Association Between Genetic Polymorphisms in the Prostaglandin Pathway and the Development of Patent Ductus Arteriosus in Preterm Infants
Abstract
1. Introduction
2. Results
3. Discussion
4. Methods
4.1. Definitions
4.2. Diagnosis of PDA
4.3. Study Design and Data Collection
4.4. Ethics
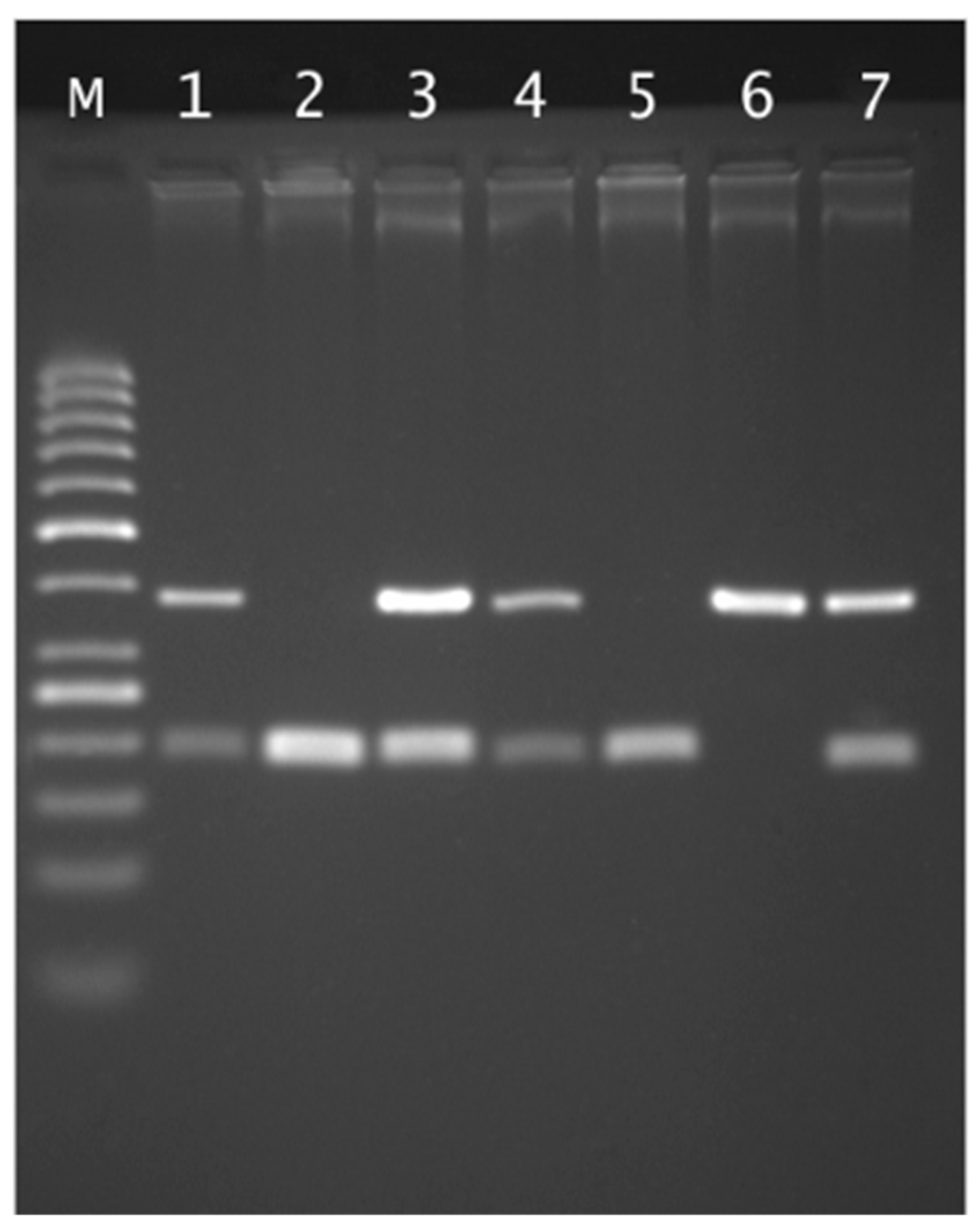
4.5. Genetic Testing Methodology
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gournay, V. The ductus arteriosus: Physiology, regulation, and functional and congenital anomalies. Arch. Cardiovasc. Dis. 2011, 104, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Hundscheid, T.; van den Broek, M.; van der Lee, R.; de Boode, W.P. Understanding the pathobiology in patent ductus arteriosus in prematurity—Beyond prostaglandins and oxygen. Pediatr. Res. 2019, 86, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Mani, A.; Meraji, S.M.; Houshyar, R.; Radhakrishnan, J.; Mani, A.; Ahangar, M.; Rezaie, T.M.; Taghavinejad, M.-A.; Broumand, B.; Zhao, H.; et al. Finding genetic contributions to sporadic disease: A recessive locus at 12q24 commonly contributes to patent ductus arteriosus. Proc. Natl. Acad. Sci. USA 2002, 99, 15054–15059. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, V.; Zhou, G.; Bizzarro, M.J.; Buhimschi, C.; Hussain, N.; Gruen, J.R.; Zhang, H. Genetic contribution to patent ductus arteriosus in the premature newborn. Pediatrics 2009, 123, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Gittenberger-de Groot, A.C.; Strengers, J.L.; Mentink, M.; Poelmann, R.E.; Patterson, D.F. Histologic studies on normal and persistent ductus arteriosus in the dog. J. Am. Coll. Cardiol. 1985, 6, 394–404. [Google Scholar] [CrossRef]
- Bokenkamp, R.; Gittenberger-De Groot, A.C.; Van Munsteren, C.J.; Grauss, R.W.; Ottenkamp, J.; Deruiter, M.C. Persistent ductus arteriosus in the Brown Norway inbred rat strain. Pediatr. Res. 2006, 60, 407–412. [Google Scholar] [CrossRef][Green Version]
- Heymann, M.A.; Rudolph, A.M. Control of the ductus arteriosus. Physiol. Rev. 1975, 55, 62–78. [Google Scholar] [CrossRef]
- Clyman, R.I. Mechanisms regulating the ductus arteriosus. Biol. Neonate 2006, 89, 330–335. [Google Scholar] [CrossRef]
- Coggins, K.G.; Latour, A.; Ngyuen, M.S.; Audoly, L.; Coffman, T.M.; Koller, B.H. Metabolism of PGE 2 by prostaglandin dehydrogenase is essential for remodeling the ductus arteriosus. Nat. Med. 2002, 8, 91–92. [Google Scholar] [CrossRef]
