Regulation of STAT1 and STAT4 Expression by Growth Factor and Interferon Supplementation in Sjögren’s Syndrome Cell Culture Models
Abstract
1. Introduction
2. Results
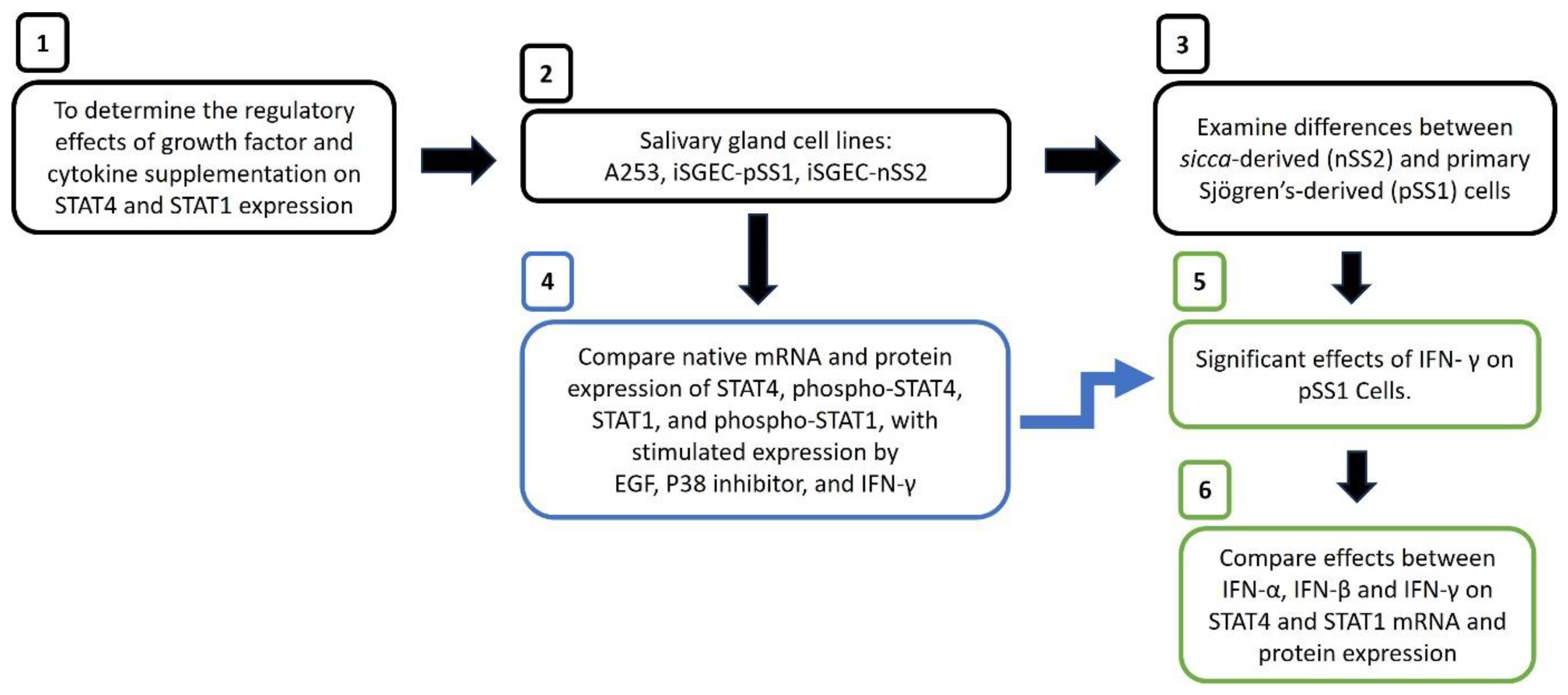
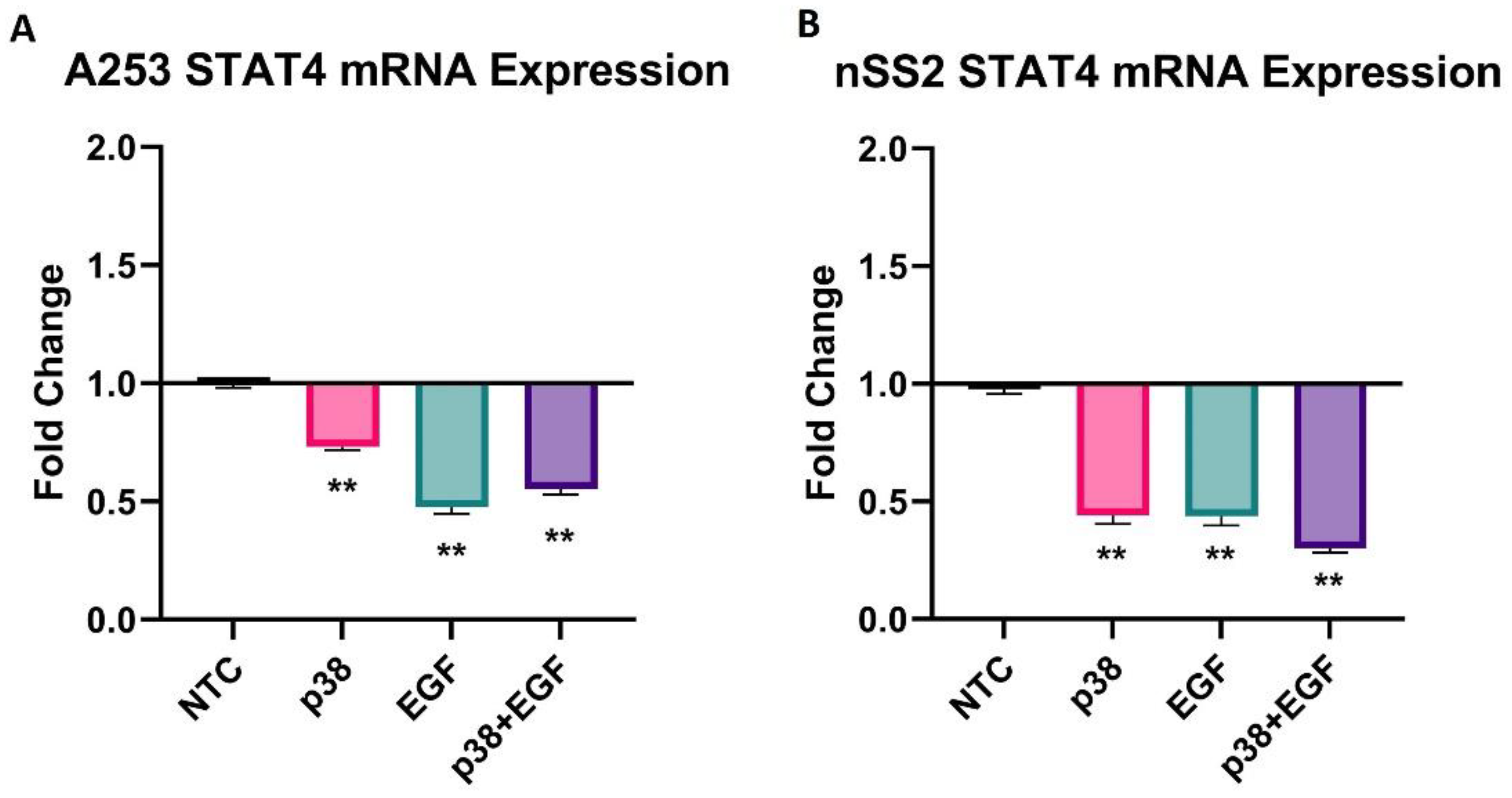
2.1. Regulation of STAT4 Expression by EGF and p38 Inhibitor
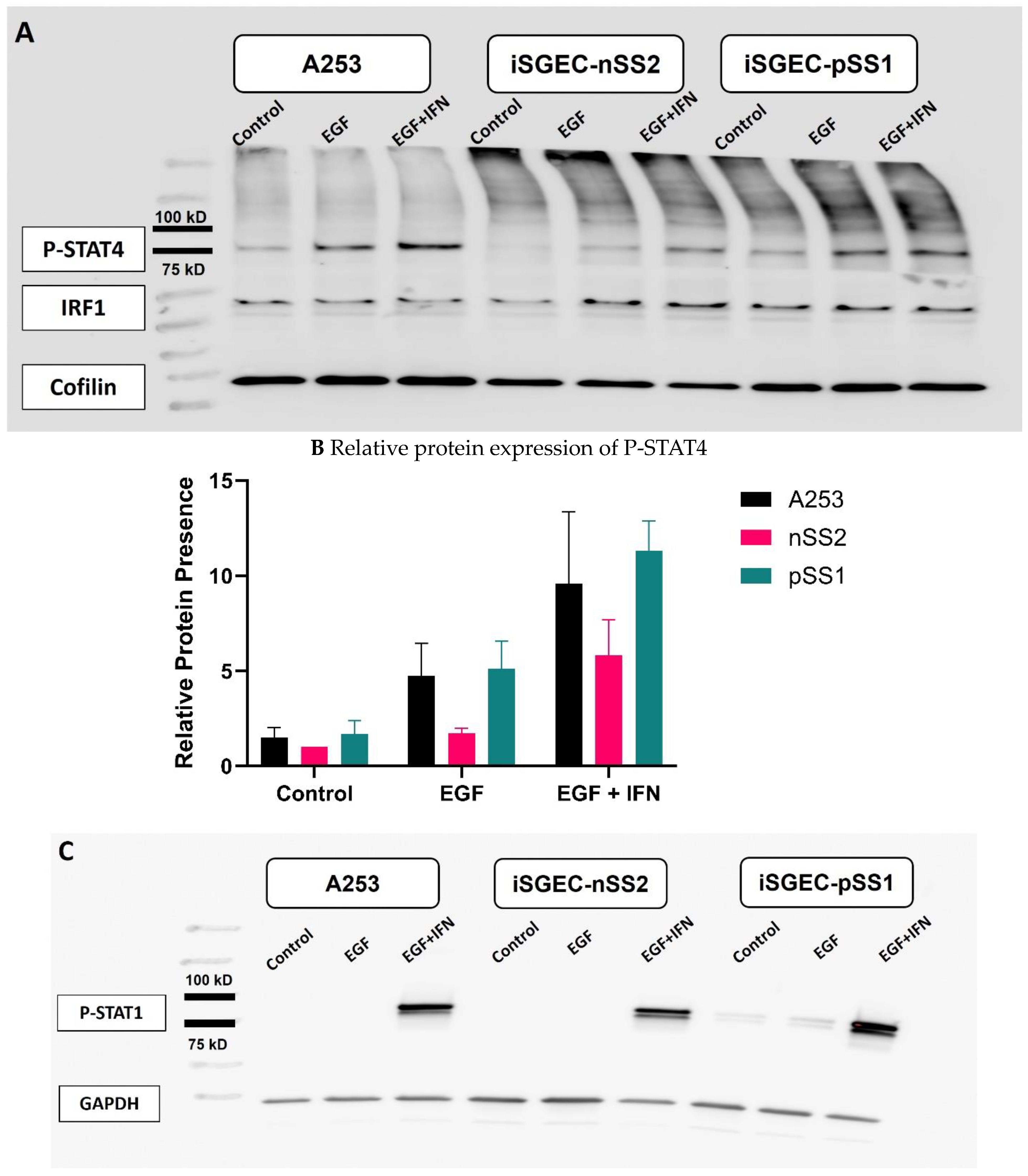
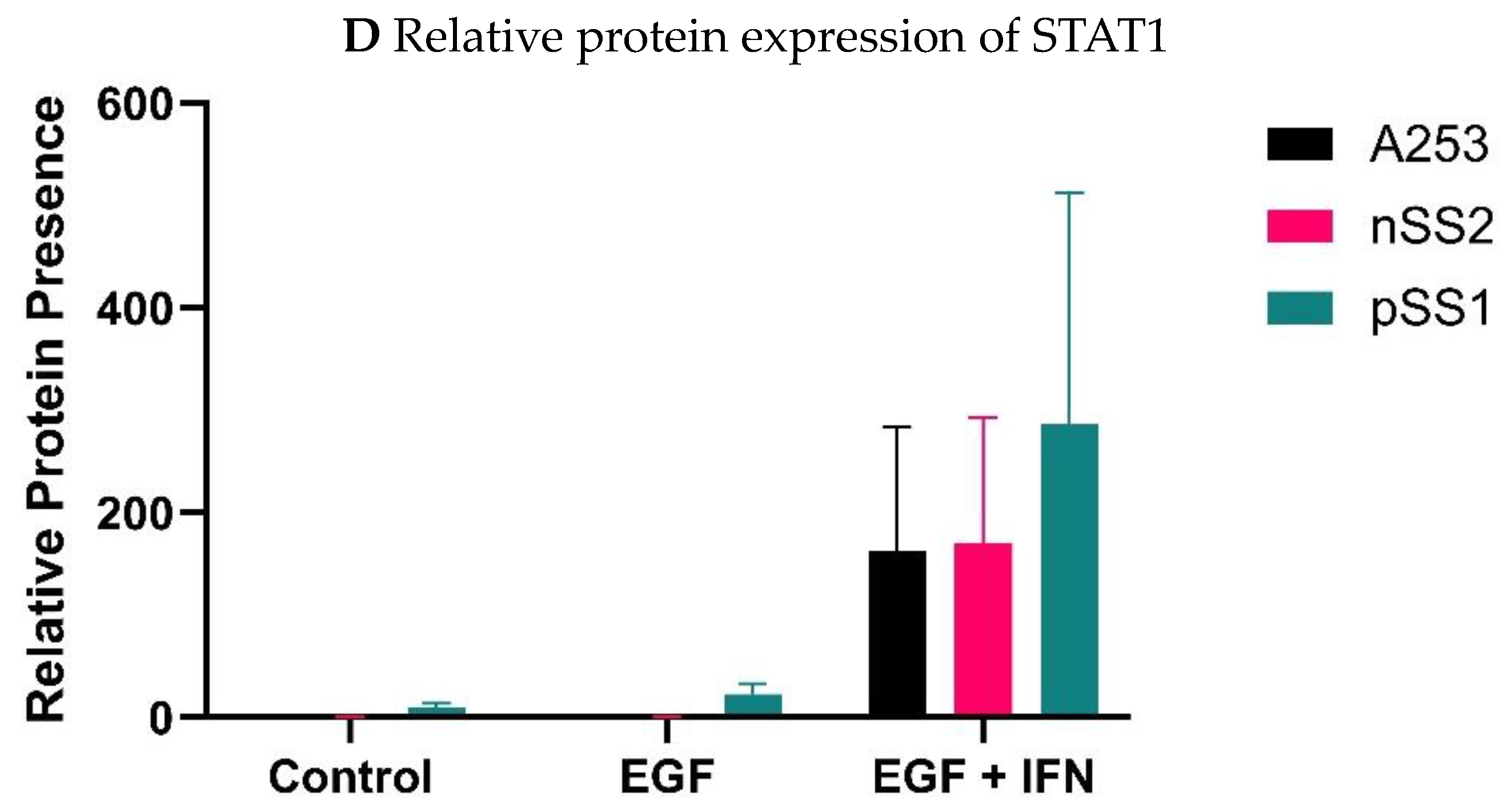
2.2. Effects of EGF and IFN-γ on Protein Expression of Phospho-STAT4 and Phospho-STAT1
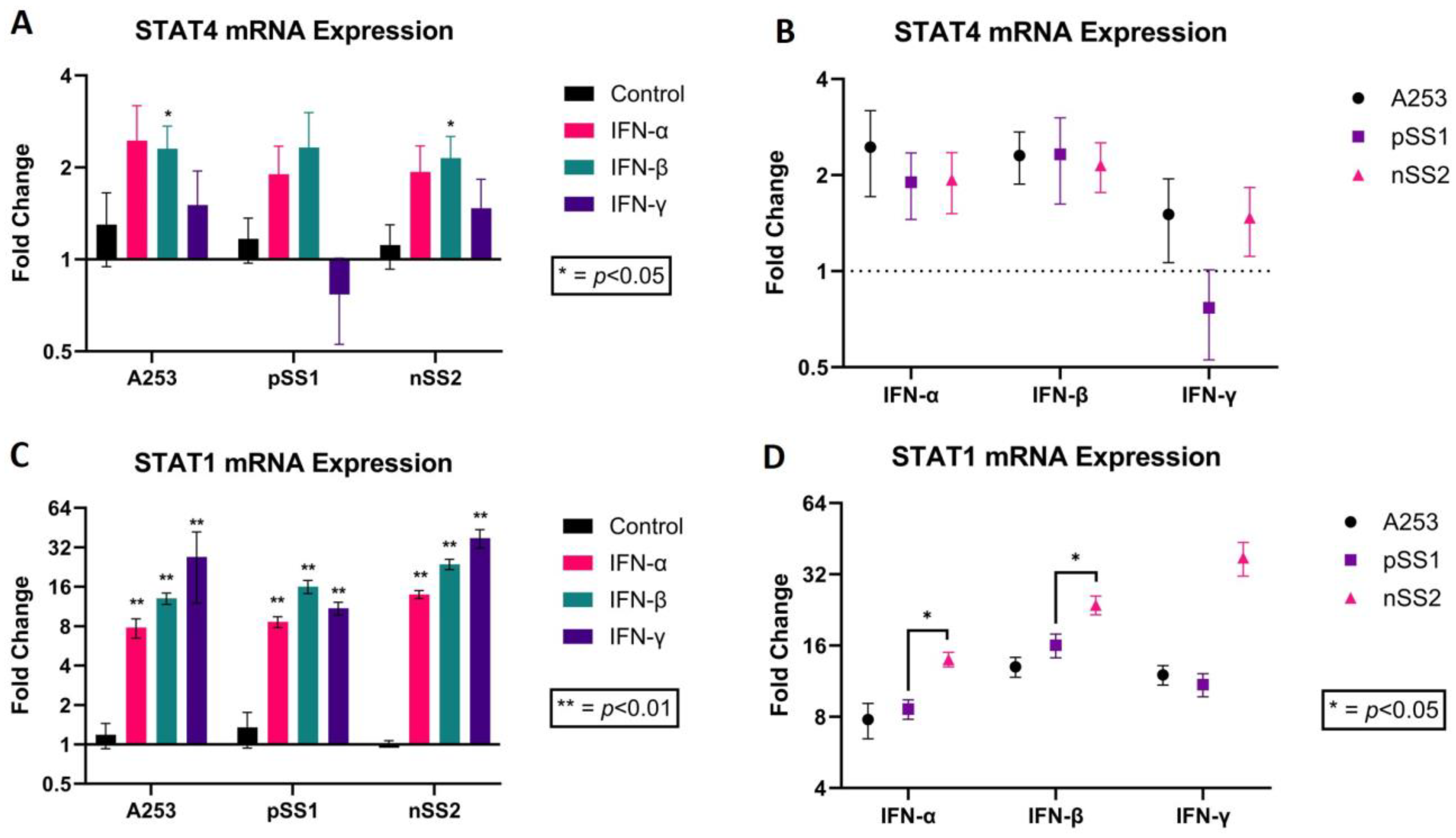
2.3. Regulation of STAT1 and STAT4 mRNA and Active Protein Expression by Interferons α, β and γ
3. Discussion
3.1. STAT4 mRNA Expression Downregulation by EGF and p38 Inhibitor
3.2. Effects of EGF and IFN-γ on Protein Expression of Phospho-STAT4 and Phospho-STAT1
3.3. Regulation of STAT1 and STAT4 mRNA and Active Protein Expression by Interferons α, β and γ
3.4. Limitations
4. Materials and Methods
4.1. Reagents
4.2. Cell Culture
4.3. Quantitative Real-Time RT-PCR
4.4. Western Blot
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parisis, D.; Chivasso, C.; Perret, J.; Soyfoo, M.S.; Delporte, C. Current State of Knowledge on Primary Sjögren’s Syndrome, an Autoimmune Exocrinopathy. J. Clin. Med. 2020, 9, 2299. [Google Scholar] [CrossRef]
