Identification of Molecular Subtypes of B-Cell Acute Lymphoblastic Leukemia in Mexican Children by Whole-Transcriptome Analysis
Abstract
1. Introduction
2. Results
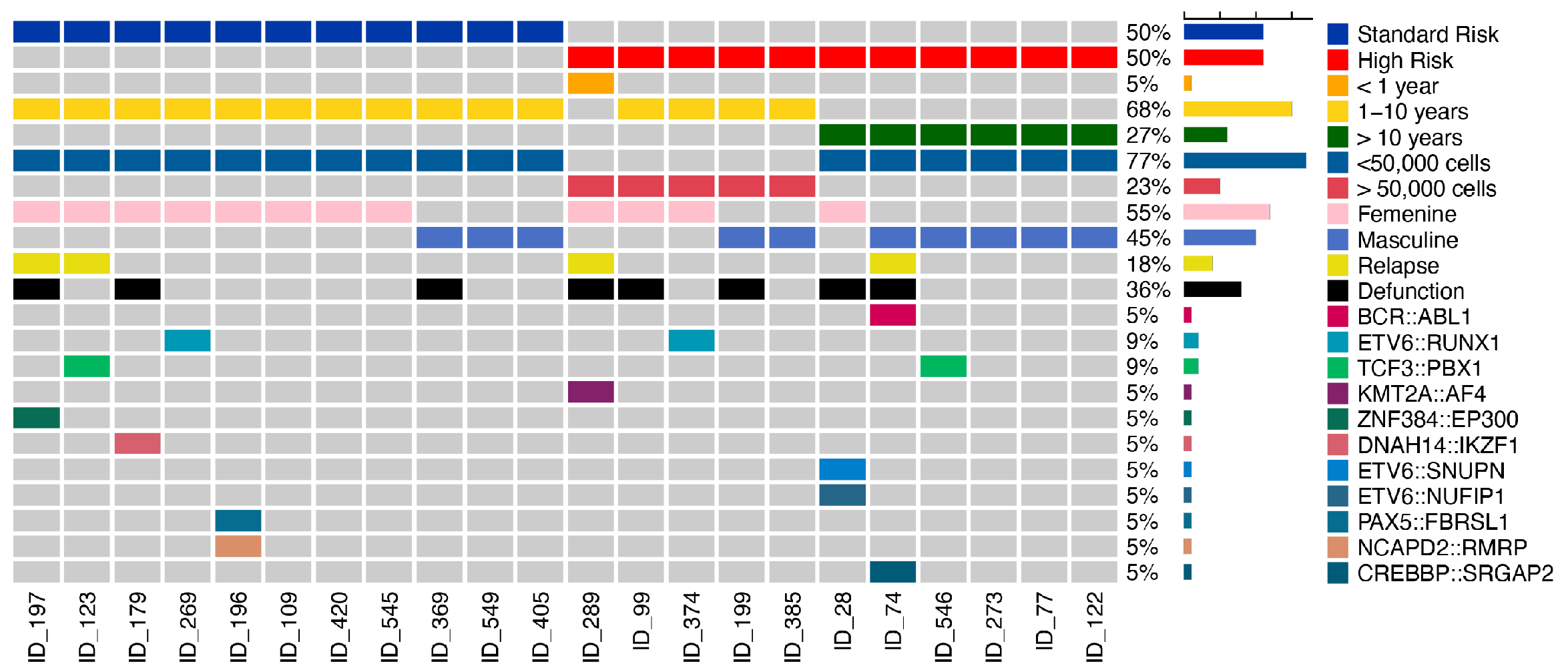
2.1. Clinical Characteristics of MIGICCL Cohort
2.2. Bioinformatic Determination of Genetic Fusions
2.3. Classification of B-ALL Molecular Subtypes by Machine Learning Classifiers
2.4. Distributions of Different Molecular Subtypes of B-ALL
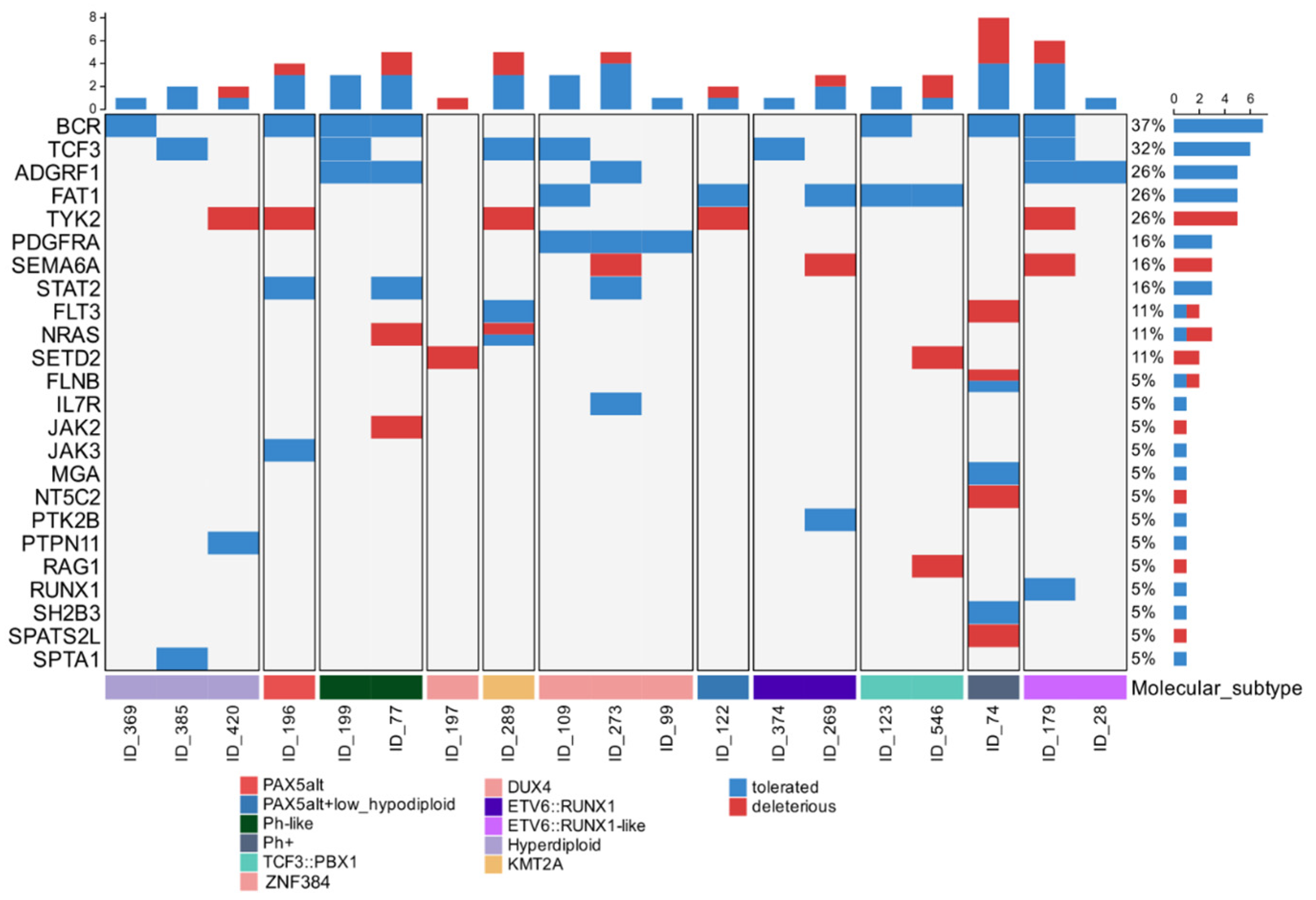
2.5. Gene Variants Associated with Molecular Subtypes
2.6. Overexpression of CRFL2 Gene in Ph-like Subtype
3. Discussion
4. Materials and Methods
4.1. MIGICCL Cohort
4.2. Bulk RNA-Seq
4.3. Bioinformatic Analysis
4.4. Validation of CRFL2 Expression by qRT-PCR
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Inaba, H.; Greaves, M.; Mullighan, C.G. Acute lymphoblastic leukaemia. Lancet 2013, 381, 1943–1955. [Google Scholar] [CrossRef] [PubMed]
- Flores-Lujano, J.; Duarte-Rodriguez, D.A.; Jimenez-Hernandez, E.; Martin-Trejo, J.A.; Allende-Lopez, A.; Penaloza-Gonzalez, J.G.; Perez-Saldivar, M.L.; Medina-Sanson, A.; Torres-Nava, J.R.; Solis-Labastida, K.A.; et al. Persistently high incidence rates of childhood acute leukemias from 2010 to 2017 in Mexico City: A population study from the MIGICCL. Front. Public Health 2022, 10, 918921. [Google Scholar] [CrossRef] [PubMed]
- Perez-Saldivar, M.L.; Fajardo-Gutierrez, A.; Bernaldez-Rios, R.; Martinez-Avalos, A.; Medina-Sanson, A.; Espinosa-Hernandez, L.; Flores-Chapa Jde, D.; Amador-Sanchez, R.; Penaloza-Gonzalez, J.G.; Alvarez-Rodriguez, F.J.; et al. Childhood acute leukemias are frequent in Mexico City: Descriptive epidemiology. BMC Cancer 2011, 11, 355. [Google Scholar] [CrossRef] [PubMed]
- Mullighan, C.G. The genomic landscape of acute lymphoblastic leukemia in children and young adults. Hematol. Am. Soc. Hematol. Educ. Program 2014, 2014, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.; Sheikh, T.; Aggarwal, N. Emerging molecular subtypes and therapies in acute lymphoblastic leukemia. Semin. Diagn. Pathol. 2023, 40, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Ryan, S.L.; Peden, J.F.; Kingsbury, Z.; Schwab, C.J.; James, T.; Polonen, P.; Mijuskovic, M.; Becq, J.; Yim, R.; Cranston, R.E.; et al. Whole genome sequencing provides comprehensive genetic testing in childhood B-cell acute lymphoblastic leukaemia. Leukemia 2023, 37, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Arber, D.A.; Orazi, A.; Hasserjian, R.P.; Borowitz, M.J.; Calvo, K.R.; Kvasnicka, H.M.; Wang, S.A.; Bagg, A.; Barbui, T.; Branford, S.; et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: Integrating morphologic, clinical, and genomic data. Blood 2022, 140, 1200–1228. [Google Scholar] [CrossRef] [PubMed]
- Alaggio, R.; Amador, C.; Anagnostopoulos, I.; Attygalle, A.D.; Araujo, I.B.O.; Berti, E.; Bhagat, G.; Borges, A.M.; Boyer, D.; Calaminici, M.; et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 2022, 36, 1720–1748. [Google Scholar] [CrossRef] [PubMed]
- Heatley, S.L.; Sadras, T.; Kok, C.H.; Nievergall, E.; Quek, K.; Dang, P.; McClure, B.; Venn, N.; Moore, S.; Suttle, J.; et al. High prevalence of relapse in children with Philadelphia-like acute lymphoblastic leukemia despite risk-adapted treatment. Haematologica 2017, 102, e490–e493. [Google Scholar] [CrossRef] [PubMed]
