A High-Yield Recombinant Inactivated Whole-Virion Nasal Influenza A(H1N1)pdm09 Virus Vaccine with an Attenuated PB2 Gene
Abstract
1. Introduction
2. Results
2.1. Generation and Comparison of the Replication Efficiency of PB2-Substituted Recombinant Pandemic 2009 (pdm09) H1N1 Viruses
2.2. Low Mammalian Virulence of PB2-Substituted High-Growth pdm09 Vaccine Strains
2.3. Quantitative Comparison of HA Antigen of PB2-Substituted High-Growth pdm09 Vaccine Strains
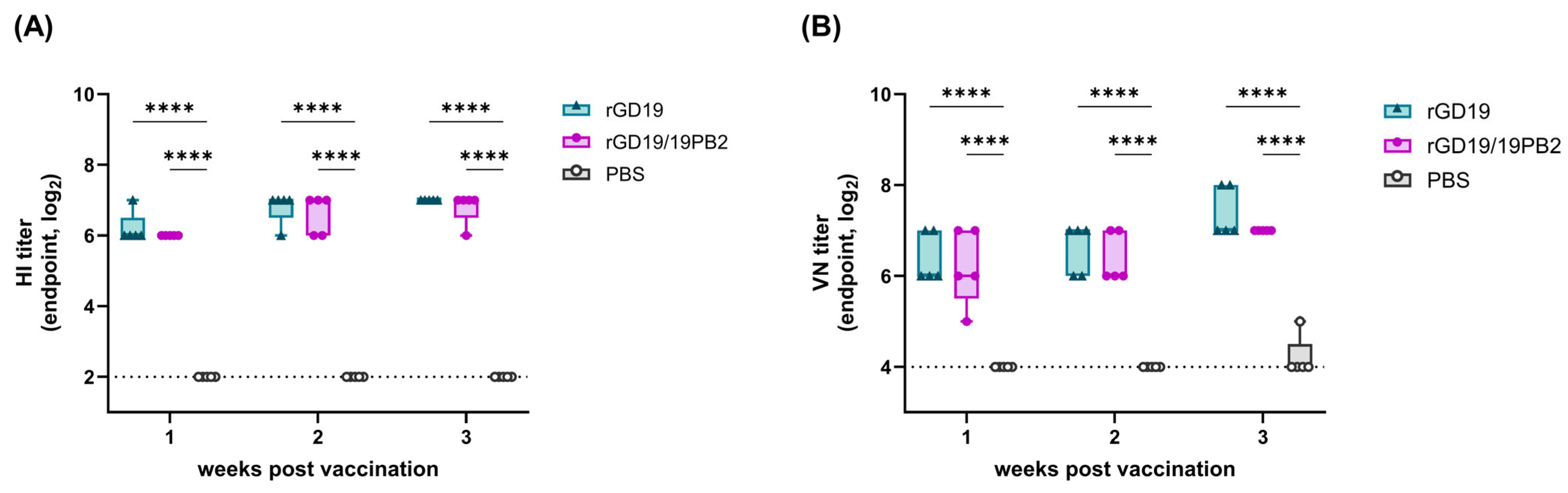
2.4. Comparable Serological Immune Response After the Intramuscular Administration of BEI-Inactivated rGD19/19PB2 Vaccine
2.5. Enhanced Humoral Immune Responses After the Intranasal Administration of BEI-Inactivated rGD19/19PB2 Vaccine
2.6. Homo- and Heterosubtypic Protection Efficacy of the Intranasally Administered BEI-Inactivated rGD19/19PB2 Vaccine
2.7. Evaluation of Cellular Immune Responses
3. Discussion
4. Materials and Methods
4.1. Eggs, Cells, and Viruses
4.2. Plasmids, Cloning, and Site-Directed Mutagenesis
4.3. Mini-Genome Assay
4.4. Generation and Titration of the Recombinant H1N1 Viruses
4.5. RT-PCR, Sequencing, and Sequence Analysis
4.6. Growth Kinetics of the Recombinant H1N1 Viruses in Mammalian Cells
4.7. Analysis of HA Yield
4.8. Inactivated Vaccine Preparation
4.9. Animal Experiments
4.10. Hemagglutinin Inhibition (HI) Test
4.11. Viral Neutralization (VN) Test
4.12. Antigen-Specific Enzyme-Linked Immunosorbent Assay (ELISA)
4.13. Flow Cytometric Analysis
4.14. Statistical Analysis
4.15. Ethical Statement
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ECE | Embryonated chicken egg |
| Pdm09 | Pandemic 2009 |
| BEI | Binary ethylenimine |
| EID | Egg infectious dose |
| TCID | Tissue culture infectious dose |
| GD19 | A/Guandong-Maonan/SWL1536/2019 |
References
- Cheung, T.K.; Poon, L.L. Biology of influenza a virus. Ann. N. Y. Acad. Sci. 2007, 1102, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Paules, C.I.; Sullivan, S.G.; Subbarao, K.; Fauci, A.S. Chasing Seasonal Influenza—The Need for a Universal Influenza Vaccine. N. Engl. J. Med. 2018, 378, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, A.; Abdelwhab, E.M.; Mettenleiter, T.C.; Pleschka, S. Zoonotic Potential of Influenza A Viruses: A Comprehensive Overview. Viruses 2018, 10, 497. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harding, A.T.; Heaton, N.S. Efforts to Improve the Seasonal Influenza Vaccine. Vaccines 2018, 6, 19. [Google Scholar] [CrossRef]
- (CDC) USCfDCaP. How Influenza (Flu) Vaccines Are Made 2022. Available online: https://www.cdc.gov/flu/vaccine-process/index.html (accessed on 16 January 2025).
