Evaluation of Ropivacaine and 3-OH-Ropivacaine Pharmacokinetics Following Interpectoral Nerve Block via LC-MS/MS—A Pilot Study
Abstract
1. Introduction
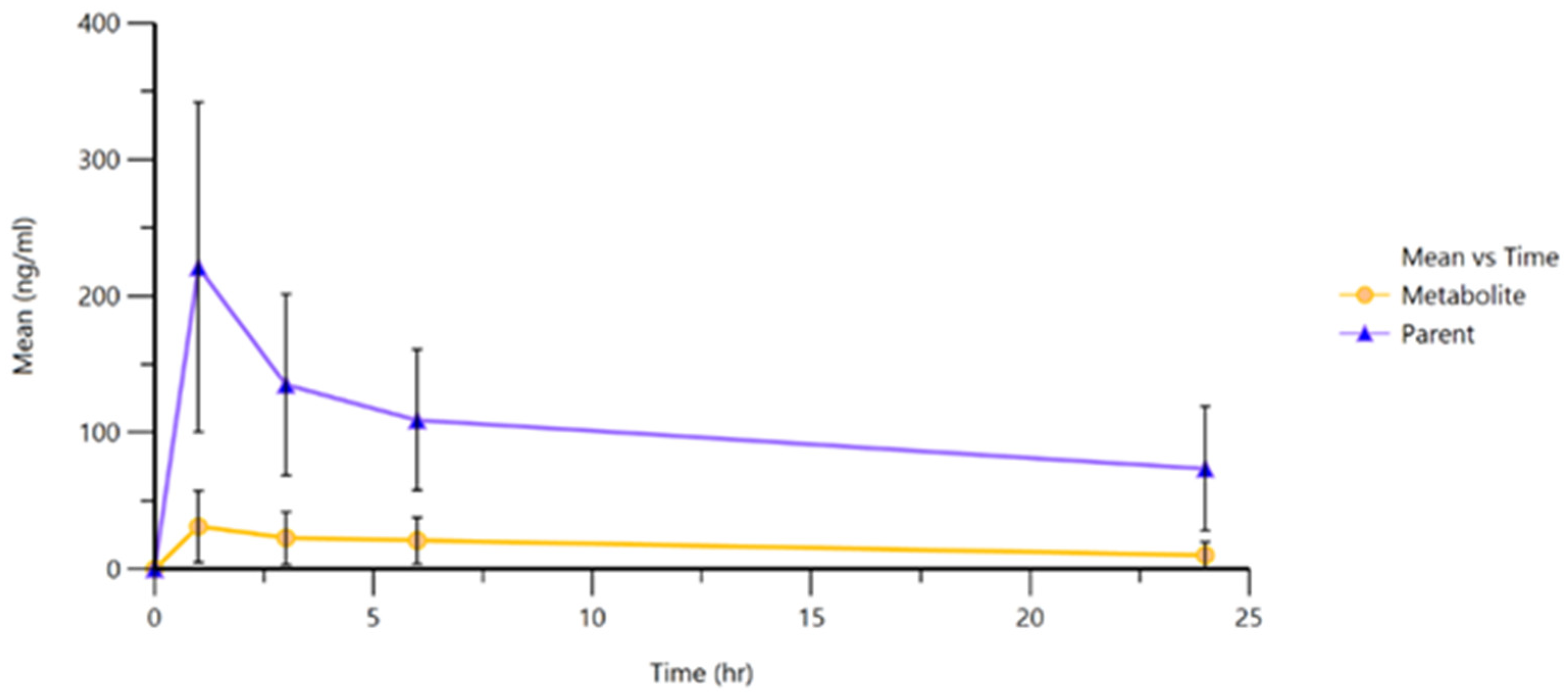
2. Results
3. Discussion
3.1. Pharmacokinetic Considerations
3.2. Clinical and Therapeutic Implications
3.3. Limitations
3.4. Future Directions
4. Materials and Methods
4.1. Selection of Study Subjects
4.2. Anesthetic Procedure for Interpectoral (PECS) Block
4.3. Sample Collection
4.4. Sample Processing
4.5. Standard Solutions and Analyte Extraction
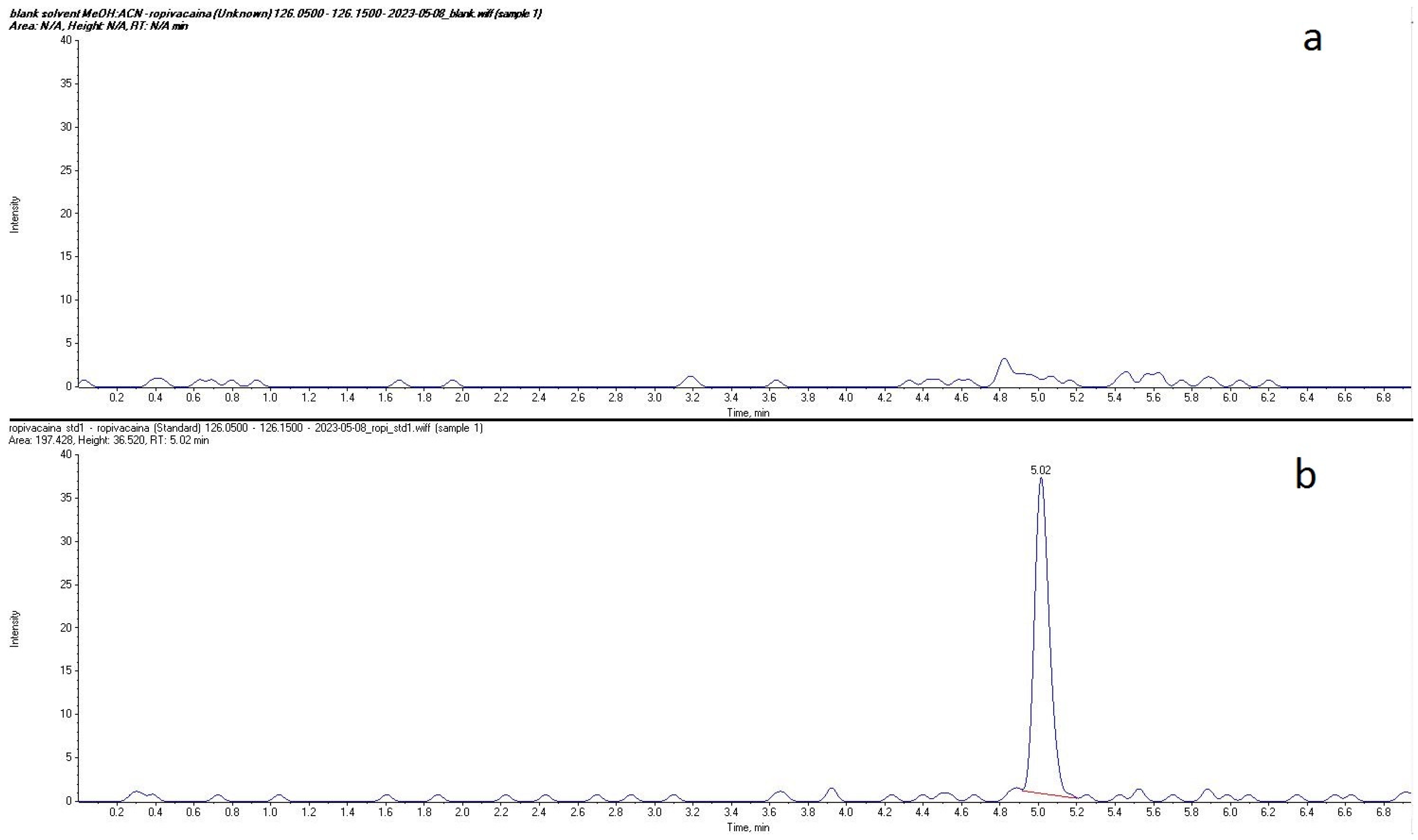
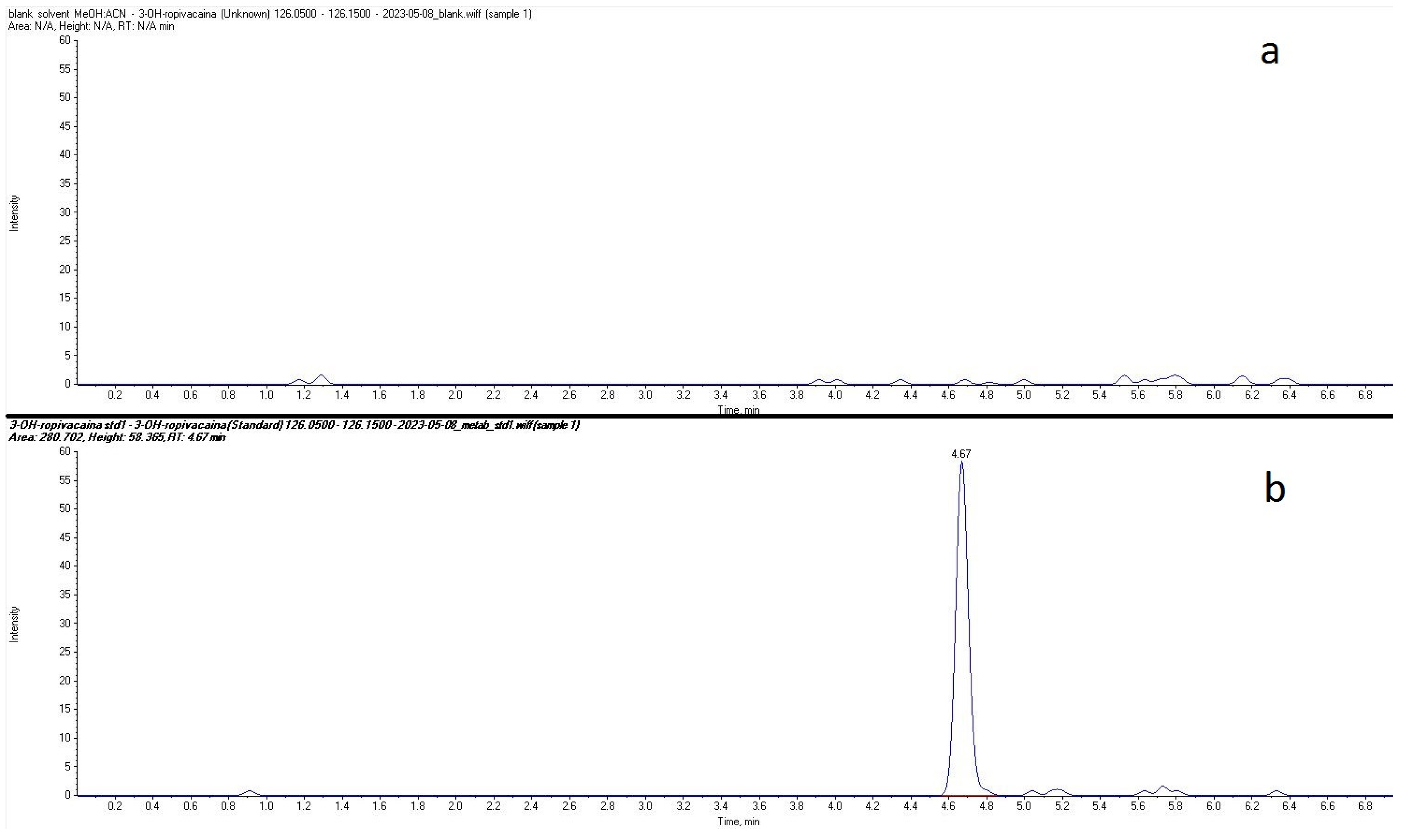
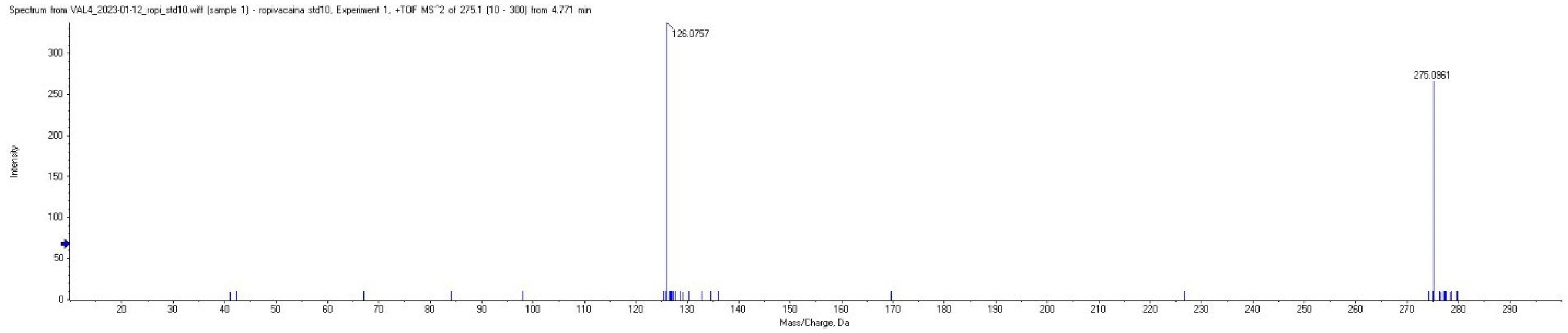
4.6. LC-MS/MS Analysis
4.7. Pharmacokinetic Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PECS II | Pectoral Nerve Block |
| LC-MS/MS | liquid chromatography coupled with tandem mass spectrometry |
| FDA | Food and Drug Administration |
| EMA | European Medicines Agency |
| Cmax | maximum plasmatic concentration |
| Tmax | time of maximum concentration |
| HPLC | high-performance liquid chromatography |
| QC | quality control |
| AUC | area under the curve |
| SD | standard deviation |
| CV | coefficient of variation |
References
- McClellan, K.J.; Faulds, D. Ropivacaine: An Update of Its Use in Regional Anaesthesia. Drugs 2000, 60, 1065–1093. [Google Scholar] [CrossRef] [PubMed]
- Devarajan, J.; Balasubramanian, S.; Shariat, A.N.; Bhatt, H.V. Regional Analgesia for Cardiac Surgery. Part 2: Peripheral Regional Analgesia for Cardiac Surgery. In Seminars in Cardiothoracic and Vascular Anesthesia; SAGE Publications: Los Angeles, CA, USA, 2021; pp. 265–279. [Google Scholar]
