22, 66. [Google Scholar] [CrossRef] [PubMed]
- Hosamane, M.; Acharya, A.B.; Vij, C.; Trivedi, D.; Setty, S.B.; Thakur, S.L. Evaluation of holy basil mouthwash as an adjunctive plaque control agent in a four-day plaque regrowth model. J. Clin. Exp. Dent. 2014, 6, e491–e496. [Google Scholar] [CrossRef] [PubMed]
- Masoudi, R.; Aldiab, D.; Hasan, N. Study of the anticoagulant effect of Ocimum basilicum extract. Res. J. Pharm. Technol. 2024, 17, 3339–3345. [Google Scholar] [CrossRef]
- Gupta, D.; Bhaskar, D.J.; Gupta, R.K.; Karim, B.; Jain, A.; Singh, R.; Karim, W. A randomized controlled clinical trial of Ocimum sanctum and chlorhexidine mouthwash on dental plaque and gingival inflammation. J. Ayurveda Integr. Med. 2014, 5, 109–116. [Google Scholar] [CrossRef]
- Maurya, S. Anti-inflammatory activity of phytochemicals from Ocimum sanctum against cyclooxygenase 2 (COX-2): A review. Plant Cell Biotechnol. Mol. Biol. 2021, 22, 82–92. [Google Scholar]
- Sultana, A.; Tasneem, A.; Krishnappa, P.; Shwetha, K.M. Efficacy of Moringa oleifera mouthwash in young adults as an antiplaque agent: An interventional study. J. Indian Assoc. Public Health Dent. 2024, 22, 185–190. [Google Scholar] [CrossRef]
- Ebhohon, E.; Miller, D. Moringa oleifera leaf extract–induced pulmonary embolism: A case report. Int. J. Emerg. Med. 2022, 15, 16. [Google Scholar] [CrossRef]
- Duarte, K.; Thomas, B.; Varma, S.R.; Kamath, V.; Shetty, B.; Kuduruhtullah, S.; Nambiar, M. Antiplaque efficacy of a novel Moringa oleifera dentifrice: A randomized clinical cross-over study. Eur. J. Dent. 2022, 16, 768–774. [Google Scholar] [CrossRef]
- Pita-Labori, L.Y.; Matos-Cantillo, D.M.; Quintero-Lores, C.M.; Castillo-Pérez, Y.; Nicó-Navarro, A.M. Uso de Petiveria alliacea Linn como tratamiento paliativo del dolor pulpar. Rev. Inf. Cient. 2023, 102, 4101. [Google Scholar] [CrossRef]
- Silva, J.J.; Cerdeira, C.; Chavasco, J.; Cintra, A.; Silva, C.; Mendonça, A.; Ishikawa, T.; Boriollo, M.; Chavasco, J. In vitro screening antibacterial activity of Bidens pilosa Linné and Annona crassiflora Mart. against oxacillin-resistant Staphylococcus aureus (ORSA) from the aerial environment at the dental clinic. Rev. Inst. Med. Trop. São Paulo 2014, 56, 333–340. [Google Scholar] [CrossRef]
- Yunes, R.A.; Pedrosa, R.C.; Filho, V.C.; Calixto, J.B. Isolation and identification of active compounds from Drimys winteri barks. J. Ethnopharmacol. 1998, 62, 223–227. [Google Scholar] [CrossRef]
- Lima, L.D.; Reis, A.C.C.; Sousa, J.A.C.; Valente, G.M.; de Mello Silva, B.; Magalhães, C.L.B.; Kohlhoff, M.; Teixeira, L.F.M.; Brandão, G.C. Anti–Zika virus activity and isolation of flavonoids from ethanol extracts of Curatella americana L. leaves. Molecules 2023, 28, 2546. [Google Scholar] [CrossRef] [PubMed]
- Sequeda, L.G. Antimicrobial Activity of Baccharis latifolia (Ruiz & Pavón) Pers. (Asteraceae) on Microorganisms Pathogens and Cariogenics. In Proceedings of the V Congreso Iberoamericano de Productos Naturales, Bogotá, Columbia, 25–29 April 2016. [Google Scholar] [CrossRef]
- Hanashiro, C.T.; Miranda González, A.H. Coriandrum sativum (Coriander) in oral health: Literature review. J. Health Sci. 2021, 23, 195–198. [Google Scholar] [CrossRef]
- Millones-Gómez, P.A.; Maurtua-Torres, D.; Bacilio-Amaranto, R.; Calla-Poma, R.D.; Requena-Mendizabal, M.F.; Valderrama-Negron, A.C.; Calderon-Miranda, M.A.; Calla-Poma, R.A.; Huauya-Leuyacc, M.E. Antimicrobial activity and antiadherent effect of Peruvian Psidium guajava (Guava) leaves on a cariogenic biofilm model. J. Contemp. Dent. Pract. 2020, 21, 739–745. [Google Scholar] [CrossRef]
- Organismo Andino de Salud-Convenio Hipólito Unanue (ORAS-CONHU). Plantas Medicinales de la Subregión Andina; ORAS-CONHU: Lima, Peru, 2014. [Google Scholar]
- Agarwal, A.; Chaudhary, B. Clinical and microbiological effects of 1% Matricaria chamomilla mouth rinse on chronic periodontitis: A double-blind randomized placebo-controlled trial. J. Indian Soc. Periodontol. 2020, 24, 354–361. [Google Scholar] [CrossRef]
- Sánchez-Tito, M.A.; Cartagena-Cutipa, R.; Flores-Valencia, E.; Castillo-Pérez, Y.; Nicó-Navarro, A.M. Chemical composition and antimicrobial activity of essential oil from Minthostachys mollis against oral pathogens. Rev. Cub. Estomatol. 2021, 58, e3647. [Google Scholar]
- Paucar-Rodríguez, E.; Peltroche-Adrianzen, N.; Cayo-Rojas, C.F. Actividad antibacteriana y antifúngica del aceite esencial de Minthostachys mollis frente a microorganismos de la cavidad oral. Rev. Cub. Investig. Bioméd. 2021, 40 (Suppl. 1), e1450. [Google Scholar]
- Idir, F.; Van Ginneken, S.; Coppola, G.A.; Grenier, D.; Steenackers, H.P.; Bendali, F. Origanum vulgare ethanolic extracts as a promising source of compounds with antimicrobial, anti-biofilm, and anti-virulence activity against dental plaque bacteria. Front. Microbiol. 2022, 13, 999839. [Google Scholar] [CrossRef]
