Astrocyte–Neuron Interaction via the Glutamate–Glutamine Cycle and Its Dysfunction in Tau-Dependent Neurodegeneration
Abstract
1. Astrocyte–Neuron Crosstalk in Normal Brain Function
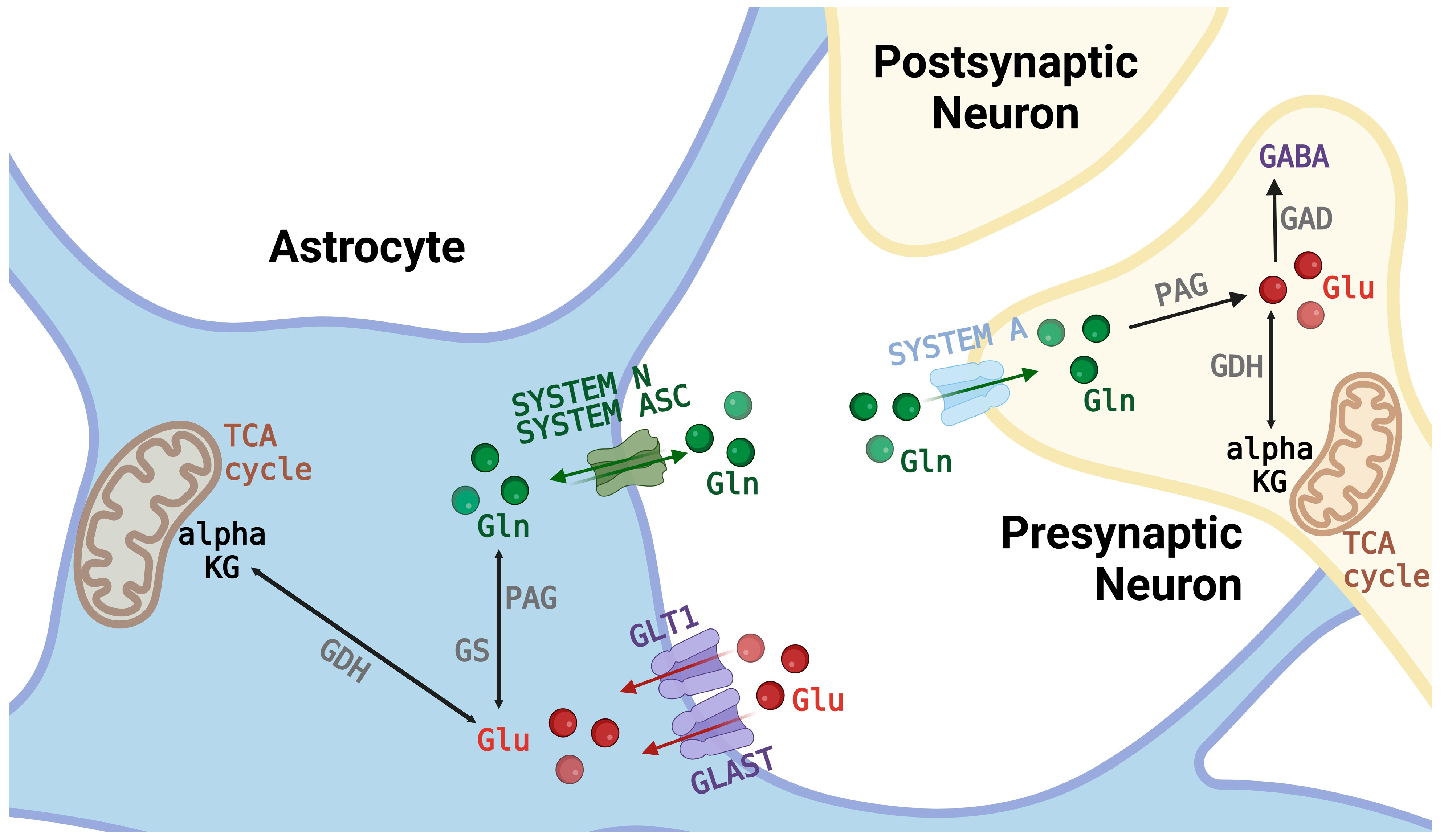
Significance of GGC Cycle
2. GGC-Involved Amino Acid Transporter Systems
2.1. Subfamily of Glutamate Transporters
2.2. Glutamine-Recognizing Systems and Carriers
3. Tau-Dependent Neurodegeneration
3.1. Tau: Its Biological Configurations and Involvement in Neurodegeneration
3.2. Contribution of the Glial Exosomal Pathway to Tauopathiespo
4. The Role of Glia in Neurodegenerative Disorders
4.1. Astrocyte and Neurodegeneration: An Overview
4.2. Significance of the Astrocyte–Microglia Network in Neurodegeneration and Neuroinflammation
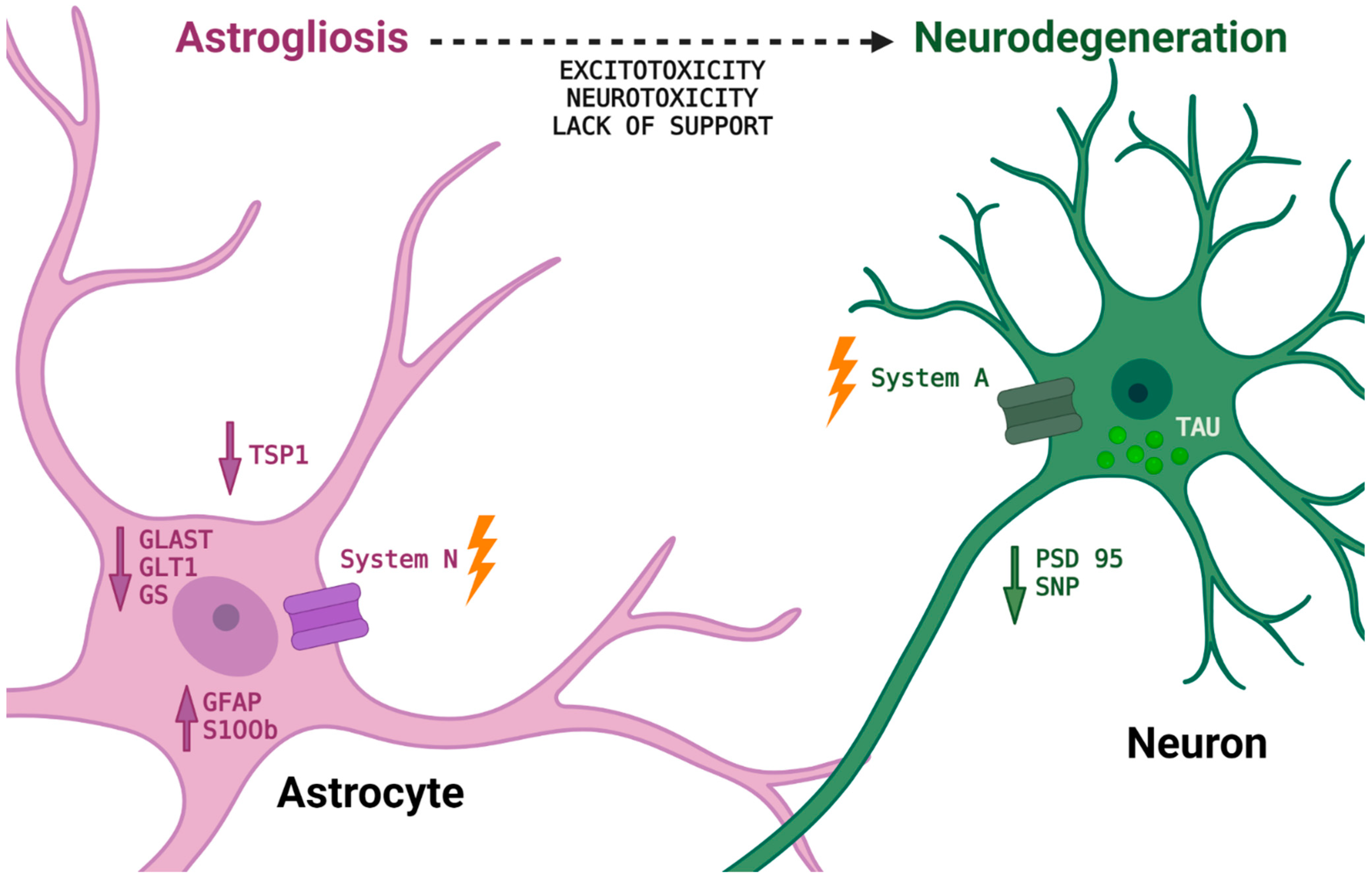
5. Astrocyte–Neuron Crosstalk in Tau-Dependent Neurodegeneration
6. Experimental Effects of Mutant Tau P301L: Reduction of Neuronal Survival by Affecting Astrocyte–Neuron Interactions and Disruption of Neuronal-Astrocytic Integrity via the GGC
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACM | astrocyte conditioned medium |
| AD | Alzheimer’s disease |
| AGD | argyrophilic grain disease |
| ARTAG | aging related Tau astrogliopathy |
| CBD | corticobasal degeneration |
| FTDP17 | frontotemporal dementia with parkinsonism linked to chromosome 17 |
| GAD | glutamate decarboxylase |
| GABA | γ-aminobutyric acid |
| GGC | glutamine-glutamate cycle |
| GGT | globular glial tauopathy |
| GLAST | glial high-affinity glutamate aspartate transporter |
| GLT1 | glial glutamate transporter |
| GS | glutamine synthetase |
| NFTs | neurofibrillary tangles |
| iPSCs | induced pluripotent stem cells |
| PSP | progressive supranuclear palsy |
| rtau | recombinant mutant tau |
| TSP1 | thrombospondin 1 |
References
- Ransom, B.; Behar, T.; Nedergaard, M. New Roles for Astrocytes (Stars at Last). Trends Neurosci. 2003, 26, 520–522. [Google Scholar] [CrossRef]
- Herculano-Houzel, S. The Glia/Neuron Ratio: How It Varies Uniformly across Brain Structures and Species and What That Means for Brain Physiology and Evolution. Glia 2014, 62, 1377–1391. [Google Scholar] [CrossRef]
- Verkhratsky, A.; Matteoli, M.; Parpura, V.; Mothet, J.; Zorec, R. Astrocytes as Secretory Cells of the Central Nervous System: Idiosyncrasies of Vesicular Secretion. EMBO J. 2016, 35, 239–257. [Google Scholar] [CrossRef] [PubMed]
- Sofroniew, M.V.; Vinters, H.V. Astrocytes: Biology and Pathology. Acta Neuropathol. 2010, 119, 7–35. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.; Ingram, E.; Takao, M.; Smith, M.J.; Jakes, R.; Virdee, K.; Yoshida, H.; Holzer, M.; Craxton, M.; Emson, P.C.; et al. Abundant Tau Filaments and Nonapoptotic Neurodegeneration in Transgenic Mice Expressing Human P301S Tau Protein. J. Neurosci. 2002, 22, 9340–9351. [Google Scholar] [CrossRef]
