Functional MPO Polymorphisms and Haplotypes Affect Both Myeloperoxidase Levels and Association with Hypertensive Disorders of Pregnancy
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Subjects
4.2. Myeloperoxidase Concentration
4.3. Genotyping
4.4. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Umesawa, M.; Kobashi, G. Epidemiology of hypertensive disorders in pregnancy: Prevalence, risk factors, predictors and prognosis. Hypertens. Res. 2017, 40, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.A.; Brown, M.A.; Hall, D.R.; Gupte, S.; Hennessy, A.; Karumanchi, S.A.; Kenny, L.C.; McCarthy, F.; Myers, J.; Poon, L.C.; et al. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2022, 27, 148–169. [Google Scholar] [CrossRef] [PubMed]
- Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obs. Gynecol. 2020, 135, e237–e260. [CrossRef] [PubMed]
- Magee, L.A.; Pels, A.; Helewa, M.; Rey, E.; von Dadelszen, P.; Canadian Hypertensive Disorders of Pregnancy Working Group. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. Pregnancy Hypertens. 2014, 4, 105–145. [Google Scholar] [CrossRef] [PubMed]
- Townsend, R.; O’Brien, P.; Khalil, A. Current best practice in the management of hypertensive disorders in pregnancy. Integr. Blood Press. Control 2016, 9, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Nauseef, W.M. Myeloperoxidase in human neutrophil host defence. Cell Microbiol. 2014, 16, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Hawkins, C.L.; Pattison, D.I.; Rees, M.D. Mammalian heme peroxidases: From molecular mechanisms to health implications. Antioxid. Redox Signal 2008, 10, 1199–1234. [Google Scholar] [CrossRef] [PubMed]
- van der Veen, B.S.; de Winther, M.P.; Heeringa, P. Myeloperoxidase: Molecular mechanisms of action and their relevance to human health and disease. Antioxid. Redox Signal 2009, 11, 2899–2937. [Google Scholar] [CrossRef] [PubMed]
- Rocha-Penha, L.; Caldeira-Dias, M.; Tanus-Santos, J.E.; de Carvalho Cavalli, R.; Sandrim, V.C. Myeloperoxidase in Hypertensive Disorders of Pregnancy and Its Relation With Nitric Oxide. Hypertension 2017, 69, 1173–1180. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, C.; Klinke, A.; Adam, M.; Baldus, S.; Sperandio, M. Myeloperoxidase: A leukocyte-derived protagonist of inflammation and cardiovascular disease. Antioxid. Redox Signal 2013, 18, 692–713. [Google Scholar] [CrossRef] [PubMed]