- Potra-Cicalău, G.I.; Ciavoi, G.; Todor, L.; Iurcov, R.C.; Iova, G.; Ganea, M.; Scrobotă, I. The benefits of Calendula officinalis extract as therapeutic agent in oral healthcare. Med. Evol. 2022, 28, 59–64. [Google Scholar] [CrossRef]
- Zhao, X.X.; Lin, F.J.; Li, H.; Li, H.B.; Wu, D.T.; Geng, F.; Ma, W.; Gan, R.Y. Recent advances in bioactive compounds, health functions and safety concerns of onion (Allium cepa L.). Front. Nutr. 2021, 8, 669805. [Google Scholar] [CrossRef]
- Kamran, M.A.; Alnazeh, A.A.; Almoammar, S.; Almagbol, M.; Baig, E.A.; Alrwuili, M.R.; Aljabab, M.A.; Alshahrani, I. Effect of plant-based mouthwash (Morinda citrifolia and Ocimum sanctum) on TNF-α, IL-α, IL-β, IL-2, and IL-6 in gingival crevicular fluid and plaque scores of patients undergoing fixed orthodontic treatment. Medicina 2023, 59, 1968. [Google Scholar] [CrossRef] [PubMed]
- Rahmawati, D.Y.; Kurniawan, V.F.; Sanjaya, O.T.C.; Sugiama, V.K.; Mandalas, H.Y. Antibacterial effects of tomato ethanol extract (Solanum lycopersicum L.) against S. mutans and P. gingivalis: A laboratory experiment. Padjadjaran J. Dent. 2023, 35, e50582. [Google Scholar] [CrossRef]
- Lugo-Flores, M.A.; Quintero-Cabello, K.P.; Palafox-Rivera, P.; Silva-Espinoza, B.A.; Cruz-Valenzuela, M.R.; Ortega-Ramirez, L.A.; Gonzalez-Aguilar, G.A.; Ayala-Zavala, J.F. Plant-derived substances with antibacterial, antioxidant, and flavoring potential to formulate oral health care products. Biomedicines 2021, 9, 1669. [Google Scholar] [CrossRef]
- Das, M.; Panda, N.R.; Bhuyan, R.; Bhuyan, S.K. Moringa oleifera and its application in dental conditions: A systematic review and meta-analysis. J. Herbmed Pharmacol. 2023, 12, 331–336. [Google Scholar] [CrossRef]
- Zuttion, G.S.; Juárez, H.A.B.; Lima, B.D.; Assumpção, D.P.; Daneris, Â.P.; Tuchtenhagen, I.H.; Casarin, M.; Muniz, F.W.M.G. Comparison of the anti-plaque and anti-gingivitis efficacy of chlorhexidine and Malva mouthwashes: Randomized crossover clinical trial. J. Dent. 2024, 150, 105313. [Google Scholar] [CrossRef]
- Günther, M.; Karygianni, L.; Argyropoulou, A.; Anderson, A.C.; Hellwig, E.; Skaltsounis, A.L.; Wittmer, A.; Vach, K.; Al-Ahmad, A. The antimicrobial effect of Rosmarinus officinalis extracts on oral initial adhesion ex vivo. Clin. Oral Investig. 2022, 26, 4369–4380. [Google Scholar] [CrossRef]
- Bayas-Morejón, F.; Ramón, R.R.; García-Pazmiño, M.; Mite-Cárdenas, G. Antibacterial and antioxidant effect of natural extracts from Baccharis latifolia (Chilka). Caspian J. Environ. Sci. 2020, 18, 489–493. [Google Scholar] [CrossRef]
- Greene, A.C.; Acharya, A.P.; Lee, S.B.; Gottardi, R.; Zaleski, E.; Little, S.R. Cranberry extract-based formulations for preventing bacterial biofilms. Drug Deliv. Transl. Res. 2021, 11, 1144–1155. [Google Scholar] [CrossRef]
- Xue, Q.; Xiang, Z.; Wang, S.; Cong, Z.; Gao, P.; Liu, X. Recent advances in nutritional composition, phytochemistry, bioactive, and potential applications of Syzygium aromaticum L. (Myrtaceae). Front. Nutr. 2022, 9, 1002147. [Google Scholar] [CrossRef]
- El-Saber Batiha, G.; Alkazmi, L.M.; Wasef, L.G.; Beshbishy, A.M.; Nadwa, E.H.; Rashwan, E.K. Syzygium aromaticum L. (Myrtaceae): Traditional uses, bioactive chemical constituents, pharmacological and toxicological activities. Biomolecules 2020, 10, 202. [Google Scholar] [CrossRef]
- Safarabadi, M.; Ghaznavi-Rad, E.; Pakniyat, A.; Rezaie, K.; Jadidi, A. Comparing the effect of Echinacea and chlorhexidine mouthwash on the microbial flora of intubated patients admitted to the intensive care unit. Iran J. Nurs. Midwifery Res. 2017, 22, 481–485. [Google Scholar] [CrossRef]
- Ahmadi, F. Phytochemistry, mechanisms, and preclinical studies of Echinacea extracts in modulating immune responses to bacterial and viral infections: A comprehensive review. Antibiotics 2024, 13, 947. [Google Scholar] [CrossRef] [PubMed]
- Kaboua, K.; Pakoussi, T.; Mouzou, A.; Assih, M.; Kadissoli, B.; Dossou-Yovo, K.M.; Bois, P. Toxicological evaluation of Hydrocotyle bonariensis Comm. ex Lamm (Araliaceae) leaves extract. Beni-Suef Univ. J. Basic Appl. Sci. 2021, 10, 69. [Google Scholar] [CrossRef]
- Shivananda, S.; Doddawad, V.G.; Bhuyan, L.; Shetty, A.; Pushpa, V.H. Assessment of the antibacterial activity of Spilanthes acmella against bacteria associated with dental caries and periodontal disease: An in vitro microbiological study. J. Pure Appl. Microbiol. 2024, 18, 476–482. [Google Scholar] [CrossRef]
- Daga-Mauricio, K.M.; Castillo-Saavedra, E.F.; Reyes-Alfaro, C.E.; Salas-Sánchez, R.M.; Vargas-Vigo, J.E. Enfermedad bucodental y masticación de hoja de coca en pobladores peruanos [Oral disease and coca leaf chewing in Peruvian residents]. Av. Odontoestomatol. 2024, 40, 78–83. Available online: https://scielo.isciii.es/pdf/odonto/v40n2/0213-1285-odonto-40-2-78.pdf (accessed on 7 September 2025).