- Ogawa, Y.; Takeuchi, T.; Tsubota, K. Autoimmune Epithelitis and Chronic Inflammation in Sjögren’s Syndrome-Related Dry Eye Disease. Int. J. Mol. Sci. 2021, 22, 11820. [Google Scholar] [CrossRef] [PubMed]
- Selmi, C.; Gershwin, M.E. Chronic Autoimmune Epithelitis in Sjögren’s Syndrome and Primary Biliary Cholangitis: A Comprehensive Review. Rheumatol. Ther. 2017, 4, 263–279. [Google Scholar] [CrossRef] [PubMed]
- Manganelli, P.; Fietta, P. Apoptosis and Sjögren syndrome. Semin. Arthritis Rheum. 2003, 33, 49–65. [Google Scholar] [CrossRef] [PubMed]
- Ping, L.; Ogawa, N.; Zhang, Y.; Sugai, S.; Masaki, Y.; Weiguo, X. p38 mitogen-activated protein kinase and nuclear factor-κB facilitate CD40-mediated salivary epithelial cell death. J. Rheumatol. 2012, 39, 1256–1264. [Google Scholar] [CrossRef]
- Visconti, R.; Gadina, M.; Chiariello, M.; Chen, E.H.; Stancato, L.F.; Gutkind, J.S.; O’Shea, J.J. Importance of the MKK6/p38 pathway for interleukin-12–induced STAT4 serine phosphorylation and transcriptional activity. Blood 2000, 96, 1844–1852. [Google Scholar] [CrossRef]
- Korman, B.D.; Kastner, D.L.; Gregersen, P.K.; Remmers, E.F. STAT4: Genetics, mechanisms, and implications for autoimmunity. Curr. Allergy Asthma Rep. 2008, 8, 398–403. [Google Scholar] [CrossRef]
- Deng, Y.; Tsao, B.P. Genetic susceptibility to systemic lupus erythematosus in the genomic era. Nat. Rev. Rheumatol. 2010, 6, 683–692. [Google Scholar] [CrossRef]