- Kaushal, B.; Chauhan, S.; Saini, K.; Bhoi, D.; Bisoi, A.K.; Sangdup, T.; Khan, M.A. Comparison of the Efficacy of Ultrasound-Guided Serratus Anterior Plane Block, Pectoral Nerves II Block, and Intercostal Nerve Block for the Management of Postoperative Thoracotomy Pain After Pediatric Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2019, 33, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Fallon, F.; Moorthy, A.; Skerritt, C.; Crowe, G.G.; Buggy, D.J. Latest Advances in Regional Anaesthesia. Medicina (B Aires) 2024, 60, 735. [Google Scholar] [CrossRef] [PubMed]
- Ekström, G.; Gunnarsson, U.B. Ropivacaine, a new amide-type local anesthetic agent, is metabolized by cytochromes P450 1A and 3A in human liver microsomes. Drug Metab. Dispos. 1996, 24, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Simpson, D.; Curran, M.P.; Oldfield, V.; Keating, G.M. Ropivacaine: A Review of Its Use in Regional Anaesthesia and Acute Pain Management. Drugs 2005, 65, 2675–2717. [Google Scholar] [CrossRef] [PubMed]
- Nikolin, B.; Imamović, B.; Medanhodzić-Vuk, S.; Sober, M. High Perfomance Liquid Chromatography in Pharmaceutical Analyses. Bosn. J. Basic. Med. Sci. 2004, 4, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Ling, J.; Xu, C.; Tang, L.; Qiu, L.; Hu, N. Comparison of the Pharmacokinetic Variations of Different Concentrations of Ropivacaine Used for Serratus Anterior Plane Block in Patients Undergoing Thoracoscopic Lobectomy: A Population Pharmacokinetics Analysis. Front. Pharmacol. 2025, 26, 1540606. [Google Scholar] [CrossRef] [PubMed]
