Sensitivity of Diffusion Tensor Imaging for Assessing Injury Severity in a Rat Model of Isolated Diffuse Axonal Injury: Comparison with Histology and Neurological Assessment
Abstract
1. Introduction
2. Results
2.1. Neurological Severity Score (NSS)
2.2. Analysis of Immunohistochemistry for β-Amyloid Precursor Protein (β-APP)
2.2.1. β-APP Accumulation in the Thalamus
2.2.2. β-APP Accumulation in the Hypothalamus
2.2.3. β-APP Accumulation in the Hippocampus
2.2.4. β-APP Accumulation in the Neocortex
2.2.5. β-APP Accumulation in the Corpus Callosum
2.3. MRI-Based Neuroimaging Outcomes
2.3.1. Fractional Anisotropy (FA)
2.3.2. Relative Anisotropy (RA)
2.3.3. Axial Diffusivity (AD)
2.3.4. Mean Diffusivity (MD)
2.3.5. Radial Diffusivity (RD)
2.4. Comparison of Sensitivity and Correlation Between NSS, MRI, and Histological Outcomes in a Rat Model of DAI
3. Discussion
4. Materials and Methods
4.1. Animals
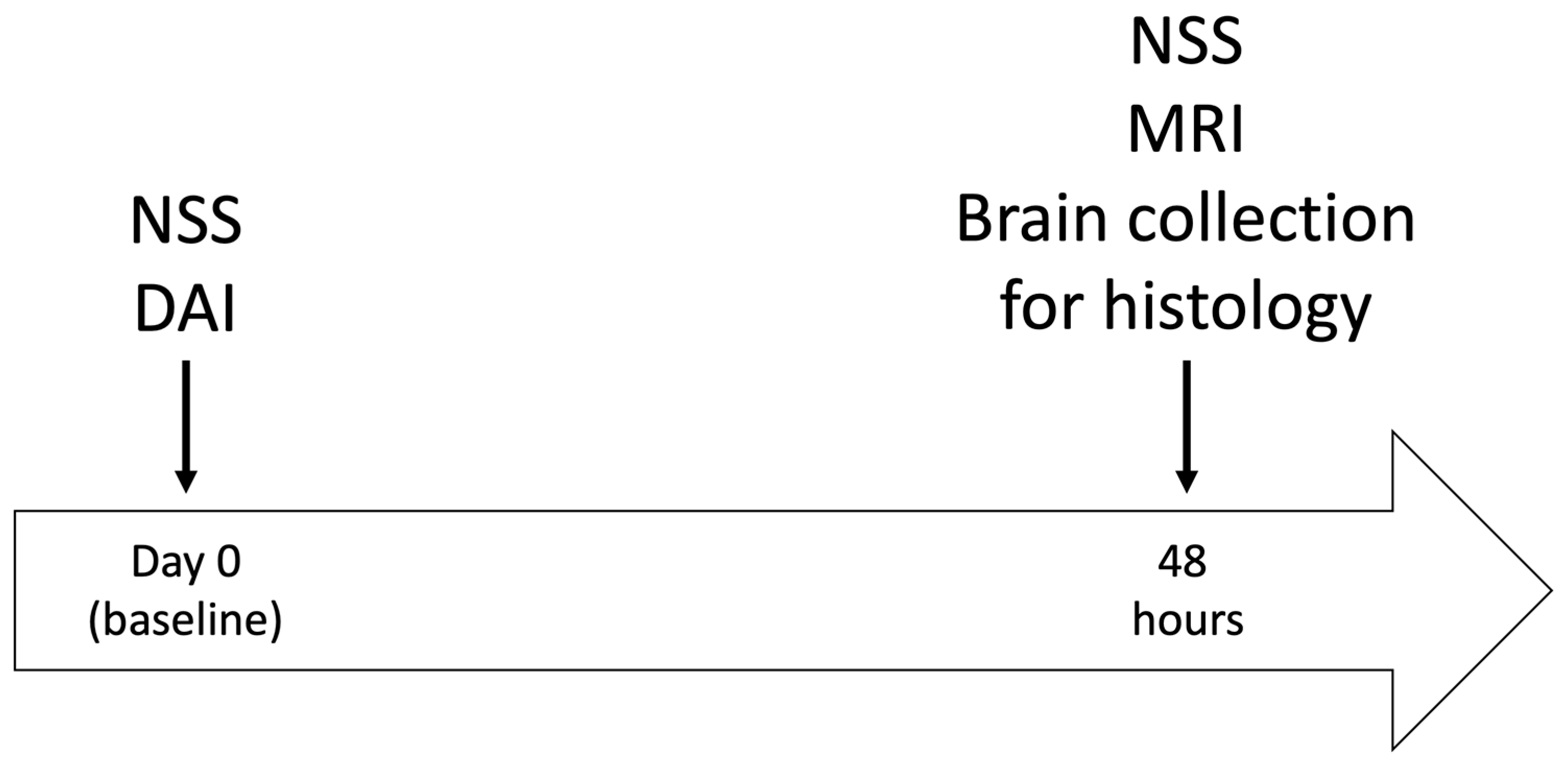
4.2. Experimental Design
4.3. Neurological Severity Score (NSS)
4.4. Induction of DAI
4.5. Histology
4.6. Diffusion-Weighted Imaging (DWI)
4.7. Regions of Interest (ROI)
4.8. Diffusion-Weighted Imaging (DWI) Parameter Map Analysis
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gruenbaum, B.F.; Zlotnik, A.; Oleshko, A.; Matalon, F.; Shiyntum, H.N.; Frenkel, A.; Boyko, M. The relationship between post-traumatic stress disorder due to brain injury and glutamate intake: A systematic review. Nutrients 2024, 16, 901. [Google Scholar] [CrossRef]
- Injury, G. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 56–87. [Google Scholar] [CrossRef]
- Oleshko, A.; Gruenbaum, B.F.; Zvenigorodsky, V.; Shelef, I.; Negev, S.; Merzlikin, I.; Melamed, I.; Zlotnik, A.; Frenkel, A.; Boyko, M. The role of isolated diffuse axonal brain injury on post-traumatic depressive-and anxiety-like behavior in rats. Transl. Psychiatry 2025, 15, 113. [Google Scholar] [CrossRef] [PubMed]
- Drieu, A.; Lanquetin, A.; Prunotto, P.; Gulhan, Z.; Pédron, S.; Vegliante, G.; Tolomeo, D.; Serrière, S.; Vercouillie, J.; Galineau, L. Persistent neuroinflammation and behavioural deficits after single mild traumatic brain injury. J. Cereb. Blood Flow Metab. 2022, 42, 2216–2229. [Google Scholar] [CrossRef] [PubMed]
- Pavlovic, D.; Pekic, S.; Stojanovic, M.; Popovic, V. Traumatic brain injury: Neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary 2019, 22, 270–282. [Google Scholar] [CrossRef] [PubMed]
- Osier, N.D.; Carlson, S.W.; DeSana, A.; Dixon, C.E. Chronic Histopathological and Behavioral Outcomes of Experimental Traumatic Brain Injury in Adult Male Animals. J. Neurotrauma 2015, 32, 1861–1882. [Google Scholar] [CrossRef]