- Dayal, S.D.; Pushpa Rani, V.; Antony Prabhu, D.; Rajeshkumar, S.; David, D.; Francis, J. Formulation and evaluation of Phaseolus lunatus seed coat mediated silver nanoparticles mouthwash: A comprehensive study on biomedical properties and toxicological assessment. Microb. Pathog. 2024, 197, 107033. [Google Scholar] [CrossRef]
- Ghorbani, A.; Ghasemzadeh, Z.; Ghaffari Hamedani, S.M.M.; Akbari, J.; Moosazadeh, M.; Mirzaee, F.; Zamanzadeh, M.; Shahani, S. Efficacy of black mulberry mouthwash for prevention of chemotherapy-induced oral mucositis: A double-blind randomized clinical trial. Front. Dent. 2025, 22, 10. [Google Scholar] [CrossRef]
- Yildirim, T.T.; Ozan, G.; Dundar, S.; Bozoglan, A.; Karaman, T.; Dildes, N.; Kaya, C.A.; Kaya, N.; Erdem, E. The effects of Morus nigra on the alveolar bone loss in experimentally induced periodontitis. Eur. Oral Res. 2019, 53, 99–105. [Google Scholar] [CrossRef]
- Halboub, E.; Al-Maweri, S.A.; Al-Wesabi, M.; Al-Kamel, A.; Shamala, A.; Al-Sharani, A.; Koppolu, P. Efficacy of propolis-based mouthwashes on dental plaque and gingival inflammation: A systematic review. BMC Oral Health 2020, 20, 198. [Google Scholar] [CrossRef] [PubMed]
| Etiology | Symptoms | Risk Factors | Clinical Management | References | |
|---|---|---|---|---|---|
| Caries | Bacterial acids cause demineralization of both enamel and dentin. | Thermal sensitivity, progressive pain, pulpitis in advanced cases. | Sugar consumption, poor hygiene, genetic predisposition. | Remineralization, restorations, and root canal treatment in severe cases. | [17,18] |
| Enamel Fracture | Trauma, bruxism, extensive restorations. | Pain while chewing, thermal sensitivity, and visible fracture in some cases. | Bruxism, repeated trauma, poorly fitted restorations. | Resin or crowns are used for moderate fractures, and root canal treatment is performed if the pulp is affected. | [17] |
| Dental Crack | Microfractures allow bacterial infiltration. | Discomfort while chewing, progressive sensitivity, and recurrent cavities. | Enamel wear, trauma, acidic diet. | Fissure sealants, preventive restorations. | [19] |
| Irritation | Acidic or irritating dental materials. | Burning sensation, temporary discomfort in soft tissues. | Improper use of dental materials, pre-existing hypersensitivity. | Use desensitizing agents to adjust adhesive materials. | [19] |
| Root Exposure | Gingival recession due to periodontitis or aggressive brushing. Bacterial biofilm causes inflammation and destruction of periodontal tissue. | Pain with thermal stimuli, persistent hypersensitivity. | Aggressive brushing, periodontal disease, aging. | Desensitizing toothpaste, changes in brushing technique. | [20] |
| Periodontal Disease | Bacterial biofilm causes inflammation and destruction of periodontal tissue. | Gingival bleeding, inflammation, tooth mobility, abscesses. | Poor hygiene, smoking, systemic diseases (diabetes). | Biofilm control, scaling, and root planing, periodontal surgery if necessary. | [17,21] |
| Criteria/Plant | Zingiber officinale Roscoe (Zingiberaceae) | Eucalyptus globulus Labill. (Myrtaceae) | Calendula officinalis L. (Asteraceae) | Psidium guajava L. (Myrtaceae) |
|---|---|---|---|---|
| Uses | Expectorant, antitussive, anti-inflammatory, antioxidant | Antiseptic, anti-inflammatory, antibacterial, analgesic, disinfectant | Anti-inflammatory, healing | Astringent, antimicrobial, immunological |
| Indications | Stomach pain, nausea, cold, arthritis, xerostomia, gingivitis | Gingivitis, bronchitis, asthma, pharyngitis, diabetes, cystitis, tonsillitis | Gingivitis, stomatitis, ulcers | Gingivitis, ulcers, diarrhea, gastritis, cavities |
| Dosage | Powder, soups, purees; 250–1000 mg/day (~400 mg/day) | 10 mL mouthwash, twice daily for 5 min, for 14 days | Mouth rinse prepared by diluting 2 mL mother tincture in 6 mL water (1:3), twice daily for 6 months | Guava leaf extract (0.15%) used as mouth rinse: 10 mL diluted 1:1 with water, twice daily for 30 days |
| Compounds | Terpenes derivatives, gingerol, shogaol | Essential oil, tannins, flavonoids, glycosides | Essential oils, salicylic acid, flavonoids | Tannins, flavonoids, vitamin C |
| Countries | Australia, India, Jamaica, China, Peru, Brazil | Colombia, Venezuela, Argentina, Brazil | Colombia, Mexico, Brazil, Peru | Bolivia, Colombia, Mexico, Brazil, Peru |
| Safety/ Contraindications | Avoid in patients taking anticoagulants (warfarin, aspirin) → bleeding risk; high doses cause gastric irritation; not recommended in pregnancy (large amounts) | Avoid ingestion of concentrated essential oil (toxic); contraindicated in pregnancy and children <6 years; may cause mucosal irritation | Avoid in patients allergic to Asteraceae family; not recommended in pregnancy/lactation without supervision | Safe in moderate use; avoid in hypersensitivity; high doses may cause constipation or mucosal irritation |
| Evidence type | Pilot randomized cross-over, single-blind clinical trial. | Randomized controlled clinical trial, in vivo, with 74 human participants (no caries or periodontal disease) | In vivo, randomized controlled clinical trial in humans (n = 240, gingivitis patients). | In vivo, randomized, double-blind, controlled clinical trial. |