- Hu, Q.; Bian, Q.; Rong, D.; Wang, L.; Song, J.; Huang, H.S.; Zeng, J.; Mei, J.; Wang, P.Y. JAK/STAT pathway: Extracellular signals, diseases, immunity, and therapeutic regimens. Front. Bioeng. Biotechnol. 2023, 11, 1110765. [Google Scholar] [CrossRef]
- Gestermann, N.; Mekinian, A.; Comets, E.; Loiseau, P.; Puechal, X.; Hachulla, E.; Gottenberg, J.E.; Mariette, X.; Miceli-Richard, C. STAT4 is a confirmed genetic risk factor for Sjögren’s syndrome and could be involved in type 1 interferon pathway signaling. Genes Immun. 2010, 11, 432–438. [Google Scholar] [CrossRef]
- Awasthi, N.; Liongue, C.; Ward, A.C. STAT proteins: A kaleidoscope of canonical and non-canonical functions in immunity and cancer. J. Hematol. Oncol. 2021, 14, 198. [Google Scholar] [CrossRef]
- O’Shea, J.J.; Holland, S.M.; Staudt, L.M. JAKs and STATs in immunity, immunodeficiency, and cancer. N. Engl. J. Med. 2013, 368, 161–170. [Google Scholar] [CrossRef]
- Banerjee, S.; Biehl, A.; Gadina, M.; Hasni, S.; Schwartz, D.M. JAK-STAT Signaling as a Target for Inflammatory and Autoimmune Diseases: Current and Future Prospects. Drugs 2017, 77, 521–546. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Li, J.; Fu, M.; Zhao, X.; Wang, W. The JAK/STAT signaling pathway: From bench to clinic. Signal Transduct. Target. Ther. 2021, 6, 402. [Google Scholar] [CrossRef]