- Mc Kenna, M.C.; Tilcion, J.T.; Stevenson, J.H.; Huang, X. New Insights into the Compartmentation of Glutamate and Glutamine in Cultured Rat Brain Astrocytes. Dev. Neurosci. 1996, 18, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, J.; Sonnewald, U.; Waagepetersen, H.S.; Schousboe, A. Glutamine in the Central Nervous System: Function and Dysfunction. Front. Biosci. 2007, 12, 332–343. [Google Scholar] [CrossRef]
- Cuellar-Santoyo, A.O.; Ruiz-Rodríguez, V.M.; Mares-Barbosa, T.B.; Patrón-Soberano, A.; Howe, A.G.; Portales-Pérez, D.P.; Miquelajáuregui Graf, A.; Estrada-Sánchez, A.M. Revealing the Contribution of Astrocytes to Glutamatergic Neuronal Transmission. Front. Cell Neurosci. 2023, 16, 1037641. [Google Scholar] [CrossRef] [PubMed]
- de Wit, H.; Walter, A.M.; Milosevic, I.; Gulyás-Kovács, A.; Riedel, D.; Sørensen, J.B.; Verhage, M. Synaptotagmin-1 Docks Secretory Vesicles to Syntaxin-1/SNAP-25 Acceptor Complexes. Cell 2009, 138, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, F.A.; Loland, C.J.; Ortega, A.; Schousboe, A. Special Issue on Neurotransmitter Transporters. Neuropharmacology 2019, 161, 107859. [Google Scholar] [CrossRef]
- Rothstein, D.M.; Pahel, G.; Tyler, B.; Magasanik, B. Regulation of Expression from the GlnA Promoter of Escherichia Coli in the Absence of Glutamine Synthetase. Proc. Natl. Acad. Sci. USA 1980, 77, 7372–7376. [Google Scholar] [CrossRef]
- Schousboe, A. Role of Astrocytes in the Maintenance and Modulation of Glutamatergic and GABAergic Neurotransmission. Neurochem. Res. 2003, 28, 347–352. [Google Scholar] [CrossRef]
- Martinez-Hernandez, A.; Bell, K.P.; Norenberg, M.D. Glutamine Synthetase: Glial Localization in Brain. Science 1977, 195, 1356–1358. [Google Scholar] [CrossRef] [PubMed]
- Bak, L.K.; Schousboe, A.; Waagepetersen, H.S. The Glutamate/GABA-Glutamine Cycle: Aspects of Transport, Neurotransmitter Homeostasis and Ammonia Transfer. J. Neurochem. 2006, 98, 641–653. [Google Scholar] [CrossRef] [PubMed]
- Norenberg, M.D.; Martinez-Hernandez, A. Fine Structural Localization of Glutamine Synthetase in Astrocytes of Rat Brain. Brain Res. 1979, 161, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Kvamme, E.; Torgner, I.A.; Roberg, B. Kinetics and Localization of Brain Phosphate Activated Glutaminase. J. Neurosci. Res. 2001, 66, 951–958. [Google Scholar] [CrossRef]
- Hertz, L.; Dringen, R.; Schousboe, A.; Robinson, S.R. Astrocytes: Glutamate Producers for Neurons. J. Neurosci. Res. 1999, 57, 417–428. [Google Scholar] [CrossRef]
- Schousboe, A.; Hertz, L.; Svenneby, G.; Kvamme, E. PHOSPHATE ACTIVATED GLUTAMINASE ACTIVITY AND GLUTAMINE UPTAKE IN PRIMARY CULTURES OF ASTROCYTES. J. Neurochem. 1979, 32, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Drejer, J.; Larsson, O.M.; Schousboe, A. Characterization of L-Glutamate Uptake into and Release from Astrocytes and Neurons Cultured from Different Brain Regions. Exp. Brain Res. 1982, 47, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Larsson, O.M.; Hertz, L.; Schousboe, A. GABA Uptake in Astrocytes in Primary Cultures: Coupling with Two Sodium Ions. J. Neurosci. Res. 1980, 5, 469–477. [Google Scholar] [CrossRef]