- Gorecki, M.; Koziol, I.; Kopystecka, A.; Budzynska, J.; Zawitkowska, J.; Lejman, M. Updates in KMT2A Gene Rearrangement in Pediatric Acute Lymphoblastic Leukemia. Biomedicines 2023, 11, 821. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Bai, W.; Cheng, Q.; Fang, J. ZNF384-Related Fusion Genes in Acute Lymphoblastic Leukemia. Cancer Control 2023, 30, 10732748231182787. [Google Scholar] [CrossRef] [PubMed]
- Qiu, K.Y.; Xu, H.G.; Luo, X.Q.; Mai, H.R.; Liao, N.; Yang, L.H.; Zheng, M.C.; Wan, W.Q.; Wu, X.D.; Liu, R.Y.; et al. Prognostic Value and Outcome for ETV6/RUNX1-Positive Pediatric Acute Lymphoblastic Leukemia: A Report from the South China Children’s Leukemia Group. Front. Oncol. 2021, 11, 797194. [Google Scholar] [CrossRef] [PubMed]
- Zaliova, M.; Kotrova, M.; Bresolin, S.; Stuchly, J.; Stary, J.; Hrusak, O.; Te Kronnie, G.; Trka, J.; Zuna, J.; Vaskova, M. ETV6/RUNX1-like acute lymphoblastic leukemia: A novel B-cell precursor leukemia subtype associated with the CD27/CD44 immunophenotype. Genes. Chromosomes Cancer 2017, 56, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Lilljebjorn, H.; Henningsson, R.; Hyrenius-Wittsten, A.; Olsson, L.; Orsmark-Pietras, C.; von Palffy, S.; Askmyr, M.; Rissler, M.; Schrappe, M.; Cario, G.; et al. Identification of ETV6-RUNX1-like and DUX4-rearranged subtypes in paediatric B-cell precursor acute lymphoblastic leukaemia. Nat. Commun. 2016, 7, 11790. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.R.; Antillon-Klussmann, F.; Pei, D.; Yang, W.; Roberts, K.G.; Li, Z.; Devidas, M.; Yang, W.; Najera, C.; Lin, H.P.; et al. Association of Genetic Ancestry with the Molecular Subtypes and Prognosis of Childhood Acute Lymphoblastic Leukemia. JAMA Oncol. 2022, 8, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Bastian, L.; Schroeder, M.P.; Eckert, C.; Schlee, C.; Tanchez, J.O.; Kampf, S.; Wagner, D.L.; Schulze, V.; Isaakidis, K.; Lazaro-Navarro, J.; et al. PAX5 biallelic genomic alterations define a novel subgroup of B-cell precursor acute lymphoblastic leukemia. Leukemia 2019, 33, 1895–1909. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Lee, S.H.R.; Chin, W.H.N.; Lu, Y.; Jiang, N.; Lim, E.H.; Coustan-Smith, E.; Chiew, K.H.; Oh, B.L.Z.; Koh, G.S.; et al. Distinct clinical characteristics of DUX4- and PAX5-altered childhood B-lymphoblastic leukemia. Blood Adv. 2021, 5, 5226–5238. [Google Scholar] [CrossRef] [PubMed]
- Almeida, A.R.M.; Neto, J.L.; Cachucho, A.; Euzebio, M.; Meng, X.; Kim, R.; Fernandes, M.B.; Raposo, B.; Oliveira, M.L.; Ribeiro, D.; et al. Interleukin-7 receptor alpha mutational activation can initiate precursor B-cell acute lymphoblastic leukemia. Nat. Commun. 2021, 12, 7268. [Google Scholar] [CrossRef] [PubMed]
- Bastian, L.; Hartmann, A.M.; Beder, T.; Hanzelmann, S.; Kassens, J.; Bultmann, M.; Hoeppner, M.P.; Franzenburg, S.; Wittig, M.; Franke, A.; et al. UBTF::ATXN7L3 gene fusion defines novel B cell precursor ALL subtype with CDX2 expression and need for intensified treatment. Leukemia 2022, 36, 1676–1680. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Habeebu, S.S.M.; Li, W. Prognostic and Predictive Biomarkers in Precursor B-cell Acute Lymphoblastic Leukemia. In Leukemia; Li, W., Ed.; Exon Publications: Brisbane, Australia, 2022. [Google Scholar]