- Mihalic, Z.N.; Kloimbock, T.; Cosic-Mujkanovic, N.; Valadez-Cosmes, P.; Maitz, K.; Kindler, O.; Wadsack, C.; Heinemann, A.; Marsche, G.; Gauster, M.; et al. Myeloperoxidase enhances the migration and invasion of human choriocarcinoma JEG-3 cells. Redox Biol. 2023, 67, 102885. [Google Scholar] [CrossRef] [PubMed]
- Anatoliotakis, N.; Deftereos, S.; Bouras, G.; Giannopoulos, G.; Tsounis, D.; Angelidis, C.; Kaoukis, A.; Stefanadis, C. Myeloperoxidase: Expressing inflammation and oxidative stress in cardiovascular disease. Curr. Top. Med. Chem. 2013, 13, 115–138. [Google Scholar] [CrossRef] [PubMed]
- Sandrim, V.C.; Palei, A.C.; Metzger, I.F.; Gomes, V.A.; Cavalli, R.C.; Tanus-Santos, J.E. Nitric oxide formation is inversely related to serum levels of antiangiogenic factors soluble fms-like tyrosine kinase-1 and soluble endogline in preeclampsia. Hypertension 2008, 52, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Osol, G.; Ko, N.L.; Mandala, M. Altered Endothelial Nitric Oxide Signaling as a Paradigm for Maternal Vascular Maladaptation in Preeclampsia. Curr. Hypertens. Rep. 2017, 19, 82. [Google Scholar] [CrossRef] [PubMed]
- Melchiorre, K.; Giorgione, V.; Thilaganathan, B. The placenta and preeclampsia: Villain or victim? Am. J. Obs. Gynecol. 2022, 226, S954–S962. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.M. Preeclampsia epidemiology(ies) and pathophysiology(ies). Best. Pract. Res. Clin. Obs. Gynaecol. 2024, 94, 102480. [Google Scholar] [CrossRef] [PubMed]
- Ndrepepa, G. Myeloperoxidase—A bridge linking inflammation and oxidative stress with cardiovascular disease. Clin. Chim. Acta 2019, 493, 36–51. [Google Scholar] [CrossRef] [PubMed]
- Hung, T.H.; Chen, S.F.; Lo, L.M.; Li, M.J.; Yeh, Y.L.; Hsieh, T.T. Myeloperoxidase in the plasma and placenta of normal pregnant women and women with pregnancies complicated by preeclampsia and intrauterine growth restriction. Placenta 2012, 33, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Bowen, R.S.; Moodley, J.; Dutton, M.F.; Fickl, H. Systemic inflammatory indices in pre-eclampsia and eclampsia. J. Obs. Gynaecol. 2001, 21, 563–569. [Google Scholar] [CrossRef]
- Karacay, O.; Sepici-Dincel, A.; Karcaaltincaba, D.; Sahin, D.; Yalvac, S.; Akyol, M.; Kandemir, O.; Altan, N. A quantitative evaluation of total antioxidant status and oxidative stress markers in preeclampsia and gestational diabetic patients in 24-36 weeks of gestation. Diabetes Res. Clin. Pract. 2010, 89, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Noyan, T.; Guler, A.; Sekeroglu, M.R.; Kamaci, M. Serum advanced oxidation protein products, myeloperoxidase and ascorbic acid in pre-eclampsia and eclampsia. Aust. N. Z. J. Obs. Gynaecol. 