- Schwartz, D.M.; Kanno, Y.; Villarino, A.; Ward, M.; Gadina, M.; O’Shea, J.J. Erratum: JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat. Rev. Drug Discov. 2018, 17, 78. [Google Scholar] [CrossRef]
- Luo, K. Signaling Cross Talk between TGF-β/Smad and Other Signaling Pathways. Cold Spring Harb. Perspect. Biol. 2017, 9, a022137. [Google Scholar] [CrossRef]
- Azuma, N.; Katada, Y.; Kitano, S.; Nishioka, A.; Sekiguchi, M.; Kitano, M.; Hashimoto, N.; Matsui, K.; Iwasaki, T.; Sano, H. Salivary epidermal growth factor (EGF) in Sjögren’s syndrome: Association between salivary EGF levels and the severity of intraoral manifestations. Nihon Rinsho Meneki Gakkai Kaishi 2016, 39, 42–50. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sisto, M.; Lisi, S.; Lofrumento, D.D.; D’amore, M.; Frassanito, M.A.; Ribatti, D. Sjögren’s syndrome pathological neovascularization is regulated by VEGF-A-stimulated TACE-dependent crosstalk between VEGFR2 and NF-κB. Genes Immun. 2012, 13, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.Y.; Yuan, Y.R.; Kong, Y.L.; Zhang, T.; Liang, Y. Vascular Endothelial Growth Factor-A Is Associated with Platelets and Complement 4 in Patients with Primary Sjögren’s Syndrome. Ann. Clin. Lab. Sci. 2020, 50, 790–796. [Google Scholar] [PubMed]