- Rheinlaender, C.; Weber, S.C.; Sarioglu, N.; Strauss, E.; Obladen, M.; Koehne, P. Changing expression of cyclooxygenases and prostaglandin receptor EP4 during development of the human ductus arteriosus. Pediatr. Res. 2006, 60, 270–275. [Google Scholar] [CrossRef]
- Ben-David, Y.; Hallak, M.; Rotschild, A.; Sorokin, Y.; Auslender, R.; Abramovici, H. Indomethacin and fetal ductus arteriosus: Complete closure after cessation of prolonged therapeutic course. Fetal Diagn. Ther. 1996, 11, 341–344. [Google Scholar] [CrossRef]
- Li, L.; Qi, L.; Lv, N.; Gao, Q.; Cheng, Y.; Wei, Y.; Ye, J.; Yan, X.; Dang, A. Association between lipoprotein-associated phospholipase A2 gene polymorphism and coronary artery disease in the Chinese Han population. Ann. Hum. Genet. 2011, 75, 605–611. [Google Scholar] [CrossRef]
- Gu, X.; Lin, W.; Xu, Y.; Che, D.; Tan, Y.; Lu, Z.; Pi, L.; Fu, L.; Zhou, H.; Jiang, Z.; et al. The rs1051931 G>A Polymorphism in the PLA2G7 Gene Confers Resistance to Immunoglobulin Therapy in Kawasaki Disease in a Southern Chinese Population. Front. Pediatr. 2020, 8, 338. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maiolino, G.; Lenzini, L.; Pedon, L.; Cesari, M.; Seccia, T.M.; Frigo, A.C.; Rossitto, G.; Caroccia, B.; Rossi, G.P. Lipoprotein-associated phospholipase A2 single-nucleotide polymorphisms and cardiovascular events in patients with coronary artery disease. J. Cardiovasc. Med. 2015, 16, 29–36, Erratum in J. Cardiovasc. Med. 2015, 16, 259. [Google Scholar] [CrossRef] [PubMed]
- Loftin, C.D.; Trivedi, D.B.; Tiano, H.F.; Clark, J.A.; Lee, C.A.; Epstein, J.A.; Morham, S.G.; Breyer, M.D.; Nguyen, M.; Hawkins, B.M.; et al. Failure of ductus arteriosus closure and remodeling in neonatal mice deficient in cyclooxygenase-1 and cyclooxygenase-2. Proc. Natl. Acad. Sci. USA 2001, 98, 1059–1064. [Google Scholar] [CrossRef]
- Reese, J.; Paria, B.C.; Brown, N.; Zhao, X.; Morrow, J.D.; Dey, S.K. Coordinated regulation of fetal and maternal prostaglandins directs successful birth and postnatal adaptation in the mouse. Proc. Natl. Acad. Sci. USA 2000, 97, 9759–9764. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Camenisch, T.; Snouwaert, J.N.; Hicks, E.; Coffman, T.M.; Anderson, P.A.W.; Malouf, N.N.; Koller, B.H. The prostaglandin receptor EP4 triggers remodelling of the cardiovascular system at birth. Nature 1997, 390, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Yi, X.Y.; Zhou, Q.; Lin, J.; Chi, L.F.; Chi, W.Z. Interaction between ALOX5AP-SG13S114A/T and COX-2-765G/C increases susceptibility to cerebral infarction in a Chinese population. Genet. Mol. Res. 2013, 12, 1660–1669. [Google Scholar] [CrossRef] [PubMed]