- Wallace, E.; Mathias, J.; Ward, L. The relationship between diffusion tensor imaging findings and cognitive outcomes following adult traumatic brain injury: A meta-analysis. Neurosci. Biobehav. Rev. 2018, 92, 93–103. [Google Scholar] [CrossRef]
- Frank, D.; Gruenbaum, B.F.; Zvenigorodsky, V.; Shelef, I.; Oleshko, A.; Matalon, F.; Tsafarov, B.; Zlotnik, A.; Frenkel, A.; Boyko, M. Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats. Int. J. Mol. Sci. 2024, 25, 4234. [Google Scholar] [CrossRef]
- Boyko, M.; Zvenigorodsky, V.; Grinshpun, J.; Shiyntum, H.N.; Melamed, I.; Kutz, R.; Shelef, I.; Brotfain, E.; Frank, D.; Zlotnik, A. Establishment of novel technical methods for evaluating brain edema and lesion volume in stroked rats: A standardization of measurement procedures. Brain Res. 2019, 1718, 12–21. [Google Scholar] [CrossRef]
- Benjamini, D.; Iacono, D.; Komlosh, M.E.; Perl, D.P.; Brody, D.L.; Basser, P.J. Diffuse axonal injury has a characteristic multidimensional MRI signature in the human brain. Brain 2021, 144, 800–816. [Google Scholar] [CrossRef]
- Hellstrøm, T.; Westlye, L.T.; Kaufmann, T.; Trung Doan, N.; Søberg, H.L.; Sigurdardottir, S.; Nordhøy, W.; Helseth, E.; Andreassen, O.A.; Andelic, N. White matter microstructure is associated with functional, cognitive and emotional symptoms 12 months after mild traumatic brain injury. Sci. Rep. 2017, 7, 13795. [Google Scholar] [CrossRef]
- Sanker, V.; Nordin, E.O.R.; Heesen, P.; Satish, P.; Salman, A.; Dondapati, V.V.K.; Levinson, S.; Desai, A.; Singh, H. Frequency of Diffuse Axonal Injury and Its Outcomes in Severe Traumatic Brain Injury (sTBI): A Systematic Review and Meta-Analysis. J. Neurotrauma 2025. [Google Scholar] [CrossRef]
- Lannsjo, M.; Borg, J.; Lewen, A.; von Seth, C.; Enblad, P.; Abu Hamdeh, S. Long-Term Outcomes of Moderate to Severe Diffuse Axonal Traumatic Brain Injury: A Prospective Study. J. Rehabil. Med. Clin. Commun. 2025, 8, 42299. [Google Scholar] [CrossRef]
- Skandsen, T.; Kvistad, K.A.; Solheim, O.; Strand, I.H.; Folvik, M.; Vik, A. Prevalence and impact of diffuse axonal injury in patients with moderate and severe head injury: A cohort study of early magnetic resonance imaging findings and 1-year outcome. J. Neurosurg. 2010, 113, 556–563. [Google Scholar] [CrossRef]
- Kamagata, K.; Andica, C.; Kato, A.; Saito, Y.; Uchida, W.; Hatano, T.; Lukies, M.; Ogawa, T.; Takeshige-Amano, H.; Akashi, T.; et al. Diffusion Magnetic Resonance Imaging-Based Biomarkers for Neurodegenerative Diseases. Int. J. Mol. Sci. 2021, 22, 5216. [Google Scholar] [CrossRef]