- Bartoloni, E.; Baldini, C.; Schillaci, G.; Quartuccio, L.; Priori, R.; Carubbi, F.; Bini, V.; Alunno, A.; Bombardieri, S.; De Vita, S.; et al. Cardiovascular disease risk burden in primary Sjögren’s syndrome: Results of a population-based multicentre cohort study. J. Intern. Med. 2015, 278, 185–192. [Google Scholar] [CrossRef]
- Błochowiak, K.J.; Trzybulska, D.; Olewicz-Gawlik, A.; Sikora, J.J.; Nowak-Gabryel, M.; Kocięcki, J.; Witmanowski, H.; Sokalski, J. Levels of EGF and VEGF in patients with primary and secondary Sjögren’s syndrome. Adv. Clin. Exp. Med. 2018, 27, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Miklossy, G.; Hilliard, T.S.; Turkson, J. Therapeutic modulators of STAT signalling for human diseases. Nat. Reviews. Drug Discov. 2013, 12, 611–629. [Google Scholar] [CrossRef]
- George, G.; Shyni, G.L.; Abraham, B.; Nisha, P.; Raghu, K.G. Downregulation of TLR4/MyD88/p38MAPK and JAK/STAT pathway in RAW 264.7 cells by Alpinia galanga reveals its beneficial effects in inflammation. J. Ethnopharmacol. 2021, 275, 114132. [Google Scholar] [CrossRef]
- Thomas, C.; Couch, D.; Wang, B. p38-MAPK and JAK/STAT Pathway Inhibition Reduces Indoxyl Sulfate-Inducted Impairment of Human Edothelial Cells. Heart Lung Circ. 2022, 31, S313–S314. [Google Scholar] [CrossRef]