- Versyck, B.; Vermeylen, K.; Willemse, J.; van Geffen, G.J.; Leunen, I.; Soetens, F.; Devos, S.; Serum, L.R. Concentrations of Local Anesthetics After Unilateral Interpectoral-Pectoserratus Plane Block in Breast Cancer Surgery: A Pharmacokinetic Study. Reg. Anesth. Pain. Med. 2023, 48, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, I.M.; Meng, C.; Dong, Z.; Lou, B.; Xu, G. Potentiometric Sensors for the Determination of Pharmaceutical Drugs. Anal. Sci. 2022, 38, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Guo, X.; Wang, K.; Chen, Q.; Wang, Y.; Chen, L.; Gao, W.; Cheng, B.; Jin, Z. A retrospective multicenter study comparing bupivacaine and ropivacaine in endoscopic ultrasound guided celiac plexus neurolysis. Ann. Palliat. Med. 2021, 10, 1755–1762. [Google Scholar] [CrossRef] [PubMed]
- Butiulca, M.; Farczadi, L.; Imre, S.; Vari, C.E.; Vlase, L.; Cordos, B.; Azamfirei, L.; Lazar, A.E. LC-MS/MS assisted pharmacokinetic and tissue distribution study of ropivacaine and 3-OH-ropivacaine on rats after plane block anesthesia. Front. Pharmacol. 2024, 15, 1494646. [Google Scholar] [CrossRef] [PubMed]
- Rössel, T.; Uhlig, C.; Pietsch, J.; Ludwig, S.; Koch, T.; Richter, T.; Spieth, P.M.; Kersting, S. Effects of Regional Anesthesia Techniques on Local Anesthetic Plasma Levels and Complications in Carotid Surgery: A Randomized Controlled Pilot Trial. BMC Anesthesiol. 2019, 19, 218. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yuan, L.; Pan, L.; Ji, Q.C. Bioanalysis of Biological Matrix Samples Using Liquid Chromatography–Tandem Mass Spectrometry Detection. In Specification of Drug Substances and Products, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Mathur, V.; Kumari, B.; Verma, A.K.; Khare, A.; Garg, D.K. Comparison of Ropivacaine with Ropivacaine–Dexamethasone Combination for Postoperative Analgesia in the Pectoral Nerve Block for Modified Radical Mastectomy: A Randomized Clinical trial. Indian Anaesth. Forum. 2024, 25, 86–91. [Google Scholar] [CrossRef]
- Janc, J.; Szamborski, M.; Milnerowicz, A.; Łysenko, L.; Leśnik, P. Evaluation of the Effectiveness of Modified Pectoral Nerve Blocks Type II (PECS II) for Vascular Access Port Implantation Using Cephalic Vein Venesection. J. Clin. Med. 2021, 10, 5759. [Google Scholar] [CrossRef] [PubMed]
- Latzke, D.; Marhofer, P.; Kettner, S.C.; Koppatz, K.; Turnheim, K.; Lackner, E.; Sauermann, R.; Müller, M.; Zeitlinger, M. Pharmacokinetics of the Local Anesthetic Ropivacaine After Transversus Abdominis Plane Block in Healthy Volunteers. Eur. J. Clin. Pharmacol. 2012, 68, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Leite-Moreira, A.M.; Correia, A.; Vale, N.; Mourão, J.B. Pharmacokinetics in Regional Anesthesia. Curr. Opin. Anesthesiology 2024, 37, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Lv, C.; Yang, L.; Wang, S.; Zhang, M.; Guo, X. Pharmacokinetics of Ropivacaine in Elderly Patients Receiving Fascia Iliaca Compartment Block. Exp. Ther. Med. 2019, 18, 2648–2652. [Google Scholar] [CrossRef] [PubMed]
- Matsota, P.; Karalis, V.; Saranteas, T.; Kiospe, F.; Markantonis, S.L. Ropivacaine Pharmacokinetics in the Arterial and Venous Pools After Ultrasound-Guided Continuous Thoracic Paravertebral Nerve Block. J. Anaesthesiol. Clin. Pharmacol. 2024, 40, 283–292. [Google Scholar] [CrossRef] [PubMed]