- Robertson, J.S.; Nicolson, C.; Harvey, R.; Johnson, R.; Major, D.; Guilfoyle, K.; Roseby, S.; Newman, R.; Collin, R.; Wallis, C.; et al. The development of vaccine viruses against pandemic A(H1N1) influenza. Vaccine 2011, 29, 1836–1843. [Google Scholar] [CrossRef]
- (CDC) USCfDCaP. 2023–2024 Influenza Season Vaccine Supply 2024 [Updated 17 September 2024]. Available online: https://www.cdc.gov/flu/hcp/vaccine-supply/2023-2024.html (accessed on 24 January 2025).
- (CDC) USCfDCaP. Vaccine Supply & Distribution Information for Health Care Providers 2024 [updated 13 November 2024]. Available online: https://www.cdc.gov/flu/hcp/vaccine-supply/?CDC_AAref_Val=https://www.cdc.gov/flu/prevent/vaccine-supply-distribution.htm (accessed on 24 January 2025).
- (CDC) USCfDCaP. Key Facts About Seasonal Flu Vaccine 2024 [Updated Janurary 2025]. Available online: https://www.cdc.gov/flu/vaccines/keyfacts.html (accessed on 24 January 2025).
- Sparrow, E.; Wood, J.G.; Chadwick, C.; Newall, A.T.; Torvaldsen, S.; Moen, A.; Torelli, G. Global production capacity of seasonal and pandemic influenza vaccines in 2019. Vaccine 2021, 39, 512–520. [Google Scholar] [CrossRef]
- Carbone, V.; Schneider, E.K.; Rockman, S.; Baker, M.; Huang, J.X.; Ong, C.; Cooper, M.A.; Yuriev, E.; Li, J.; Velkov, T. Molecular Characterisation of the Haemagglutinin Glycan-Binding Specificity of Egg-Adapted Vaccine Strains of the Pandemic 2009 H1N1 Swine Influenza A Virus. Molecules 2015, 20, 10415–10434. [Google Scholar] [CrossRef]
- Garretson, T.A.; Petrie, J.G.; Martin, E.T.; Monto, A.S.; Hensley, S.E. Identification of human vaccinees that possess antibodies targeting the egg-adapted hemagglutinin receptor binding site of an H1N1 influenza vaccine strain. Vaccine 2018, 36, 4095–4101. [Google Scholar] [CrossRef]
- Takemae, N.; Ruttanapumma, R.; Parchariyanon, S.; Yoneyama, S.; Hayashi, T.; Hiramatsu, H.; Sriwilaijaroen, N.; Uchida, Y.; Kondo, S.; Yagi, H.; et al. Alterations in receptor-binding properties of swine influenza viruses of the H1 subtype after isolation in embryonated chicken eggs. J. Gen. Virol. 2010, 91, 938–948. [Google Scholar] [CrossRef]
- Cobbin, J.C.A.; Verity, E.E.; Gilbertson, B.P.; Rockman, S.P.; Brown, L.E. The Source of the PB1 Gene in Influenza Vaccine Reassortants Selectively Alters the Hemagglutinin Content of the Resulting Seed Virus. J. Virol. 2013, 87, 5577–5585. [Google Scholar] [CrossRef]
- Hussain, S.; Turnbull, M.L.; Pinto, R.M.; McCauley, J.W.; Engelhardt, O.G.; Digard, P. Segment 2 from influenza A(H1N1) 2009 pandemic viruses confers temperature-sensitive haemagglutinin yield on candidate vaccine virus growth in eggs that can be epistatically complemented by PB2 701D. J. Gen. Virol. 2019, 100, 1079–1092. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Wan, H.; Li, X.; Rakic Martinez, M.; Klenow, L.; Gao, Y.; Ye, Z.; Daniels, R. Balancing the influenza neuraminidase and hemagglutinin responses by exchanging the vaccine virus backbone. PLOS Pathog. 2021, 17, e1009171. [Google Scholar] [CrossRef] [PubMed]