- Andica, C.; Kamagata, K.; Hatano, T.; Saito, Y.; Ogaki, K.; Hattori, N.; Aoki, S. MR Biomarkers of Degenerative Brain Disorders Derived from Diffusion Imaging. J. Magn. Reson. Imaging 2020, 52, 1620–1636. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Han, W.; Kim, H. Diffusion tensor imaging biomarkers for assessing cognitive and physical function in aging. J. Neuroeng. Rehabil. 2025, 22, 157. [Google Scholar] [CrossRef]
- Boyer, R.B.; Kelm, N.D.; Riley, D.C.; Sexton, K.W.; Pollins, A.C.; Shack, R.B.; Dortch, R.D.; Nanney, L.B.; Does, M.D.; Thayer, W.P. 4.7-T diffusion tensor imaging of acute traumatic peripheral nerve injury. Neurosurg. Focus 2015, 39, E9. [Google Scholar] [CrossRef]
- Pusnik, L.; Gabor, A.; Radochova, B.; Janacek, J.; Saudek, F.; Alibegovic, A.; Sersa, I.; Cvetko, E.; Umek, N.; Snoj, Z. High-Field Diffusion Tensor Imaging of Median, Tibial, and Sural Nerves in Type 2 Diabetes with Morphometric Analysis. J. Neuroimaging 2025, 35, e70025. [Google Scholar] [CrossRef] [PubMed]
- Voser, T.; Martin, M.; Muriset, I.; Winkler, M.; Ledoux, J.B.; Aleman-Gomez, Y.; Durand, S. Outcome Prediction by Diffusion Tensor Imaging (DTI) in Patients with Traumatic Injuries of the Median Nerve. Neurol. Int. 2024, 16, 1026–1038. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Gruenbaum, B.F.; Shelef, I.; Zvenigorodsky, V.; Benjamin, Y.; Shapoval, O.; Gal, R.; Zlotnik, A.; Melamed, I.; Boyko, M. A novel histological technique to assess severity of traumatic brain injury in rodents: Comparisons to neuroimaging and neurological outcomes. Front. Neurosci. 2021, 15, 733115. [Google Scholar] [CrossRef] [PubMed]
- Boyko, M.; Gruenbaum, B.F.; Shelef, I.; Zvenigorodsky, V.; Severynovska, O.; Binyamin, Y.; Knyazer, B.; Frenkel, A.; Frank, D.; Zlotnik, A. Traumatic brain injury-induced submissive behavior in rats: Link to depression and anxiety. Transl. Psychiatry 2022, 12, 239. [Google Scholar] [CrossRef]
- Xiong, Y.; Mahmood, A.; Chopp, M. Animal models of traumatic brain injury. Nat. Rev. Neurosci. 2013, 14, 128–142. [Google Scholar] [CrossRef]
- Tsenter, J.; Beni-Adani, L.; Assaf, Y.; Alexandrovich, A.G.; Trembovler, V.; Shohami, E. Dynamic changes in the recovery after traumatic brain injury in mice: Effect of injury severity on T2-weighted MRI abnormalities, and motor and cognitive functions. J. Neurotrauma 2008, 25, 324–333. [Google Scholar] [CrossRef]