| Primary targets/pathways | Postoperative pain control (Visual Analogue Scale—VAS). Gingival inflammation reduction (Modified Gingival Index—MGI). | Inhibition of bacterial biofilm formation (measured via absorbance and crystal violet staining) | Dental plaque formation, gingival inflammation, and sulcular bleeding (clinical pathways assessed via PI, GI, SBI, OHI-S). | Plaque Index (PI) Gingival Index (GI) Microbial counts (CFU) in plate samples. Salivary antioxidant levels. |
| Oral results/indications | Ginger powder may be a safe alternative to ibuprofen for managing postoperative pain and gingival inflammation in periodontal surgery | Eucalyptus oil can be used as an effective alternative to chlorhexidine for oral hygiene maintenance, without adverse effects. | The Calendula mouthwash is effective in reducing dental plaque and gingivitis, serving as a useful adjunct to scaling. | Comparable to chlorhexidine and superior to placebo in reducing PI, GI, and microbial counts. Improved salivary antioxidant levels (not statistically significant). Useful adjunct to professional prophylaxis. |
| References | [40,41,42] | [43,44,45] | [46,47] | [46,47,48] |
| Criteria/Plant | Origanum vulgare L. (Lamiaceae) | Aloe vera (L.) Burm.f (Asphodelaceae) | Ocimum sanctum L. (Lamiaceae) | Moringa oleifera Lam. (Moringaceae) |
|---|---|---|---|---|
| Uses | Antioxidant, antimicrobial, antifungal | Antioxidant, antimicrobial, anti-inflammatory, astringent, analgesic, healing | Antimicrobial and antiparasitic activity, carminative, antispasmodic, sedative, insecticide | Digestive, anti-inflammatory, antimicrobial, antiparasitic |
| Indications | Indicated for combating bacterial strains | Gingivitis, periodontitis, gut flora, burns, ulcers, stomatitis | Biofilm control, digestive discomfort, dyspepsia, bloating | Periodontitis, nervous disorders, circulatory system disorders |
| Dosage | Oil | 10 mL, twice daily; 2% gel, three times daily for ≥10 days | Mouthwash with aqueous holy basil extract (3.5 g%), used twice daily for 4 days | 5 mL, twice daily for 28 days in young adults with gingivitis |
| Compounds | Carvacrol, thymol, apigenin, luteolin, aglycones, alcohols | Aloin A and B, aloesin A, B, and C, glucomannans, polysaccharides, tannins, saponins | Eugenol, linalool, estragole, carotenoids, calcium, phosphorus | Minerals: calcium, iron, magnesium, zinc. Vitamins: B1, B2, B3, C, E, K. Includes antioxidants |
| Countries | Chile, Bolivia, Peru | Mexico, Dominican Republic, Venezuela, China, Brazil, Colombia | Mexico, Colombia, Venezuela, Bolivia, Iran, India, Pakistan | Cuba, Guatemala, Mexico, Colombia, Venezuela, Spain |
| Safety/ Contraindications | Generally well tolerated; high doses may cause abdominal discomfort, nausea, constipation/diarrhea, dizziness, headache. Rare hypersensitivity reactions. Contraindicated in pregnancy (abortifacient risk). | Avoid in pregnancy (risk of uterine contractions/abortifacient). Possible GI discomfort (diarrhea, constipation, nausea), headache, dizziness, rare hypersensitivity. | May significantly prolong prothrombin time; caution in patients on anticoagulant therapy. | A clinical case of pulmonary embolism reported after prolonged use of Moringa leaf extract; caution in patients on anticoagulants/antiplatelets or with bleeding disorders. |
| Evidence type | In vitro study (disk diffusion, MIC, MBC, biofilm assays, RT-qPCR, molecular docking, cytotoxicity test on HaCaT cells). | In vivo, randomized controlled clinical trial (30 orthodontic patients, Aloe vera vs. 0.2% chlorhexidine, 35 days). | In vivo, triple-blind randomized controlled clinical trial | In vivo, randomized clinical crossover study (20 subjects with mild to moderate gingivitis). |
| Primary targets/ pathways | Virulence genes of S. mutans (gtfB/C/D, spaP, gbpB, vicR, relA, brpA); inhibition of acid production, hydrophobicity, and biofilm formation. Key compounds: carvacrol, γ-terpinene, p-cymene. | ↓ IL-1β, IL-17 (GCF), ↑ fibroblast migration, ↓ P. gingivalis biofilm | COX-2 and LOX enzyme inhibition (anti-inflammatory); NF-κB pathway and cytokine (TNF-α, IL-6) suppression, esp. via eugenol (in THP-1 cells) | Inhibition of Streptococcus mutans growth and cariogenic biofilm; phenolic compounds in ethanol extract likely interfere with bacterial adhesion and acid production. |
| Oral results/indications | potential anti-caries agent due to anti-biofilm and anti-virulence activity. | Significant reduction in PI, GI, and BOP from baseline to day 35 in both groups. Aloe vera mouthwash showed effects comparable to chlorhexidine, with no adverse effects reported. | Comparable to chlorhexidine in reducing PI, GI, and gingival bleeding; significantly better than placebo; no adverse effects reported. | Significant reduction in PI and GI compared to baseline and miswak dentifrice. Demonstrated efficacy in reducing plaque accumulation and gingival inflammation. Safe and effective as an adjunctive oral hygiene aid. |
| References | [49,50,51,52] | [49,53,54,55,56] | [49,57,58,59,60] | [15,49,61,62,63] |
| Plant (Family) | Interactions (e.g., Anticoagulants) | Allergy Risks | Pregnancy/Lactation | Mucosal Irritation | Dose/Form/Duration | Evidence Type | References |
|---|---|---|---|---|---|---|---|
| Zingiber officinale Roscoe (Zingiberaceae) | Avoid with anticoagulants (warfarin, aspirin); bleeding risk at high doses | Rare hypersensitivity | Not recommended in pregnancy (large amounts) | May cause gastric irritation | Up to 1000 mg/day (powdered form) | Clinical and experimental | [40,41,42] |