- Almeida, F.; Santos, L.A.; Trigueiro-Louro, J.M.; Rebelo-de-Andrade, H. Optimization of A(H1N1)pdm09 vaccine seed viruses: The source of PB1 and HA vRNA as a major determinant for antigen yield. Virus Res. 2022, 315, 198795. [Google Scholar] [CrossRef]
- Guan, L.; Ping, J.; Lopes, T.J.S.; Fan, S.; Presler, R.; Neumann, G.; Kawaoka, Y. Development of an Enhanced High-Yield Influenza Vaccine Backbone in Embryonated Chicken Eggs. Vaccines 2023, 11, 1364. [Google Scholar] [CrossRef]
- Lee, C.-Y.; An, S.-H.; Choi, J.-G.; Lee, Y.-J.; Kim, J.-H.; Kwon, H.-J. Rank orders of mammalian pathogenicity-related PB2 mutations of avian influenza A viruses. Sci. Rep. 2020, 10, 5359. [Google Scholar] [CrossRef]
- An, S.-H.; Son, S.-E.; Song, J.-H.; Hong, S.-M.; Lee, C.-Y.; Lee, N.-H.; Jeong, Y.-J.; Choi, J.-G.; Lee, Y.-J.; Kang, H.-M.; et al. Selection of an Optimal Recombinant Egyptian H9N2 Avian Influenza Vaccine Strain for Poultry with High Antigenicity and Safety. Vaccines 2022, 10, 162. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.-W.; Lee, C.-Y.; Kim, I.-h.; Choi, J.-G.; Lee, Y.-J.; Yuk, S.-S.; Lee, J.-H.; Song, C.-S.; Kim, J.-H.; Kwon, H.-J. Optimized clade 2.3. 2.1 c H5N1 recombinant-vaccine strains against highly pathogenic avian influenza. J. Vet. Sci. 2017, 18, 299–306. [Google Scholar] [CrossRef]
- An, S.-H.; Hong, S.-M.; Song, J.-H.; Son, S.-E.; Lee, C.-Y.; Choi, K.-S.; Kwon, H.-J. Engineering an Optimal Y280-Lineage H9N2 Vaccine Strain by Tuning PB2 Activity. Int. J. Mol. Sci. 2023, 24, 8840. [Google Scholar] [CrossRef]
- Smith, G.J.D.; Vijaykrishna, D.; Bahl, J.; Lycett, S.J.; Worobey, M.; Pybus, O.G.; Ma, S.K.; Cheung, C.L.; Raghwani, J.; Bhatt, S.; et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 2009, 459, 1122–1125. [Google Scholar] [CrossRef]
- Garten, R.J.; Davis, C.T.; Russell, C.A.; Shu, B.; Lindstrom, S.; Balish, A.; Sessions, W.M.; Xu, X.; Skepner, E.; Deyde, V.; et al. Antigenic and Genetic Characteristics of Swine-Origin 2009 A(H1N1) Influenza Viruses Circulating in Humans. Science 2009, 325, 197–201. [Google Scholar] [CrossRef]
- Takada, A.; Matsushita, S.; Ninomiya, A.; Kawaoka, Y.; Kida, H. Intranasal immunization with formalin-inactivated virus vaccine induces a broad spectrum of heterosubtypic immunity against influenza A virus infection in mice. Vaccine 2003, 21, 3212–3218. [Google Scholar] [CrossRef] [PubMed]