2006, 46, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Gandley, R.E.; Rohland, J.; Zhou, Y.; Shibata, E.; Harger, G.F.; Rajakumar, A.; Kagan, V.E.; Markovic, N.; Hubel, C.A. Increased myeloperoxidase in the placenta and circulation of women with preeclampsia. Hypertension 2008, 52, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Kurdoglu, Z.; Ozkol, H.; Kurdoglu, M.; Kamaci, M. Evaluation of the relationship between adenosine deaminase, myeloperoxidase, cholinesterase, preeclampsia severity, and neonatal outcomes. Clin. Exp. Hypertens. 2012, 34, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Mellembakken, J.R.; Hogasen, K.; Mollnes, T.E.; Hack, C.E.; Abyholm, T.; Videm, V. Increased systemic activation of neutrophils but not complement in preeclampsia. Obs. Gynecol. 2001, 97, 371–374. [Google Scholar] [CrossRef]
- Schaid, D.J.; Chen, W.; Larson, N.B. From genome-wide associations to candidate causal variants by statistical fine-mapping. Nat. Rev. Genet. 2018, 19, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; He, D.; Zhou, W.; Guo, Z.; Ma, Y.; Liu, L.; He, H.; He, S.; Huang, Y. Polymorphisms in myeloperoxidase and tissue inhibitor of metalloproteinase-1 genes and their association with preeclampsia in the Chinese Han population. Heliyon 2024, 10, e36685. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, E.; Balat, O.; Pehlivan, S.; Ugur, M.G.; Sever, T. Genetic variation of myeloperoxidase gene contributes to preeclampsia: A preliminary association study in Turkish population. Hypertens. Pregnancy 2011, 30, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Boyle, A.P.; Hong, E.L.; Hariharan, M.; Cheng, Y.; Schaub, M.A.; Kasowski, M.; Karczewski, K.J.; Park, J.; Hitz, B.C.; Weng, S.; et al. Annotation of functional variation in personal genomes using RegulomeDB. Genome Res. 2012, 22, 1790–1797. [Google Scholar] [CrossRef] [PubMed]
- Consortium, E.P. An integrated encyclopedia of DNA elements in the human genome. Nature 2012, 489, 57–74. [Google Scholar] [CrossRef] [PubMed]
- Rocha-Penha, L.; Bettiol, H.; Barbieri, M.A.; Cardoso, V.C.; Cavalli, R.C.; Sandrim, V.C. Myeloperoxidase is not a good biomarker for preeclampsia prediction. Sci. Rep. 2017, 7, 10257. [Google Scholar] [CrossRef] [PubMed]