- Chouvarine, P.; Antic, Z.; Lentes, J.; Schroder, C.; Alten, J.; Bruggemann, M.; Carrillo-de Santa Pau, E.; Illig, T.; Laguna, T.; Schewe, D.; et al. Transcriptional and Mutational Profiling of B-Other Acute Lymphoblastic Leukemia for Improved Diagnostics. Cancers 2021, 13, 5653. [Google Scholar] [CrossRef] [PubMed]
- Walter, W.; Shahswar, R.; Stengel, A.; Meggendorfer, M.; Kern, W.; Haferlach, T.; Haferlach, C. Clinical application of whole transcriptome sequencing for the classification of patients with acute lymphoblastic leukemia. BMC Cancer 2021, 21, 886. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.M.; Lonsdale, A.; Zhu, A.; Davidson, N.M.; Schmidt, B.; Hawkins, A.; Wallach, E.; Martin, M.; Mechinaud, F.M.; Khaw, S.L.; et al. The application of RNA sequencing for the diagnosis and genomic classification of pediatric acute lymphoblastic leukemia. Blood Adv. 2020, 4, 930–942. [Google Scholar] [CrossRef] [PubMed]
- Yap, K.L.; Furtado, L.V.; Kiyotani, K.; Curran, E.; Stock, W.; McNeer, J.L.; Kadri, S.; Segal, J.P.; Nakamura, Y.; Le Beau, M.M.; et al. Diagnostic evaluation of RNA sequencing for the detection of genetic abnormalities associated with Ph-like acute lymphoblastic leukemia (ALL). Leuk. Lymphoma 2017, 58, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Mata-Rocha, M.; Rangel-Lopez, A.; Jimenez-Hernandez, E.; Morales-Castillo, B.A.; Gonzalez-Torres, C.; Gaytan-Cervantes, J.; Alvarez-Olmos, E.; Nunez-Enriquez, J.C.; Fajardo-Gutierrez, A.; Martin-Trejo, J.A.; et al. Identification and Characterization of Novel Fusion Genes with Potential Clinical Applications in Mexican Children with Acute Lymphoblastic Leukemia. Int. J. Mol. Sci. 2019, 20, 2394. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, B.; Brown, L.M.; Ryland, G.L.; Lonsdale, A.; Kosasih, H.J.; Ludlow, L.E.; Majewski, I.J.; Blombery, P.; Ekert, P.G.; Davidson, N.M.; et al. ALLSorts: An RNA-Seq subtype classifier for B-cell acute lymphoblastic leukemia. Blood Adv. 2022, 6, 4093–4097. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Jia, Z.; Liu, J.; Mao, A.; Han, H.; Gu, Z. MD-ALL: An integrative platform for molecular diagnosis of B-acute lymphoblastic leukemia. Haematologica 2024, 109, 1741–1754. [Google Scholar] [CrossRef] [PubMed]
- Beder, T.; Hansen, B.T.; Hartmann, A.M.; Zimmermann, J.; Amelunxen, E.; Wolgast, N.; Walter, W.; Zaliova, M.; Antic, Z.; Chouvarine, P.; et al. The Gene Expression Classifier ALLCatchR Identifies B-cell Precursor ALL Subtypes and Underlying Developmental Trajectories Across Age. Hemasphere 2023, 7, e939. [Google Scholar] [CrossRef] [PubMed]
- Byron, S.A.; Van Keuren-Jensen, K.R.; Engelthaler, D.M.; Carpten, J.D.; Craig, D.W. Translating RNA sequencing into clinical diagnostics: Opportunities and challenges. Nat. Rev. Genet. 2016, 17, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Niksic, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Esteve, J.; et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef] [PubMed]
- Ward, Z.J.; Yeh, J.M.; Bhakta, N.; Frazier, A.L.; Girardi, F.; Atun, R. Global childhood cancer survival estimates and priority-setting: A simulation-based analysis. Lancet Oncol. 2019, 20, 972–983. [Google Scholar] [CrossRef] [PubMed]