- Ainai, A.; Suzuki, T.; Tamura S-i Hasegawa, H. Intranasal Administration of Whole Inactivated Influenza Virus Vaccine as a Promising Influenza Vaccine Candidate. Viral Immunol. 2017, 30, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, P.K.; Dowse, G.K.; Effler, P.V.; Carcione, D.; Blyth, C.C.; Richmond, P.C.; Geelhoed, G.C.; Mascaro, F.; Scully, M.; Weeramanthri, T.S. Epidemiological study of severe febrile reactions in young children in Western Australia caused by a 2010 trivalent inactivated influenza vaccine. BMJ Open 2011, 1, e000016. [Google Scholar] [CrossRef] [PubMed]
- Rockman, S.; Becher, D.; Dyson, A.; Koernig, S.; Morelli, A.B.; Barnden, M.; Camuglia, S.; Soupourmas, P.; Pearse, M.; Maraskovsky, E. Role of viral RNA and lipid in the adverse events associated with the 2010 Southern Hemisphere trivalent influenza vaccine. Vaccine 2014, 32, 3869–3876. [Google Scholar] [CrossRef]
- Uhlendorff, J.; Matrosovich, T.; Klenk, H.-D.; Matrosovich, M. Functional significance of the hemadsorption activity of influenza virus neuraminidase and its alteration in pandemic viruses. Arch. Virol. 2009, 154, 945–957. [Google Scholar] [CrossRef]
- Lin, Y.P.; Gregory, V.; Collins, P.; Kloess, J.; Wharton, S.; Cattle, N.; Lackenby, A.; Daniels, R.; Hay, A. Neuraminidase Receptor Binding Variants of Human Influenza A(H3N2) Viruses Resulting from Substitution of Aspartic Acid 151 in the Catalytic Site: A Role in Virus Attachment? J. Virol. 2010, 84, 6769–6781. [Google Scholar] [CrossRef]
- Trifkovic, S.; Gilbertson, B.; Fairmaid, E.; Cobbin, J.; Rockman, S.; Brown, L.E. Gene Segment Interactions Can Drive the Emergence of Dominant Yet Suboptimal Gene Constellations During Influenza Virus Reassortment. Front. Microbiol. 2021, 12, 3152. [Google Scholar] [CrossRef]
- Wagner, R.; Matrosovich, M.; Klenk, H.-D. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 2002, 12, 159–166. [Google Scholar] [CrossRef]
- Bialas, K.M.; Bussey, K.A.; Stone, R.L.; Takimoto, T. Specific Nucleoprotein Residues Affect Influenza Virus Morphology. J. Virol. 2014, 88, 2227–2234. [Google Scholar] [CrossRef]
- Peterl, S.; Lahr, C.M.; Schneider, C.N.; Meyer, J.; Podlipensky, X.; Lechner, V.; Villiou, M.; Eis, L.; Klein, S.; Funaya, C.; et al. Morphology-dependent entry kinetics and spread of influenza A virus. bioRxiv 2024. [Google Scholar] [CrossRef]
- Stöhr, K.; Bucher, D.; Colgate, T.; Wood, J. Influenza Virus Surveillance, Vaccine Strain Selection, and Manufacture. In Influenza Virus: Methods and Protocols; Kawaoka, Y., Neumann, G., Eds.; Humana Press: Totowa, NJ, USA, 2012; pp. 147–162. [Google Scholar]
- (CHMP) CfMPfHu. Guideline on Influenza Vaccines—Quality Module; EMA/CHMP/BWP/310834/2012 Rev.1; European Medicines Agency: Amsterdam, The Netherlands, 2017.