| Eucalyptus globulus Labill. (Myrtaceae) | None reported; avoid ingestion of essential oil (toxic) | Possible allergic reaction in sensitive individuals | Contraindicated in pregnancy and children <6 years | May cause mucosal irritation | Used as infusion or diluted essential oil | Clinical reports | [43,44,45] |
| Calendula officinalis L. (Asteraceae) | None reported | Contraindicated in Asteraceae allergy | Not recommended during pregnancy or lactation without supervision | Mild irritation in sensitive individuals | Topical or oral rinse | Clinical and ethnobotanical | [46,47] |
| Psidium guajava L. (Myrtaceae) | None reported | Avoid in hypersensitivity | Generally safe in moderate use | Possible mild irritation at high doses | Oral gel, infusion, topical | Clinical and ethnobotanical | [48,49] |
| Origanum vulgare L. (Lamiaceae) | Possible interaction with anticoagulants at high doses | Rare hypersensitivity | Contraindicated in pregnancy (abortifacient risk) | GI discomfort (nausea, diarrhea, dizziness) | Oil or fluid extract | Clinical and ethnobotanical | [49,50,51,52] |
| Aloe vera (L.) Burm.f. (Asphodelaceae) | None reported | Rare hypersensitivity | Avoid in pregnancy (risk of uterine contractions) | Possible GI discomfort (diarrhea, nausea, dizziness) | Topical gel or mouth rinse | Clinical trials | [49,53,54,55,56] |
| Ocimum sanctum L. (Lamiaceae) CE | May prolong prothrombin time; caution with anticoagulant therapy | None reported | Not reported | None reported | Mouthwash, twice daily for 4 days | Clinical | [49,57,58,59,60] |
| Moringa oleifera Lam. (Moringaceae) | Caution in patients on anticoagulants/antiplatelets | None reported | Use with caution in pregnancy | None reported | 5 mL leaf extract twice daily for 28 days | Clinical and ethnobotanical | [15,49,61,62,63] |
| # | Common Name | Scientific Name | Traditional/Dental Uses | Relevant Pharmacological Activity | Precautions/Contraindications | Administration/Form | Countries Reported in Latin America | Main References |
|---|---|---|---|---|---|---|---|---|
| 1 | Anamú | Petiveria alliacea L. (Petiveriaceae) | Dental pain, oral inflammation. | Anti-inflammatory, analgesic, antimicrobial | Pregnancy, lactation, prolonged use | Infusion, poultice | Colombia, Venezuela, Brazil | [64] |
| 2 | Cadillo | Bidens pilosa L. (Asteraceae) | Mouth ulcers, gastric ulcers. | Anti-inflammatory, healing | Pregnancy, lactation, kidney failure | Infusion, syrup, capsules | Peru, Colombia, Central America | [65] |
| 3 | Mountain cinnamon | Drimys winteri J.R.Forst. & G.Forst. (Winteraceae) | Allergic processes, stomach pain; reduces bacterial plaque index. | Analgesic, anti-inflammatory | Not reported | Infusion (oral) | Chile, Argentina | [66] |
| 4 | Chaparro | Curatella americana L. (Dilleniaceae) | Effective against Candida albicans, C. tropicalis, and C. parapsilosis, all highly relevant in oral candidiasis and denture stomatitis. | Anti-inflammatory, astringent | Pregnancy/reproductive effects: may alter estrous cycle and embryonic development; caution in pregnancy | Infusion (oral) | Brazil (Cerrado), Venezuela, Colombia | [67] |
| 5 | Chilca | Baccharis latifolia (Ruiz & Pav.) Pers. (Asteraceae) | Stomach pain, oral inflammations. | Anti-inflammatory, antioxidant | Safety not established; lacks pharmacological/toxicological validation | Infusion (oral, topical) | Peru, Bolivia, Colombia | [68] |
| 6 | Cilantro | Coriandrum sativum | Efficacy against Candida spp. isolated from the oral cavity of patients with periodontitis, including Candida albicans. | Anti-inflammatory, antimicrobial | Pregnancy, lactation, children <3 years | Infusion (oral) | Brazil, Colombia, Central America | [69] |
| 7 | Guava | Psidium guajava L. (Myrtaceae) | Comparable to chlorhexidine and superior to placebo in reducing PI, GI, and microbial counts. Improved salivary antioxidant levels (not statistically significant). Useful adjunct to professional prophylaxis. | Local anti-inflammatory | Hypersensitivity to the plant | Topical gel | Colombia (endemic) | [70] |
| 8 | Gualanday | Jacaranda caucana Pittier (Bignoniaceae) | Leishmaniasis, boils, skin infections, oral inflammation. | Antiseptic, healing | External use only | Topical gel | Colombia (endemic) | [71] |
| 9 | Plantain | Plantago major L. (Plantaginaceae) | Aqueous mouthwash trial in a patient reduced gingival inflammation and dental biofilm without side effects. | Healing, anti-inflammatory | External use only | Topical (poultice, ointment) | Colombia, Ecuador, Bolivia | [71] |
| 10 | Chamomile (EC) | Matricaria chamomilla L. (Asteraceae) (syn. Matricaria recutita L.). | Gingivitis, dental pain, oral inflammation, reduced plaque. | Anti-inflammatory, antispasmodic | Hypersensitivity | Infusion, oral extract | Colombia, Bolivia, Peru | [72] |
| 11 | Cashew | Minthostachys mollis (Benth.) Griseb. (Lamiaceae) | Essential oil effectively inhibited Candida albicans in a dental-relevant model. | Anti-inflammatory, hypoglycemic | Contact dermatitis, CNS toxicity in excess | Bark decoction (oral) | Colombia, Brazil, Venezuela | [71,73] |
| 12 | Muña | Minthostachys mollis | Essential oil active against E. faecalis, P. gingivalis, and C. albicans (most sensitive); key compounds: menthone and eucalyptol. | Antimicrobial against Streptococcus mutans | Prolonged or high-dose use linked to liver and lung toxicity in animal studies; caution advised due to possible hepatotoxic effects | Infusion, tincture | Ecuador, Peru, Bolivia | [71,74] |