- Korner, A.; Garten, A.; Bluher, M.; Tauscher, R.; Kratzsch, J.; Kiess, W. Molecular characteristics of serum visfatin and differential detection by immunoassays. J. Clin. Endocrinol. Metab. 2007, 92, 4783–4791. [Google Scholar] [CrossRef] [PubMed]
- Weng, K.P.; Hsieh, K.S.; Huang, S.H.; Wu, H.W.; Chien, J.H.; Lin, C.C.; Tang, C.W.; Ou, S.F.; Huang, S.J.; Ger, L.P. Myeloperoxidase genetic polymorphisms and susceptibility to Kawasaki disease in Taiwanese children. J. Microbiol. Immunol. Infect. 2016, 49, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Saygili, E.I.; Aksoy, N.; Pehlivan, M.; Sever, T.; Yilmaz, M.; Cimenci, I.G.; Pehlivan, S. Enzyme levels and G-463A polymorphism of myeloperoxidase in chronic lymphocytic leukemia and multiple myeloma. Leuk. Lymphoma 2009, 50, 2030–2037. [Google Scholar] [CrossRef] [PubMed]
- Ramachandra, C.J.A.; Ja, K.; Chua, J.; Cong, S.; Shim, W.; Hausenloy, D.J. Myeloperoxidase As a Multifaceted Target for Cardiovascular Protection. Antioxid. Redox Signal 2020, 32, 1135–1149. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tan, G.J.; Han, L.N.; Bai, Y.Y.; He, M.; Liu, H.B. Novel biomarkers for cardiovascular risk prediction. J. Geriatr. Cardiol. 2017, 14, 135–150. [Google Scholar] [CrossRef] [PubMed]
- Mori, T.; Watanabe, K.; Iwasaki, A.; Kimura, C.; Matsushita, H.; Shinohara, K.; Wakatsuki, A. Differences in vascular reactivity between pregnant women with chronic hypertension and preeclampsia. Hypertens. Res. 2014, 37, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, A.M.; Pereira, N.R.; Costa, C.A.; Mann, G.E.; Cordeiro, V.S.; de Moura, R.S.; Brunini, T.M.; Mendes-Ribeiro, A.C.; Resende, A.C. L-arginine-nitric oxide pathway and oxidative stress in plasma and platelets of patients with pre-eclampsia. Hypertens. Res. 2013, 36, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin Summary, Number 222. Obs. Gynecol. 2020, 135, 1492–1495. [CrossRef] [PubMed]
- Lacchini, R.; Jacob-Ferreira, A.L.; Luizon, M.R.; Gasparini, S.; Ferreira-Sae, M.C.; Schreiber, R.; Nadruz, W., Jr.; Tanus-Santos, J.E. Common matrix metalloproteinase 2 gene haplotypes may modulate left ventricular remodelling in hypertensive patients. J. Hum. Hypertens. 2012, 26, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Schaid, D.J.; Rowland, C.M.; Tines, D.E.; Jacobson, R.M.; Poland, G.A. Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am. J. Hum. Genet. 2002, 70, 425–434. [Google Scholar] [CrossRef] [PubMed]
| Parameters | HP (n = 136) | GH (n = 118) | PE (n = 140) |
|---|---|---|---|
| Age (years) | 23.0 (20.0–28.0) | 27.5 (22.7–32.0) * | 26.0 (21.3–32.0) * |