- Dalile, B.; Van Oudenhove, L.; Vervliet, B.; Verbeke, K. The Role of Short-Chain Fatty Acids in Microbiota-Gut-Brain Communication. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 461–478. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, H.; Zhang, X.; Wang, W.; Chen, Y.; Cai, Z.; Wang, Q.; Wang, J.; Shi, Y. Promotion of Astrocyte-Neuron Glutamate-Glutamine Shuttle by SCFA Contributes to the Alleviation of Alzheimer’s Disease. Redox Biol. 2023, 62, 102690. [Google Scholar] [CrossRef] [PubMed]
- Danbolt, N.C. Glutamate Uptake. Prog. Neurobiol. 2001, 65, 1–105. [Google Scholar] [CrossRef] [PubMed]
- Zerangue, N.; Kavanaugh, M.P. ASCT-1 Is a Neutral Amino Acid Exchanger with Chloride Channel Activity. J. Biol. Chem. 1996, 271, 27991–27994. [Google Scholar] [CrossRef] [PubMed]
- Levy, L.M.; Warr, O.; Attwell, D. Stoichiometry of the Glial Glutamate Transporter GLT-1 Expressed Inducibly in a Chinese Hamster Ovary Cell Line Selected for Low Endogenous Na+-Dependent Glutamate Uptake. J. Neurosci. 1998, 18, 9620–9628. [Google Scholar] [CrossRef]
- Bröer, S. Molecular mechanisms of glutamate and glutamine transport in astrocytes. In The Role of Glia in Neurotoxicity; CRC Press: Boca Raton, FL, USA, 2004; pp. 113–130. [Google Scholar] [CrossRef]
- Amara, S.G.; Fontana, A.C.K. Excitatory Amino Acid Transporters: Keeping up with Glutamate. Neurochem. Int. 2002, 41, 313–318. [Google Scholar] [CrossRef]
- Kanner, B.I. Structure and Function of Sodium-Coupled GABA and Glutamate Transporters. J. Membr. Biol. 2006, 213, 89–100. [Google Scholar] [CrossRef]
- Schousboe, A.; Sarup, A.; Bak, L.K.; Waagepetersen, H.S.; Larsson, O.M. Role of Astrocytic Transport Processes in Glutamatergic and GABAergic Neurotransmission. Neurochem. Int. 2004, 45, 521–527. [Google Scholar] [CrossRef]
- Palacín, M.; Estévez, R.; Bertran, J.; Zorzano, A. Molecular Biology of Mammalian Plasma Membrane Amino Acid Transporters. Physiol. Rev. 1998, 78, 969–1054. [Google Scholar] [CrossRef] [PubMed]
- Hediger, M.A. Membrane Permeability. The Diversity of Transmembrane Transport Processes. Curr. Opin. Cell Biol. 1997, 9, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, F.A.; Reimer, R.J.; Edwards, R.H. The Glutamine Commute: Take the N Line and Transfer to the A. J. Cell Biol. 2002, 157, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Bröer, A.; Albers, A.; Setiawan, I.; Edwards, R.H.; Chaudhry, F.A.; Lang, F.; Wagner, C.A.; Bröer, S. Regulation of the Glutamine Transporter SN1 by Extracellular PH and Intracellular Sodium Ions. J. Physiol. 2002, 539, 3. [Google Scholar] [CrossRef] [PubMed]
- Bröer, S.; Brookes, N. Transfer of Glutamine between Astrocytes and Neurons. J. Neurochem. 2001, 77, 705–719. [Google Scholar] [CrossRef] [PubMed]