- de Smith, A.J.; Jimenez-Morales, S.; Mejia-Arangure, J.M. The genetic risk of acute lymphoblastic leukemia and its implications for children of Latin American origin. Front. Oncol. 2023, 13, 1299355. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; de Smith, A.J.; Vergara-Lluri, M.; Muskens, I.S.; McKean-Cowdin, R.; Kogan, S.; Brynes, R.; Wiemels, J.L. Trends in Acute Lymphoblastic Leukemia Incidence in the United States by Race/Ethnicity From 2000 to 2016. Am. J. Epidemiol. 2021, 190, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Schroder, J.; Kumar, A.; Wong, S.Q. Overview of Fusion Detection Strategies Using Next-Generation Sequencing. Methods Mol. Biol. 2019, 1908, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Mata-Rocha, M.; Rangel-Lopez, A.; Jimenez-Hernandez, E.; Nunez-Enriquez, J.C.; Morales-Castillo, B.A.; Sanchez-Escobar, N.; Sepulveda-Robles, O.A.; Bravata-Alcantara, J.C.; Najera-Cortes, A.S.; Perez-Saldivar, M.L.; et al. Low Prevalence of ETV6::RUNX1 Fusion Gene in a Hispanic Population. Front. Pediatr. 2022, 10, 837656. [Google Scholar] [CrossRef] [PubMed]
- Bekker-Mendez, V.C.; Miranda-Peralta, E.; Nunez-Enriquez, J.C.; Olarte-Carrillo, I.; Guerra-Castillo, F.X.; Pompa-Mera, E.N.; Ocana-Mondragon, A.; Rangel-Lopez, A.; Bernaldez-Rios, R.; Medina-Sanson, A.; et al. Prevalence of gene rearrangements in Mexican children with acute lymphoblastic leukemia: A population study-report from the Mexican Interinstitutional Group for the identification of the causes of childhood leukemia. BioMed Res. Int. 2014, 2014, 210560. [Google Scholar] [CrossRef] [PubMed]
- Juarez-Avendano, G.; Luna-Silva, N.C.; Chargoy-Vivaldo, E.; Juarez-Martinez, L.A.; Martinez-Rangel, M.N.; Zarate-Ortiz, N.; Martinez-Valencia, E.; Lopez-Martinez, B.; Pelayo, R.; Balandran, J.C. Poor Prognosis Biomolecular Factors Are Highly Frequent in Childhood Acute Leukemias From Oaxaca, Mexico. Technol. Cancer Res. Treat. 2020, 19, 1533033820928436. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.U.; Chi, H.S.; Park, C.J.; Jang, S.; Seo, E.J. Rapid detection of prognostically significant fusion transcripts in acute leukemia using simplified multiplex reverse transcription polymerase chain reaction. J. Korean Med. Sci. 2012, 27, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Barron, C.; Burack, W.R.; Rothberg, P.G.; Ding, Y. Next-Generation Sequencing for Minimal Residual Disease Surveillance in Acute Lymphoblastic Leukemia: An Update. Crit. Rev. Oncog. 2017, 22, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Stefan, A.I.; Radu, L.E.; Jardan, D.; Colita, A. The emerging role of next-generation sequencing in minimal residual disease assessment in acute lymphoblastic leukemia: A systematic review of current literature. Front. Med. 2025, 12, 1570041. [Google Scholar] [CrossRef] [PubMed]
- Heyer, E.E.; Blackburn, J. Sequencing Strategies for Fusion Gene Detection. Bioessays 2020, 42, e2000016. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.V.; Nagasaka, M.; Atz, J.; Solca, F.; Mullauer, L. Oncogenic gene fusions in cancer: From biology to therapy. Signal Transduct. Target. Ther. 2025, 10, 111. [Google Scholar] [CrossRef] [PubMed]