| 13 | Oregano (EC) | Origanum vulgare L. (Lamiaceae) | Potential anti-caries agent due to anti-biofilm and anti-virulence activity. | Antioxidant, antimicrobial, antifungal | Generally well tolerated; high doses may cause abdominal discomfort, nausea, constipation/diarrhea, dizziness, headache Rare hypersensitivity reactions Contraindicated in pregnancy (abortifacient risk) | Oil, fluid extract | Chile, Bolivia, Peru, Colombia | [75] |
| 14 | Arnica (EC) | Arnica montana L. (Asteraceae) | Arnica reduced post-extraction pain almost as effectively as ibuprofen, with good tolerance and no adverse effects. | Topical anti-inflammatory, analgesic | Risk of gastrointestinal irritation and for safety reasons typical of homeopathic preparations | Gel, cream, topical tincture | Bolivia, Mexico, Colombia | [71] |
| 15 | Calendula (EC) | Calendula officinalis L. (Asteraceae) | The Calendula mouthwash is effective in reducing dental plaque and gingivitis, serving as a useful adjunct to scaling. | Anti-inflammatory, healing, antimicrobial | Hypersensitivity | Infusion, mouth rinse, cream | Bolivia, Colombia, Chile, Peru | [47,76] |
| 16 | Aloe | Aloe vera (L.) Burm.f. (Asphodelaceae) | Significant reduction in PI, GI, and BOP from baseline to day 35 in both groups. Aloe vera mouthwash showed effects comparable to chlorhexidine, with no adverse effects reported. | Anti-inflammatory, healing, antimicrobial | Avoid in pregnancy (risk of uterine contractions/abortifacient). Possible GI discomfort (diarrhea, constipation, nausea), headache, dizziness, rare hypersensitivity | Topical gel, mouth rinse | Colombia, Bolivia, Mexico, Venezuela | [49,53,54,55,56] |
| 17 | Onion (EC) | Allium cepa L. (Amaryllidaceae) | Bactericidal activity even in resting cells and remained stable after 48 h; promising for preventing dental caries and periodontitis. | Antimicrobial, healing, anti-inflammatory | Gastric irritation if in excess | Extract, poultice, infusion | Colombia, Bolivia, Mexico, Peru | [71,77] |
| 18 | Basil (EC) | Ocimum sanctum L. (Lamiaceae)) | Comparable to chlorhexidine in reducing PI, GI, and gingival bleeding; significantly better than placebo; no adverse effects reported. | Antimicrobial and antiparasitic activity, carminative, antispasmodic, sedative, insecticide | May significantly prolong prothrombin time; caution in patients on anticoagulant therapy | Mouthwash with aqueous holy basil extract (3.5 g%), used twice daily for 4 days | Mexico, Colombia, Venezuela, Bolivia, Iran, India, Pakistan | [78] |
| 19 | Tree tomato | Solanum lycopersicum L. (Solanaceae). | Activity by inhibiting Streptococcus mutans (large inhibition zone) and Porphyromonas gingivalis (moderate effect). | Antioxidant, antihypertensive | Not reported | Infusion, juice | Colombia, Ecuador, Bolivia | [71,79] |
| 20 | Lemon balm (EC) | Melissa officinalis L. (Lamiaceae) | Lemon balm oil hydrogel reduced Candida albicans adhesion on denture surfaces, showing antifungal potential. | Sedative, oral antimicrobial, anti-inflammatory | Not reported | Infusion, extract, essence | Colombia, Ecuador, Bolivia | [71,80] |
| 21 | Lavender (EC) | Lavandula angustifolia Mill. (Lamiaceae) | Lavender oil reduced sulfur compounds from F. nucleatum, showing anti-halitosis potential comparable to chlorhexidine. | Antiseptic, anti-inflammatory, anxiolytic | Animal studies found no acute toxicity or irritation at high doses; human long-term safety still unclear | Infusion, tincture, oil | Chile, Colombia, Bolivia | [71] |
| 22 | Papaya | Carica papaya L. | Stomatitis, post-extraction healing, CPLE toothpaste (± mouthwash) effectively reduced interdental bleeding compared to control. | Anti-inflammatory, healing, proteolytic | Latex may irritate | Juice, latex, seeds | Colombia, Bolivia, Mexico, Peru | [71,79] |
| 23 | Moringa oleifera (EC) | Moringa oleifera Lam. (Moringaceae) | Periodontitis, nervous disorders, circulatory system disorders. | Digestive, anti-inflammatory, antimicrobial, antiparasitic | A clinical case of pulmonary embolism reported after prolonged use of Moringa leaf extract; caution in patients on anticoagulants/antiplatelets or with bleeding disorders | 5 mL, twice daily for 28 days in young adults with gingivitis | Cuba, Guatemala, Mexico, Colombia, Venezuela, Spain | [81] |
| 24 | Chulena | Calceolaria thyrsiflora Graham | Gum inflammation, tongue ulcers. | Oral anti-inflammatory, vulnerary | Not reported | Infusion, rinse | Chile, possibly Bolivia, Colombia | [71] |
| 25 | Vervain | Verbena litoralis Kunth | GI problems, diarrhea, sedative use. | Anti-inflammatory, sedative | CNS depressants, not with alcohol | Extract, oral infusion | Bolivia, Peru, Colombia | [71] |
| 26 | Spearmint (EC) | Mentha spicata L. | Stomach pain, halitosis, oral hygiene. | Antiseptic, digestive, oral antimicrobial | Hypersensitivity, nausea if excessive | Infusion, mouth rinse | Colombia, Bolivia, Peru | [71] |
| 27 | Zingiber officinale Roscoe (Zingiberaceae) (EC) | Zingiber officinale Roscoe (Zingiberaceae) | Ginger powder may be a safe alternative to ibuprofen for managing postoperative pain and gingival inflammation in periodontal surgery. | Expectorant, antitussive, anti-inflammatory, antioxidant | Avoid in patients taking anticoagulants (warfarin, aspirin) → bleeding risk; high doses cause gastric irritation; not recommended in pregnancy (large amounts) | Powder, soups, purees; 250–1000 mg/day (~400 mg/day [46]) | Australia, India, Jamaica, China, Peru, Brazil | [40,41,42] |