- Khatri, B.; Tessneer, K.L.; Rasmussen, A.; Aghakhanian, F.; Reksten, T.R.; Adler, A.; Alevizos, I.; Anaya, J.M.; Aqrawi, L.A.; Baecklund, E.; et al. Genome-wide association study identifies Sjögren’s risk loci with functional implications in immune and glandular cells. Nat. Commun. 2022, 13, 4287. [Google Scholar] [CrossRef] [PubMed]
- Gandolfo, S.; Ciccia, F. JAK/STAT Pathway Targeting in Primary Sjögren Syndrome. Rheumatol. Immunol. Res. 2022, 3, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Pertovaara, M.; Silvennoinen, O.; Isomäki, P. Cytokine-induced STAT1 activation is increased in patients with primary Sjögren’s syndrome. Clin. Immunol. 2016, 165, 60–67. [Google Scholar] [CrossRef]
- Colafrancesco, S.; Ciccacci, C.; Priori, R.; Latini, A.; Picarelli, G.; Arienzo, F.; Novelli, G.; Valesini, G.; Perricone, C.; Borgiani, P. STAT4, TRAF3IP2, IL10, and HCP5 Polymorphisms in Sjögren’s Syndrome: Association with Disease Susceptibility and Clinical Aspects. J. Immunol. Res. 2019, 2019, 7682827. [Google Scholar] [CrossRef]
- Rivière, E.; Pascaud, J.; Tchitchek, N.; Boudaoud, S.; Paoletti, A.; Ly, B.; Dupré, A.; Chen, H.; Thai, A.; Allaire, N.; et al. Salivary gland epithelial cells from patients with Sjögren’s syndrome induce B-lymphocyte survival and activation. Ann. Rheum. Dis. 2020, 79, 1468–1477. [Google Scholar] [CrossRef]