- Untergasser, A.; Cutcutache, I.; Koressaar, T.; Ye, J.; Faircloth, B.C.; Remm, M.; Rozen, S.G. Primer3—New capabilities and interfaces. Nucleic Acids Res. 2012, 40, e115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chang, J.P.; Guu, T.W.; Chen, Y.C.; Gałecki, P.; Walczewska, A.; Su, K.P. BanI polymorphism of cytosolic phospholipase A2 gene and somatic symptoms in medication-free acute depressed patients. Prostaglandins Leukot Essent Fat. Acids 2018, 136, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, Q.; Noguti, R.; Bottino, C.M.; Vallada, H. Study of association between genetic polymorphisms of phospholipase A2 enzymes and Alzheimer’s disease. Arq. Neuro-Psiquiatr. 2010, 68, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Zhuo, X.; Guo, B.; Su, C.; Yan, X.; Yan, J.; Hu, S.; Tie, X.; Chen, Y. Lp-PLA2 variants associated with delayed encephalopathy after acute carbon monoxide poisoning. Int. J. Clin. Exp. Med. 2016, 9, 16393–16398. [Google Scholar]
| Characteristic | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| PDA | p | HsPDA | p | PDA vs. HsPDA | p | ||||
| Sex | Female | 12 | p = 0.089 | Female | 7 | p = 1.0 | Female | 12 vs. 7 | p = 1.0 |
| Male | 24 | Male | 14 | Male | 24 vs. 14 | ||||
| Gestational Age (week) | <28 | 18 | p = 0.111 | <28 | 13 | p = 0.176 | <28 | 18 vs. 13 | p = 0.552 |
| >28 | 18 | >28 | 8 | >28 | 18 vs. 8 | ||||
| Birth weight (g) | <1000 g | 17 | p = 0.070 | <1000 g | 13 | p = 0.080 | <1000 g | 17 vs. 13 | p = 0.426 |
| >1000 g | 19 | >1000 g | 8 | >1000 g | 19 vs. 8 | ||||
| Prenatal steroid therapy | Yes | 30 | p = 0.524 | Yes | 18 | p = 1.0 | Yes | 30 vs. 18 | p = 1.000 |
| No | 6 | No | 3 | No | 6 vs. 3 | ||||
| Invasive ventilation | Yes | 23 | p = 0.0069 | Yes | 14 | p = 0.9532 | Yes | 23 vs. 14 | p = 0.552 |
| No | 13 | No | 7 | No | 13 vs. 7 | ||||
| Pharmacological ligation | Yes | 21 | p < 0.0001 | Yes | 21 | p < 0.0001 | Yes | 21 vs. 21 | p = 0.0017 |
| No | 15 | No | 0 | No | 15 vs. 0 | ||||
| Ibuprofen | Yes | 7 | Yes | 7 | Yes | 7 vs. 7 | |||
| No | 0 | No | 0 | No | 0 vs. 0 | ||||
| Paracetamol | Yes | 19 | Yes | 18 | Yes | 19 vs. 18 | |||
| No | 3 | No | 3 | No | 3 vs. 3 | ||||
| Complications | |||||||||
| NEC | Yes | 11 | p = 0.012 | Yes | 5 | p = 0.501 | Yes | 11 vs. 5 | p = 0.895 |
| No | 25 | No | 15 | No | 25 vs. 15 | ||||
| IVH | Yes | 19 | p = 0.0629 | Yes | 14 | p = 0.1017 | Yes | 19 vs. 14 | p = 0.4554 |
| No | 17 | No | 7 | No | 17 vs. 7 | ||||