- Segawa, H.; Fukasawa, Y.; Miyamoto, K.I.; Takeda, E.; Endou, H.; Kanai, Y. Identification and Functional Characterization of a Na+-Independent Neutral Amino Acid Transporter with Broad Substrate Selectivity. J. Biol. Chem. 1999, 274, 19745–19751. [Google Scholar] [CrossRef] [PubMed]
- Christensen, H.N. Organic Ion Transport during Seven Decades. The Amino Acids. Biochim. Biophys. Acta 1984, 779, 255–269. [Google Scholar] [CrossRef] [PubMed]
- Arriza, J.L.; Kavanaugh, M.P.; Fairman, W.A.; Wu, Y.N.; Murdoch, G.H.; North, R.A.; Amara, S.G. Cloning and Expression of a Human Neutral Amino Acid Transporter with Structural Similarity to the Glutamate Transporter Gene Family. J. Biol. Chem. 1993, 268, 15329–15332. [Google Scholar] [CrossRef]
- Utsunomiya-Tate, N.; Endou, H.; Kanai, Y. Cloning and Functional Characterization of a System ASC-like Na+-Dependent Neutral Amino Acid Transporter. J. Biol. Chem. 1996, 271, 14883–14890. [Google Scholar] [CrossRef]
- Bröer, A.; Brookes, N.; Ganapathy, V.; Dimmer, K.S.; Wagner, C.A.; Lang, F.; Bröer, S. The Astroglial ASCT2 Amino Acid Transporter as a Mediator of Glutamine Efflux. J. Neurochem. 1999, 73, 2184–2194. [Google Scholar] [CrossRef]
- Nagaraja, T.N.; Brookes, N. Glutamine Transport in Mouse Cerebral Astrocytes. J. Neurochem. 1996, 66, 1665–1674. [Google Scholar] [CrossRef]
- Su, T.Z.; Campbell, G.W.; Oxender, D.L. Glutamine Transport in Cerebellar Granule Cells in Culture. Brain Res. 1997, 757, 69–78. [Google Scholar] [CrossRef]
- Pineda, M.; Fernández, E.; Torrents, D.; Estévez, R.; López, C.; Camps, M.; Lloberas, J.; Zorzano, A.; Palacín, M. Identification of a Membrane Protein, LAT-2, That Co-Expresses with 4F2 Heavy Chain, an L-Type Amino Acid Transport Activity with Broad Specificity for Small and Large Zwitterionic Amino Acids. J. Biol. Chem. 1999, 274, 19738–19744. [Google Scholar] [CrossRef] [PubMed]
- Rossier, G.; Meier, C.; Bauch, C.; Summa, V.; Sordat, B.; Verrey, F.; Kühn, L.C. LAT2, a New Basolateral 4F2hc/CD98-Associated Amino Acid Transporter of Kidney and Intestine. J. Biol. Chem. 1999, 274, 34948–34954. [Google Scholar] [CrossRef] [PubMed]
- Varoqui, H.; Zhu, H.; Yao, D.; Ming, H.; Erickson, J.D. Cloning and Functional Identification of a Neuronal Glutamine Transporter. J. Biol. Chem. 2000, 275, 4049–4054. [Google Scholar] [CrossRef] [PubMed]
- Reimer, R.J.; Chaudhry, F.A.; Gray, A.T.; Edwards, R.H. Amino Acid Transport System a Resembles System N in Sequence but Differs in Mechanism. Proc. Natl. Acad. Sci. USA 2000, 97, 7715–7720. [Google Scholar] [CrossRef] [PubMed]
- Yao, D.; Mackenzie, B.; Ming, H.; Varoqui, H.; Zhu, H.; Hediger, M.A.; Erickson, J.D. A Novel System A Isoform Mediating Na+/Neutral Amino Acid Cotransport. J. Biol. Chem. 2000, 275, 22790–22797. [Google Scholar] [CrossRef]