- Hasty, P.; Montagna, C. Chromosomal Rearrangements in Cancer: Detection and potential causal mechanisms. Mol. Cell. Oncol. 2014, 1, e29904. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.C.; Chan-Seng-Yue, M.; Ge, S.; Zeng, A.G.X.; Ng, K.; Gan, O.I.; Garcia-Prat, L.; Flores-Figueroa, E.; Woo, T.; Zhang, A.X.W.; et al. Transcriptomic classes of BCR-ABL1 lymphoblastic leukemia. Nat. Genet. 2023, 55, 1186–1197. [Google Scholar] [CrossRef] [PubMed]
- Jakobczyk, H.; Jiang, Y.; Debaize, L.; Soubise, B.; Avner, S.; Serandour, A.A.; Rouger-Gaudichon, J.; Rio, A.G.; Carroll, J.S.; Raslova, H.; et al. ETV6-RUNX1 and RUNX1 directly regulate RAG1 expression: One more step in the understanding of childhood B-cell acute lymphoblastic leukemia leukemogenesis. Leukemia 2022, 36, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Bursen, A.; Schwabe, K.; Ruster, B.; Henschler, R.; Ruthardt, M.; Dingermann, T.; Marschalek, R. The AF4.MLL fusion protein is capable of inducing ALL in mice without requirement of MLL.AF4. Blood 2010, 115, 3570–3579. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Wong, S.H.; Kurzer, J.H.; Schneidawind, C.; Wei, M.C.; Duque-Afonso, J.; Jeong, J.; Feng, X.; Cleary, M.L. SETDB2 Links E2A-PBX1 to Cell-Cycle Dysregulation in Acute Leukemia through CDKN2C Repression. Cell Rep. 2018, 23, 1166–1177. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, K.M.; Qu, C.; Gao, Q.; Iacobucci, I.; Gu, Z.; Yoshihara, H.; Backhaus, E.A.; Chang, Y.; Janke, L.J.; Xu, B.; et al. ZNF384 Fusion Oncoproteins Drive Lineage Aberrancy in Acute Leukemia. Blood Cancer Discov. 2022, 3, 240–263. [Google Scholar] [CrossRef] [PubMed]
- Fischer, U.; Yang, J.J.; Ikawa, T.; Hein, D.; Vicente-Duenas, C.; Borkhardt, A.; Sanchez-Garcia, I. Cell Fate Decisions: The Role of Transcription Factors in Early B-cell Development and Leukemia. Blood Cancer Discov. 2020, 1, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Cieslik, M.; Chinnaiyan, A.M. Cancer transcriptome profiling at the juncture of clinical translation. Nat. Rev. Genet. 2018, 19, 93–109. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef] [PubMed]
- Choon, Y.W.; Choon, Y.F.; Nasarudin, N.A.; Al Jasmi, F.; Remli, M.A.; Alkayali, M.H.; Mohamad, M.S. Artificial intelligence and database for NGS-based diagnosis in rare disease. Front. Genet. 2023, 14, 1258083. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, N.; Shahid, S.; Bakhshi, T.; Riaz, S.; Ghufran, H.; Yaqoob, M. Identification of significant risks in pediatric acute lymphoblastic leukemia (ALL) through machine learning (ML) approach. Med. Biol. Eng. Comput. 2020, 58, 2631–2640. [Google Scholar] [CrossRef] [PubMed]
- Ayyappan, V.; Chang, A.; Zhang, C.; Paidi, S.K.; Bordett, R.; Liang, T.; Barman, I.; Pandey, R. Identification and Staging of B-Cell Acute Lymphoblastic Leukemia Using Quantitative Phase Imaging and Machine Learning. ACS Sens. 2020, 5, 3281–3289. [Google Scholar] [CrossRef] [PubMed]