- Miyaki, C.; Quintilio, W.; Miyaji, E.N.; Botosso, V.F.; Kubrusly, F.S.; Santos, F.L.; Iourtov, D.; Higashi, H.G.; Raw, I. Production of H5N1 (NIBRG-14) inactivated whole virus and split virion influenza vaccines and analysis of immunogenicity in mice using different adjuvant formulations. Vaccine 2010, 28, 2505–2509. [Google Scholar] [CrossRef] [PubMed]
- Mehle, A.; Doudna, J.A. Adaptive strategies of the influenza virus polymerase for replication in humans. Proc. Natl. Acad. Sci. USA 2009, 106, 21312–21316. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Massin, P.; van der Werf, S.; Naffakh, N. Residue 627 of PB2 Is a Determinant of Cold Sensitivity in RNA Replication of Avian Influenza Viruses. J. Virol. 2001, 75, 5398–5404. [Google Scholar] [CrossRef]
- Liu, Q.; Qiao, C.; Marjuki, H.; Bawa, B.; Ma, J.; Guillossou, S.; Webby, R.J.; Richt, J.A.; Ma, W. Combination of PB2 271A and SR Polymorphism at Positions 590/591 Is Critical for Viral Replication and Virulence of Swine Influenza Virus in Cultured Cells and In Vivo. J. Virol. 2012, 86, 1233–1237. [Google Scholar] [CrossRef] [PubMed]
- Bhoye, D.; Behera, A.K.; Cherian, S.S. A molecular modelling approach to understand the effect of co-evolutionary mutations (V344M, I354L) identified in the PB2 subunit of influenza A 2009 pandemic H1N1 virus on m7GTP ligand binding. J. Gen. Virol. 2016, 97, 1785–1796. [Google Scholar] [CrossRef]
- Samantaray, M.; Pushan, S.S.; Rajagopalan, M.; Ramaswamy, A. Structural dynamics of the RNA dependent RNA polymerase of H1N1 strain affecting humans: A bioinformatics approach. J. Biomol. Struct. Dyn. 2024, 42, 10876–10889. [Google Scholar] [CrossRef]
- Sang, X.; Wang, A.; Ding, J.; Kong, H.; Gao, X.; Li, L.; Chai, T.; Li, Y.; Zhang, K.; Wang, C.; et al. Adaptation of H9N2 AIV in guinea pigs enables efficient transmission by direct contact and inefficient transmission by respiratory droplets. Sci. Rep. 2015, 5, 15928. [Google Scholar] [CrossRef] [PubMed]
- Sutton, T.C.; Finch, C.; Shao, H.; Angel, M.; Chen, H.; Capua, I.; Cattoli, G.; Monne, I.; Perez, D.R. Airborne Transmission of Highly Pathogenic H7N1 Influenza Virus in Ferrets. J. Virol. 2014, 88, 6623–6635. [Google Scholar] [CrossRef]
- Lubna, S.; Bandyopadhyay, D. Consortium of ‘consistent amino acid substitutions’ on influenza A (H1N1) viral proteins emerged at specific stages of viral infection: A big data analysis. J. Biomol. Struct. Dyn. 2024, 1–14. [Google Scholar] [CrossRef]
- Ilyushina, N.A.; Khalenkov, A.M.; Seiler, J.P.; Forrest, H.L.; Bovin, N.V.; Marjuki, H.; Barman, S.; Webster, R.G.; Webby, R.J. Adaptation of pandemic H1N1 influenza viruses in mice. J. Virol. 2010, 84, 8607–8616. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sun, Y.; Xu, Q.; Shen, Y.; Liu, L.; Wei, K.; Sun, H.; Pu, J.; Chang, K.C.; Liu, J. Naturally occurring mutations in the PA gene are key contributors to increased virulence of pandemic H1N1/09 influenza virus in mice. J. Virol. 2014, 88, 4600–4604. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kistner, O.; Crowe, B.A.; Wodal, W.; Kerschbaum, A.; Savidis-Dacho, H.; Sabarth, N.; Falkner, F.G.; Mayerhofer, I.; Mundt, W.; Reiter, M.; et al. A Whole Virus Pandemic Influenza H1N1 Vaccine Is Highly Immunogenic and Protective in Active Immunization and Passive Protection Mouse Models. PLoS ONE 2010, 5, e9349. [Google Scholar] [CrossRef] [PubMed]