- Kilberg, M.S.; Handlogten, M.E.; Christensen, H.N. Characteristics of an Amino Acid Transport System in Rat Liver for Glutamine, Asparagine, Histidine, and Closely Related Analogs. J. Biol. Chem. 1980, 255, 4011–4019. [Google Scholar] [CrossRef] [PubMed]
- Boulland, J.L.; Osen, K.K.; Levy, L.M.; Danbolt, N.C.; Edwards, R.H.; Storm-Mathisen, J.; Chaudhry, F.A. Cell-Specific Expression of the Glutamine Transporter SN1 Suggests Differences in Dependence on the Glutamine Cycle. Eur. J. Neurosci. 2002, 15, 1615–1631. [Google Scholar] [CrossRef]
- Chaudhry, F.A.; Reimer, R.J.; Krizaj, D.; Barber, D.; Storm-Mathisen, J.; Copenhagen, D.R.; Edwards, R.H. Molecular Analysis of System N Suggests Novel Physiological Roles in Nitrogen Metabolism and Synaptic Transmission. Cell 1999, 99, 769–780. [Google Scholar] [CrossRef]
- Aldana, B.I.; Zhang, Y.; Jensen, P.; Chandrasekaran, A.; Christensen, S.K.; Nielsen, T.T.; Nielsen, J.E.; Hyttel, P.; Larsen, M.R.; Waagepetersen, H.S.; et al. Glutamate-Glutamine Homeostasis Is Perturbed in Neurons and Astrocytes Derived from Patient IPSC Models of Frontotemporal Dementia. Mol. Brain 2020, 13, 125. [Google Scholar] [CrossRef]
- Goedert, M. Neurodegeneration. Alzheimer’s and Parkinson’s Diseases: The Prion Concept in Relation to Assembled Aβ, Tau, and α-Synuclein. Science 2015, 349, 1255555. [Google Scholar] [CrossRef]
- Arendt, T.; Stieler, J.T.; Holzer, M. Tau and Tauopathies. Brain Res. Bull. 2016, 126, 238–292. [Google Scholar] [CrossRef]
- Binder, L.I.; Frankfurter, A.; Rebhun, L.I. The Distribution of Tau in the Mammalian Central Nervous System. J. Cell Biol. 1985, 101, 1371–1378. [Google Scholar] [CrossRef] [PubMed]
- Spillantini, M.G.; Goedert, M. Tau Pathology and Neurodegeneration. Lancet Neurol. 2013, 12, 609–622. [Google Scholar] [CrossRef] [PubMed]
- Goedert, M.; Spillantini, M.G.; Crowther, R.A. Cloning of a Big Tau Microtubule-Associated Protein Characteristic of the Peripheral Nervous System. Proc. Natl. Acad. Sci. USA 1992, 89, 1983–1987. [Google Scholar] [CrossRef]
- Goedert, M.; Spillantini, M.G.; Jakes, R.; Rutherford, D.; Crowther, R.A. Multiple Isoforms of Human Microtubule-Associated Protein Tau: Sequences and Localization in Neurofibrillary Tangles of Alzheimer’s Disease. Neuron 1989, 3, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Goedert, M.; Eisenberg, D.S.; Crowther, R.A. Propagation of Tau Aggregates and Neurodegeneration. Annu. Rev. Neurosci. 2017, 40, 189–210. [Google Scholar] [CrossRef] [PubMed]
- Basso, M.; Bonetto, V. Extracellular Vesicles and a Novel Form of Communication in the Brain. Front. Neurosci. 2016, 10, 127. [Google Scholar] [CrossRef] [PubMed]
- Spillantini, M.G.; Van Swieten, J.C.; Goedert, M. Tau Gene Mutations in Frontotemporal Dementia and Parkinsonism Linked to Chromosome 17 (FTDP-17). Neurogenetics 2000, 2, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Rizzu, P.; Van Swieten, J.C.; Joosse, M.; Hasegawa, M.; Stevens, M.; Tibben, A.; Niermeijer, M.F.; Hillebrand, M.; Ravid, R.; Oostra, B.A.; et al. High Prevalence of Mutations in the Microtubule-Associated Protein Tau in a Population Study of Frontotemporal Dementia in the Netherlands. Am. J. Hum. Genet. 1999, 64, 414–421. [Google Scholar] [CrossRef]