- Kashef, A.; Khatibi, T.; Mehrvar, A. Prediction of Cranial Radiotherapy Treatment in Pediatric Acute Lymphoblastic Leukemia Patients Using Machine Learning: A Case Study at MAHAK Hospital. Asian Pac. J. Cancer Prev. 2020, 21, 3211–3219. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Liu, G.; Lin, F.; Zhong, S.; Xia, H.; Sun, X.; Liang, H. Machine learning applications for prediction of relapse in childhood acute lymphoblastic leukemia. Sci. Rep. 2017, 7, 7402. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Cho, S.; Hong, S.E.; Kang, D.; Choi, H.; Lee, J.M.; Yoon, J.H.; Cho, B.S.; Lee, S.; Kim, H.J.; et al. Integrative Analysis of Gene Expression Data by RNA Sequencing for Differential Diagnosis of Acute Leukemia: Potential Application of Machine Learning. Front. Oncol. 2021, 11, 717616. [Google Scholar] [CrossRef] [PubMed]
- Makinen, V.P.; Rehn, J.; Breen, J.; Yeung, D.; White, D.L. Multi-Cohort Transcriptomic Subtyping of B-Cell Acute Lymphoblastic Leukemia. Int. J. Mol. Sci. 2022, 23, 4574. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.J. Targeting signaling pathways in acute lymphoblastic leukemia: New insights. Hematol. Am. Soc. Hematol. Educ. Program 2013, 2013, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Vojcek, A.; Pajor, L. High hyperdiploid acute lymphoblastic leukemia is a highly curable subtype of childhood leukemia. Magy. Onkol. 2018, 62, 214–221. [Google Scholar] [PubMed]
- Li, J.F.; Dai, Y.T.; Lilljebjorn, H.; Shen, S.H.; Cui, B.W.; Bai, L.; Liu, Y.F.; Qian, M.X.; Kubota, Y.; Kiyoi, H.; et al. Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1,223 cases. Proc. Natl. Acad. Sci. USA 2018, 115, E11711–E11720. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; McCastlain, K.; Yoshihara, H.; Xu, B.; Chang, Y.; Churchman, M.L.; Wu, G.; Li, Y.; Wei, L.; Iacobucci, I.; et al. Deregulation of DUX4 and ERG in acute lymphoblastic leukemia. Nat. Genet. 2016, 48, 1481–1489. [Google Scholar] [CrossRef] [PubMed]
- Brady, S.W.; Roberts, K.G.; Gu, Z.; Shi, L.; Pounds, S.; Pei, D.; Cheng, C.; Dai, Y.; Devidas, M.; Qu, C.; et al. The genomic landscape of pediatric acute lymphoblastic leukemia. Nat. Genet. 2022, 54, 1376–1389. [Google Scholar] [CrossRef] [PubMed]
- Schwab, C.; Cranston, R.E.; Ryan, S.L.; Butler, E.; Winterman, E.; Hawking, Z.; Bashton, M.; Enshaei, A.; Russell, L.J.; Kingsbury, Z.; et al. Integrative genomic analysis of childhood acute lymphoblastic leukaemia lacking a genetic biomarker in the UKALL2003 clinical trial. Leukemia 2023, 37, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Krali, O.; Marincevic-Zuniga, Y.; Arvidsson, G.; Enblad, A.P.; Lundmark, A.; Sayyab, S.; Zachariadis, V.; Heinaniemi, M.; Suhonen, J.; Oksa, L.; et al. Multimodal classification of molecular subtypes in pediatric acute lymphoblastic leukemia. NPJ Precis. Oncol. 2023, 7, 131. [Google Scholar] [CrossRef]
- Duarte-Rodriguez, D.A.; Flores-Lujano, J.; McNally, R.J.Q.; Perez-Saldivar, M.L.; Jimenez-Hernandez, E.; Martin-Trejo, J.A.; Espinoza-Hernandez, L.E.; Medina-Sanson, A.; Paredes-Aguilera, R.; Merino-Pasaye, L.E.; et al. Evidence of spatial clustering of childhood acute lymphoblastic leukemia cases in Greater Mexico City: Report from the Mexican Inter-Institutional Group for the identification of the causes of childhood leukemia. Front. Oncol. 2024, 14, 1304633. [Google Scholar] [CrossRef] [PubMed]
- Acharya, S.; Hsieh, S.; Shinohara, E.T.; DeWees, T.; Frangoul, H.; Perkins, S.M. Effects of Race/Ethnicity and Socioeconomic Status on Outcome in Childhood Acute Lymphoblastic Leukemia. J. Pediatr. Hematol. Oncol. 2016, 38, 350–354. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Almaguer, D.; Ruiz-Arguelles, G.J.; Ponce-de-Leon, S. Nutritional status and socio-economic conditions as prognostic factors in the outcome of therapy in childhood acute lymphoblastic leukemia. Int. J. Cancer Suppl. 1998, 11, 52–55. [Google Scholar] [CrossRef]