- Al-Khayatt, R.; Jennings, R.; Potter, C.W. Interpretation of responses and protective levels of antibody against attenuated influenza A viruses using single radial haemolysis. J. Hyg. 1984, 93, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Hobson, D.; Curry, R.L.; Beare, A.S.; Ward-Gardner, A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. Epidemiol. Infect. 1972, 70, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Luytjes, W.; Enouf, V.; Schipper, M.; Gijzen, K.; Liu, W.M.; van der Lubben, M.; Meijer, A.; van der Werf, S.; Soethout, E.C. HI responses induced by seasonal influenza vaccination are associated with clinical protection and with seroprotection against non-homologous strains. Vaccine 2012, 30, 5262–5269. [Google Scholar] [CrossRef]
- Pedersen, G.K.; Wørzner, K.; Andersen, P.; Christensen, D. Vaccine Adjuvants Differentially Affect Kinetics of Antibody and Germinal Center Responses. Front. Immunol. 2020, 11, 579761. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boyden, A.W.; Legge, K.L.; Waldschmidt, T.J. Pulmonary Infection with Influenza A Virus Induces Site-Specific Germinal Center and T Follicular Helper Cell Responses. PLoS ONE 2012, 7, e40733. [Google Scholar] [CrossRef]
- Vono, M.; Taccone, M.; Caccin, P.; Gallotta, M.; Donvito, G.; Falzoni, S.; Palmieri, E.; Pallaoro, M.; Rappuoli, R.; Di Virgilio, F.; et al. The adjuvant MF59 induces ATP release from muscle that potentiates response to vaccination. Proc. Natl. Acad. Sci. USA 2013, 110, 21095–21100. [Google Scholar] [CrossRef]
- Ruan, B.-Y.; Yao, Y.; Wang, S.-Y.; Gong, X.-Q.; Liu, X.-M.; Wang, Q.; Yu, L.-X.; Zhu, S.-Q.; Wang, J.; Shan, T.-L.; et al. Protective efficacy of a bivalent inactivated reassortant H1N1 influenza virus vaccine against European avian-like and classical swine influenza H1N1 viruses in mice. Vet. Microbiol. 2020, 246, 108724. [Google Scholar] [CrossRef]
- Budimir, N.; de Haan, A.; Meijerhof, T.; Gostick, E.; Price, D.A.; Huckriede, A.; Wilschut, J. Heterosubtypic cross-protection induced by whole inactivated influenza virus vaccine in mice: Influence of the route of vaccine administration. Influenza Other Respir. Viruses 2013, 7, 1202–1209. [Google Scholar] [CrossRef]
- Renegar, K.B.; Small, P.A.; Boykins, L.G., Jr.; Wright, P.F. Role of IgA versus IgG in the Control of Influenza Viral Infection in the Murine Respiratory Tract1. J. Immunol. 2004, 173, 1978–1986. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kawaguchi, A.; Ainai, A.; Tamura, S.-I.; Ito, R.; Multihartina, P.; Setiawaty, V.; Pangesti, K.N.A.; Odagiri, T.; Tashiro, M.; et al. Relationship of the quaternary structure of human secretory IgA to neutralization of influenza virus. Proc. Natl. Acad. Sci. USA 2015, 112, 7809–7814. [Google Scholar] [CrossRef]
- Woof, J.M.; Russell, M.W. Structure and function relationships in IgA. Mucosal Immunol. 2011, 4, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Muramatsu, M.; Yoshida, R.; Yokoyama, A.; Miyamoto, H.; Kajihara, M.; Maruyama, J.; Nao, N.; Manzoor, R.; Takada, A. Comparison of Antiviral Activity between IgA and IgG Specific to Influenza Virus Hemagglutinin: Increased Potential of IgA for Heterosubtypic Immunity. PLoS ONE 2014, 9, e85582. [Google Scholar] [CrossRef] [PubMed]
- Gianchecchi, E.; Manenti, A.; Kistner, O.; Trombetta, C.; Manini, I.; Montomoli, E. How to assess the effectiveness of nasal influenza vaccines? Role and measurement of sIgA in mucosal secretions. Influenza Other Respir. Viruses 2019, 13, 429–437. [Google Scholar] [CrossRef]
- Mazanec, M.B.; Coudret, C.L.; Fletcher, D.R. Intracellular neutralization of influenza virus by immunoglobulin A anti-hemagglutinin monoclonal antibodies. J. Virol. 1995, 69, 1339–1343. [Google Scholar] [CrossRef]