- Gentleman, S.M.; Nash, M.J.; Sweeting, C.J.; Graham, D.I.; Roberts, G.W. β-Amyloid precursor protein (βAPP) as a marker for axonal injury after head injury. Neurosci. Lett. 1993, 160, 139–144. [Google Scholar] [CrossRef]
- Sherriff, F.; Bridges, L.; Sivaloganathan, S. Early detection of axonal injury after human head trauma using immunocytochemistry for β-amyloid precursor protein. Acta Neuropathol. 1994, 87, 55–62. [Google Scholar] [CrossRef]
- Blumbergs, P.C.; Scott, G.; Manavis, J.; Wainwright, H.; Simpson, D.A.; McLean, A.J. Topography of axonal injury as defined by amyloid precursor protein and the sector scoring method in mild and severe closed head injury. J. Neurotrauma 1995, 12, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, W.L.; Povlishock, J.T.; Graham, D.L. A mechanistic analysis of nondisruptive axonal injury: A review. J. Neurotrauma 1997, 14, 419–440. [Google Scholar] [CrossRef] [PubMed]
- Tu, T.-W.; Williams, R.A.; Lescher, J.D.; Jikaria, N.; Turtzo, L.C.; Frank, J.A. Radiological-pathological correlation of diffusion tensor and magnetization transfer imaging in a closed head traumatic brain injury model. Ann. Neurol. 2016, 79, 907–920. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, X.-Y.; Feng, D.-F.; Gu, L. Quantitative evaluation of microscopic injury with diffusion tensor imaging in a rat model of diffuse axonal injury. Eur. J. Neurosci. 2011, 33, 933–945. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.-W.; Wang, Y.; Sun, P.; Lin, T.-H.; Trinkaus, K.; Cross, A.H.; Song, S.-K. Quantifying white matter tract diffusion parameters in the presence of increased extra-fiber cellularity and vasogenic edema. Neuroimage 2014, 101, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Arfanakis, K.; Haughton, V.M.; Carew, J.D.; Rogers, B.P.; Dempsey, R.J.; Meyerand, M.E. Diffusion tensor MR imaging in diffuse axonal injury. AJNR Am. J. Neuroradiol. 2002, 23, 794–802. [Google Scholar]
- Hu, S.; Exner, C.; Sienel, R.I.; When, A.C.; Seker, F.B.; Boldoczki, F.M.; Guo, Y.; Duering, M.; Pasternak, O.; Plesnila, N.; et al. Characterization of Vasogenic and Cytotoxic Brain Edema Formation After Experimental Traumatic Brain Injury by Free Water Diffusion Magnetic Resonance Imaging. J. Neurotrauma 2024, 41, 393–406. [Google Scholar] [CrossRef]
- Li, W.; Long, J.A.; Watts, L.; Shen, Q.; Liu, Y.; Jiang, Z.; Duong, T.Q. Spatiotemporal changes in diffusion, T2 and susceptibility of white matter following mild traumatic brain injury. NMR Biomed. 2016, 29, 896–903. [Google Scholar] [CrossRef][Green Version]
