Biotype Determines Survival of Yersinia enterocolitica in Red Blood Cell Concentrates
Abstract
1. Introduction
2. Results
2.1. Whole-Genome Sequencing of Y. enterocolitica Isolates
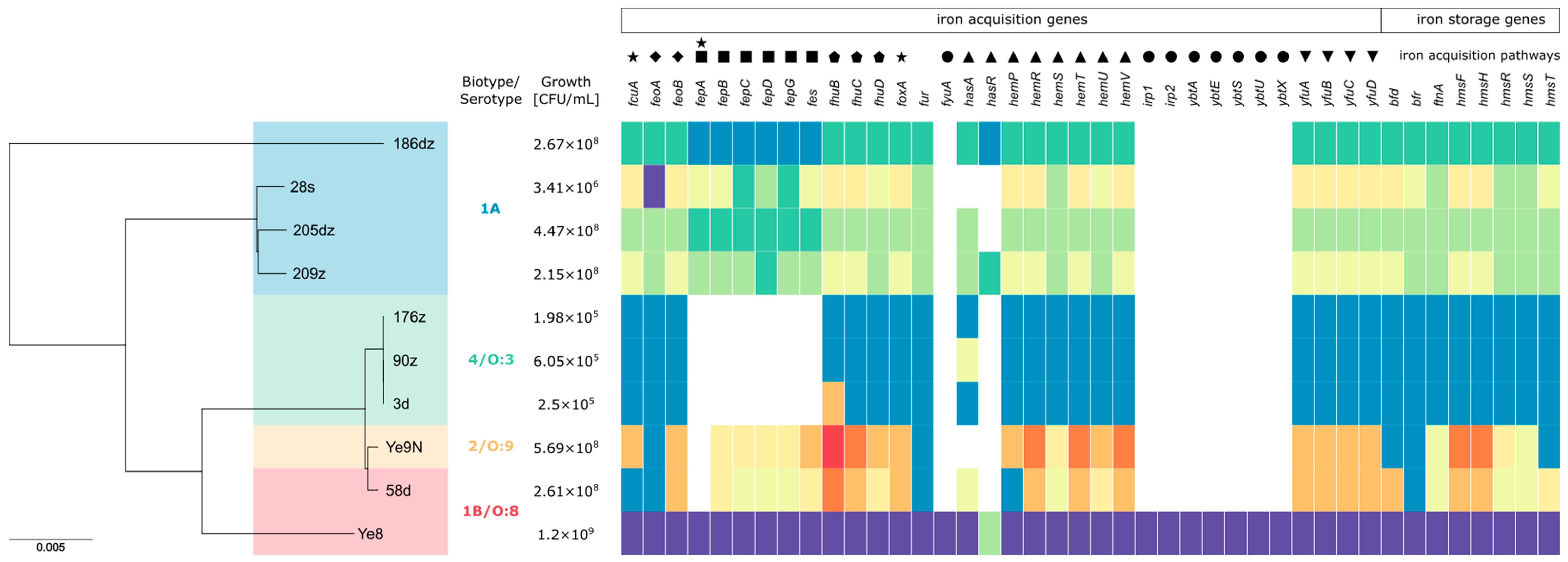
2.2. Phylogenetic Analysis and Detection of Iron Metabolism Genes in Y. enterocolitica Isolates
2.3. Growth of Y. enterocolitica in the RBC Units
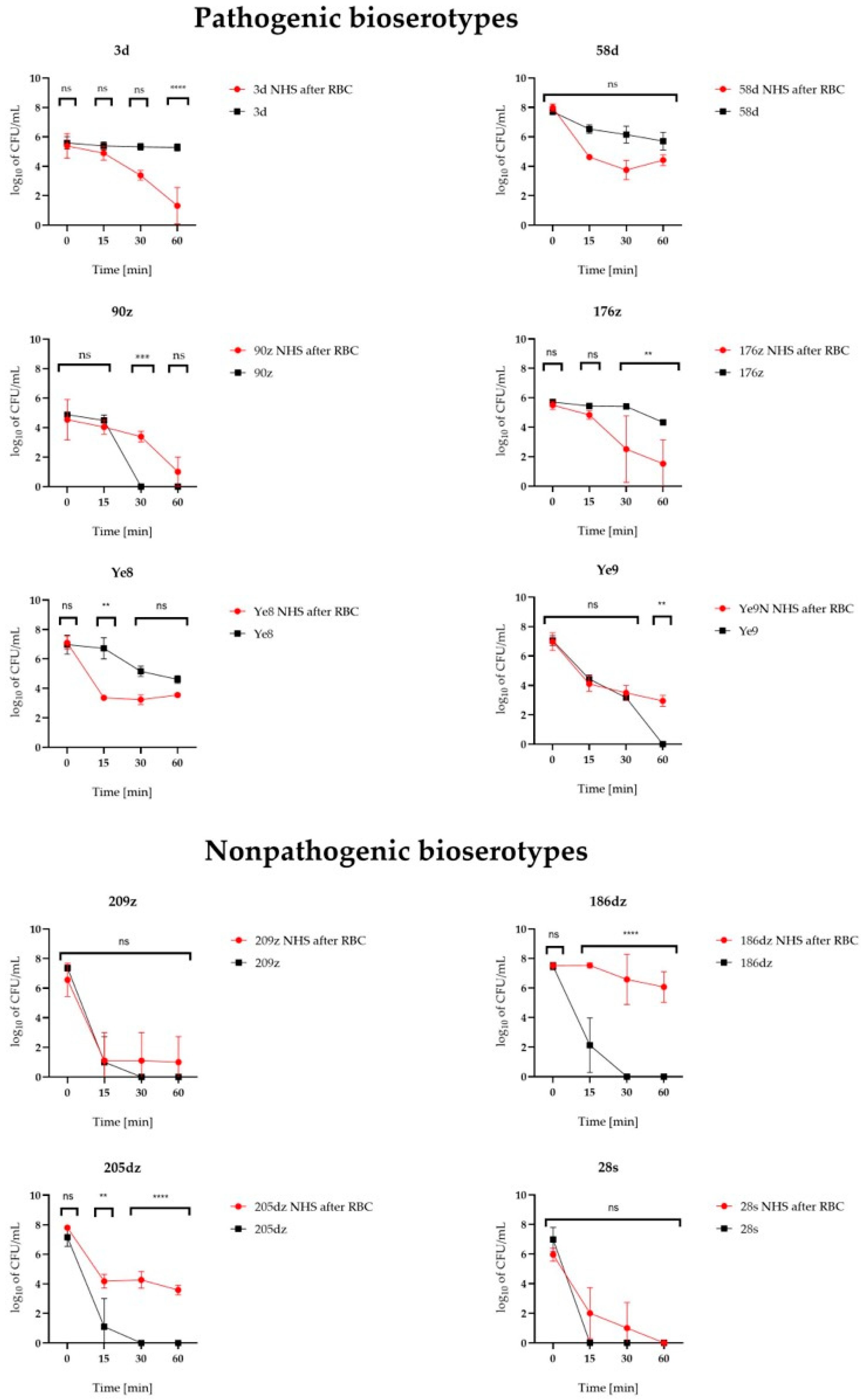
2.4. Pathogenic Bioserotypes Survived Longer Exposure to NHS
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains
4.2. Detection of Virulence-Associated Genes of Y. enterocolitica
4.3. Sequencing of the Genomes
4.4. Phylogenetic Analysis of the Isolates and Iron Metabolism Gene Detection
4.5. Red Blood Cell Concentrate Units
4.6. Incubation of Y. enterocolitica in Red Blood Cells
4.7. Normal Human Serum Bactericidal Tests
4.8. Statistical Methods
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guinet, F.; Carniel, E.; Leclercq, A. Transfusion-transmitted Yersinia Enterocolitica sepsis. Clin. Infect. Dis. 2011, 53, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Prax, M.; Spindler-Raffel, E.; McDonald, C.P.; Bearne, J.; Satake, M.; Kozakai, M.; Rojo, J.; Hanschmann, K.O.; Lambrecht, B.; Grundmann, U.; et al. Establishment of Transfusion-relevant Bacteria Reference Strains for Red Blood Cells. Vox Sang. 2021, 116, 692–701. [Google Scholar] [CrossRef]
- Shepel, M.; Boyd, J.; Luider, J.; Gibb, A.P. Interaction of Yersinia enterocolitica and Y. Pseudotuberculosis with Platelets. J. Med. Microbiol. 2001, 50, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Arcos, S.; Kou, Y.; Cayer, M.; De Grandmont, M.; Girard, M.; Cloutier, M. The Impact of Red Blood Cell Manufacturing Variables on Bacterial Growth Dynamics: A Pilot Study. Vox Sang. 2019, 114, 478–486. [Google Scholar] [CrossRef]
- Hoelen, D.W.M.; Tjan, D.H.T.; Schouten, M.A.; Dujardin, B.C.G.; van Zanten, A.R.H. Severe Yersinia Enterocolitica Sepsis after Blood Transfusion. Neth. J. Med. 2007, 65, 301–303. [Google Scholar]
- Strobel, E.; Heesemann, J.; Mayer, G.; Peters, J.; Müller-Weihrich, S.; Emmerling, P. Bacteriological and Serological Findings in a Further Case of Transfusion-Mediated Yersinia enterocolitica Sepsis. J. Clin. Microbiol. 2000, 38, 2788–2790. [Google Scholar] [CrossRef] [PubMed]
- Frati, P.; Busardò, F.P.; Di Stefano, M.A.; Neri, M.; Sessa, F.; Fineschi, V. A Fatal Case of Post-Transfusion Sepsis Caused by Yersinia Enterocolitica after Delivery. Blood Transfus. 2015, 13, 528–531. [Google Scholar] [CrossRef]
- Wagner, S.J. Transfusion-transmitted Bacterial Infection: Risks, Sources and Interventions. Vox Sang. 2004, 86, 157–163. [Google Scholar] [CrossRef]
- Bruining, A.; De Wilde-Huizen, C.C.M. A case of contamination of donor blood by Yersinia enterocolitica type 9. Med. Ned. 1975, 4, 25–26. [Google Scholar]