- Wu, E.; Palmer, N.; Tian, Z.; Moseman, A.P.; Galdzicki, M.; Wang, X.; Berger, B.; Zhang, H.; Kohane, I.S. Comprehensive dissection of PDGF-PDGFR signaling pathways in PDGFR genetically defined cells. PLoS ONE 2008, 3, e3794. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Ghazanfari, R.; Zacharaki, D.; Ditzel, N.; Isern, J.; Ekblom, M.; Mendez-Ferrer, S.; Kassem, M.; Scheding, S. Low/negative expression of PDGFR-alpha identifies the candidate primary mesenchymal stromal cells in adult human bone marrow. Stem Cell Rep. 2014, 3, 965–974. [Google Scholar] [CrossRef] [PubMed]
- Artinyan, A.; Kim, J.; Soriano, P.; Chow, W.; Bhatia, S.; Ellenhorn, J.D. Metastatic gastrointestinal stromal tumors in the era of imatinib: Improved survival and elimination of socioeconomic survival disparities. Cancer Epidemiol. Biomark. Prev. 2008, 17, 2194–2201. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sun, Y.; Yue, L.; Xu, P.; Hu, W. An overview of agents and treatments for PDGFRA-mutated gastrointestinal stromal tumors. Front. Oncol. 2022, 12, 927587. [Google Scholar] [CrossRef] [PubMed]
- Bauer, S.; George, S.; von Mehren, M.; Heinrich, M.C. Early and Next-Generation KIT/PDGFRA Kinase Inhibitors and the Future of Treatment for Advanced Gastrointestinal Stromal Tumor. Front. Oncol. 2021, 11, 672500. [Google Scholar] [CrossRef] [PubMed]
- Pui, C.H.; Roberts, K.G.; Yang, J.J.; Mullighan, C.G. Philadelphia Chromosome-like Acute Lymphoblastic Leukemia. Clin. Lymphoma Myeloma Leuk. 2017, 17, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.G.; Morin, R.D.; Zhang, J.; Hirst, M.; Zhao, Y.; Su, X.; Chen, S.C.; Payne-Turner, D.; Churchman, M.L.; Harvey, R.C.; et al. Genetic alterations activating kinase and cytokine receptor signaling in high-risk acute lymphoblastic leukemia. Cancer Cell 2012, 22, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Maude, S.L.; Tasian, S.K.; Vincent, T.; Hall, J.W.; Sheen, C.; Roberts, K.G.; Seif, A.E.; Barrett, D.M.; Chen, I.M.; Collins, J.R.; et al. Targeting JAK1/2 and mTOR in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood 2012, 120, 3510–3518. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.G.; Yang, Y.L.; Payne-Turner, D.; Lin, W.; Files, J.K.; Dickerson, K.; Gu, Z.; Taunton, J.; Janke, L.J.; Chen, T.; et al. Oncogenic role and therapeutic targeting of ABL-class and JAK-STAT activating kinase alterations in Ph-like ALL. Blood Adv. 2017, 1, 1657–1671. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Roberts, K.G.; Jabbour, E.; Patel, K.; Eterovic, A.K.; Chen, K.; Zweidler-McKay, P.; Lu, X.; Fawcett, G.; Wang, S.A.; et al. Ph-like acute lymphoblastic leukemia: A high-risk subtype in adults. Blood 2017, 129, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.G.; Pei, D.; Campana, D.; Payne-Turner, D.; Li, Y.; Cheng, C.; Sandlund, J.T.; Jeha, S.; Easton, J.; Becksfort, J.; et al. Outcomes of children with BCR-ABL1-like acute lymphoblastic leukemia treated with risk-directed therapy based on the levels of minimal residual disease. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2014, 32, 3012–3020. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Anaya, D.; Moreno-Lorenzana, D.; Reyes-Leon, A.; Juarez-Figueroa, U.; Dean, M.; Aguilar-Hernandez, M.M.; Rivera-Sanchez, N.; Garcia-Islas, J.; Vieyra-Fuentes, V.; Zapata-Tarres, M.; et al. Characterization of Philadelphia-like Pre-B Acute Lymphoblastic Leukemia: Experiences in Mexican Pediatric Patients. Int. J. Mol. Sci. 2022, 23, 9587. [Google Scholar] [CrossRef] [PubMed]