- EMEA/CHMP/EWP/192217/2009 Rev. 1 Corr. 2** Committee for Medicinal Products for Human Use (CHMP) [Internet]. 2011. Guideline on Bioanalytical Method Validation. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-bioanalytical-method-validation_en.pdf (accessed on 8 July 2025).
- Lamy, E.; Fall, F.; Boigne, L.; Gromov, K.; Fabresse, N.; Grassin-Delyle, S. Validation According to European and American regulatory Agencies Guidelines of an LC-MS/MS Method for the Quantification of Free and Total Ropivacaine in Human Plasma. Clin. Chem. Lab. Med. 2020, 58, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Butiulca, M.; Farczadi, L.; Vari, C.E.; Imre, S.; Pui, M.; Lazar, A. LC-MS/MS Assisted Biomonitoring of Ropivacaine and 3-OH-Ropivacaine After Plane Block Anesthesia for Cardiac Device Implantation. Front. Mol. Biosci. 2023, 10, 1243103. [Google Scholar] [CrossRef] [PubMed]


| Probe No. | Cmax (ng·mL−1) | Tmax (h) | AUC (hr ∗ ng mL−1) | Elimination Rate Constant (1 h−1) | Half-Time (h) | Distribution Volume (L kg−1) | Clearance (L h−1 kg−1) |
|---|---|---|---|---|---|---|---|
| 1 | 537.61 | 1.00 | 3037.65 | 0.05 | 15.16 | 9.38 | 428.54 |
| 2 | 427.72 | 1.00 | 5260.61 | 0.02 | 29.77 | 6.60 | 153.70 |
| 3 | 308.92 | 1.00 | 2224.24 | 0.13 | 5.45 | 6.76 | 859.54 |
| 4 | 169.74 | 1.00 | 2270.55 | 0.03 | 25.09 | 14.86 | 410.45 |
| 5 | 198.65 | 1.00 | 2031.03 | 0.03 | 20.13 | 15.89 | 547.03 |
| 6 | 167.57 | 6.00 | 2727.88 | 0.06 | 11.04 | 8.87 | 557.17 |
| 7 | 216.72 | 1.00 | 2781.24 | 0.04 | 17.50 | 11.21 | 444.09 |