- Leclercq, A.; Martin, L.; Vergnes, M.L.; Ounnoughene, N.; Laran, J.; Giraud, P.; Carniel, E. Fatal Yersinia enterocolitica Biotype 4 Serovar O:3 Sepsis after Red Blood Cell Transfusion. Transfusion 2005, 45, 814–818. [Google Scholar] [CrossRef]
- Benavides, S.; Nicol, K.; Koranyi, K.; Nahata, M.C. Yersinia Septic Shock Following an Autologous Transfusion in a Pediatric Patient. Transfus. Apher. Sci. 2003, 28, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Dziennik Urzędowy Ministra Zdrowia. Obwieszczenie Ministra Zdrowia z dnia 30 marca 2021 r. w Sprawie Wymagań Dobrej Praktyki Pobierania Krwi i jej Składników, Badania, Preparatyki, Przechowywania, Wydawania i Transportu dla Jednostek Organizacyjnych Publicznej Służby Krwi. DZ. URZ. Min. Zdr. 2021.28. Available online: https://dziennikmz.mz.gov.pl/legalact/2021/28/ (accessed on 15 April 2025).
- Ramirez-Arcos, S.; Perkins, H.; Kou, Y.; Mastronardi, C.; Kumaran, D.; Taha, M.; Yi, Q.-L.; McLaughlin, N.; Kahwash, E.; Lin, Y.; et al. Bacterial Growth in Red Blood Cell Units Exposed to Uncontrolled Temperatures: Challenging the 30-minute Rule. Vox Sang. 2013, 105, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Orozova, P.; Markova, N.; Radoucheva, T. Properties of Yersinia entetocolitica and Yersinia Pseudotuberculosis in Red Blood Cell Concentrate of Different ABO Groups during 30-Day Storage at 4 °C. Clin. Microbiol. Infect. 2001, 7, 358–361. [Google Scholar] [CrossRef]
- Kanaujia, P.K.; Bajaj, P.; Virdi, J.S. Analysis of Iron Acquisition and Storage-related Genes in Clinical and Non-clinical Strains of Yersinia Enterocolitica Biovar 1A. APMIS 2015, 123, 858–866. [Google Scholar] [CrossRef]
- Jaworska, K.; Nieckarz, M.; Ludwiczak, M.; Raczkowska, A.; Brzostek, K. OmpR-Mediated Transcriptional Regulation and Function of Two Heme Receptor Proteins of Yersinia Enterocolitica Bio-Serotype 2/O:9. Front. Cell. Infect. Microbiol. 2018, 8, 333. [Google Scholar] [CrossRef]
- Rakin, A.; Schneider, L.; Podladchikova, O. Hunger for Iron: The Alternative Siderophore Iron Scavenging Systems in Highly Virulent Yersinia. Front. Cell. Infect. Microbiol. 2012, 2, 151. [Google Scholar] [CrossRef] [PubMed]
- Carniel, E. The Yersinia High-Pathogenicity Island: An Iron-Uptake Island. Microbes Infect. 2001, 3, 561–569. [Google Scholar] [CrossRef]
- Schubert, S.; Fischer, D.; Heesemann, J. Ferric Enterochelin Transport in Yersinia enterocolitica: Molecular and Evolutionary Aspects. J. Bacteriol. 1999, 181, 6387–6395. [Google Scholar] [CrossRef]
- Jaworska, K.; Ludwiczak, M.; Murawska, E.; Raczkowska, A.; Brzostek, K. The Regulator OmpR in Yersinia enterocolitica Participates in Iron Homeostasis by Modulating Fur Level and Affecting the Expression of Genes Involved in Iron Uptake. Int. J. Mol. Sci. 2021, 22, 1475. [Google Scholar] [CrossRef]
- Ventola, E.; Lovari, S.; Farneti, S.; Finazzi, G.; Bilei, S.; Owczarek, S.; Delibato, E. Molecular Characterization of Yersinia enterocolitica Strains to Evaluate Virulence Associated Genes. Ann. Ist. Super. Sanita 2023, 59, 280–285. [Google Scholar] [CrossRef]