| BPD | Yes | 26 | p = 0.0075 | Yes | 15 | p = 0.556 | Yes | 26 vs. 15 | p = 1.0000 |
| No | 10 | No | 6 | No | 10 vs. 6 | ||||
| ROP | Yes | 22 | p = 0.048 | Yes | 13 | p = 1.000 | Yes | 22 vs. 13 | p = 1.000 |
| No | 14 | No | 8 | No | 14 vs. 8 | ||||
| Gene | rs Number | Genotypes, N (%) | Alleles | HWE (p-Value) |
|---|---|---|---|---|
| PTGS1 (COX1) | rs1236913 | CC 86 (86.87%) CT 13 (13.13%) TT 0 (0.00%) | C 185 (93.43%) T 13 (6.56%) | 1.000 |
| PTGES2 | rs13283456 | CC 91 (91.92%) CT 7 (7.07%) TT 1 (1.01%) | C 189 (95.45%) T 9 (4.55%) | 0.173 |
| PTGER4 | rs4613763 | TT 68 (68.69%) TC 29 (29.29%) CC 2 (2.02%) | T 165 (83.33%) C 33 (16.67%) | 1.000 |
| PLA2G4A | rs10798059 | GG 35 (35.35%) AG 52 (52.53%) AA 12 (12.12%) | G 122 (61.62%) A 76 (38.38%) | 0.394 |
| PLA2G4C | rs1549637 | TT 77 (77.78%) TA 19 (19.19%) AA 3 (3.03%) | T 173 (87.37%) A 25 (12.63%) | 0.177 |
| PLA2G6 | rs4375 | TT 29 (29.29%) CT 60 (60.61%) CC 10 (10.10%) | T 118 (59.60%) C 80 (40.40%) | 0.013 |
| PLA2G7 | rs1805017 | CC 52 (52.53%) CT 40 (40.40%) TT 7 (7.07%) | C 144 (72.73%) T 54 (27.27%) | 1.000 |
| PLA2G7 | rs1051931 | GG 61 (61.62%) AG 33 (33.33%) AA 5 (5.05%) | G 155 (78.28%) A 43 (21.72%) | 0.773 |
| Model | Genotypes | NO N (%) | YES N (%) | OR (95%CI) | p-Value | AIC |
|---|---|---|---|---|---|---|
| rs1236913 | ||||||
| Codominant | CC | 54 (85.7) | 32 (88.9) | 1.00 | 0.649 | 133.6 |
| CT | 9 (14.3) | 4 (11.1) | 0.75 (0.21–2.63) | |||
| rs13283456 | ||||||
| Codominant | CC | 57 (90.5) | 34 (94.4) | 1.00 | 1.000 | 134.7 |
| CT | 5 (7.9) | 2 (5.6) | 0.67 (0.12–3.65) | |||
| TT | 1 (1.6) | 0 (0.0) | — | |||
| Dominant | CC | 57 (90.5) | 34 (94.4) | 1.00 | 0.474 | 133.3 |
| CT-TT | 6 (9.5) | 2 (5.6) | 0.56 (0.11–2.93) | |||
| Recessive | CC-CT | 62 (98.4) | 36 (100.0) | 1.00 | 1.000 | 132.9 |
| TT | 1 (1.6) | 0 (0.0) | — | |||
| Overdominant | CC-TT | 58 (92.1) | 34 (94.4) | 1.00 | 0.651 | 133.6 |
| CT | 5 (7.9) | 2 (5.6) | 0.68 (0.13–3.71) | |||
| rs4613763 | ||||||
| Codominant | TT | 46(73.0) | 22 (61.1) | 1.00 | 0.470 | 134.3 |
| TC | 16 (25.4) | 13 (36.1) | 1.70 (0.70–4.14) | |||
| CC | 1 (1.6) | 1 (2.8) | 2.09 (0.12–35.01) | |||
| Dominant | TT | 46 (73.0) | 22 (61.1) | 1.00 | 0.222 | 132.3 |
| TC-CC | 17 (27.0) | 14 (38.9) | 1.72 (0.72–4.11) | |||
| Recessive | TT-TC | 62 (98.4) | 35 (97.2) | 1.00 | 0.691 | 133.6 |
| CC | 1 (1.6) | 1 (2.8) | 1.77 (0.11–29.21) | |||
| Overdominant | TT-CC | 47 (74.6) | 23 (63.9) | 1.00 | 0.263 | 132.5 |
| TC | 16 (25.4) | 13 (36.1) | 1.66 (0.68–4.03) | |||
| rs10798059 | ||||||