- Li, Y.; Jin, L.; Chen, T. The Effects of Secretory IgA in the Mucosal Immune System. Biomed. Res. Int. 2020, 2020, 2032057. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Okuya, K.; Yoshida, R.; Manzoor, R.; Saito, S.; Suzuki, T.; Sasaki, M.; Saito, T.; Kida, Y.; Mori-Kajihara, A.; Kondoh, T.; et al. Potential Role of Nonneutralizing IgA Antibodies in Cross-Protective Immunity against Influenza A Viruses of Multiple Hemagglutinin Subtypes. J. Virol. 2020, 94. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Delrue, I.; Verzele, D.; Madder, A.; Nauwynck, H.J. Inactivated virus vaccines from chemistry to prophylaxis: Merits, risks and challenges. Expert Rev. Vaccines 2012, 11, 695–719. [Google Scholar] [CrossRef]
- Altenburg, A.F.; Rimmelzwaan, G.F.; de Vries, R.D. Virus-specific T cells as correlate of (cross-)protective immunity against influenza. Vaccine 2015, 33, 500–506. [Google Scholar] [CrossRef]
- World Health Organization. Recommended Composition of Influenza Virus Vaccines for Use in the 2020–2021 Northern Hemisphere Influenza Season; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Hoffmann, E.; Neumann, G.; Kawaoka, Y.; Hobom, G.; Webster, R.G. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 2000, 97, 6108–6113. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-Y.; An, S.-H.; Kim, I.; Go, D.-M.; Kim, D.-Y.; Choi, J.-G.; Lee, Y.-J.; Kim, J.-H.; Kwon, H.-J. Prerequisites for the acquisition of mammalian pathogenicity by influenza A virus with a prototypic avian PB2 gene. Sci. Rep. 2017, 7, 10205. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine 2002, 20, 3165–3170. [Google Scholar] [CrossRef]
- Zhou, B.; Donnelly, M.E.; Scholes, D.T.; George, K.S.; Hatta, M.; Kawaoka, Y.; Wentworth, D.E. Single-Reaction Genomic Amplification Accelerates Sequencing and Vaccine Production for Classical and Swine Origin Human Influenza A Viruses. J. Virol. 2009, 83, 10309–10313. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.A.; Russo, R.C.; Thurston, R.V. Trimmed Spearman–Karber method for estimating median lethal concentrations in bioassays. Environ. Sci. Technol. 1977, 11, 714–719. [Google Scholar] [CrossRef]
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef]
- World Health Organization. WHO Manual on Animal Influenza Diagnosis and Surveillance; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, S.-E.; Song, J.-H.; Kim, H.-W.; An, S.-H.; Kim, S.-J.; Lee, C.-Y.; Kwon, H.-J.; Choi, K.-S. A High-Yield Recombinant Inactivated Whole-Virion Nasal Influenza A(H1N1)pdm09 Virus Vaccine with an Attenuated PB2 Gene. Int. J. Mol. Sci. 2025, 26, 5489. https://doi.org/10.3390/ijms26125489
Son S-E, Song J-H, Kim H-W, An S-H, Kim S-J, Lee C-Y, Kwon H-J, Choi K-S. A High-Yield Recombinant Inactivated Whole-Virion Nasal Influenza A(H1N1)pdm09 Virus Vaccine with an Attenuated PB2 Gene. International Journal of Molecular Sciences. 2025; 26(12):5489. https://doi.org/10.3390/ijms26125489
Chicago/Turabian StyleSon, Seung-Eun, Jin-Ha Song, Ho-Won Kim, Se-Hee An, Seung-Ji Kim, Chung-Young Lee, Hyuk-Joon Kwon, and Kang-Seuk Choi. 2025. "A High-Yield Recombinant Inactivated Whole-Virion Nasal Influenza A(H1N1)pdm09 Virus Vaccine with an Attenuated PB2 Gene" International Journal of Molecular Sciences 26, no. 12: 5489. https://doi.org/10.3390/ijms26125489
APA StyleSon, S.-E., Song, J.-H., Kim, H.-W., An, S.-H., Kim, S.-J., Lee, C.-Y., Kwon, H.-J., & Choi, K.-S. (2025). A High-Yield Recombinant Inactivated Whole-Virion Nasal Influenza A(H1N1)pdm09 Virus Vaccine with an Attenuated PB2 Gene. International Journal of Molecular Sciences, 26(12), 5489. https://doi.org/10.3390/ijms26125489