- Bercovich, D.; Ganmore, I.; Scott, L.M.; Wainreb, G.; Birger, Y.; Elimelech, A.; Shochat, C.; Cazzaniga, G.; Biondi, A.; Basso, G.; et al. Mutations of JAK2 in acute lymphoblastic leukaemias associated with Down’s syndrome. Lancet 2008, 372, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Chiaretti, S.; Brugnoletti, F.; Messina, M.; Paoloni, F.; Fedullo, A.L.; Piciocchi, A.; Elia, L.; Vitale, A.; Mauro, E.; Ferrara, F.; et al. CRLF2 overexpression identifies an unfavourable subgroup of adult B-cell precursor acute lymphoblastic leukemia lacking recurrent genetic abnormalities. Leuk. Res. 2016, 41, 36–42. [Google Scholar] [CrossRef] [PubMed]
- He, R.; Geha, R.S. Thymic stromal lymphopoietin. Ann. N. Y. Acad. Sci. 2010, 1183, 13–24. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Escobar, N.; Romero-Tlalolini, M.d.l.Á.; Rosas-Vargas, H.; Jiménez-Hernández, E.; Núñez Enríquez, J.C.; Rangel-López, A.; Sánchez López, J.M.; Rojo-Serrato, D.; Jasso Mata, A.M.; Márquez Aguilar, E.A.; et al. Identification of Molecular Subtypes of B-Cell Acute Lymphoblastic Leukemia in Mexican Children by Whole-Transcriptome Analysis. Int. J. Mol. Sci. 2025, 26, 7003. https://doi.org/10.3390/ijms26147003
Sánchez-Escobar N, Romero-Tlalolini MdlÁ, Rosas-Vargas H, Jiménez-Hernández E, Núñez Enríquez JC, Rangel-López A, Sánchez López JM, Rojo-Serrato D, Jasso Mata AM, Márquez Aguilar EA, et al. Identification of Molecular Subtypes of B-Cell Acute Lymphoblastic Leukemia in Mexican Children by Whole-Transcriptome Analysis. International Journal of Molecular Sciences. 2025; 26(14):7003. https://doi.org/10.3390/ijms26147003
Chicago/Turabian StyleSánchez-Escobar, Norberto, María de los Ángeles Romero-Tlalolini, Haydeé Rosas-Vargas, Elva Jiménez-Hernández, Juan Carlos Núñez Enríquez, Angélica Rangel-López, José Manuel Sánchez López, Daniela Rojo-Serrato, América Mariana Jasso Mata, Efraín Abimael Márquez Aguilar, and et al. 2025. "Identification of Molecular Subtypes of B-Cell Acute Lymphoblastic Leukemia in Mexican Children by Whole-Transcriptome Analysis" International Journal of Molecular Sciences 26, no. 14: 7003. https://doi.org/10.3390/ijms26147003
APA StyleSánchez-Escobar, N., Romero-Tlalolini, M. d. l. Á., Rosas-Vargas, H., Jiménez-Hernández, E., Núñez Enríquez, J. C., Rangel-López, A., Sánchez López, J. M., Rojo-Serrato, D., Jasso Mata, A. M., Márquez Aguilar, E. A., Flores-Lujano, J., Bravata-Alcántara, J. C., Martín-Trejo, J. A., Jiménez-Morales, S., Arellano-Galindo, J., Sanson, A. M., Gonzalez, J. G. P., Mejía-Aranguré, J. M., & Mata-Rocha, M. (2025). Identification of Molecular Subtypes of B-Cell Acute Lymphoblastic Leukemia in Mexican Children by Whole-Transcriptome Analysis. International Journal of Molecular Sciences, 26(14), 7003. https://doi.org/10.3390/ijms26147003