- Ulrich, G.; Salvadè, A.; Boersema, P.; Calì, T.; Foglieni, C.; Sola, M.; Picotti, P.; Papin, S.; Paganetti, P. Phosphorylation of Nuclear Tau Is Modulated by Distinct Cellular Pathways. Sci. Rep. 2018, 8, 17702. [Google Scholar] [CrossRef]
- Sola, M.; Rendon-Angel, A.; Rojo Martinez, V.; Sgrignani, J.; Magrin, C.; Piovesana, E.; Cavalli, A.; Paganetti, P.; Papin, S. Tau Protein Binds to the P53 E3 Ubiquitin Ligase MDM2. Sci. Rep. 2023, 13, 10208. [Google Scholar] [CrossRef]
- Delobel, P.; Flament, S.; Hamdane, M.; Jakes, R.; Rousseau, A.; Delacourte, A.; Vilain, J.P.; Goedert, M.; Buée, L. Functional Characterization of FTDP-17 Tau Gene Mutations through Their Effects on Xenopus Oocyte Maturation. J. Biol. Chem. 2002, 277, 9199–9205. [Google Scholar] [CrossRef]
- Lewis, J.; McGowan, E.; Rockwood, J.; Melrose, H.; Nacharaju, P.; Van Slegtenhorst, M.; Gwinn-Hardy, K.; Murphy, M.P.; Baker, M.; Yu, X.; et al. Neurofibrillary Tangles, Amyotrophy and Progressive Motor Disturbance in Mice Expressing Mutant (P301L) Tau Protein. Nat. Genet. 2000, 25, 402–405. [Google Scholar] [CrossRef] [PubMed]
- Mothes, T.; Portal, B.; Konstantinidis, E.; Eltom, K.; Libard, S.; Streubel-Gallasch, L.; Ingelsson, M.; Rostami, J.; Lindskog, M.; Erlandsson, A. Astrocytic Uptake of Neuronal Corpses Promotes Cell-to-Cell Spreading of Tau Pathology. Acta Neuropathol. Commun. 2023, 11, 97. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Bhaskar, K. Degradation and Transmission of Tau by Autophagic-Endolysosomal Networks and Potential Therapeutic Targets for Tauopathy. Front. Mol. Neurosci. 2020, 13, 586731. [Google Scholar] [CrossRef] [PubMed]
- Sidoryk-Wegrzynowicz, M.; Strużyńska, L. Dysfunctional Glia: Contributors to Neurodegenerative Disorders. Neural Regen. Res. 2021, 16, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Sheng, S.; Wang, Y.; Ding, L.; Xu, X.; Xia, X.; Zheng, J.C. Astrocyte-Derived Extracellular Vesicles: A Double-Edged Sword in Central Nervous System Disorders. Neurosci. Biobehav. Rev. 2021, 125, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Phatnani, H.; Maniatis, T. Astrocytes in Neurodegenerative Disease. Cold Spring Harb. Perspect. Biol. 2015, 7, a020628. [Google Scholar] [CrossRef] [PubMed]
- Mohn, T.C.; Koob, A.O. Adult Astrogenesis and the Etiology of Cortical Neurodegeneration. J. Exp. Neurosci. 2015, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.X.; Cheng, S.S.; Chen, L.; Wang, Q.H.; Shi, Y.; Xu, Y.; Yin, Z.Y.; Chen, G.Q. Astroglial Activation and Tau Hyperphosphorylation Precede to Neuron Loss in a Neurodegenerative Mouse Model. CNS Neurosci. Ther. 2016, 22, 244–247. [Google Scholar] [CrossRef]