- Wauters, G.; Kandolo, K.; Janssens, M. Revised Biogrouping Scheme of Yersinia enterocolitica. Contrib. Microbiol. Immunol. 1987, 9, 14–21. [Google Scholar] [PubMed]
- Bottone, E.J. Yersinia enterocolitica: Overview and Epidemiologic Correlates. Microbes Infect. 1999, 1, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Skorek, K.; Raczkowska, A.; Dudek, B.; Miętka, K.; Guz-Regner, K.; Pawlak, A.; Klausa, E.; Bugla-Płoskońska, G.; Brzostek, K. Regulatory Protein OmpR Influences the Serum Resistance of Yersinia Enterocolitica O:9 by Modifying the Structure of the Outer Membrane. PLoS ONE 2013, 8, e79525. [Google Scholar] [CrossRef]
- Platt-Samoraj, A.; Syczyło, K.; Szczerba-Turek, A.; Bancerz-Kisiel, A.; Jabłoński, A.; Łabuć, S.; Pajdak, J.; Oshakbaeva, N.; Szweda, W. Presence of ail and ystB Genes in Yersinia enterocolitica Biotype 1A Isolates from Game Animals in Poland. Vet. J. 2017, 221, 11–13. [Google Scholar] [CrossRef]
- Joutsen, S.; Johansson, P.; Laukkanen-Ninios, R.; Björkroth, J.; Fredriksson-Ahomaa, M. Two Copies of the ail Gene Found in Yersinia enterocolitica and Yersinia kristensenii. Vet. Microbiol. 2020, 247, 108798. [Google Scholar] [CrossRef] [PubMed]
- Sihvonen, L.M.; Hallanvuo, S.; Haukka, K.; Skurnik, M.; Siitonen, A. The ail Gene Is Present in Some Yersinia enterocolitica Biotype 1A Strains. Foodborne Pathog. Dis. 2011, 8, 455–457. [Google Scholar] [CrossRef]
- Kraushaar, B.; Dieckmann, R.; Wittwer, M.; Knabner, D.; Konietzny, A.; Mäde, D.; Strauch, E. Characterization of a Yersinia enterocolitica Biotype 1A Strain Harbouring an ail Gene. J. Appl. Microbiol. 2011, 111, 997–1005. [Google Scholar] [CrossRef]
- Platt-Samoraj, A. Toxigenic Properties of Yersinia enterocolitica Biotype 1A. Toxins 2022, 14, 118. [Google Scholar] [CrossRef]
- Batzilla, J.; Heesemann, J.; Rakin, A. The Pathogenic Potential of Yersinia Enterocolitica 1A. Int. J. Med. Microbiol. 2011, 301, 556–561. [Google Scholar] [CrossRef]
- Aplin, K.; Pitt, T.; Allen, J.; Roy, A.; Tidey, K.; Ball, J.; McDonald, C.P. Extending the 30-minute Rule for Red Cell Units—Investigation of the Bacterial Risk of 60-minute Exposures to Ambient Temperature. Vox Sang. 2019, 114, 189–197. [Google Scholar] [CrossRef]
- Ramirez-Arcos, S.; Mastronardi, C.; Perkins, H.; Kou, Y.; Turner, T.; Mastronardi, E.; Hansen, A.; Yi, Q.; McLaughlin, N.; Kahwash, E.; et al. Evaluating the 4-hour and 30-minute Rules: Effects of Room Temperature Exposure on Red Blood Cell Quality and Bacterial Growth. Transfusion 2013, 53, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Gravemann, U.; Handke, W.; Schulze, T.J.; Seltsam, A. Growth and Distribution of Bacteria in Contaminated Whole Blood and Derived Blood Components. Transfus. Med. Hemother. 2024, 51, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Bhagat, N.; Virdi, J.S. Distribution of Virulence-Associated Genes in Yersinia enterocolitica Biovar 1A Correlates with Clonal Groups and Not the Source of Isolation. FEMS Microbiol. Lett. 2007, 266, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Bhagat, N.; Virdi, J.S. The Enigma of Yersinia enterocolitica Biovar 1A. Crit. Rev. Microbiol. 2011, 37, 25–39. [Google Scholar] [CrossRef]