| 28 | Proteaceae | Oreocallis grandiflora (Lam.) R. Br. | Treatment of ulcers, mouth rinses for pain, cleansing. | Anti-inflammatory, antimicrobial, healing, antioxidant | toxicity, allergic reactions, limited use | Infusion, decoction, gel, rinse, topical form | Peru, Colombia, Mexico, Brazil | [71] |
| 29 | Amazonian clematis | Clematis guadeloupae Pers. | Preserve teeth, gum relief. | Presumed anti-inflammatory/astringent | Avoid on sensitive mucosa | Bark/stem infusion, poultice | Peru, Bolivia, Colombia, Ecuador | [71] |
| 30 | Lareta | Azorella ruizii (sin. Laretia acaulis) | Topical resin for toothache; decoction digestive. | Topical anti-inflammatory, mild analgesic | Not reported orally | Resin, decoction | Chile, Argentina, Bolivia, Peru | [71] |
| 31 | Mallow (EC) | Malva sylvestris L. | Ulcers, mucositis, dry mouth. In vitro anti-inflammatory co-culture model with periodontal pathogen (Aggregatibacter actinomycetemcomitans). | Oral anti-inflammatory, antimicrobial, anti-caries, healing | No enamel staining observed with hydroalcoholic extract application, suggesting it maintains aesthetic safety | Infusion, rinse, poultice | Latin America (Mexico to Venezuela) | [82] |
| 32 | Maqui | Aristotelia chilensis (Molina) Stuntz | Potential antifungal for oral candidiasis (reduces hyphae and boosts nystatin). | Anti-inflammatory, antimicrobial (anti-Candida), antioxidant | Caution on sensitive mucosa | Infusion, topical extracts | Chile, Argentina, Bolivia, Colombia, Peru | [71] |
| 33 | Walnut (EC) | Juglans regia L. (Juglandaceae) | Decoctions for canker sores, tonsillitis. | Antimicrobial, antifungal, anti-caries, whitening | Juglone may irritate/stain | Decoction rinse | Latin America | [71] |
| 34 | Thyme (EC) | Thymus vulgaris L. (Lamiaceae) | Potential adjunct irrigant in root canal therapy, helping lower NaOCl use and reduce cytotoxicity. | Antimicrobial (S. mutans), anti-inflammatory, antioxidant | May irritate mucosa; avoid in pregnancy/lactation | Infusion, tincture, essential oil, rinse | Chile, Bolivia, Colombia, Peru, Mexico | [71] |
| 35 | Rosemary (EC) | Salvia rosmarinus Spenn. (Rosmarinus officinalis L.) | Rosemary extract dentifrice reduced early Streptococcus mutans biofilm formation, suggesting cariostatic potential. | Antimicrobial (S. mutans, P. gingivalis), anti-inflammatory, antioxidant | Gastric irritation; contraindicated in epilepsy, pregnancy | Infusion, tincture, diluted essential oil | Chile, Bolivia, Colombia, Peru, Mexico, Argentina | [71,83] |
| 36 | Chilca (int.) | Baccharis latifolia (Ruiz & Pav.) Pers. (Asteraceae) | Oral inflammation, ulcers inhibition of S. aureus and E. faecalis (both relevant in endodontic and oral infections) suggests potential applicability in controlling oral Gram-positive pathogens. | Anti-inflammatory, healing, antioxidant, antimicrobial | Avoid in pregnancy/lactation; high doses irritate | Not reported | Bolivia, Colombia, Peru, Ecuador, Chile | [84] |
| 37 | Leliantu | Geum chilense Balb. ex Lindl. (Rosaceae) | Toothache, inflamed gums. The modulatory effect of the extracts on neutrophil function, attributed mainly to gemin A, supports the traditional use of this plant material for oral inflammation, including mucositis, gingivitis, and periodontitis. | Anti-inflammatory, antioxidant, astringent | May affect cyclosporine metabolism | Infusion, decoction, topical use | Chile, Bolivia, Argentina | [71] |
| 38 | Cranberry (EC) | Vaccinium macrocarpon Aiton (Ericaceae) | Antimicrobial and antioxidant. Cranberry mouthwash reduced S. mutans by 68%, showing efficacy comparable to chlorhexidine and supporting its use as an alternative oral rinse. | Anti-biofilm, immunomodulatory | Acidic pH may erode enamel; warfarin interaction | Juice, extract, rinse | Ecuador, Colombia, Bolivia, Peru | [85] |
| 39 | Clove (EC) | Syzygium aromaticum (L.) Merr. & L.M. Perry (Myrtaceae) | Analgesic, antiseptic, Streptococcus mutans; in vitro antimicrobial and antibiofilm assays. | Eugenol: anesthetic, anti-inflammatory, antibacterial, antifungal | Toxic in excess; not in children/pregnancy | Oil, tincture, rinse, paste | Ecuador, Colombia, Peru, Bolivia, Central America | [86,87] |
| 40 | Echinacea (EC) | Echinacea purpurea (L.) Moench (Asteraceae) | Oral rinses for gingivitis, canker sores. Inhibited Streptococcus mutans growth and reduced biofilm formation. Showed antibacterial and antifungal activity against cariogenic bacteria and Candida albicans. Demonstrated low cytotoxicity, suggesting potential as a safe herbal mouthwash. | Anti-inflammatory, immunomodulatory | Hepatotoxic if >8 weeks | Infusion, tincture, capsules, rinse | Ecuador, Colombia, Bolivia, Peru, Central America | [88,89] |
| 41 | Eucalyptus (EC) | Eucalyptus globulus Labill. (Myrtaceae) | Eucalyptus oil can be used as an effective alternative to chlorhexidine for oral hygiene maintenance, without adverse effects. | Anti-inflammatory, antioxidant, antimicrobial | Not for children; mucosa irritation | Infusion, essential oil, rinse | Andes (Ecuador–Chile), Colombia, Peru, Mexico, Brazil | [43,44,45] |
| 42 | Devil’s claw (EC) | Harpagophytum procumbens (Burch.) DC. ex Meisn. (Pedaliaceae) | Periodontitis, oral inflammation. Its strong anti-inflammatory and analgesic properties—effective in arthritis and neuropathic pain models—suggest potential usefulness in managing oral inflammatory conditions such as mucositis or post-procedural pain. | Anti-inflammatory, antioxidant | Contraindicated in pregnancy/lactation | Infusion, capsules, gels | Ecuador, Bolivia, Colombia, Peru, Brazil, Argentina | [71] |