- Davies, J.E.; Pröschel, C.; Zhang, N.; Noble, M.; Mayer-Pröschel, M.; Davies, S.J.A. Transplanted Astrocytes Derived from BMP- or CNTF-Treated Glial-Restricted Precursors Have Opposite Effects on Recovery and Allodynia after Spinal Cord Injury. J. Biol. 2008, 7, 24. [Google Scholar] [CrossRef]
- Lepore, A.C.; Rauck, B.; Dejea, C.; Pardo, A.C.; Rao, M.S.; Rothstein, J.D.; Maragakis, N.J. Focal Transplantation-Based Astrocyte Replacement Is Neuroprotective in a Model of Motor Neuron Disease. Nat. Neurosci. 2008, 11, 1294–1301. [Google Scholar] [CrossRef]
- Boucherie, C.; Schäfer, S.; Lavand’homme, P.; Maloteaux, J.M.; Hermans, E. Chimerization of Astroglial Population in the Lumbar Spinal Cord after Mesenchymal Stem Cell Transplantation Prolongs Survival in a Rat Model of Amyotrophic Lateral Sclerosis. J. Neurosci. Res. 2009, 87, 2034–2046. [Google Scholar] [CrossRef]
- Sofroniew, M.V. Molecular Dissection of Reactive Astrogliosis and Glial Scar Formation. Trends Neurosci. 2009, 32, 638–647. [Google Scholar] [CrossRef]
- Liddelow, S.A.; Guttenplan, K.A.; Clarke, L.E.; Bennett, F.C.; Bohlen, C.J.; Schirmer, L.; Bennett, M.L.; Münch, A.E.; Chung, W.-S.; Peterson, T.C.; et al. Neurotoxic Reactive Astrocytes Are Induced by Activated Microglia HHS Public Access. Nature 2017, 541, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Sadick, J.S.; Liddelow, S.A. Don’t Forget Astrocytes When Targeting Alzheimer’s Disease. Br. J. Pharmacol. 2019, 176, 3585–3598. [Google Scholar] [CrossRef]
- Sidoryk-Węgrzynowicz, M.; Struzyńska, L. Astroglial Contribution to Tau-Dependent Neurodegeneration. Biochem. J. 2019, 476, 3493–3504. [Google Scholar] [CrossRef]
- Li, B.; Xia, M.; Zorec, R.; Parpura, V.; Verkhratsky, A. Astrocytes in Heavy Metal Neurotoxicity and Neurodegeneration. Brain Res. 2021, 1752, 147234. [Google Scholar] [CrossRef]
- Hampton, D.W.; Webber, D.J.; Bilican, B.; Goedert, M.; Spillantini, M.G.; Chandran, S. Cell-Mediated Neuroprotection in a Mouse Model of Human Tauopathy. J. Neurosci. 2010, 30, 9973–9983. [Google Scholar] [CrossRef] [PubMed]
- Sidoryk-Wegrzynowicz, M.; Gerber, Y.N.; Ries, M.; Sastre, M.; Tolkovsky, A.M.; Spillantini, M.G. Astrocytes in Mouse Models of Tauopathies Acquire Early Deficits and Lose Neurosupportive Functions. Acta Neuropathol. Commun. 2017, 5, 89. [Google Scholar] [CrossRef]
- Crescenzi, R.; DeBrosse, C.; Nanga, R.P.R.; Reddy, S.; Haris, M.; Hariharan, H.; Iba, M.; Lee, V.M.Y.; Detre, J.A.; Borthakur, A.; et al. In Vivo Measurement of Glutamate Loss Is Associated with Synapse Loss in a Mouse Model of Tauopathy. Neuroimage 2014, 101, 185–192. [Google Scholar] [CrossRef]
- Ginsberg, S.D.; Martin, L.J.; Rothstein, J.D. Regional Deafferentation Down-Regulates Subtypes of Glutamate Transporter Proteins. J. Neurochem. 1995, 65, 2800–2803. [Google Scholar] [CrossRef]