- Tennant, S.M.; Grant, T.H.; Robins-Browne, R.M. Pathogenicity of Yersinia enterocolitica Biotype 1A. FEMS Immunol. Med. Microbiol. 2003, 38, 127–137. [Google Scholar] [CrossRef]
- Morka, K.; Bystroń, J.; Bania, J.; Korzeniowska-Kowal, A.; Korzekwa, K.; Guz-Regner, K.; Bugla-Płoskońska, G. Identification of Yersinia Enterocolitica Isolates from Humans, Pigs and Wild Boars by MALDI TOF MS. BMC Microbiol. 2018, 18, 86. [Google Scholar] [CrossRef]
- Wannet, W.J.B.; Reessink, M.; Brunings, H.A.; Maas, H.M.E. Detection of Pathogenic Yersinia enterocolitica by a Rapid and Sensitive Duplex PCR Assay. J. Clin. Microbiol. 2001, 39, 4483–4486. [Google Scholar] [CrossRef] [PubMed]
- Bancerz-Kisiel, A.; Szczerba-Turek, A.; Platt-Samoraj, A.; Socha, P.; Szweda, W. Bioserotypes and Virulence Markers of Y. Enterocolitica Strains Isolated from Roe Deer (Capreolus capreolus) and Red Deer (Cervus elaphus). Pol. J. Vet. Sci. 2014, 17, 315–319. [Google Scholar] [CrossRef]
- Macori, G.; Romano, A.; Adriano, D.; Razzuoli, E.; Bianchi, D.M.; Gallina, S.; Bellio, A.; Decastelli, L. Draft Genome Sequences of Four Yersinia enterocolitica Strains, Isolated from Wild Ungulate Carcasses. Genome Announc. 2017, 5, e00192-17. [Google Scholar] [CrossRef]
- Mikheenko, A.; Prjibelski, A.; Saveliev, V.; Antipov, D.; Gurevich, A. Versatile Genome Assembly Evaluation with QUAST-LG. Bioinformatics 2018, 34, i142–i150. [Google Scholar] [CrossRef]
- Jolley, K.A.; Maiden, M.C. BIGSdb: Scalable Analysis of Bacterial Genome Variation at the Population Level. BMC Bioinform. 2010, 11, 595. [Google Scholar] [CrossRef] [PubMed]
- Savin, C.; Criscuolo, A.; Guglielmini, J.; Le Guern, A.-S.; Carniel, E.; Pizarro-Cerdá, J.; Brisse, S. Genus-Wide Yersinia Core-Genome Multilocus Sequence Typing for Species Identification and Strain Characterization. Microb. Genom. 2019, 5, 301. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, M.; Mailund, T.; Pedersen, C.N.S. Rapid Neighbour-Joining. In Algorithms in Bioinformatics, Proceedings of the 8th International Workshop, WABI 2008, Karlsruhe, Germany, 15–19 September 2008; Springer: Berlin/Heidelberg, Germany, 2008; Volume 5251, pp. 113–123. [Google Scholar] [CrossRef]
- Hadfield, J.; Croucher, N.J.; Goater, R.J.; Abudahab, K.; Aanensen, D.M.; Harris, S.R. Phandango: An Interactive Viewer for Bacterial Population Genomics. Bioinformatics 2018, 34, 292–293. [Google Scholar] [CrossRef]
- Doerr, P., Dr. (Ed.) Guide to the Preparation, Use and Quality Assurance of Blood Components; European Committee (Partial Agreement) on Blood Transfusion (CD-P-TS). 21. wyd; European Directorate for the Quality of Medicines & HealthCare (EDQM) Council of Europe: Strasbourg, France, 2023. [Google Scholar]