| Race (white, %) | 61.9 | 71.8 | 71.3 |
| BMI (Kg/m2) before pregnancy | 22.7 (20.1–26.3) | 29.0 (25.2–33.7) * | 27.4 (23.3–32.3) *,# |
| Current smoker (%) | 11.5 | 5.2 | 11.9 |
| SBP (mmHg) | 110.0 (100.0–120.0) | 130.0 (120.0–140.0) * | 130.0 (122.0–140.0) * |
| DBP (mmHg) | 70.0 (70.0–80.0) | 80.0 (70.0–90.0) * | 90.0 (80.0–94.0) *,# |
| Antihypertensive drugs at blood collection | |||
| α-Methyldopa(%) | NA | 73.5 | 74.0 |
| Nifedipine(%) | NA | 0.9 | 6.3 # |
| Hydralazine (%) | 1.7 | 0 | |
| GA at blood collection (weeks) | 37.0 (36.0–39.0) | 37.0 (34.0–39.0) | 35.0 (32.0–37.0) *,# |
| RBC count (×106/mL) | 4.0 (3.7–4.4) | 4.1 (3.8–4.4) | 4.2 (3.9–4.4) |
| Hemoglobin (g/dL) | 11.9 (10.9–12.7 | 12.0 (11.2–12.9) | 12.0 (11.1–12.7) |
| WBC count (×103/mL) | 11.9 (8.1–13.1) | 9.7 (8.1–11.4) | 10.0 (8.4–12.0) |
| Neutrophils (%) | 72.5 (69.1–83.7) | 69.4 (63.8–74.0) * | 70.1 (66.0–74.0) * |
| Proteinuria (mg/24 h) | ND | 151.6 (109.9–205.4) | 409.8 (303.2–920.4) # |
| Plasma nitrite (nM) | 115.8 (72.5–166.5) | 73.7 (41.9–127.6) * | 80.8 (52.1–124.4) * |
| Whole blood nitrite (nM) | 72.6 (49.5–168.6) | 74.9 (31.9–101.2) | 49.1 (24.5–83.2) * |
| GA at delivery (weeks) | 40.0 (39.0–41.0) | 39.0 (38.0–40.0) * | 37.0 (35.0–39.0) *,# |
| Newborn weight (g) | 3255.0 (3025.0–3650.0) | 3225.0 (2900.0–3525.0) | 2825.0 (2040.0–3288.0) *,# |
| Polymorphism | HP (%) | GH (%) | OR (95% CI) | p Value | PE (%) | OR (95% CI) | p Value |
|---|---|---|---|---|---|---|---|
| T–765C (rs2243828) | |||||||
| TT | 0.590 | 0.544 | 1.000 (Reference) | – | 0.656 | 1.000 (Reference) | – |
| TC | 0.385 | 0.351 | 0.989 (0.572–1.709) | 0.969 | 0.290 | 0.677 (0.396–1.158) | 0.153 |
| CC | 0.026 | 0.105 | 4.452 (1.200–16.52) | 0.016 * | 0.053 | 2.597 (0.643–10.48) | 0.167 |
| A allele | 0.782 | 0.719 | 1.000 (Reference) | – | 0.802 | 1.000 (Reference) | – |
| G allele | 0.218 | 0.281 | 1.400 (0.916–2.140) | 0.119 | 0.198 | 0.888 (0.575–1.372) | 0.593 |
| 9890A>C (rs2071409) | |||||||
| AA | 0.812 | 0.886 | 1.000 (Reference) | – | 0.870 | 1.000 (Reference) | – |
| AC+CC | 0.188 | 0.114 | 0.556 (0.265–1.166) | 0.116 | 0.130 | 0.644 (0.323–1.283) | 0.208 |
| T allele | 0.902 | 0.925 | 1.000 (Reference) | – | 0.935 | 1.000 (Reference) | – |
| G allele | 0.098 | 0.075 | 0.739 (0.383–1.424) | 0.364 | 0.065 | 0.636 (0.331–1.224) | 0.172 |
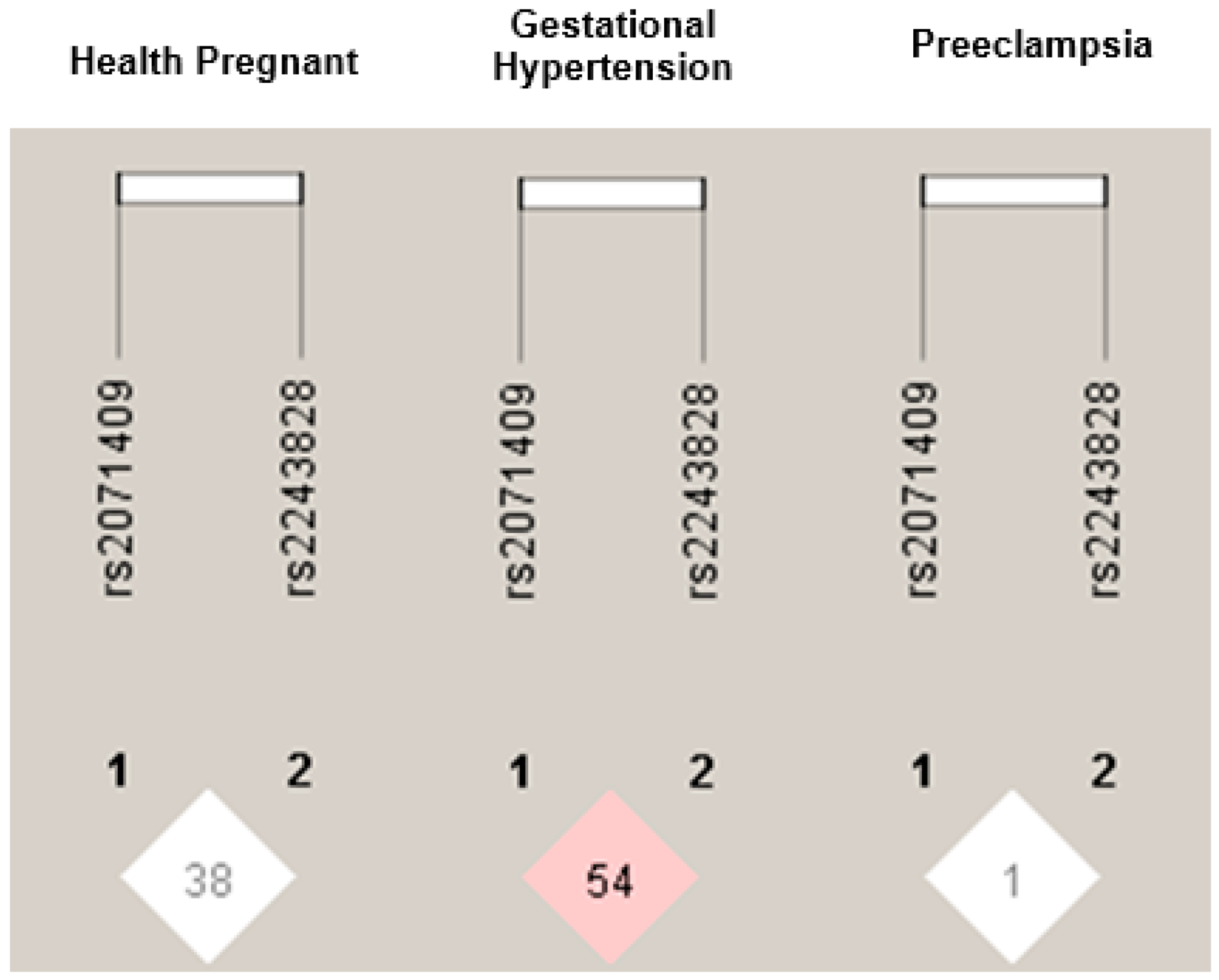
| Haplotype | HP (n = 117 × 2) | GH (n = 118 × 2) | p | OR (95% CI) | PE (n = 131 × 2) | p | OR (95% CI) |