| 43 | Apiaceae (Hydrocotyle) | Hydrocotyle bonariensis Comm. ex Lam. (Araliaceae) | Shows anti-inflammatory and analgesic effects; may help manage oral inflammation, mucositis, or post-procedural pain. | Anti-inflammatory, healing, antioxidant | Not reported | Infusion, decoction, extracts | Peru, Bolivia, Colombia, Ecuador, Brazil, Argentina | [90] |
| 44 | Acmella | Spilanthes acmella (S. acmella), | Toothache, caries, anesthetic. | Analgesic, antimicrobial, healing | Not reported | Infusion, fresh extract | Peru, Bolivia, Colombia, Ecuador, Brazil, Venezuela | [71,91] |
| 45 | Ullucu | Ullucus tuberosus Caldas (Basellaceae) | Toothache, inflammation. | Anti-inflammatory, antimicrobial | No major toxicity; caution with oxalates | Cataplasms, decoctions | Andes (Peru, Bolivia, Colombia, Ecuador, Chile, Argentina) | [71] |
| 46 | Coca | Erythroxylum coca Lam. (Erythroxylaceae) | Toothache, gingival pain. Traditionally used as a natural anesthetic for toothache and oral pain relief—via chewing or poultice application. | Topical anesthetic, analgesic, antimicrobial | Chewing coca leaves may cause oral epithelial changes and is linked to risk of oral squamous cell carcinoma (OSCC), even without classic risk factors | Leaf chewing, infusions, rinses | Andes (Peru, Bolivia, Colombia, Ecuador, Argentina) | [92] |
| 47 | Lima bean | Phaseolus lunatus L. (Fabaceae) | Toothache. | Anti-inflammatory, analgesic, antimicrobial | Unprocessed seeds have cyanogenic compounds and lectins that can release toxic hydrogen cyanide, making proper preparation essential for safe use | Cooking, poultices | Peru, Bolivia, Colombia, Ecuador, Chile, Mexico | [93] |
| 48 | Andean gentian | Gentianella rima (G.Don) Fabris (Gentianaceae) | Toothache, gum inflammation. | Bitter tonic, anti-inflammatory | Not in pregnancy/gastritis | Infusion, decoction | Andes (Peru, Bolivia, Colombia, Ecuador) | [71] |
| 49 | Black mulberry | Morus nigra L. (Moraceae) | Gingivitis, stomatitis, sore throat. Black mulberry juice mouthwash reduced plaque and gingival inflammation, showing comparable effectiveness to chlorhexidine in managing gingivitis. | Anti-inflammatory, antioxidant | Hypoglycemia risk | Infusion, syrup, gargles | Peru, Bolivia, Colombia, Ecuador, Brazil, Mexico, Chile, Paraguay | [94,95] |
| 50 | White myrtle | Luma chequen (Molina) A.Gray (Myrtaceae) | Effective in reducing ulcer severity and improving oral health outcomes in RAS patients, with good safety profile. | Aromatic oils, antimicrobial | Not reported | Infusion, rinse, aromatherapy | Andes (Peru, Chile, Argentina, Bolivia, Ecuador) | [71] |
| Plant (Family) | Interactions (e.g., Anticoagulants) | Allergy Risks | Pregnancy/ Lactation | Mucosal Irritation | Dose/Form/ Duration | Evidence Type/ Main Findings | References |
|---|---|---|---|---|---|---|---|
| Propolis (Apidae product) | Possible interaction with anticoagulants (high doses) | Rare allergic reactions in sensitive individuals (bee-related) | Use with caution during pregnancy and lactation | None reported | Topical gel and oral solution; combined with SRP in Wistar rats (in vivo model) | In vivo study: combined with SRP, significantly reduced IL-1β, TNF-α, and MDA; propolis alone showed no relevant effects. | [96] |
| Aloe vera (L.) Burm.f. (Asphodelaceae) | None reported | Rare hypersensitivity | Safe in animal models; avoid excessive oral use during pregnancy | None reported | Aloe vera gel + β-TCP for 8 weeks in dogs with furcation defects | In vivo study: enhanced periodontal regeneration (bone, PDL fibers, vascularization) with no adverse effects. | [49,53,54,55,56] |
| Basil (Ocimum basilicum L.) (Lamiaceae) | None reported | Possible mild allergy to Lamiaceae family | Not reported | None reported | Hydroalcoholic extract (1–10%) in agar diffusion assays (S. mutans, E. faecalis, S. sanguinis) | In vitro study: demonstrated antibacterial activity with both individual and synergistic effects, although less potent than chlorhexidine. | [57] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramírez-Torres, V.; Torres-León, C.; Londoño-Hernandez, L.; Gómez-García, R.; Ramírez-Guzmán, N. Therapeutic Potential of Latin American Medicinal Plants in Oral Diseases: From Dental Pain to Periodontal Inflammation—A Systematic Review. Int. J. Mol. Sci. 2025, 26, 11502. https://doi.org/10.3390/ijms262311502
Ramírez-Torres V, Torres-León C, Londoño-Hernandez L, Gómez-García R, Ramírez-Guzmán N. Therapeutic Potential of Latin American Medicinal Plants in Oral Diseases: From Dental Pain to Periodontal Inflammation—A Systematic Review. International Journal of Molecular Sciences. 2025; 26(23):11502. https://doi.org/10.3390/ijms262311502
Chicago/Turabian StyleRamírez-Torres, Valentina, Cristian Torres-León, Liliana Londoño-Hernandez, Ricardo Gómez-García, and Nathiely Ramírez-Guzmán. 2025. "Therapeutic Potential of Latin American Medicinal Plants in Oral Diseases: From Dental Pain to Periodontal Inflammation—A Systematic Review" International Journal of Molecular Sciences 26, no. 23: 11502. https://doi.org/10.3390/ijms262311502
APA StyleRamírez-Torres, V., Torres-León, C., Londoño-Hernandez, L., Gómez-García, R., & Ramírez-Guzmán, N. (2025). Therapeutic Potential of Latin American Medicinal Plants in Oral Diseases: From Dental Pain to Periodontal Inflammation—A Systematic Review. International Journal of Molecular Sciences, 26(23), 11502. https://doi.org/10.3390/ijms262311502