- Miętka, K.; Brzostek, K.; Guz-Regner, K.; Bugla-Płoskońska, G. The Mechanisms of Complement Activation in Normal Bovine Serum and Normal Horse Serum against Yersinia Enterocolitica O:9 Strains with Different Outer Membrane Proteins Content. Pol. J. Vet. Sci. 2016, 19, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Neubauer, H.; Hensel, A.; Aleksic, S.; Meyer, H. Identification of Yersinia enterocolitica within the genus Yersinia. Syst. Appl. Microbiol. 2000, 23, 58–62. [Google Scholar] [CrossRef]
- Gierczyński, R. Evaluation of the usefulness of selected virulence markers for identification of virulent Yersinia enterocolitica strains. II. Genotypic markers associated with the pYV plasmid. Med. Dosw. Mikrobiol. 2000, 52, 35–49. [Google Scholar]
- Platt-Samoraj, A.; Ugorski, M.; Szweda, W.; Szczerba-Turek, A.; Wojciech, K.; Procajło, Z. Analysis of the presence of ail, ystA and ystB genes in Yersinia enterocolitica strains isolated from aborting sows and aborted fetuses. J. Vet. Med. B Infect. Dis. Vet. Public Health 2006, 53, 341–346. [Google Scholar] [CrossRef]
- Momtaz, H.; Davood Rahimian, M.; Safarpoor Dehkordi, F. Identification and characterization of Yersinia enterocolitica isolated from raw chicken meat based on molecular and biological techniques. J. Appl. Poul. Res. 2013, 22, 137–145. [Google Scholar] [CrossRef]
- Bancerz-Kisiel, A.; Szczerba-Turek, A.; Platt-Samoraj, A.; Szweda, W. Distribution of the ymoA and ystA genes and enterotoxins yst production by Yersinia enterocolitica strains isolated from humans and pigs. Pol. J. Vet. Sci. 2012, 15, 609–614. [Google Scholar] [CrossRef]
- Zacharczuk, K. Investigation of molecular virulence factors of Yersinia enterocolitica 1B/08 human clinical isolates collected in Poland in 2009. Med. Dosw. Mikrobiol. 2013, 65, 233–243. [Google Scholar]
- Sharma, S.; Mittal, S.; Mallik, S.; Virdi, J.S. Molecular characterization of β-lactamase genes blaA and blaB of Yersinia enterocolitica biovar 1A. FEMS Microbiol. Lett. 2006, 257, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Thisted Lambertz, S.; Danielsson-Tham, M.L. Identification and characterization of pathogenic Yersinia enterocolitica isolates by PCR and pulsed-field gel electrophoresis. Appl. Environ. Microbiol. 2005, 71, 3674–3681. [Google Scholar] [CrossRef] [PubMed]
- Gierczyński, R.; Jagielski, M.; Rastawicki, W. Evaluation of usefulness for selected virulence markers for identifying pathogenic Yersinia enterocolitica strains, I.V. Genes myfA and ureC. Med. Dosw. Mikrobiol. 2002, 54, 347–355. [Google Scholar] [PubMed]

| Days/Isolate | 0 | 3 | 7 | 14 | 21 | 28 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 3d, human, 4/O:3 | 3.50 × 101 | 3.12 × 101 | 1.76 × 102 | 2.01 × 102 | 1.11 × 104 | 1.91 × 104 | 1.21 × 104 | 1.76 × 104 | 2.50 × 104 | 1.19 × 104 | 2.50 × 105 | 4.81 × 104 |