| 8 | 285.97 | 1.00 | 2678.63 | 0.03 | 20.79 | 12.53 | 417.88 |
| 9 | 101.88 | 1.00 | 2066.14 | 0.05 | 12.81 | 14.30 | 773.57 |
| 10 | 293.92 | 1.00 | 4887.17 | 0.02 | 33.09 | 7.56 | 158.39 |
| 11 | 127.46 | 1.00 | 1053.57 | 0.04 | 18.37 | 30.23 | 1141.09 |
| 12 | 297.75 | 1.00 | 2778.64 | 0.11 | 6.58 | 6.33 | 667.60 |
| 13 | 217.28 | 1.00 | 1369.15 | 0.05 | 15.38 | 22.30 | 1005.34 |
| 14 | 106.96 | 1.00 | 1704.85 | 0.06 | 11.04 | 15.77 | 989.71 |
| 15 | 130.01 | 1.00 | 1474.43 | 0.03 | 22.47 | 21.46 | 662.03 |
| 16 | 109.04 | 1.00 | 2039.96 | 0.05 | 15.38 | 15.88 | 715.48 |
| 17 | 101.96 | 1.00 | 1646.73 | 0.02 | 31.33 | 21.61 | 478.04 |
| 18 | 208.90 | 1.00 | 2532.91 | 0.02 | 35.27 | 14.89 | 292.60 |
| Nr. Ctr. | Cmax (ng mL−1) | Tmax (h) | AUC (hr ∗ ng mL−1) | Elimination Rate Constant (1 h−1) | Half-Time (h) | Volume of Distribution (L kg−1) | Clearance (L h−1 kg−1) |
|---|---|---|---|---|---|---|---|
| 1 | 35.90 | 1.00 | 257.11 | 0.05 | 14.53 | 114.58 | 5464.18 |
| 2 | 18.71 | 1.00 | 219.09 | 0.00 | 211.26 | 109.07 | 357.87 |
| 3 | 26.07 | 1.00 | 264.71 | 0.08 | 8.47 | 79.62 | 6519.28 |
| 4 | 7.67 | 6.00 | 126.07 | 0.06 | 10.95 | 191.71 | 12,133.02 |
| 5 | 14.50 | 1.00 | 167.78 | 0.03 | 20.90 | 192.32 | 6379.93 |
| 6 | 33.60 | 1.00 | 402.42 | 0.02 | 36.78 | 102.89 | 1939.08 |
| 7 | 8.21 | 6.00 | 137.47 | 0.06 | 12.49 | 187.73 | 10,419.02 |
| 8 | 47.81 | 1.00 | 439.43 | 0.04 | 16.18 | 67.22 | 2878.89 |
| 9 | 3.29 | 6.00 | 54.77 | 0.05 | 13.42 | 501.02 | 25,870.16 |
| 10 | 25.39 | 1.00 | 147.85 | 0.06 | 12.46 | 188.99 | 10,511.42 |
| 11 | 36.07 | 6.00 | 548.37 | 0.08 | 8.34 | 37.27 | 3098.18 |