| Codominant | GG | 23 (36.5) | 12 (33.3) | 1.00 | 0.899 | 135.6 |
| GA | 32 (50.8) | 20 (55.6) | 1.20 (0.49–2.93) | |||
| AA | 8 (12.7) | 4 (11.1) | 0.96 (0.24–3.84) | |||
| Dominant | GG | 23 (36.5) | 12 (33.3) | 1.00 | 0.750 | 133.7 |
| GA-AA | 40 (63.5) | 24 (66.7) | 1.15 (0.49–2.72) | |||
| Recessive | GG-GA | 55 (87.3) | 32 (88.9) | 1.00 | 0.815 | 133.7 |
| AA | 8 (12.7) | 4 (11.1) | 0.86 (0.24–3.08) | |||
| Overdominant | GG-AA | 31 (49.2) | 16 (44.4) | 1.00 | 0.648 | 133.6 |
| GA | 32 (50.8) | 20 (55.6) | 1.21 (0.53–2.76) | |||
| rs1549637 | ||||||
| Codominant | TT | 51 (81.0) | 26 (72.2) | 1.00 | 0.444 | 134.2 |
| TA | 11 (17.5) | 8 (22.2) | 1.43 (0.51–3.98) | |||
| AA | 1 (1.6) | 2 (5.6) | 3.92 (0.34–45.30) | |||
| Dominant | TT | 51 (81.0) | 26 (72.2) | 1.00 | 0.320 | 132.8 |
| TA-AA | 12 (19.0) | 10 (27.8) | 1.63 (0.62–4.28) | |||
| Recessive | TT-TA | 62 (98.4) | 34 (94.4) | 1.00 | 0.282 | 132.6 |
| AA | 1 (1.6) | 2 (5.6) | 3.65 (0.32–41.70) | |||
| Overdominant | TT-AA | 52 (82.5) | 28 (77.8) | 1.00 | 0.566 | 133.5 |
| TA | 11 (17.5) | 8 (22.2) | 1.35 (0.49–3.75) | |||
| rs4375 | ||||||
| Codominant | TT | 19 (30.2) | 10 (27.8) | 1.00 | 0.950 | 135.7 |
| TC | 38 (60.3) | 22 (61.1) | 1.10 (0.43–2.78) | |||
| CC | 6 (9.5) | 4 (11.1) | 1.27 (0.29–5.56) | |||
| Dominant | TT | 19 (30.2) | 10 (27.8) | 1.00 | 0.802 | 133.7 |
| TC-CC | 44 (69.8) | 26 (72.2) | 1.12 (0.45–2.78) | |||
| Recessive | TT-TC | 57 (90.5) | 32 (88.9) | 1.00 | 0.802 | 133.7 |
| CC | 6 (9.5) | 4 (11.1) | 1.19 (0.31–4.52) | |||
| Overdominant | TT-CC | 25 (39.7) | 14 (38.9) | 1.00 | 0.938 | 133.8 |
| TC | 38 (60.3) | 22 (61.1) | 1.03 (0.45–2.39) | |||
| rs1805017 | ||||||
| Codominant | CC | 32 (50.8) | 20 (55.6) | 1.00 | 0.401 | 134.0 |
| CT | 25 (39.7) | 15 (41.7) | 0.96 (0.41–2.25) | |||
| TT | 6 (9.5) | 1 (2.8) | 0.27 (0.03–2.38) | |||
| Dominant | CC | 32 (50.8) | 20 (55.6) | 1.00 | 0.648 | 133.6 |
| CT-TT | 31 (49.2) | 16 (44.4) | 0.83 (0.36–1.88) | |||
| Recessive | CC-CT | 57 (90.5) | 35 (97.2) | 1.00 | 0.178 | 132.0 |
| TT | 6 (9.5) | 1 (2.8) | 0.27 (0.03–2.35) | |||
| Overdominant | CC-TT | 38 (60.3) | 21 (58.3) | 1.00 | 0.847 | 133.7 |
| CT | 25 (39.7) | 15 (41.7) | 1.09 (0.47–2.50) | |||
| rs1051931 | ||||||
| Codominant | GG | 44 (69.8) | 17 (47.2) | 1.00 | 0.028 | 128.7 |
| GA | 18 (28.6) | 15 (41.7) | 2.16 (0.89–5.22) | |||
| AA | 1 (1.6) | 4 (11.1) | 10.35 (1.08–99.38) | |||
| Dominant | GG | 44 (69.8) | 17 (47.2) | 1.00 | 0.027 | 128.9 |
| GA-AA | 19 (30.2) | 19 (52.8) | 2.59 (1.11–6.04) | |||