| 58d, human, 1B/O:8 | 2.00 × 101 | 1.00 × 101 | 2.42 × 102 | 3.97 × 102 | 1.40 × 103 | 2.15 × 103 | 8.27 × 104 | 5.85 × 104 | 3.03 × 106 | 2.16 × 106 | 2.61 × 108 | 1.32 × 108 |
| 90z, pig, 4/O:3 | 2.53 × 101 | 2.57 × 101 | 3.77 × 101 | 1.97 × 101 | 1.88 × 102 | 1.59 × 101 | 4.22 × 103 | 4.65 × 102 | 2.21 × 104 | 9.54 × 102 | 6.05 × 105 | 2.94 × 105 |
| 176z, pig, 4/O:3 | 4.89 × 101 | 2.17 × 101 | 1.98 × 102 | 2.15 × 102 | 1.07 × 103 | 1.29 × 103 | 5.11 × 103 | 2.71 × 103 | 3.79 × 104 | 1.75 × 104 | 1.98 × 105 | 8.91 × 104 |
| 209z, pig, 1A | 5.68 × 101 | 2.01 × 101 | 4.01 × 102 | 2.91 × 102 | 7.27 × 104 | 1.25 × 105 | 1.97 × 106 | 2.98 × 106 | 2.71 × 107 | 1.77 × 107 | 2.15 × 108 | 2.69 × 107 |
| 186dz, wild boar, 1A | 7.00 × 101 | 7.94 × 101 | 9.83 × 101 | 9.09 × 101 | 1.17 × 103 | 1.01 × 103 | 7.13 × 105 | 9.07 × 105 | 6.55 × 106 | 2.49 × 106 | 2.67 × 108 | 8.42 × 107 |
| 205dz, wild boar, 1A | 5.67 × 101 | 4.17 × 101 | 4.26 × 102 | 6.70 × 102 | 4.42 × 104 | 7.34 × 104 | 1.45 × 106 | 2.13 × 106 | 1.49 × 107 | 3.20 × 106 | 4.47 × 108 | 2.52 × 108 |
| 28s, roe deer, 1A | 4.67 × 101 | 1.26 × 101 | 1.41 × 102 | 1.58 × 102 | 1.12 × 104 | 1.89 × 104 | 8.10 × 104 | 1.02 × 105 | 2.04 × 106 | 1.03 × 106 | 3.41 × 106 | 8.02 × 105 |
| Ye9N, reference strain 2/O:9 | 4.00 × 101 | 3.97 × 101 | 3.79 × 102 | 6.07 × 102 | 2.14 × 104 | 3.56 × 104 | 4.91 × 105 | 7.96 × 105 | 9.22 × 108 | 1.20 × 109 | 5.69 × 108 | 8.78 × 108 |
| Ye8, reference strain 1B/O:8 | 3.00 × 101 | 2.00 × 101 | 1.43 × 102 | 1.16 × 102 | 8.49 × 103 | 1.09 × 104 | 7.76 × 107 | 1.30 × 108 | 1.24 × 109 | 1.14 × 109 | 1.20 × 109 | 1.01 × 109 |
| Isolate/ Time [min] | Before RBC | After RBC | Before RBC | After RBC | Before RBC | After RBC | Before RBC | After RBC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 15 | 30 | 60 | |||||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| 3d | 5.07 × 105 | 3.33 × 105 | 7.60 × 105 | 1.16 × 106 | 2.77 × 105 | 1.55 × 105 | 1.18 × 105 | 1.30 × 105 | 2.31 × 105 | 1.05 × 105 | 2.89 × 103 | 1.65 × 103 | 2.14 × 105 | 9.83 × 104 | 1.10 × 102 | 1.65 × 102 |
| 58d | 5.15 × 107 | 1.18 × 105 | 1.09 × 108 | 6.41 × 107 | 3.95 × 106 | 2.52 × 106 | 4.29 × 104 | 3.19 × 103 | 2.21 × 106 | 1.79 × 106 | 9.50 × 103 | 7.47 × 103 | 9.13 × 105 | 1.07 × 106 | 3.33 × 104 | 2.82 × 104 |
| 90z | 7.58 × 104 | 8.08 × 103 | 4.44 × 105 | 7.59 × 105 | 3.79 × 104 | 2.41 × 104 | 1.49 × 104 | 1.10 × 104 | 0 | 0 | 3.00 × 103 | 2.18 × 103 | 0 | 0 | 3.67 × 101 | 5.51 × 101 |
| 176z | 5.26 × 105 | 9.97 × 104 | 3.71 × 105 | 2.53 × 105 | 2.80 × 105 | 2.16 × 104 | 8.15 × 104 | 5.96 × 104 | 2.59 × 105 | 1.96 × 104 | 8.60 × 103 | 1.27 × 104 | 2.24 × 104 | 7.37 × 103 | 6.07 × 102 | 1.03 × 103 |
| 209z | 2.48 × 107 | 1.06 × 107 | 2.23 × 107 | 3.68 × 107 | 3.33 × 102 | 5.77 × 102 | 6.67 × 102 | 1.15 × 103 | 0 | 0 | 6.67 × 102 | 1.15 × 103 | 0 | 0 | 3.77 × 102 | 5.41 × 102 |