|---|---|---|---|---|---|---|---|
| T, A | 0.734 | 0.696 | 0.404 | 1.000 (Reference) | 0.750 | 0.531 | 1.000 (Reference) |
| T, C | 0.047 | 0.023 | 0.178 | 0.578 (0.202–1.648) | 0.051 | 0.811 | 1.027 (0.427–2.469) |
| C, A | 0.167 | 0.231 | 0.068 | 1.484 (0.910–2.421) | 0.184 | 0.771 | 1.113 (0.675–1.838) |
| C, C | 0.050 | 0.048 | 0.805 | 0.985 (0.450–2.159) | 0.013 | 0.025 * | 0.246 (0.062–0.971) |
| Polymorphism | Genotype | HP | GH | PE | |
|---|---|---|---|---|---|
| Concentration | Concentration | Concentration | |||
| rs2243828 | TT | 15.0 ± 1.7 | 6.1 ± 0.5 | 14.0 ± 1.4 | |
| TC+CC | 17.3 ± 2.7 | 37.4 ± 3.5 # | 16.8 ± 2.4 | ||
| rs2071409 | AA | 22.6 ± 2.5 | 19.2 ± 1.9 | 13.7 ± 1.2 | |
| AC+CC | 23.3 ± 4.8 | 8.1 ± 2.3 * | 17.8 ± 3.9 | ||
| Haplotype | HP | GH | PE |
|---|---|---|---|
| Concentration | Concentration | Concentration | |
| T,A | 5.0 ± 0.36 | 3.3 ± 0.2 | 4.0 ± 0.2 |
| T,C | 3.5 ± 0.5 | 5.4 ± 1.5 | 2.7 ± 0.4 |
| C,A | 3.2 ± 0.3 | 3.6 ± 0.4 | 3.4 ± 0.3 |
| C,C | 2.4 ± 0.3 | 1.9 ± 0.1 | 2.0 ± 0.2 # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alves Pereira, D.; Rizzatti Luizon, M.; Carvalho Cavalli, R.; Tanus-Santos, J.E.; Cristina Sandrim, V. Functional MPO Polymorphisms and Haplotypes Affect Both Myeloperoxidase Levels and Association with Hypertensive Disorders of Pregnancy. Int. J. Mol. Sci. 2025, 26, 7071. https://doi.org/10.3390/ijms26157071
Alves Pereira D, Rizzatti Luizon M, Carvalho Cavalli R, Tanus-Santos JE, Cristina Sandrim V. Functional MPO Polymorphisms and Haplotypes Affect Both Myeloperoxidase Levels and Association with Hypertensive Disorders of Pregnancy. International Journal of Molecular Sciences. 2025; 26(15):7071. https://doi.org/10.3390/ijms26157071
Chicago/Turabian StyleAlves Pereira, Daniela, Marcelo Rizzatti Luizon, Ricardo Carvalho Cavalli, Jose Eduardo Tanus-Santos, and Valéria Cristina Sandrim. 2025. "Functional MPO Polymorphisms and Haplotypes Affect Both Myeloperoxidase Levels and Association with Hypertensive Disorders of Pregnancy" International Journal of Molecular Sciences 26, no. 15: 7071. https://doi.org/10.3390/ijms26157071
APA StyleAlves Pereira, D., Rizzatti Luizon, M., Carvalho Cavalli, R., Tanus-Santos, J. E., & Cristina Sandrim, V. (2025). Functional MPO Polymorphisms and Haplotypes Affect Both Myeloperoxidase Levels and Association with Hypertensive Disorders of Pregnancy. International Journal of Molecular Sciences, 26(15), 7071. https://doi.org/10.3390/ijms26157071