| Recessive | GG-GA | 62 (98.4) | 32 (88.9) | 1.00 | 0.040 | 129.6 |
| AA | 1 (1.6) | 4 (11.1) | 7.75 (0.83–72.25) | |||
| Overdominant | GG-AA | 45 (71.4) | 21 (58.3) | 1.00 | 0.186 | 132.0 |
| GA | 18 28.6) | 15 (41.7) | 1.79 (0.76–4.22) |
| Genotypes | NO N (%) | YES N (%) | OR (95%CI) | p-Value | AIC | |
|---|---|---|---|---|---|---|
| rs1236913 Codominant | CC | 13 (86.7) | 19 (90.5) | 1.00 | 0.722 | 52.8 |
| CT | 2 (13.3) | 2 (9.5) | 0.68 (0.09–5.49) | |||
| rs13283456 Codominant | CC | 13 (86.7) | 21 (100.0) | 1.00 | 0.167 | 49.2 |
| CT | 2 (13.3) | 0 (0.0) | — | |||
| rs4613763 Codominant | TT | 9 (60.0) | 13 (61.9) | 1.00 | 0.697 | 53.1 |
| TC | 5 (33.3) | 8 (38.1) | 1.11 (0.27–4.51) | |||
| CC | 1 (6.7) | 0 (0.0) | — | |||
| Dominant | TT | 9 (60.0) | 13 (61.9) | 1.00 | 0.908 | 52.9 |
| TC-CC | 6 (40.0) | 8 (38.1) | 0.92 (0.24–3.59) | |||
| Recessive | TT-TC | 14 (93.3) | 21 (100.0) | 1.00 | 0.417 | 51.1 |
| CC | 1 (6.7) | 0 (0.0) | — | |||
| Overdominant | TT-CC | 10 (66.7) | 13 (61.9) | 1.00 | 0.769 | 52.8 |
| TC | 5 (33.3) | 8 (38.1) | 1.23 (0.31–4.93) | |||
| rs10798059 Codominant | GG | 5 (33.3) | 7 (33.3) | 1.00 | 0.190 | 50.0 |
| GA | 10 (66.7) | 10 (47.6) | 0.71 (0.17–3.03) | |||
| AA | 0 (0.0) | 4 (19.0) | — | |||
| Dominant | GG | 5 (33.3) | 7 (33.3) | 1.00 | 1.000 | 52.9 |
| GA-AA | 10 (66.7) | 14 (66.7) | 1.00 (0.25–4.08) | |||
| Recessive | GG-GA | 15 (100.0) | 17 (81.0) | 1.00 | 0.125 | 48.2 |
| AA | 0 (0.0) | 4 (19.0) | — | |||
| Overdominant | GG-AA | 5 (33.3) | 11 (52.4) | 1.00 | 0.254 | 51.6 |
| GA | 10 (66.7) | 10 (47.6) | 0.45 (0.12–1.79) | |||
| rs1549637 Codominant | TT | 12 (80.0) | 14 (66.7) | 1.00 | 0.711 | 52.5 |
| TA | 3 (20.0) | 5 (23.8) | 1.43 (0.28–7.26) | |||
| AA | 0 (0.0) | 2 (9.5) | — | |||
| Dominant | TT | 12 (80.0) | 14 (66.7) | 1.00 | 0.373 | 52.1 |
| TA-AA | 3 (20.0) | 7 (33.3) | 2.00 (0.42–9.49) | |||
| Recessive | TT-TA | 15 (100.0) | 19 (90.5) | 1.00 | 0.500 | 50.7 |
| AA | 0 (0.0) | 2 (9.5) | — | |||
| Overdominant | TT-AA | 12 (80.0) | 16 (76.2) | 1.00 | 0.786 | 52.8 |
| TA | 3 (20.0) | 5 (23.8) | 1.25 (0.25–6.29) | |||
| rs4375 Codominant | TT | 6 (40.0) | 4 (19.0) | 1.00 | 0.350 | 52.8 |
| TC | 8 (53.3) | 14 (66.7) | 2.62 (0.57–12.18) | |||
| CC | 1 (6.7) | 3 (14.3) | 4.50 (0.34–60.15) | |||
| Dominant | TT | 6 (40.0) | 4 (19.0) | 1.00 | 0.168 | 51.0 |
| TC-CC | 9 (60.0) | 17 (81.0) | 2.83 (0.63–12.71) | |||
| Recessive | TT-TC | 14 (93.3) | 18 (85.7) | 1.00 | 0.461 | 52.4 |
| CC | 1 (6.7) | 3 (14.3) | 2.33 (0.22–24.92) | |||