- Wang, Y.; Sun, P.; Wang, Q.; Trinkaus, K.; Schmidt, R.E.; Naismith, R.T.; Cross, A.H.; Song, S.K. Differentiation and quantification of inflammation, demyelination and axon injury or loss in multiple sclerosis. Brain 2015, 138, 1223–1238. [Google Scholar] [CrossRef]
- Frank, D.; Melamed, I.; Gruenbaum, B.F.; Grinshpun, J.; Kuts, R.; Shvartsur, R.; Azab, A.N.; Assadi, M.H.; Vinokur, M.; Boyko, M. Induction of diffuse axonal brain injury in rats based on rotational acceleration. JoVE (J. Vis. Exp.) 2020, 159, 61198. [Google Scholar]
- Paxinos, G.; Watson, C. The Rat Brain in Stereotaxic Coordinates: Hard Cover Edition; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Chen, X.; Chen, Y.; Xu, Y.; Gao, Q.; Shen, Z.; Zheng, W. Microstructural and neurochemical changes in the rat brain after diffuse axonal injury. J. Magn. Reson. Imaging 2019, 49, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Mac Donald, C.L.; Dikranian, K.; Bayly, P.; Holtzman, D.; Brody, D. Diffusion tensor imaging reliably detects experimental traumatic axonal injury and indicates approximate time of injury. J. Neurosci. 2007, 27, 11869–11876. [Google Scholar] [CrossRef] [PubMed]


| NSS Values of the Study Groups | ||
|---|---|---|
| Animal Groups | N | Median (Range) |
| Sham-Operated | 16 | 0(0–0.25) |
| DAI Mild | 16 | 1(0–3) * |
| DAI Moderate | 16 | 2(1–3) ** |
| DAI Severe | 16 | 4.5(3–7.5) ** |
| MRI | ROI | Study Groups ( ± SD.; Variability; * p ≤ 0.05 and ** p ≤ 0.01) | |||
|---|---|---|---|---|---|
| Sham-Operated | Mild DAI | Moderate DAI | Severe DAI | ||
| Fractional Anisotropy | Thalamus | 0.49 ± 0.07; 15 | 0.42 ± 0.14; 34; * | 0.33 ± 0.08; 26; ** | 0.31 ± 0.05; 16; ** |
| Hypothalamus | 0.42 ± 0.06; 16 | 0.37 ± 0.09; 24 | 0.33 ± 0.04; 12; ** | 0.3 ± 0.07; 24; ** | |
| Hippocampus | 0.38 ± 0.07; 17 | 0.34 ± 0.07; 20 | 0.28 ± 0.06; 21; ** | 0.25 ± 0.07; 26; ** | |
| Corpus Callosum | 0.47 ± 0.12; 25 | 0.37 ± 0.08; 21; * | 0.31 ± 0.07; 21; ** | 0.42 ± 0.12; 28 | |
| Neocortex | 0.43 ± 0.07; 16 | 0.34 ± 0.08; 23; ** | 0.26 ± 0.04; 17; ** | 0.29 ± 0.07; 24; ** | |
| W. Brain | 0.5 ± 0.03; 7 | 0.45 ± 0.03; 7; ** | 0.39 ± 0.03; 8; ** | 0.34 ± 0.02; 7; ** | |
| variability between all ROI | 16 | 21 | 16 | 21 | |
| Relative Anisotropy | Thalamus | 0.45 ± 0.08; 17 | 0.38 ± 0.15; 39 | 0.27 ± 0.07; 26; ** | 0.27 ± 0.05; 17; ** |
| Hypothalamus | 0.38 ± 0.07; 18 | 0.33 ± 0.09; 27 | 0.28 ± 0.04; 14; ** | 0.26 ± 0.07; 25; ** | |
| Hippocampus | 0.32 ± 0.07; 22 | 0.29 ± 0.06; 23 | 0.24 ± 0.06; 27; ** | 0.21 ± 0.06; 27; ** | |
| Corpus Callosum | 0.43 ± 0.13; 29 | 0.33 ± 0.08; 23; * | 0.27 ± 0.06; 24; ** | 0.39 ± 0.15; 38 | |