| 186dz | 3.36 × 107 | 1.59 × 107 | 3.28 × 107 | 6.10 × 106 | 1.17 × 103 | 1.26 × 103 | 3.54 × 107 | 1.37 × 107 | 0 | 0 | 2.48 × 107 | 2.31 × 107 | 0 | 0 | 3.24 × 106 | 3.02 × 106 |
| 205dz | 2.22 × 107 | 1.69 × 107 | 6.43 × 107 | 1.24 × 107 | 6.67 × 102 | 1.15 × 103 | 2.09 × 104 | 1.78 × 104 | 0 | 0 | 2.86 × 104 | 2.49 × 104 | 0 | 0 | 4.70 × 103 | 3.75 × 103 |
| 28s | 1.98 × 107 | 1.66 × 107 | 1.31 × 106 | 1.35 × 106 | 0 | 0 | 6.67 × 102 | 5.77 × 102 | 0 | 0 | 3.33 × 102 | 5.77 × 102 | 0 | 0 | 1.33 × 101 | 2.31 × 101 |
| Ye8 | 1.55 × 107 | 1.25 × 107 | 1.62 × 107 | 1.39 × 107 | 9.36 × 106 | 7.48 × 106 | 2.34 × 103 | 4.74 × 102 | 1.73 × 105 | 9.96 × 104 | 2.00 × 103 | 1.41 × 103 | 4.52 × 104 | 2.29 × 104 | 3.68 × 103 | 9.55 × 102 |
| Ye9N | 1.35 × 107 | 8.03 × 106 | 1.84 × 107 | 2.42 × 107 | 3.09 × 104 | 1.61 × 104 | 1.79 × 104 | 1.39 × 104 | 1.56 × 103 | 5.10 × 102 | 4.67 × 103 | 4.73 × 103 | 0 | 0 | 1.10 × 103 | 8.06 × 102 |
| Y. enterocolitica | Origin | Bioserotype | Virulence-Associated Genes Content |
|---|---|---|---|
| 3d | Human feces | 4/O:3 | yadA, ail, inv, yst, ystA, ystC, myfA, myfB, ureC, ymoA, rfbC, blaA, blaB |
| 58d | 1B/O:8 | yadA, ail, inv, yst, ystA, ystC, myfA, myfB, ureC, ymoA, rfbC, fepD, blaA, blaB | |
| 90z | Pigs | 4/O:3 | yadA, ail, inv, yst, ystA, ystC, myfA, myfB, ureC, ymoA, rfbC, blaA, blaB |
| 176z | 4/O:3 | yadA, ail, inv, yst, ystA, ystC, myfA, myfB, ureC, ymoA, rfbC, hreP, sat, blaA, blaB | |
| 209z | 1A/O:9 | inv, ystB, ureC, ymoA, fepD | |
| 186dz | Wild boars | 1A/NT | inv, ureC, ymoA, fepA, fepD |
| 205dz | 1A/NT | ail, inv, ystB, myfA, ureC, ymoA, hreP, fepD | |
| 28s | Roe deer | 1A/NT | inv, ystB, ureC, ymoA, tccC, hreP, fepA, fepD |
| Ye9N | Reference | 2/O:9 | yadA, virF, ail, inv, yst, ystA, ystC, myfA, myfB, ureC, ymoA, tccC, hreP, fepD, blaA, blaB |
| Ye8 | 1B/O:8 | yadA, ail, inv, yst, ystA, ystC, myfA, myfB, ureC, ymoA, irp1, irp2, fyuA, chiY, Yts1M, hreP, fepD, blaB, ysrS |
| No. | Strain | Blood Group | Characteristics of RBC Concentrate Units | Volume [mL] | Age of RBC Concentrate on the Infecting Day |
|---|---|---|---|---|---|
| 1 | 3d | 0 RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.2 J | 50 | 31 |
| 2 | 0 RhD+ | SAGM/450 mL/2-6C, irradiated, leukoreduced, 0.4 J | 84 | 7 | |
| 3 | B RhD+ | SAGM/450 mL/2-6C, irradiated, leukoreduced, 0.4 J | 100 | 9 | |
| 4 | 58d | A RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.2 J | 50 | 27 |
| 5 | A RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 93 | 25 | |
| 6 | A RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 103 | 13 | |
| 7 | 90z | A RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 128 | 25 |
| 8 | A RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 139 | 21 | |
| 9 | 0 RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 119 | 12 | |
| 10 | 176dz | 0 RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.8 J | 167 | 22 |
| 11 | B RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 100 | 12 | |