- Theander, E.; Jonsson, R.; Sjöström, B.; Brokstad, K.; Olsson, P.; Henriksson, G. Prediction of Sjögren’s Syndrome Years Before Diagnosis and Identification of Patients With Early Onset and Severe Disease Course by Autoantibody Profiling. Arthritis Rheumatol. 2015, 67, 2427–2436. [Google Scholar] [CrossRef]
- Del Papa, N.; Minniti, A.; Lorini, M.; Carbonelli, V.; Maglione, W.; Pignataro, F.; Montano, N.; Caporali, R.; Vitali, C. The Role of Interferons in the Pathogenesis of Sjögren’s Syndrome and Future Therapeutic Perspectives. Biomolecules 2021, 11, 251. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Kawakami, A.; Yamasaki, S.; Kawabe, Y.; Nakamura, T.; Eguchi, K. Expression of mitogen activated protein kinases in labial salivary glands of patients with Sjögren’s syndrome. Ann. Rheum. Dis. 1999, 58, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Cao, N.; Shi, H.; Chen, C.; Zheng, L.; Yu, C. Inhibition of the TLR9-dependent p38 MAPK signaling pathway improves the pathogenesis of primary Sjögren’s syndrome in the NOD/Ltj mouse. J. Biol. Regul. Homeost. Agents 2021, 35, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Zou, J.; He, L.; Zhang, Y. Dry eye management in a Sjögren’s syndrome mouse model by inhibition of p38-MAPK pathway. Diagn. Pathol. 2014, 9, 5. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mougeot, J.-L.C.; Thornburg, T.E.; Noll, B.D.; Brennan, M.T.; Mougeot, F.B. Regulation of STAT1 and STAT4 Expression by Growth Factor and Interferon Supplementation in Sjögren’s Syndrome Cell Culture Models. Int. J. Mol. Sci. 2024, 25, 3166. https://doi.org/10.3390/ijms25063166
Mougeot J-LC, Thornburg TE, Noll BD, Brennan MT, Mougeot FB. Regulation of STAT1 and STAT4 Expression by Growth Factor and Interferon Supplementation in Sjögren’s Syndrome Cell Culture Models. International Journal of Molecular Sciences. 2024; 25(6):3166. https://doi.org/10.3390/ijms25063166
Chicago/Turabian StyleMougeot, Jean-Luc C., Thomas E. Thornburg, Braxton D. Noll, Michael T. Brennan, and Farah Bahrani Mougeot. 2024. "Regulation of STAT1 and STAT4 Expression by Growth Factor and Interferon Supplementation in Sjögren’s Syndrome Cell Culture Models" International Journal of Molecular Sciences 25, no. 6: 3166. https://doi.org/10.3390/ijms25063166
APA StyleMougeot, J.-L. C., Thornburg, T. E., Noll, B. D., Brennan, M. T., & Mougeot, F. B. (2024). Regulation of STAT1 and STAT4 Expression by Growth Factor and Interferon Supplementation in Sjögren’s Syndrome Cell Culture Models. International Journal of Molecular Sciences, 25(6), 3166. https://doi.org/10.3390/ijms25063166