| Neocortex | 0.4 ± 0.08; 19 | 0.29 ± 0.07; 25; ** | 0.22 ± 0.04; 18; ** | 0.25 ± 0.07; 26; ** | |
| W. Brain | 0.47 ± 0.04; 9 | 0.42 ± 0.04; 9; ** | 0.36 ± 0.03; 9; ** | 0.3 ± 0.02; 7; ** | |
| variability between all ROI | 19 | 24 | 20 | 24 | |
| Axial Diffusivity | Thalamus | 1.21 ± 0.21; 18 | 1.2 ± 0.34; 28 | 1.08 ± 0.1; 9 | 0.81 ± 0.3; 37; ** |
| Hypothalamus | 1.51 ± 0.31; 20 | 1.45 ± 0.47; 32 | 1.23 ± 0.23; 19 | 0.99 ± 0.26; 26; ** | |
| Hippocampus | 1.33 ± 0.26; 20 | 1.17 ± 0.17; 15 | 1.19 ± 0.18; 15 | 1.05 ± 0.21; 20; ** | |
| Corpus Callosum | 1.24 ± 0.35; 29 | 1.21 ± 0.16; 14 | 1.1 ± 0.16; 15 | 0.93 ± 0.22; 23; ** | |
| Neocortex | 1.23 ± 0.19; 15 | 1.04 ± 0.18; 17; * | 1.03 ± 0.16; 15; * | 1.02 ± 0.2; 19; * | |
| W. Brain | 1.51 ± 0.13; 9 | 1.44 ± 0.17; 12 | 1.39 ± 0.15; 11 | 1 ± 0.25; 26; ** | |
| variability between all ROI | 20 | 20 | 14 | 25 | |
| Mean Diffusivity | Thalamus | 0.83 ± 0.16; 19 | 0.87 ± 0.15; 17 | 0.8 ± 0.08; 10 | 0.61 ± 0.22; 36; ** |
| Hypothalamus | 1.06 ± 0.27; 25 | 1.05 ± 0.28; 26 | 1 ± 0.29; 28 | 0.73 ± 0.15; 21; ** | |
| Hippocampus | 0.95 ± 0.17; 17 | 0.86 ± 0.11; 12 | 0.91 ± 0.11; 12 | 0.83 ± 0.13; 16 | |
| Corpus Callosum | 0.85 ± 0.13; 16 | 0.86 ± 0.09; 11 | 0.84 ± 0.1; 13 | 0.65 ± 0.17; 26; * | |
| Neocortex | 0.84 ± 0.15; 17 | 0.77 ± 0.12; 16 | 0.81 ± 0.11; 14 | 0.78 ± 0.13; 16 | |
| W. Brain | 0.96 ± 0.09; 10 | 0.95 ± 0.11; 11 | 0.95 ± 0.09; 9 | 0.8 ± 0.12; 15; ** | |
| variability between all ROI | 17 | 16 | 15 | 22 | |
| Radial Diffusivity | Thalamus | 0.57 ± 0.12; 21 | 0.67 ± 0.15; 22 | 0.66 ± 0.1; 15 | 0.54 ± 0.14; 25 |
| Hypothalamus | 0.81 ± 0.23; 29 | 0.86 ± 0.34; 39 | 0.83 ± 0.23; 28 | 0.63 ± 0.11; 18 | |
| Hippocampus | 0.74 ± 0.13; 17 | 0.71 ± 0.09; 13 | 0.77 ± 0.09; 11 | 0.73 ± 0.1; 14 | |
| Corpus Callosum | F 0.56 ± 0.11; 20 M 0.7 ± 0.09; 14 | F 0.7 ± 0.09; 13 M 0.68 ± 0.1; 14 | F 0.75 ± 0.11; 14 ** M 0.67 ± 0.06; 9 | F 0.54 ± 0.12; 22 M 0.49 ± 0.21; 42 * | |
| Neocortex | 0.64 ± 0.12; 18 | 0.63 ± 0.11; 17 | 0.71 ± 0.1; 14 | 0.66 ± 0.11; 17 | |
| W. Brain | 0.67 ± 0.08; 12 | 0.7 ± 0.08; 11 | 0.74 ± 0.08; 11 | 0.66 ± 0.09; 14 | |
| variability between all ROI | 19 | 19 | 15 | 20 | |
| DTI | ROI | Immunohistochemistry for β-APP | |||||
|---|---|---|---|---|---|---|---|
| Thalamus | Hypothalamus | Hippocampus | Corpus Callosum | Neocortex | NSS | ||
| Axial Diffusivity | Thalamus | rs = 0.374 ** | NS | ||||
| Hypothalamus | rp = 0.302 * | rs = 0.373 ** | |||||
| Hippocampus | rs = 0.257 * | NS | |||||
| Corpus Callosum | rs = 0.293 * | rs = 0.336 ** | |||||
| Neocortex | rs = 0.262 * | NS | |||||