| 12 | B RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 105 | 21 | |
| 13 | 209z | A RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 65 | 23 |
| 14 | A RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 93 | 25 | |
| 15 | 0 RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 116 | 28 | |
| 16 | 186dz | B RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 86 | 18 |
| 17 | A RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 142 | 19 | |
| 18 | AB RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 100 | 22 | |
| 19 | 205dz | 0 RhD+ | SAGM/450 mL/2-6C leukoreduced, 0.6 J | 140 | 25 |
| 20 | A RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 82 | 25 | |
| 21 | 0 RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 101 | 27 | |
| 22 | 28s | B RhD+ | SAGM/450mL/2-6C, leukoreduced, 0.6 J | 154 | 29 |
| 23 | A RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 134 | 15 | |
| 24 | A RhD- | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 135 | 20 | |
| 25 | Ye9N | B RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 71 | 23 |
| 26 | 0 RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 150 | 23 | |
| 27 | 0 RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.6 J | 150 | 22 | |
| 28 | Ye8 | 0 RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 88 | 29 |
| 29 | B RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 65 | 18 | |
| 30 | B RhD+ | SAGM/450 mL/2-6C, leukoreduced, 0.4 J | 118 | 21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morka, K.; Banaszkiewicz, S.; Korkus, J.; Bania, J.; Bystroń, J.; Bugla-Płoskońska, G.; Stanek, M.; Sokalska, U.; Szymczyk-Nużka, M.; Sheppard, S.K.; et al. Biotype Determines Survival of Yersinia enterocolitica in Red Blood Cell Concentrates. Int. J. Mol. Sci. 2025, 26, 5775. https://doi.org/10.3390/ijms26125775
Morka K, Banaszkiewicz S, Korkus J, Bania J, Bystroń J, Bugla-Płoskońska G, Stanek M, Sokalska U, Szymczyk-Nużka M, Sheppard SK, et al. Biotype Determines Survival of Yersinia enterocolitica in Red Blood Cell Concentrates. International Journal of Molecular Sciences. 2025; 26(12):5775. https://doi.org/10.3390/ijms26125775
Chicago/Turabian StyleMorka, Katarzyna, Sylwia Banaszkiewicz, Jakub Korkus, Jacek Bania, Jarosław Bystroń, Gabriela Bugla-Płoskońska, Marta Stanek, Urszula Sokalska, Małgorzata Szymczyk-Nużka, Samuel K. Sheppard, and et al. 2025. "Biotype Determines Survival of Yersinia enterocolitica in Red Blood Cell Concentrates" International Journal of Molecular Sciences 26, no. 12: 5775. https://doi.org/10.3390/ijms26125775
APA StyleMorka, K., Banaszkiewicz, S., Korkus, J., Bania, J., Bystroń, J., Bugla-Płoskońska, G., Stanek, M., Sokalska, U., Szymczyk-Nużka, M., Sheppard, S. K., & Pascoe, B. (2025). Biotype Determines Survival of Yersinia enterocolitica in Red Blood Cell Concentrates. International Journal of Molecular Sciences, 26(12), 5775. https://doi.org/10.3390/ijms26125775