- Burbaeva, G.S.; Boksha, I.S.; Tereshkina, E.B.; Savushkina, O.K.; Prokhorova, T.A.; Vorobyeva, E.A. Glutamate and GABA-Metabolizing Enzymes in Post-Mortem Cerebellum in Alzheimer’s Disease: Phosphate-Activated Glutaminase and Glutamic Acid Decarboxylase. Cerebellum 2014, 13, 607–615. [Google Scholar] [CrossRef]
- Hasel, P.; Dando, O.; Jiwaji, Z.; Baxter, P.; Todd, A.C.; Heron, S.; Márkus, N.M.; McQueen, J.; Hampton, D.W.; Torvell, M.; et al. Neurons and Neuronal Activity Control Gene Expression in Astrocytes to Regulate Their Development and Metabolism. Nat. Commun. 2017, 8, 15132. [Google Scholar] [CrossRef] [PubMed]
- Sidoryk-Węgrzynowicz, M.; Dąbrowska-Bouta, B.; Sulkowski, G.; Strużyńska, L. Mutant Tau Protein-Induced Abnormalities in the Na+-Dependent Glutamine Translocation and Recycling and Their Impact on Astrocyte-Neuron Integrity in Vitro. Neurochem. Int. 2023, 168, 105551. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, L.H.; Rae, C.; Ittner, L.M.; Götz, J.; Sonnewald, U. Glutamate Metabolism Is Impaired in Transgenic Mice with Tau Hyperphosphorylation. J. Cereb. Blood Flow Metab. 2013, 33, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Vemula, P.; Jing, Y.; Zhang, H.; Hunt, J.B.; Sandusky-Beltran, L.A.; Lee, D.C.; Liu, P. Altered Brain Arginine Metabolism in a Mouse Model of Tauopathy. Amino Acids 2019, 51, 513–528. [Google Scholar] [CrossRef] [PubMed]
| Amino Acids Transporting System in the CNS | Variant(s); Cellular Specificity; Noticeable Activity | Competitive Substrate Used for the Functional Study | References |
|---|---|---|---|
| N | SNAT3, SNAT5; astrocyte | MeAIB, Thr, Leu | [32,33] |
| A | SNAT1, SNAT2; astrocyte/neuron | Thr, Leu, His | [34] |
| ASC | ASCT1; astrocyte | MeAIB, His, Leu | [32] |
| L | LAT1, LAT2; neuron | MeAIB, Thr, His | [35] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sidoryk-Węgrzynowicz, M.; Adamiak, K.; Strużyńska, L. Astrocyte–Neuron Interaction via the Glutamate–Glutamine Cycle and Its Dysfunction in Tau-Dependent Neurodegeneration. Int. J. Mol. Sci. 2024, 25, 3050. https://doi.org/10.3390/ijms25053050
Sidoryk-Węgrzynowicz M, Adamiak K, Strużyńska L. Astrocyte–Neuron Interaction via the Glutamate–Glutamine Cycle and Its Dysfunction in Tau-Dependent Neurodegeneration. International Journal of Molecular Sciences. 2024; 25(5):3050. https://doi.org/10.3390/ijms25053050
Chicago/Turabian StyleSidoryk-Węgrzynowicz, Marta, Kamil Adamiak, and Lidia Strużyńska. 2024. "Astrocyte–Neuron Interaction via the Glutamate–Glutamine Cycle and Its Dysfunction in Tau-Dependent Neurodegeneration" International Journal of Molecular Sciences 25, no. 5: 3050. https://doi.org/10.3390/ijms25053050
APA StyleSidoryk-Węgrzynowicz, M., Adamiak, K., & Strużyńska, L. (2024). Astrocyte–Neuron Interaction via the Glutamate–Glutamine Cycle and Its Dysfunction in Tau-Dependent Neurodegeneration. International Journal of Molecular Sciences, 25(5), 3050. https://doi.org/10.3390/ijms25053050