| Whole Brain | rs = 0.424 ** | ||||||
| Fractional Anisotropy | Thalamus | rp = 0.728 ** | rs = 0.632 ** | ||||
| Hypothalamus | rp = 0.765 ** | rs = 0.7 ** | |||||
| Hippocampus | rp = 0.696 ** | rs = 0.719 ** | |||||
| Corpus Callosum | rs = 0.461 ** | rs = 0.445 ** | |||||
| Neocortex | rs = 0.822 ** | rs = 0.646 ** | |||||
| Whole Brain | rs = 0.727 ** | ||||||
| Radial Diffusivity | Thalamus | rp = 0.728 ** | NS | ||||
| Hypothalamus | NS | rs = 0.259 * | |||||
| Hippocampus | NS | NS | |||||
| Corpus Callosum | NS | NS | |||||
| Neocortex | NS | NS | |||||
| Whole Brain | NS | ||||||
| Relative Anisotropy | Thalamus | rs = 0.843 ** | rs = 0.655 ** | ||||
| Hypothalamus | rp = 0.786 ** | rs = 0.718 ** | |||||
| Hippocampus | rp = 0.686 ** | rs = 0.785 ** | |||||
| Corpus Callosum | rs = 0.585 ** | rs = 0.529 ** | |||||
| Neocortex | rs = 0.839 ** | rs = 0.69 ** | |||||
| Whole Brain | rs = 0.769 ** | ||||||
| Mean Diffusivity | Thalamus | rs = 0.28 * | rs = 0.264 * | ||||
| Hypothalamus | rs = 0.291 * | rs = 0.336 ** | |||||
| Hippocampus | NS | NS | |||||
| Corpus Callosum | NS | NS | |||||
| Neocortex | NS | NS | |||||
| Whole Brain | rs = 0.251 * | ||||||
| NSS | rs = 0.745 ** | rs = 0.795 ** | rs = 0.714 ** | rs = 0.816 ** | rs = 0.772 ** | ||
| Study Groups | ROI | β-APP | NSS | MRI | ||||
|---|---|---|---|---|---|---|---|---|
| FA | RA | AD | MD | RD | ||||
| DAI mild | Thalamus | n = 2 | n = 15 | n = 40 | n = 47 | n = 12,520 | n = 236 | n = 29 |
| Hypothalamus | n = 2 | n = 41 | n = 41 | n = 691 | n = 11,862 | n = 529 | ||
| Neocortex | n = 2 | n = 11 | n = 8 | n = 15 | n = 60 | n = 2078 | ||
| Hippocampus | n = 2 | n = 49 | n = 35 | n = 30 | n = 40 | n = 218 | ||
| Corpus Callosum | n = 2 | n = 16 | n = 19 | n = 1289 | n = 1960 | n = 49 | ||
| W. Brain | n = 6 | n = 11 | n = 74 | n = 1584 | n = 112 | |||
| DAI moderate | Thalamus | n = 2 | n = 6 | n = 4 | n = 3 | n = 26 | n = 279 | n = 24 |
| Hypothalamus | n = 2 | n = 7 | n = 6 | n = 1092 | n = 342 | n = 2074 | ||
| Neocortex | n = 3 | n = 2 | n = 2 | n = 13 | n = 302 | n = 40 | ||
| Hippocampus | n = 3 | n = 7 | n = 5 | n = 40 | n = 201 | n = 218 | ||
| Corpus Callosum | n = 2 | n = 6 | n = 7 | n = 60 | n = 2274 | n = 28 | ||
| W. Brain | n = 2 | n = 2 | n = 2 | n = 22 | n = 1271 | n = 21 | ||
| DAI severe | Thalamus | n = 2 | n = 5 | n = 2 | n = 3 | n = 7 | n = 12 | n = 297 |
| Hypothalamus | n = 2 | n = 6 | n = 6 | n = 19 | n = 2 | n = 16 | ||
| Neocortex | n = 3 | n = 5 | n = 4 | n = 14 | n = 86 | n = 520 | ||
| Hippocampus | n = 3 | n = 5 | n = 3 | n = 12 | n = 25 | n = 2109 | ||