| Overdominant | TT-CC | 7 (46.7) | 7 (33.3) | 1.00 | 0.419 | 52.2 |
| TC | 8 (53.3) | 14 (66.7) | 1.75 (0.45–6.82) | |||
| rs1805017 Codominant | CC | 9 (60.0) | 11 (52.4) | 1.00 - | 0.491 | 52.6 |
| CT | 5 (33.3) | 10 (47.6) | 1.64 (0.41–6.56) | |||
| TT | 1 (6.7) | 0 (0.0) | — | |||
| Dominant | CC | 9 (60.0) | 11 (52.4) | 1.00 | 0.650 | 52.7 |
| CT-TT | 6 (40.0) | 10 (47.6) | 1.36 (0.36–5.22) | |||
| Recessive | CC-CT | 14 (93.3) | 21 (100.0) | 1.00 | 0.417 | 51.1 |
| TT | 1 (6.7) | 0 (0.0) | — | |||
| Overdominant | CC-TT | 10 (66.7) | 11 (52.4) | 1.00 | 0.389 | 52.2 |
| CT | 5 (33.3) | 10 (47.6) | 1.82 (0.46–7.18) | |||
| rs1051931 Codominant | GG | 7 (46.7) | 10 (47.6) | 1.00 | 0.321 | 52.6 |
| GA | 5 (33.3) | 10 (47.6) | 1.40 (0.33–5.93) | |||
| AA | 3 (20.0) | 1 (4.8) | 0.23 (0.02–2.73) | |||
| Dominant | GG | 7 (46.7) | 10 (47.6) | 1.00 | 0.955 | 52.9 |
| GA-AA | 8 (53.3) | 11 (52.4) | 0.96 (0.26–3.63) | |||
| Recessive | GG-GA | 12 (80.0) | 20 (95.2) | 1.00 | 0.151 | 50.8 |
| AA | 3 (20.0) | 1 (4.8) | 0.20 (0.02–2.15) | |||
| Overdominant | GG-AA | 10 (66.7) | 11 (52.4) | 1.00 | 0.389 | 52.2 |
| GA | 5 (33.3) | 10 (47.6) | 1.82 (0.46–7.18) |
| Parameter | Criterion |
|---|---|
| Ductal diameter (measured at the widest point from the pulmonary artery side) | ≥1.5 mm for preterm infants below 27 weeks of gestation ≤2.5 mm for preterm infants above 27 weeks of gestation |
| PDA/LPA (ratio of PDA diameter to left pulmonary artery) | Small < 0.5 Moderate 0.5–1.0 Large > 1.0 |
| La/ao (ratio of anteroposterior left atrium to aortic root) | >1.8 |
| Left ventricular enlargement | LV end-diastolic diameter (LVDd) according to Z-score |
| Flow in descending aorta below the PDA origin | Absence of diastolic flow or retrograde flow during diastole |
| End-diastoliv flow velocity in the left pulmonary artery | >0.2 m/s |
| Flow assessment in the anterior cerebral artery, renal arteries and celiac trunk | Resistance index (RI) > 0.9 |
| Gene | Transcript | Variant ID | Genomic Position (GRCh38.p14) | SNP | Location |
|---|---|---|---|---|---|
| PTGS1 (COX1) | NM_000962.4 | rs3842787 | chr9:122371228 | c.50C>T, p.Pro17Leu | Exon 2 |
| PTGES2 | NM_025072.6 | rs13283456 | chr9:128122474 (GRCh38.p14) | c.893G>A, p. Arg298His (isoform1) | Exon 6 |
| PTGER4 | NC_000005.10 | rs4613763 | chr5:40392626 (GRCh38.p14) | g.40392626T>C | Intergenic variant |
| PLA2G4A | NM_024420.2 | rs10798059 | chr1:186830478 (GRCh38.p14) | c.-70+1443G>A | Intron 1 |
| PLA2G4C | NM_003706.2 | rs1549637 | chr19:48048700 (GRCh38.p14) | c.1581-312T>A | Intron 16 |