| 12 | 99.48 | 1.00 | 1176.18 | 0.10 | 6.83 | 15.43 | 1564.44 |
| 13 | 33.23 | 1.00 | 207.48 | 0.28 | 2.46 | 43.32 | 12,194.29 |
| 14 | 38.35 | 1.00 | 501.29 | 0.03 | 21.18 | 63.47 | 2077.53 |
| 15 | 77.63 | 1.00 | 1072.98 | 0.01 | 61.25 | 39.53 | 447.36 |
| 16 | 40.53 | 3.00 | 531.15 | 0.03 | 27.11 | 61.58 | 1574.20 |
| 17 | 27.28 | 3.00 | 384.83 | 0.06 | 11.72 | 65.94 | 3899.52 |
| 18 | 58.42 | 1.00 | 620.60 | 0.02 | 29.53 | 58.54 | 1373.95 |
| Ropivacaine | Mean | SD | CV (%) | Median | Geometric Mean |
|---|---|---|---|---|---|
| Cmax (ng mL−1) | 222.67 | 119.60 | 53.71 | 203.77 | 196.93 |
| Tmax (h) | 1.28 | 1.18 | 92.23 | 1.00 | 1.10 |
| AUC (hr ∗ ng mL−1) | 2475.85 | 1094.68 | 44.21 | 2247.39 | 2284.99 |
| Elimination rate constant (1 h−1) | 0.05 | 0.03 | 61.91 | 0.04 | 0.04 |
| Half-time (h) | 19.26 | 8.85 | 45.93 | 17.93 | 17.16 |
| Volume of distribution (L kg−1) | 14.25 | 6.52 | 45.73 | 14.58 | 12.90 |
| Clearance (1 h−1 kg−1) | 594.57 | 282.71 | 47.55 | 552.10 | 521.32 |
| 3-OH-Ropivacaine | Mean | SD | CV (%) | Median | Geometric Mean |
|---|---|---|---|---|---|
| Cmax (ng mL−1) | 35.12 | 24.40 | 69.49 | 33.41 | 26.75 |
| Tmax (h) | 2.33 | 2.11 | 90.62 | 1.00 | 1.68 |
| AUC (hr ∗ ng mL−1) | 414.42 | 307.58 | 74.22 | 393.62 | 317.65 |
| Elimination rate constant (1 h−1) | 0.06 | 0.06 | 102.72 | 0.05 | 0.04 |
| Half-time (h) | 29.22 | 47.45 | 162.42 | 13.98 | 16.90 |
| Volume of distribution (L kg−1) | 117.79 | 111.96 | 95.05 | 73.42 | 86.06 |
| Clearance (L h−1 kg−1) | 6039.02 | 6366.91 | 105.43 | 3498.85 | 3529.67 |
| Analyte | Monoisotopic Molecular Weight (g/mol) | Expected Parent Ion [M + 1] (m/z) | Observed Parent Ion (m/z) | Fragment Ion (m/z) |