| Corpus Callosum | n = 2 | n = 91 | n = 194 | n = 14 | n = 9 | n = 29 | ||
| W. Brain | n = 2 | n = 2 | n = 3 | n = 7 | n = 1137 | |||
| Assessment Modality | Sensitivity (Mild) | Sensitivity (Moderate) | Sensitivity (Severe) | Typical Group Size Needed | Key Features |
|---|---|---|---|---|---|
| Histology | High | High | High | 2–3 | Well-established method for detecting axonal pathology (β-APP); labor-intensive; invasive |
| DTI (FA/RA) | Moderate | High | High | 2–49+ (varies by ROI) | Strong correlations with histology and NSS; sensitive to microstructural changes |
| DTI (RD/MD) | Low | Low–Moderate | Moderate | 7–12,000 (variable) | Less robust correlations; requires large N to detect subtle changes |
| NSS | Moderate | High | High | 2–15 | Non-invasive; correlates well with both DTI (FA/RA) and histology; functional readout |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zvenigorodsky, V.; Gruenbaum, B.F.; Shelef, I.; Frank, D.; Tsafarov, B.; Negev, S.; Zeldetz, V.; Azab, A.N.; Boyko, M.; Zlotnik, A. Sensitivity of Diffusion Tensor Imaging for Assessing Injury Severity in a Rat Model of Isolated Diffuse Axonal Injury: Comparison with Histology and Neurological Assessment. Int. J. Mol. Sci. 2025, 26, 7333. https://doi.org/10.3390/ijms26157333
Zvenigorodsky V, Gruenbaum BF, Shelef I, Frank D, Tsafarov B, Negev S, Zeldetz V, Azab AN, Boyko M, Zlotnik A. Sensitivity of Diffusion Tensor Imaging for Assessing Injury Severity in a Rat Model of Isolated Diffuse Axonal Injury: Comparison with Histology and Neurological Assessment. International Journal of Molecular Sciences. 2025; 26(15):7333. https://doi.org/10.3390/ijms26157333
Chicago/Turabian StyleZvenigorodsky, Vladislav, Benjamin F. Gruenbaum, Ilan Shelef, Dmitry Frank, Beatris Tsafarov, Shahar Negev, Vladimir Zeldetz, Abed N. Azab, Matthew Boyko, and Alexander Zlotnik. 2025. "Sensitivity of Diffusion Tensor Imaging for Assessing Injury Severity in a Rat Model of Isolated Diffuse Axonal Injury: Comparison with Histology and Neurological Assessment" International Journal of Molecular Sciences 26, no. 15: 7333. https://doi.org/10.3390/ijms26157333
APA StyleZvenigorodsky, V., Gruenbaum, B. F., Shelef, I., Frank, D., Tsafarov, B., Negev, S., Zeldetz, V., Azab, A. N., Boyko, M., & Zlotnik, A. (2025). Sensitivity of Diffusion Tensor Imaging for Assessing Injury Severity in a Rat Model of Isolated Diffuse Axonal Injury: Comparison with Histology and Neurological Assessment. International Journal of Molecular Sciences, 26(15), 7333. https://doi.org/10.3390/ijms26157333