| PLA2G6 | NM_003560.2 | rs4375 | chr22:38143034 (GRCh38.p14) | c.609+71A>G | Intron 4 |
| PLA2G7 | NM_005084.4 | rs1805017 | chr6:46716485 (GRCh38.p14) | c.275G>A, p.Arg92His | Exon 4 |
| PLA2G7 | NM_005084.4 | rs1051931 | chr6:46705206 (GRCh38.p14) | c.1136T>A, p.Val379Glu | Exon 11 |
| Variant ID | Primers | Autor | Enzyme |
|---|---|---|---|
| rs3842787 | 5′-GGTGCCCGGTG GGGAATTTTC-3′ 5′-GAGGGGAAAGGAGGGGGTTG-3′ | Yi et al., 2013 [18] | FauI |
| rs13283456 | 5′-CCCACTCTGAGGACAGAACC-3′ 5′-GAGACCCTCTTCCCTGCTG-3′ | Primer3Plus [19] | EcoNI |
| rs4613763 | 5′-CAGCCATGGCATTATCACAG-3′ 5′-GATGGCTAGAATGACCCCAAT-3′ | Primer3Plus [19] | BccI |
| rs10798059 | 5′-TGTGCATTTGCTCAAAGGAG-3′ 5′-ATCTTGGCTCACTGCAACCT-3′ | Chang et al., 2018 [20] | BanI |
| rs1549637 | 5′-TCCACTCCCATGATCCAAACA-3′ 5′-AGAAGACCTGGAAGCCTCTA-3′ | Primer3Plus [19] | BstYI |
| rs4375 | 5′-GGGGTTTATTTTGCTGGGTT-3′ 5′-CAAGGGTGATGGGGAGATC-3′ | Cordeiro et al., 2010 [21] | AvrII |
| rs1805017 | 5′-TCTTCAATCACCACAGCAGC-3′ 5′-TCTGGAGAGTTTGATGGCTT-3′ | Zhao et al., 2016 [22] | BclI |
| rs1051931 | 5′-ATACTGCTTTGTTCCATTGT-3′ 5′-ATCAAGATACCAAGCAAGAAC-3′ | Zhao et al., 2016 [22] | SatI |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minta, M.; Kurzawińska, G.; Minta, Z.-B.; Seremak Mrozikiewicz, A.; Szpecht, D. Association Between Genetic Polymorphisms in the Prostaglandin Pathway and the Development of Patent Ductus Arteriosus in Preterm Infants. Int. J. Mol. Sci. 2025, 26, 9274. https://doi.org/10.3390/ijms26199274
Minta M, Kurzawińska G, Minta Z-B, Seremak Mrozikiewicz A, Szpecht D. Association Between Genetic Polymorphisms in the Prostaglandin Pathway and the Development of Patent Ductus Arteriosus in Preterm Infants. International Journal of Molecular Sciences. 2025; 26(19):9274. https://doi.org/10.3390/ijms26199274
Chicago/Turabian StyleMinta, Marcin, Grażyna Kurzawińska, Zuzanna-Banach Minta, Agnieszka Seremak Mrozikiewicz, and Dawid Szpecht. 2025. "Association Between Genetic Polymorphisms in the Prostaglandin Pathway and the Development of Patent Ductus Arteriosus in Preterm Infants" International Journal of Molecular Sciences 26, no. 19: 9274. https://doi.org/10.3390/ijms26199274
APA StyleMinta, M., Kurzawińska, G., Minta, Z.-B., Seremak Mrozikiewicz, A., & Szpecht, D. (2025). Association Between Genetic Polymorphisms in the Prostaglandin Pathway and the Development of Patent Ductus Arteriosus in Preterm Infants. International Journal of Molecular Sciences, 26(19), 9274. https://doi.org/10.3390/ijms26199274