|---|---|---|---|---|
| Ropivacaine | 274.2 | 275.2 | 275.096 | 126.076 |
| 3-OH-ropivacaine | 290.2 | 291.2 | 291.087 | 126.076 |
| Ropivacaine-d7 (internal standard) | 281.2 | 282.2 | 282.096 | 133.076 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Butiulca, M.; Farczadi, L.; Imre, S.; Vari, C.E.; Vlase, L.; Azamfirei, L.; Lazar, A.E. Evaluation of Ropivacaine and 3-OH-Ropivacaine Pharmacokinetics Following Interpectoral Nerve Block via LC-MS/MS—A Pilot Study. Int. J. Mol. Sci. 2025, 26, 6696. https://doi.org/10.3390/ijms26146696
Butiulca M, Farczadi L, Imre S, Vari CE, Vlase L, Azamfirei L, Lazar AE. Evaluation of Ropivacaine and 3-OH-Ropivacaine Pharmacokinetics Following Interpectoral Nerve Block via LC-MS/MS—A Pilot Study. International Journal of Molecular Sciences. 2025; 26(14):6696. https://doi.org/10.3390/ijms26146696
Chicago/Turabian StyleButiulca, Mihaela, Lenard Farczadi, Silvia Imre, Camil Eugen Vari, Laurian Vlase, Leonard Azamfirei, and Alexandra Elena Lazar. 2025. "Evaluation of Ropivacaine and 3-OH-Ropivacaine Pharmacokinetics Following Interpectoral Nerve Block via LC-MS/MS—A Pilot Study" International Journal of Molecular Sciences 26, no. 14: 6696. https://doi.org/10.3390/ijms26146696
APA StyleButiulca, M., Farczadi, L., Imre, S., Vari, C. E., Vlase, L., Azamfirei, L., & Lazar, A. E. (2025). Evaluation of Ropivacaine and 3-OH-Ropivacaine Pharmacokinetics Following Interpectoral Nerve Block via LC-MS/MS—A Pilot Study. International Journal of Molecular Sciences, 26(14), 6696. https://doi.org/10.3390/ijms26146696







